Pancreatitis

On this page
🔥 The Pancreatic Inferno: When Digestive Fire Burns Out of Control
Pancreatitis transforms the pancreas from a quiet digestive organ into a site of catastrophic self-destruction, where the body's own enzymes turn inward to digest living tissue. You'll master the pathophysiology driving this enzymatic avalanche, recognize the clinical patterns that distinguish mild from life-threatening disease, and deploy the diagnostic and therapeutic strategies that can mean the difference between recovery and multi-organ failure. This lesson builds your ability to rapidly assess severity, navigate complex treatment algorithms, and understand how local pancreatic inflammation cascades into systemic crisis affecting every major organ system.
📌 Remember: GET SMASHED - Gallstones, Ethanol, Trauma, Steroids, Mumps, Autoimmune, Scorpion stings, Hyperlipidemia, ERCP, Drugs. This mnemonic covers 85% of acute pancreatitis cases, with gallstones (45%) and alcohol (35%) dominating the landscape.
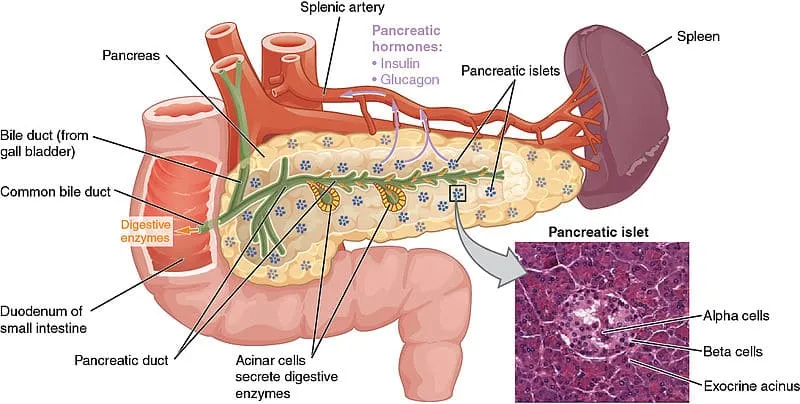
The pancreas operates through two distinct functional units: the exocrine system producing 20+ digestive enzymes and the endocrine system secreting 4 major hormones. Pancreatitis primarily affects the exocrine component, where acinar cells normally produce inactive enzyme precursors (zymogens) that activate only upon reaching the duodenum.
- Acute Pancreatitis Spectrum
- Mild cases: 80% of presentations, mortality <1%
- Moderately severe: 15% of cases, mortality 5-10%
- Local complications present
- Transient organ failure <48 hours
- Severe pancreatitis: 5% of cases, mortality 15-30%
- Persistent organ failure >48 hours
- Pancreatic necrosis >30% of gland
⭐ Clinical Pearl: The "48-hour rule" distinguishes severity - persistent organ dysfunction beyond 48 hours defines severe acute pancreatitis and dramatically increases mortality risk from <5% to >20%.
| Parameter | Mild | Moderate | Severe |
|---|---|---|---|
| Organ Failure | None | Transient (<48h) | Persistent (>48h) |
| Local Complications | None | Present | Present |
| Mortality Rate | <1% | 5-10% | 15-30% |
| ICU Requirement | Rare | 25% | 85% |
| Length of Stay | 3-5 days | 7-14 days | 21+ days |
The pathophysiology centers on premature trypsinogen activation within pancreatic acinar cells. Normally, trypsinogen remains inactive until duodenal enterokinase converts it to trypsin. In pancreatitis, intracellular calcium overload and lysosomal enzyme release trigger premature activation, creating a proteolytic cascade that digests pancreatic tissue, blood vessels, and surrounding structures.
Understanding pancreatitis transforms your approach to abdominal pain evaluation, as this condition can mimic 15+ different diagnoses while potentially causing life-threatening complications within hours of onset.
🔥 The Pancreatic Inferno: When Digestive Fire Burns Out of Control
⚡ The Enzymatic Avalanche: Cellular Chaos Unleashed
📌 Remember: TAILS describes the enzymatic cascade - Trypsin activates All other enzymes, Including Lipase and elaStase. Once trypsin forms, it becomes an autocatalytic process where trypsin activates more trypsinogen, creating exponential enzyme production.
The "first hit" in pancreatitis involves disruption of normal cellular calcium homeostasis. Acinar cells normally maintain cytoplasmic calcium at 100 nanomolar, but triggering events cause sustained elevation to >1 micromolar. This 10-fold increase overwhelms protective mechanisms and triggers colocalization of digestive enzymes with lysosomal hydrolases.
