Secondary glomerular diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Secondary glomerular diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Secondary glomerular diseases US Medical PG Question 1: A 62-year-old woman with type 2 diabetes mellitus comes to the physician because of a 3-month history of fatigue and weakness. Her hemoglobin A1c concentration was 13.5% 12 weeks ago. Her blood pressure is 152/92 mm Hg. Examination shows lower extremity edema. Serum studies show:
K+ 5.1 mEq/L
Phosphorus 5.0 mg/dL
Ca2+ 7.8 mg/dL
Urea nitrogen 60 mg/dL
Creatinine 2.2 mg/dL
Which of the following is the best parameter for early detection of this patient’s renal condition?
- A. Serum total protein
- B. Serum creatinine
- C. Urinary red blood cell casts
- D. Serum urea nitrogen
- E. Urinary albumin (Correct Answer)
Secondary glomerular diseases Explanation: ***Urinary albumin***
- **Microalbuminuria** is often the earliest detectable sign of **diabetic nephropathy**, occurring before changes in GFR or serum creatinine become apparent.
- Regular screening for urinary albumin in diabetic patients allows for early intervention to slow the progression of **renal damage**.
*Serum total protein*
- **Hypoalbuminemia** can be seen in advanced renal disease due to significant proteinuria, but it is not an early marker.
- Other conditions like **liver disease** or **malnutrition** can also cause altered serum total protein, making it less specific for early renal damage.
*Serum creatinine*
- **Serum creatinine** levels rise significantly only after a substantial portion of kidney function (around 50%) has been lost.
- Therefore, it is a marker of established renal dysfunction rather than an early indicator.
*Urinary red blood cell casts*
- The presence of **red blood cell casts** in urine indicates **glomerulonephritis** or other inflammatory conditions affecting the glomeruli.
- While concerning, it is not the typical or earliest presentation of **diabetic nephropathy**, which primarily involves proteinuria.
*Serum urea nitrogen*
- **Blood urea nitrogen (BUN)** levels, like creatinine, increase with declining kidney function and are used to assess the severity of **renal impairment**.
- However, BUN levels can also be influenced by factors like **hydration status** and **protein intake**, and they are not an early marker of nascent renal disease.
Secondary glomerular diseases US Medical PG Question 2: A 50-year-old woman comes to the emergency department because of fever and productive cough with blood in the sputum for 1 day. She also reports a sharp pain under her ribs that is worsened on taking deep breaths. Over the past 2 years, she has had repeated episodes of sinusitis, for which she used over the counter medication. She has recently started a new job at a wire-mesh factory. Her temperature is 38.3°C (100.9 °F), pulse is 72/min, respirations are 16/min, and blood pressure is 120/80 mm Hg. Physical examination shows palpable nonblanching skin lesions over her hands and feet. Examination of the nasal cavity shows ulcerations of the nasopharyngeal mucosa and a small septal perforation. Pulmonary examination shows stridor on inspiration. Laboratory studies show:
Hemoglobin 13.2 g/dL
Leukocyte count 10,300/mm3
Platelet count 205,000/mm3
Serum
Urea nitrogen 24 mg/dL
Creatinine 2.4 mg/dL
Urine
Protein 2+
RBC 70/hpf
RBC casts numerous
WBC 1–2/hpf
A chest x-ray shows multiple cavitating, nodular lesions bilaterally. Which of the following additional findings is most likely to be present in this patient?
- A. Increased p-ANCA titers
- B. Increased anti-Smith titers
- C. Increased anti-GBM titers
- D. Increased c-ANCA titers (Correct Answer)
- E. Decreased ADAMTS13 activity
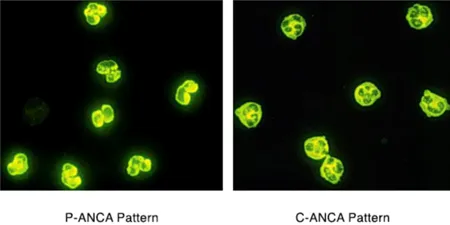
Secondary glomerular diseases Explanation: ### ***Increased c-ANCA titers***
- The patient's presentation with **sinusitis**, **nasal ulcerations**, **pulmonary cavitating nodules** with hemoptysis, and **rapidly progressive glomerulonephritis** (elevated creatinine, proteinuria, RBC casts) is highly indicative of **Granulomatosis with Polyangiitis (GPA)**.
- **c-ANCA (cytoplasmic antineutrophil cytoplasmic antibodies)**, primarily targeting **proteinase 3 (PR3)**, are serological markers commonly elevated in GPA and help confirm the diagnosis.
### *Increased p-ANCA titers*
- **p-ANCA (perinuclear antineutrophil cytoplasmic antibodies)**, typically targeting **myeloperoxidase (MPO)**, are more commonly associated with **microscopic polyangiitis** or **eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)**.
- While both GPA and microscopic polyangiitis can present with kidney and lung involvement, the prominent upper airway disease (sinusitis, nasal ulcerations, septal perforation) in this patient points more strongly towards GPA and c-ANCA positivity.
### *Increased anti-Smith titers*
- **Anti-Smith antibodies** are highly specific for **Systemic Lupus Erythematosus (SLE)**.
- The clinical presentation of **upper airway destruction**, **cavitating lung lesions**, and **glomerulonephritis with RBC casts** is not typical for SLE, which more commonly presents with malar rash, arthritis, serositis, and other systemic symptoms.
### *Increased anti-GBM titers*
- **Anti-GBM (anti-glomerular basement membrane) antibodies** are characteristic of **Goodpasture syndrome**, which causes a **rapidly progressive glomerulonephritis** and often **pulmonary hemorrhage**.
- However, Goodpasture syndrome does not typically involve **upper airway disease** (sinusitis, nasal ulcerations, septal perforation) or **palpable skin lesions**, which are prominent features in this patient.
### *Decreased ADAMTS13 activity*
- **Decreased ADAMTS13 activity** is diagnostic of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is characterized by the pentad of **thrombocytopenia**, **microangiopathic hemolytic anemia**, **neurological symptoms**, **renal insufficiency**, and **fever**, but it does not involve the prominent **destructive upper airway disease** or **cavitating lung lesions** seen in this patient.
Secondary glomerular diseases US Medical PG Question 3: A 70-year-old man with a long-standing history of diabetes mellitus type 2 and hypertension presents with complaints of constant wrist and shoulder pain. Currently, the patient undergoes hemodialysis 2 to 3 times a week and is on the transplant list for a kidney. The patient denies any recent traumas. Which of the following proteins is likely to be increased in his plasma, causing the patient’s late complaints?
- A. Amyloid precursor protein
- B. Amyloid A (AA)
- C. β2-microglobulin (Correct Answer)
- D. Transthyretin (TTR)
- E. Ig light chains
Secondary glomerular diseases Explanation: **β2-microglobulin**
- The patient's presentation with **chronic wrist and shoulder pain**, particularly in the setting of **long-term hemodialysis for end-stage renal disease (ESRD)**, is highly suggestive of **dialysis-related amyloidosis (DRA)**.
- **β2-microglobulin** is a small protein that is normally filtered by the kidneys. In ESRD patients on hemodialysis, it accumulates and forms amyloid deposits, primarily in joint capsules, synovium, and bones.
*Amyloid precursor protein*
- **Amyloid precursor protein (APP)** is primarily associated with **Alzheimer's disease**, where its proteolytic cleavage leads to the formation of amyloid-beta plaques in the brain.
- It is not directly implicated in joint pain or musculoskeletal amyloidosis in the context of renal failure.
*Amyloid A (AA)*
- **Amyloid A (AA)** is the protein responsible for **secondary (reactive) amyloidosis**, which is typically associated with chronic inflammatory conditions like rheumatoid arthritis or chronic infections.
- While the patient has some chronic conditions (diabetes, hypertension), his joint pain is more characteristic of dialysis-related amyloidosis, not systemic inflammation-induced AA amyloidosis.
*Transthyretin (TTR)*
- **Transthyretin (TTR)** is associated with **familial amyloid polyneuropathy** and **senile systemic amyloidosis (SSA)**, causing heart failure or carpal tunnel syndrome, but it is not directly linked to dialysis-related amyloidosis.
- The patient's symptoms are more indicative of the specific type of amyloidosis seen in ESRD.
*Ig light chains*
- **Immunoglobulin (Ig) light chains** are involved in **primary (AL) amyloidosis**, which is caused by a plasma cell dyscrasia.