- Pathophysiological Cascade Stages
- Stage 1: Acinar cell injury (0-6 hours)
- Calcium overload and membrane damage
- Premature enzyme activation begins
- Stage 2: Local inflammation (6-24 hours)
- Cytokine release: TNF-α, IL-1β, IL-6
- Complement activation and neutrophil recruitment
- Stage 3: Systemic response (24-72 hours)
- SIRS development in 25% of cases
- Capillary leak and third-spacing
- Potential organ dysfunction
- Stage 1: Acinar cell injury (0-6 hours)
⭐ Clinical Pearl: Lipase elevation persists longer than amylase because lipase has a longer half-life (7-14 hours vs 2-4 hours). Lipase levels >3 times normal maintain 95% specificity for pancreatitis, while amylase can normalize within 24-48 hours despite ongoing pancreatic inflammation.
| Enzyme | Normal Range | Half-Life | Peak Time | Duration Elevated |
|---|---|---|---|---|
| Amylase | 30-110 U/L | 2-4 hours | 6-12 hours | 3-5 days |
| Lipase | 10-140 U/L | 7-14 hours | 24-48 hours | 7-14 days |
| Trypsinogen | <50 ng/mL | 1-2 hours | 2-6 hours | 2-4 days |
| Elastase-1 | <200 ng/mL | 4-6 hours | 12-24 hours | 5-7 days |
| Phospholipase A2 | <10 ng/mL | 3-5 hours | 24-72 hours | 7-10 days |
💡 Master This: The transition from local to systemic disease occurs when pancreatic inflammation overwhelms local containment mechanisms. Elastase degrades blood vessel walls, phospholipase A2 destroys cell membranes, and trypsin activates complement cascades, creating the perfect storm for multi-organ dysfunction.
Understanding this enzymatic avalanche reveals why early intervention focuses on "pancreatic rest" and aggressive supportive care rather than specific enzyme inhibitors, as the cascade becomes self-perpetuating once established.
⚡ The Enzymatic Avalanche: Cellular Chaos Unleashed
🎯 Pattern Recognition Mastery: Decoding the Pancreatic Crisis
📌 Remember: PANCREAS for classic presentation - Pain (epigastric, radiating to back), Amylase/lipase elevated, Nausea/vomiting, CT changes, Risk factors present, Epigastric tenderness, Alcohol/gallstone history, Systemic signs. This constellation appears in 60% of acute cases.
The pain pattern provides the strongest diagnostic clue. Classic pancreatic pain demonstrates specific characteristics that distinguish it from other abdominal conditions:
- Classic Pain Pattern Recognition
- Location: Epigastric (85%), left upper quadrant (60%)
- Radiates to back in 70% of cases
- Band-like distribution across upper abdomen
- Character: Constant, boring, deep visceral pain
- Intensity 8-10/10 in 80% of acute cases
- Described as "worst pain ever" in 45%
- Positional factors:
- Worse when supine (90% of patients)
- Relief with sitting forward (75%)
- No relief with antacids or position changes
- Location: Epigastric (85%), left upper quadrant (60%)
⭐ Clinical Pearl: The "pancreatic position" - patients sitting forward with knees drawn up - appears in 75% of acute pancreatitis cases. This position reduces retroperitoneal pressure and provides partial pain relief, distinguishing pancreatic pain from peptic ulcer disease or biliary colic.
Laboratory pattern recognition requires understanding the temporal evolution of pancreatic enzymes. The "lipase-to-amylase ratio" provides diagnostic insights:
| Clinical Scenario | Lipase:Amylase Ratio | Diagnostic Significance |
|---|---|---|
| Acute Pancreatitis | >2:1 | Classic pattern, 85% sensitivity |
| Chronic Pancreatitis | <1:1 | Reduced enzyme production |
| Alcohol-Related | >3:1 | Lipase predominance typical |
| Gallstone Pancreatitis | 1.5-2.5:1 | Moderate elevation pattern |
| Late Presentation | Variable | Amylase normalizes first |
Atypical presentations challenge diagnostic skills and occur more frequently in specific populations:
- High-Risk Atypical Presentations
- Elderly patients (>70 years): 40% present atypically
- Minimal pain in 25% of cases
- Confusion or altered mental status in 15%
- Hypotension without obvious cause
- Diabetic patients: 30% have atypical presentations
- Neuropathy masks classic pain patterns
- DKA may be presenting feature
- Post-operative patients: 50% have delayed recognition
- Pain attributed to surgical procedure
- Enzyme elevation dismissed as surgical stress
- Elderly patients (>70 years): 40% present atypically
The "silent pancreatitis" pattern appears in 15% of cases and carries higher mortality (25% vs 8%) due to delayed recognition. These patients present with systemic complications before obvious pancreatic symptoms develop.