- While AL amyloidosis can affect various organs, including joints, the patient's history of ESRD and hemodialysis makes **β2-microglobulin amyloidosis** the most specific and likely cause of his musculoskeletal symptoms.
Secondary glomerular diseases US Medical PG Question 4: A 6-year-old boy presents to your office with hematuria. Two weeks ago the patient had symptoms of a sore throat and fever. Although physical exam is unremarkable, laboratory results show a decreased serum C3 level and an elevated anti-DNAse B titer. Which of the following would you most expect to see on renal biopsy?
- A. Immune complex deposits with a "spike and dome" appearance on electron microscopy
- B. Large, hypercellular glomeruli on light microscopy (Correct Answer)
- C. Wirelooping and hyaline thrombi on light microscopy
- D. Polyclonal IgA deposition on immunofluorescence
- E. Antibodies to GBM resulting in a linear immunofluorescence pattern
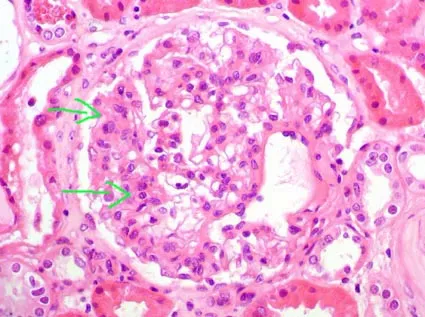
Secondary glomerular diseases Explanation: ***Large, hypercellular glomeruli on light microscopy***
- The clinical presentation, including recent **sore throat**, **hematuria**, decreased **C3**, and elevated **anti-DNAse B titer**, is highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- On light microscopy, PSGN characteristically shows **diffuse proliferative glomerulonephritis** with **enlarged, hypercellular glomeruli** due to inflammatory cell infiltration and proliferation of intrinsic glomerular cells.
*Immune complex deposits with a "spike and dome" appearance on electron microscopy*
- This "spike and dome" appearance refers to **subepithelial deposits** with new basement membrane formation, which is characteristic of **membranous nephropathy**, not PSGN.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults, which is different from the child's presentation here.
*Wirelooping and hyaline thrombi on light microscopy*
- These features, particularly **"wire-loop" lesions** and **hyaline thrombi**, suggest severe **lupus nephritis**, a manifestation of **systemic lupus erythematosus**.
- Lupus nephritis often presents with a range of kidney pathologies and systemic symptoms not seen in this patient.
*Polyclonal IgA deposition on immunofluorescence*
- **IgA deposition** in the mesangium is the hallmark of **IgA nephropathy (Berger's disease)**, which typically presents with recurrent hematuria, often after an upper respiratory infection.
- While there is hematuria and a recent infection, the decreased C3 and elevated anti-DNAse B titer point away from IgA nephropathy.
*Antibodies to GBM resulting in a linear immunofluorescence pattern*
- A **linear pattern** of IgG deposits along the glomerular basement membrane (GBM) is characteristic of **Goodpasture syndrome (anti-GBM disease)**.
- This condition involves antibodies specifically targeting the GBM and often presents with rapidly progressive glomerulonephritis and pulmonary hemorrhage, which are not described here.
Secondary glomerular diseases US Medical PG Question 5: A 40-year-old woman comes to the emergency department because of difficulty walking for the past 4 hours. She first noticed her symptoms after getting up this morning and her foot dragging while walking. She feels tired. She has a history of chronic sinusitis. Six months ago, she was diagnosed with asthma. Current medications include an albuterol inhaler and inhaled corticosteroids. Her temperature is 38.9°C (102°F), pulse is 80/min, and her blood pressure is 140/90 mm Hg. Auscultation of her lungs shows diffuse wheezing over bilateral lung fields. Physical examination shows tender subcutaneous nodules on the extensor surfaces of the elbows. There are palpable, non-blanching erythematous lesions on both shins. Dorsiflexion of the right foot is impaired. Sensation to pinprick, light touch, and vibration is decreased over the ulnar aspect of the left forearm. Laboratory studies show:
Hemoglobin 11.3 g/dL
Leukocyte count 24,500
Segmented neutrophils 48%
Eosinophils 29%
Lymphocytes 19%
Monocytes 4%
Platelet count 290,000/mm3
Serum
Urea nitrogen 32 mg/dL
Creatinine 1.85 mg/dL
Urine
Blood 2+
Protein 3+
Which of the following is the most likely diagnosis in this patient?
- A. Granulomatosis with polyangiitis
- B. Excessive glucocorticoid use
- C. Goodpasture syndrome
- D. Henoch-Schönlein purpura
- E. Eosinophilic granulomatosis with polyangiitis (Correct Answer)
Secondary glomerular diseases Explanation: ***Eosinophilic granulomatosis with polyangiitis (EGPA)***
- This patient presents with a classic triad: **asthma**, **eosinophilia** (29%), and **multisystem vasculitis** as evidenced by mononeuropathy, skin lesions (nodules and palpable purpura), and kidney involvement.
- The history of chronic sinusitis, new-onset foot drop (mononeuropathy), **palpable purpura**, and elevated creatinine with proteinuria strongly point towards EGPA.
*Granulomatosis with polyangiitis (GPA)*
- While GPA can cause sinusitis, kidney disease, and neuropathy, it typically presents with **neutrophilic inflammation** and **c-ANCA** positivity, not prominent eosinophilia or severe asthma.
- Granulomatosis with polyangiitis typically involves the **upper and lower respiratory tracts** and kidneys but lacks the pronounced eosinophilia and severe asthma seen here.
*Excessive glucocorticoid use*
- This condition is associated with Cushingoid features, **osteoporosis**, and immunosuppression, none of which fully explain the patient's acute neurological deficits, eosinophilia, or vasculitic manifestations.
- Although the patient has asthma, her symptoms are not consistent with the side effects of inhaled corticosteroids or chronic systemic glucocorticoid use.
*Goodpasture syndrome*
- Goodpasture syndrome is characterized by **recurrent pulmonary hemorrhage** and rapidly progressive **glomerulonephritis** due to anti-GBM antibodies.
- It does not explain the prominent eosinophilia, asthma, or the presence of subcutaneous nodules and palpable purpura.
*Henoch-Schönlein purpura (HSP)*
- HSP typically presents in children with **palpable purpura** on the buttocks and lower extremities, **arthralgias**, abdominal pain, and **IgA nephropathy**.
- It does not involve significant eosinophilia, severe asthma, or mononeuropathy as seen in this adult patient.
Secondary glomerular diseases US Medical PG Question 6: A 21-year-old male presents to your office with hematuria 3 days after the onset of a productive cough and fever. Following renal biopsy, immunofluorescence shows granular IgA deposits in the glomerular mesangium. Which of the following do you suspect in this patient?
- A. Lipoid nephrosis
- B. Berger’s disease (Correct Answer)
- C. HIV infection
- D. Systemic lupus erythematosus
- E. Poststreptococcal glomerulonephritis
Secondary glomerular diseases Explanation: ***Berger’s disease***
- The presentation of **hematuria occurring 3 days after a respiratory infection** (productive cough and fever) is characteristic of **IgA nephropathy** or Berger's disease, showing a synpharyngitic pattern.
- **Immunofluorescence showing granular IgA deposits in the glomerular mesangium** is the histological hallmark of IgA nephropathy.
*Lipoid nephrosis*
- This condition is also known as **minimal change disease** and typically presents with **nephrotic syndrome** (heavy proteinuria, edema, hypoalbuminemia), not primarily hematuria.
- Renal biopsy would reveal **effacement of foot processes** on electron microscopy with normal light microscopy and negative immunofluorescence, unlike the IgA deposits described.
*HIV infection*
- HIV can lead to **HIV-associated nephropathy (HIVAN)**, which typically presents as **focal segmental glomerulosclerosis** (FSGS) and can include proteinuria and progressive renal failure.
- While hematuria can occur, the characteristic **IgA deposits in the mesangium** described are not typical for HIVAN.
*Systemic lupus erythematosus*
- **Lupus nephritis** is a common complication of SLE, and can present with hematuria, proteinuria, and various patterns of glomerulonephritis.
- However, immunofluorescence in lupus nephritis usually shows **IgG, IgM, IgA, C3, and C1q deposits** (full-house staining), not isolated IgA deposits.
*Poststreptococcal glomerulonephritis*
- This condition typically presents with **hematuria 10-14 days after a streptococcal infection** (post-infectious glomerulonephritis), a longer latency period than seen in this patient.