Mastering these patterns enables rapid triage decisions and appropriate resource allocation, as early recognition within 6 hours significantly improves outcomes across all severity categories.
🎯 Pattern Recognition Mastery: Decoding the Pancreatic Crisis
🔬 Diagnostic Precision: The Investigative Arsenal
📌 Remember: LAB-CT for diagnostic workup - Lipase (most specific), Amylase (rapid but less specific), Basic metabolic panel (complications), CT scan (severity assessment), Triglycerides (etiology). This sequence provides comprehensive evaluation within 2-4 hours of presentation.
Laboratory diagnostics follow a hierarchical approach based on clinical probability and severity assessment:
- Tier 1 - Emergency Department Essentials
- Lipase: >3x normal = 95% specificity
- Peak levels 24-48 hours after onset
- Remains elevated 7-14 days
- Amylase: >3x normal = 85% specificity
- Rapid elevation within 6 hours
- Normalizes by 48-72 hours
- Basic metabolic panel: Identifies complications
- BUN >20 mg/dL predicts severe disease
- Creatinine >1.8 mg/dL indicates renal involvement
- Lipase: >3x normal = 95% specificity
⭐ Clinical Pearl: Lipase-to-amylase ratio >2:1 suggests alcohol-related pancreatitis with 80% accuracy. Chronic alcohol use preferentially damages lipase-producing cells, creating this characteristic pattern that helps identify etiology before detailed history is available.
Advanced laboratory assessment becomes crucial for severity stratification and etiology determination:
| Test Category | Specific Tests | Clinical Significance | Timing |
|---|---|---|---|
| Severity Markers | CRP, Procalcitonin | CRP >150 mg/L = severe disease | 48-72 hours |
| Organ Function | LFTs, Lactate, ABG | Multi-organ assessment | 0-24 hours |
| Etiology Workup | Triglycerides, Calcium | TG >1000 mg/dL causative | Initial |
| Complications | D-dimer, Fibrinogen | Coagulopathy screening | 24-48 hours |
| Nutritional | Albumin, Prealbumin | Synthetic function | 72+ hours |
Imaging strategy follows a risk-stratified approach that balances diagnostic yield with resource utilization:
- CT Imaging Indications
- Diagnostic uncertainty after laboratory evaluation
- Clinical deterioration despite appropriate therapy
- Severe disease by clinical scoring systems
- Suspected complications (fever, leukocytosis, organ dysfunction)
- Failed improvement by 48-72 hours
The "48-hour rule" for CT imaging prevents unnecessary early scanning while ensuring appropriate severity assessment. Early CT (<48 hours) underestimates necrosis in 40% of cases, while delayed CT (>72 hours) may miss optimal intervention windows.
Specialized imaging becomes necessary for complex cases and intervention planning:
-
MRCP (Magnetic Resonance Cholangiopancreatography)
- Ductal anatomy evaluation without contrast
- Biliary obstruction assessment
- Chronic changes detection
- Sensitivity >95% for ductal abnormalities
-
Endoscopic Ultrasound (EUS)
- Tissue sampling capability
- Vascular involvement assessment
- Small lesion detection (<2cm)
- Chronic pancreatitis staging
This diagnostic arsenal enables rapid triage, accurate severity assessment, and appropriate resource allocation, transforming pancreatitis management from reactive to proactive care.