- Immunofluorescence would show unique **"lumpy-bumpy" granular deposits of C3 and IgG** along the glomerular basement membrane, often with characteristic subepithelial humps on electron microscopy, rather than mesangial IgA.
Secondary glomerular diseases US Medical PG Question 7: A 73-year-old man comes to the physician because of progressive fatigue and shortness of breath on exertion for 3 weeks. He has swelling of his legs. He has not had nausea or vomiting. His symptoms began shortly after he returned from a trip to Cambodia. He occasionally takes ibuprofen for chronic back pain. He has a history of arterial hypertension and osteoarthritis of both knees. He had an episode of pneumonia 4 months ago. His current medications include lisinopril and hydrochlorothiazide. He has no history of drinking or smoking. His temperature is 37°C (98.6°F), pulse is 101/min, and blood pressure is 135/76 mm Hg. Examination shows pitting edema of the upper and lower extremities. Laboratory studies show:
Hemoglobin 14.1 g/dL
Leukocyte count 6,800/mm3
Platelet count 216,000/mm3
Serum
Urea nitrogen 26 mg/dL
Creatinine 2.9 mg/dL
Albumin 1.6 g/dL
Urine
Blood negative
Protein 4+
Glucose negative
Renal biopsy with Congo red stain shows apple-green birefringence under polarized light. Further evaluation of this patient is most likely to show which of the following findings?
- A. Positive interferon-γ release assay
- B. Dilated bronchi on chest CT
- C. Elevated anti-citrullinated peptide antibodies
- D. Positive HLA-B27 test
- E. Rouleaux formation on peripheral smear (Correct Answer)
Secondary glomerular diseases Explanation: ***Rouleaux formation on peripheral smear***
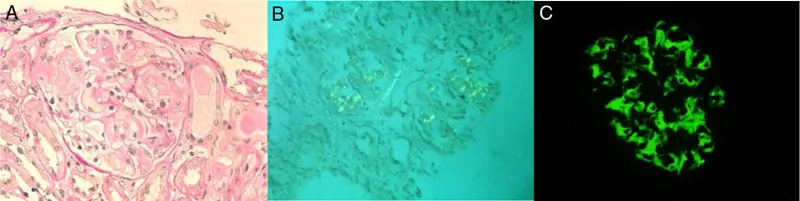
- The renal biopsy showing **apple-green birefringence** with Congo red stain is pathognomonic for **amyloidosis**.
- The clinical presentation of **nephrotic syndrome** (massive proteinuria, hypoalbuminemia, edema) with renal amyloidosis in an elderly patient is most commonly due to **AL (light chain) amyloidosis** caused by plasma cell dyscrasia.
- AL amyloidosis is associated with **monoclonal gammopathy** which causes increased serum protein viscosity, leading to **rouleaux formation** (stacking of RBCs like coins) on peripheral blood smear.
- Further workup would typically show serum/urine protein electrophoresis with monoclonal protein and possibly bone marrow plasmacytosis.
*Positive interferon-γ release assay*
- This test diagnoses **latent or active tuberculosis**.
- While TB can cause **AA (secondary) amyloidosis** through chronic inflammation, and the patient traveled to an endemic area, the renal-limited presentation without active systemic infection makes AL amyloidosis more likely.
- AA amyloidosis typically presents with chronic inflammatory conditions lasting months to years.
*Dilated bronchi on chest CT*
- **Bronchiectasis** causes chronic inflammation and can lead to **AA amyloidosis**.
- However, a single episode of pneumonia 4 months ago is insufficient to cause the chronic inflammation needed for AA amyloidosis.
- This finding would not directly relate to the amyloid deposition causing current symptoms.
*Elevated anti-citrullinated peptide antibodies*
- These antibodies are highly specific for **rheumatoid arthritis**, which can cause AA amyloidosis.
- However, the patient has **osteoarthritis** (degenerative joint disease), not inflammatory arthritis.
- There are no clinical features suggesting RA (no joint inflammation, no morning stiffness).
*Positive HLA-B27 test*
- **HLA-B27** is associated with **seronegative spondyloarthropathies** which can rarely cause AA amyloidosis.
- The patient's back pain is attributed to chronic mechanical issues, not inflammatory spondyloarthropathy.
- This finding is unrelated to the renal amyloidosis presentation.
Secondary glomerular diseases US Medical PG Question 8: A 51-year-old African American man presents to his primary care physician’s office for an annual visit. He has no major concerns and says that he has been healthy for the last year. His past medical history is significant for diabetes as well as long standing hypertension that has developed gradually since his 30's; however, he has refused to take any medications. Physical exam shows no abnormal findings. Routine laboratory testing reveals the following:
Serum creatinine concentration: 1.5 mg/dL
Blood urea nitrogen: 31 mg/dL
Based on these results, urine studies are conducted that reveal mild proteinuria of less than 1 g/day and no casts.
Which of the following is most likely associated with the cause of this patient's elevated creatinine?
- A. String of beads on angiography
- B. Kimmelstiel-Wilson lesions (Correct Answer)
- C. Apple-green birefringent lesions
- D. Renal cortex necrosis
- E. Flea-bitten kidney
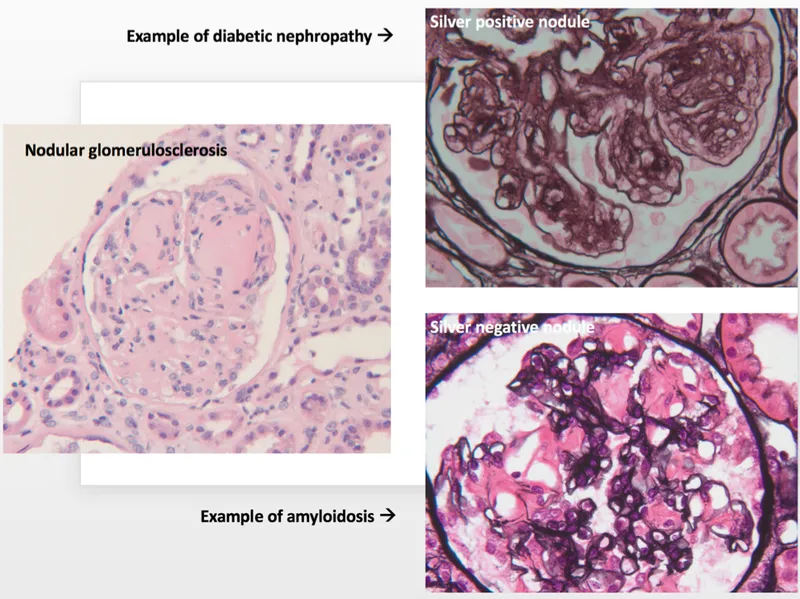
Secondary glomerular diseases Explanation: **Kimmelstiel-Wilson lesions**
- The patient has a history of long-standing diabetes and hypertension, which are the primary risk factors for **diabetic nephropathy**.
- **Kimmelstiel-Wilson lesions** are nodular glomerulosclerosis pathognomonic for **diabetic nephropathy**, characterized by hyaline nodules in the mesangium.
- This is the most likely cause given the combination of diabetes, mild proteinuria (<1 g/day), and chronic renal insufficiency.
*String of beads on angiography*
- This finding is characteristic of **fibromuscular dysplasia**, a non-inflammatory vascular disease that can cause **renal artery stenosis**.
- While renal artery stenosis can cause hypertension and renal impairment, the patient's long-standing diabetes and gradual progression make diabetic nephropathy a more probable cause.
*Apple-green birefringent lesions*
- This describes the characteristic staining of **amyloid deposits** with **Congo red stain** under polarized light.
- While amyloidosis can cause renal failure with proteinuria, it is less common than diabetic nephropathy in a patient with long-standing diabetes and the typical presentation described.
*Renal cortex necrosis*
- This is a rare and severe form of **acute kidney injury** often associated with conditions like severe sepsis, obstetric complications, or disseminated intravascular coagulation.
- The patient's history of gradual onset hypertension and diabetes, along with mild proteinuria and elevated creatinine, points to a chronic rather than acute process.
*Flea-bitten kidney*
- This describes the gross appearance of kidneys in **malignant hypertension**, showing petechial hemorrhages on the renal surface.
- While the patient has long-standing hypertension, the presentation suggests chronic kidney disease from diabetic nephropathy rather than acute malignant hypertension, which would present with markedly elevated blood pressure and acute kidney injury.