🔬 Diagnostic Precision: The Investigative Arsenal
⚖️ Treatment Algorithms: Evidence-Based Crisis Management
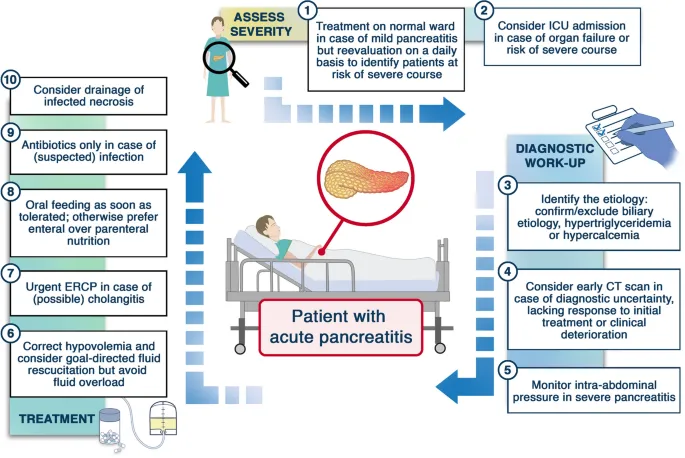
📌 Remember: FLUID-FAST for initial management - Fluid resuscitation (aggressive early), Lactated Ringer's preferred, Urine output monitoring, Infection prevention, Diet advancement when tolerated, Fasting initially, Analgesia (avoid morphine), Support organs, Thromboprophylaxis. This protocol reduces severe disease progression by 40%.
Fluid resuscitation represents the cornerstone intervention with specific protocols that dramatically impact outcomes:
- Fluid Resuscitation Protocol
- Initial bolus: 20 mL/kg lactated Ringer's over 30 minutes
- Reassess hemodynamics and urine output
- Repeat bolus if inadequate response
- Maintenance therapy: 1.5-3 mL/kg/hour based on response
- Target urine output >0.5 mL/kg/hour
- Monitor for fluid overload signs
- Goal parameters within 24 hours:
- Heart rate <120 bpm
- Mean arterial pressure >65 mmHg
- Urine output >0.5 mL/kg/hour
- Hematocrit 35-44%
- Initial bolus: 20 mL/kg lactated Ringer's over 30 minutes
⭐ Clinical Pearl: Lactated Ringer's solution reduces systemic inflammatory response compared to normal saline, decreasing CRP levels by 30% and pain scores by 25%. The balanced electrolyte composition prevents hyperchloremic acidosis that can worsen pancreatic inflammation.
| Fluid Type | Advantages | Disadvantages | Recommendation |
|---|---|---|---|
| Lactated Ringer's | Balanced, anti-inflammatory | Avoid in liver failure | First-line choice |
| Normal Saline | Widely available | Hyperchloremic acidosis | Second-line only |
| Albumin | Oncotic pressure | Expensive, limited benefit | Severe cases only |
| Crystalloids | Cost-effective | Large volumes needed | Standard therapy |
| Colloids | Volume expansion | Renal toxicity risk | Avoid routinely |
- Evidence-Based Nutrition Protocol
- Mild pancreatitis: Oral feeding within 24 hours
- Start with clear liquids if tolerated
- Advance to low-fat diet within 48 hours
- Success rate >90% without complications
- Moderate-severe disease: Enteral nutrition within 48 hours
- Nasojejunal feeding preferred over nasogastric
- Elemental formulas for severe cases
- Reduces infection risk by 50%
- Mild pancreatitis: Oral feeding within 24 hours
💡 Master This: Early enteral feeding (<48 hours) maintains gut barrier function and reduces bacterial translocation by 60%. This prevents the "second hit" phenomenon where gut-derived endotoxins worsen systemic inflammation, explaining why early feeding reduces mortality from 15% to 8% in severe cases.
Pain management requires specific protocols that avoid medications that worsen pancreatic inflammation:
- Analgesic Hierarchy
- First-line: Acetaminophen + Ketorolac (if no contraindications)
- Second-line: Tramadol or Hydromorphone
- Severe pain: Fentanyl or Hydromorphone PCA
- Avoid: Morphine (increases sphincter of Oddi pressure)
Complication management follows specific intervention thresholds and timing protocols:
- Infected Necrosis Management
- Diagnosis: CT-guided aspiration if fever + leukocytosis >7 days
- Treatment: Antibiotics + delayed intervention (>4 weeks)
- Approach: Step-up strategy - drainage → necrosectomy
- Success rate: 85% with minimally invasive approach
Organ support protocols target specific dysfunction patterns with evidence-based interventions:
- Respiratory failure: Lung-protective ventilation (6 mL/kg tidal volume)
- Renal dysfunction: Continuous renal replacement therapy for fluid overload
- Cardiovascular collapse: Norepinephrine first-line vasopressor
- Coagulopathy: Fresh frozen plasma for active bleeding only
These algorithms transform pancreatitis management from supportive care to precision medicine, targeting specific pathophysiological mechanisms with measurable outcome improvements.
⚖️ Treatment Algorithms: Evidence-Based Crisis Management
🌐 Multi-System Integration: The Inflammatory Network
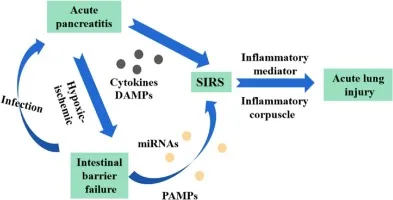
📌 Remember: SIRS-CARS describes the inflammatory balance - Systemic Inflammatory Response Syndrome followed by Compensatory Anti-inflammatory Response Syndrome. In severe pancreatitis, dysregulated SIRS affects >80% of patients, while excessive CARS increases infection risk 5-fold.
The cardiovascular-pancreatic axis demonstrates the most immediate and life-threatening interactions:
- Cardiovascular Cascade Effects
- Capillary leak syndrome: 4-6 liters third-space losses
- Hypovolemic shock in 40% of severe cases
- Cardiac output decreases 30-50% without resuscitation
- Vasodilation: Systemic vascular resistance drops 40%
- Distributive shock component develops
- Vasopressor requirements in 25% of severe cases
- Myocardial depression: Direct cytokine effects
- Ejection fraction decreases 15-25%
- Troponin elevation in 30% without coronary disease
- Capillary leak syndrome: 4-6 liters third-space losses
⭐ Clinical Pearl: Hemoconcentration (hematocrit >47% in men, >44% in women) within 24 hours predicts severe disease with 85% accuracy. This reflects massive capillary leak and inadequate fluid resuscitation, making it a critical early warning sign for impending complications.
Pulmonary-pancreatic interactions create respiratory complications in 60% of severe cases through multiple mechanisms:
| Mechanism | Pathophysiology | Clinical Manifestation | Incidence |
|---|---|---|---|
| ARDS | Cytokine-mediated lung injury | PaO2/FiO2 <300 | 20% severe cases |
| Pleural Effusion | Capillary leak + inflammation | Left-sided predominant | 40% severe cases |
| Atelectasis | Pain-limited breathing | Bibasilar changes | 60% all cases |
| Pneumonia | Immunosuppression | VAP in ventilated patients | 25% ICU cases |
| Fat Embolism | Pancreatic lipase effects | Rare but fatal | <5% severe cases |
Renal-pancreatic syndrome affects 30% of severe cases through combined mechanisms:
- Acute Kidney Injury Pathways
- Pre-renal: Hypovolemia and hypotension (60% of cases)
- Aggressive fluid resuscitation prevents progression
- Urine output <0.5 mL/kg/hour early warning sign
- Intrinsic renal: Direct cytokine injury (25% of cases)
- Acute tubular necrosis from inflammatory mediators
- Requires renal replacement therapy in 15%
- Post-renal: Rare but abdominal compartment syndrome
- Intra-abdominal pressure >20 mmHg
- Oliguria despite adequate volume status
- Pre-renal: Hypovolemia and hypotension (60% of cases)
Hepatic dysfunction occurs through shared blood supply and inflammatory mediator effects:
- Liver Function Alterations
- Transaminase elevation: ALT/AST 2-5x normal in 50%
- Cholestasis: Bilirubin >3 mg/dL in 25% of severe cases
- Synthetic dysfunction: Albumin <3 g/dL, prolonged PT/INR
- Metabolic acidosis: Lactate >4 mmol/L indicates poor perfusion
Endocrine-metabolic disruption creates long-term complications that persist beyond acute resolution:
-
Glucose homeostasis: Hyperglycemia >200 mg/dL in 70%
- Stress response and islet cell dysfunction
- Insulin requirements increase 3-5 fold
- Diabetes mellitus develops in 15% of severe cases
-
Calcium metabolism: Hypocalcemia <8 mg/dL in 40%
- Fat saponification and PTH resistance
- Tetany and cardiac arrhythmias possible
- Correlates with disease severity
Understanding these multi-system interactions enables proactive monitoring and early intervention, preventing the cascade progression that transforms manageable inflammation into life-threatening organ failure.
🌐 Multi-System Integration: The Inflammatory Network
🎯 Clinical Mastery Arsenal: Rapid Assessment & Decision Tools
📌 Remember: PANCREAS rapid assessment - Pain severity (0-10 scale), Amylase/lipase levels, Nausea/vomiting frequency, Comorbidities present, Risk factors identified, Etiology suspected, Associated symptoms, Severity scoring. This 7-step protocol enables complete evaluation in <15 minutes.
Essential Clinical Arsenal for immediate bedside assessment:
- Rapid Severity Stratification Tools
- BISAP Score (0-5 points, 24-hour assessment)
- BUN >25 mg/dL (1 point)
- Impaired mental status (1 point)
- SIRS criteria (1 point)
- Age >60 years (1 point)
- Pleural effusion (1 point)
- Score ≥3 = severe disease (mortality >15%)
- BISAP Score (0-5 points, 24-hour assessment)
⭐ Clinical Pearl: BISAP score ≥3 within 24 hours predicts severe pancreatitis with 85% sensitivity and 75% specificity. Unlike Ranson criteria, BISAP can be calculated immediately and repeated to track disease progression, making it the preferred bedside tool.
| Score | Mortality Risk | ICU Need | Length of Stay | Complications |
|---|---|---|---|---|
| 0-1 | <1% | 5% | 3-5 days | Rare |
| 2 | 2-5% | 15% | 5-7 days | 10% |
| 3 | 10-15% | 50% | 10-14 days | 35% |
| 4-5 | 20-30% | 85% | 21+ days | 60% |
- "Red Flag" Laboratory Values
- Lipase >1000 U/L: Severe disease likely (80% correlation)
- BUN >20 mg/dL: Fluid resuscitation inadequate
- Creatinine >1.8 mg/dL: Renal dysfunction developing
- Hematocrit >47% (men) or >44% (women): Hemoconcentration
- Calcium <8 mg/dL: Severe disease marker
- LDH >350 U/L: Tissue necrosis indicator
💡 Master This: BUN elevation reflects both dehydration and tissue catabolism in pancreatitis. BUN >25 mg/dL at 48 hours despite adequate fluid resuscitation indicates severe disease with >90% accuracy, making it the single best laboratory predictor of complications.
Imaging Decision Matrix for optimal resource utilization:
- CT Imaging Indications (Evidence-Based Criteria)
- Diagnostic uncertainty after clinical + laboratory assessment
- BISAP score ≥2 or clinical deterioration
- Fever >38.5°C after 48 hours
- Leukocytosis >15,000 without obvious source
- Persistent organ dysfunction beyond 48 hours
- Failed clinical improvement by 72 hours
Treatment Decision Algorithms for immediate implementation:
Complication Recognition Patterns for early intervention:
-
Infection Warning Signs (>7 days post-onset)
- Fever >38.5°C + leukocytosis >12,000
- New organ dysfunction or clinical deterioration
- Positive blood cultures or CT evidence
- Action: CT-guided aspiration + antibiotic therapy
-
Fluid Collection Management
- <4 weeks: Conservative management unless infected
- >4 weeks + symptomatic: Intervention indicated
- Approach: Step-up strategy (drainage → necrosectomy)
Discharge Readiness Criteria for safe transitions:
- Clinical Stability Markers
- Pain controlled with oral medications
- Tolerating regular diet for >24 hours
- Afebrile >24 hours without antibiotics
- Normal or improving laboratory values
- Adequate social support and follow-up arranged
This clinical mastery arsenal transforms complex decision-making into systematic protocols, enabling consistent excellent outcomes regardless of experience level or clinical setting.
🎯 Clinical Mastery Arsenal: Rapid Assessment & Decision Tools
Practice Questions: Pancreatitis
Test your understanding with these related questions
A 55-year-old man is brought to the emergency room by his roommate due to an abdominal pain that started 2 hours ago. His pain is dull, aching, and radiates to the back. He admits to binge drinking alcohol for the past 2 days. Past medical history is significant for multiple admissions to the hospital for similar abdominal pain events, hypertension, and hyperlipidemia. He takes chlorthalidone and atorvastatin. He admits to heavy alcohol consumption over the past 10 years. He has smoked a pack of cigarettes a day for the last 20 years. In the emergency department, his temperature is 38.9℃ (102.0℉), pulse rate is 100/min, and respiratory rate is 28/min. On physical examination, he looks generally unwell and diaphoretic. Auscultation of his heart and lungs reveals an elevated heart rate with a regular rhythm. His lungs are clear to auscultation bilaterally. His abdomen is tympanitic with generalized tenderness. Evaluation of lab values reveals a leukocyte count of 28,000/mm3 with 89% of neutrophils. His amylase level is 255 U/L. A CT scan of the abdomen shows the diffuse enlargement of the pancreas. Which pathological process is most likely occurring in this patient’s peripancreatic tissue?