Secondary glomerular diseases US Medical PG Question 9: A 43-year-old man is referred by his family physician because his urine dipstick reveals 3+ protein and urinalysis reveals 1-2 red cells/high power field, but is otherwise negative. He does not have any current complaints. His family history is irrelevant. He denies smoking and alcohol use. His temperature is 36.7°C (98.06°F), blood pressure is 130/82 mm Hg, and pulse is 78/min. Physical examination is unremarkable. Which of the following is the best next step in the management of this patient’s condition?
- A. Reassurance
- B. Repeat the urine dipstick test
- C. 24-hour urine collection (Correct Answer)
- D. Start captopril
- E. Urine culture
Secondary glomerular diseases Explanation: ***24-hour urine collection***
- The presence of **3+ proteinuria on dipstick** (approximately ≥300 mg/dL) is significant and requires **quantification** to assess the degree of proteinuria and guide further management.
- A **24-hour urine collection** is the traditional gold standard method to quantify total protein excretion and determine if the patient has clinically significant proteinuria (>150 mg/day is abnormal; >3.5 g/day indicates nephrotic-range proteinuria).
- Alternatively, a **spot urine protein-to-creatinine ratio (PCR)** or **albumin-to-creatinine ratio (ACR)** can be used, but among the given options, 24-hour collection is the appropriate next step.
- The concurrent finding of **microscopic hematuria (1-2 RBCs/hpf)** further supports the need for evaluation of possible **glomerular disease** or other renal pathology.
*Repeat the urine dipstick test*
- Repeating a dipstick is appropriate for **trace or 1+ proteinuria** to rule out transient causes (exercise, fever, orthostatic proteinuria, concentrated urine).
- However, **3+ proteinuria is too significant** to simply repeat the dipstick; it requires quantification to determine the severity and guide further diagnostic workup (e.g., renal biopsy if nephrotic-range).
*Urine culture*
- While infection can cause proteinuria and hematuria, the urinalysis is described as "otherwise negative," suggesting an absence of **leukocytes, nitrites, or bacteria** typical of a urinary tract infection.
- The patient is **asymptomatic** without dysuria, frequency, or fever, making infection unlikely.
- A urine culture would be appropriate if there were clinical signs of UTI.
*Reassurance*
- Giving reassurance would be **inappropriate and potentially harmful** given the finding of **3+ proteinuria**, which is a significant indicator of potential renal pathology.
- Proteinuria of this magnitude can indicate **glomerulonephritis, diabetic nephropathy, hypertensive nephrosclerosis**, or other kidney diseases requiring further evaluation.
- The presence of concurrent **microscopic hematuria** raises additional concern for glomerular disease.
*Start captopril*
- Captopril, an **ACE inhibitor**, is used to reduce proteinuria and provide renoprotection in patients with **confirmed chronic kidney disease**, particularly in the setting of **diabetes or hypertension**.
- Initiating treatment is **premature** without first quantifying the proteinuria, establishing a diagnosis, and ruling out secondary causes.
- The patient's blood pressure (130/82 mm Hg) is at the upper limit of normal but does not mandate immediate antihypertensive therapy before completing the diagnostic evaluation.
Secondary glomerular diseases US Medical PG Question 10: A 76-year-old woman presents to the office with a generalized weakness for the past month. She has a past medical history significant for uncontrolled hypertension and type 2 diabetes mellitus. Her temperature is 37.0°C (98.6°F), blood pressure is 135/82 mm Hg, pulse is 90/min, respiratory rate is 17/min, and oxygen saturation is 99% on room air. Physical exam shows no remarkable findings. Her last recorded glomerular filtration rate was 30 mL/min. A radiograph of the patient’s hand is given. Which of the following lab findings is most likely to be found in this patient?
- A. Increased PTH, decreased calcium, increased phosphate (Correct Answer)
- B. Increased PTH, decreased calcium, decreased phosphate
- C. Normal PTH, increased calcium, normal phosphate
- D. Increased PTH, increased calcium, decreased phosphate
- E. Increased PTH, increased calcium, increased phosphate
Secondary glomerular diseases Explanation: ***Increased PTH, decreased calcium, increased phosphate***
- The patient's **glomerular filtration rate (GFR) of 30 mL/min** indicates **Stage 4 chronic kidney disease (CKD)**. In CKD, the kidneys are unable to adequately excrete phosphate, leading to **hyperphosphatemia**.
- Hyperphosphatemia leads to the formation of calcium-phosphate complexes, causing a decrease in free calcium (hypocalcemia) by precipitating out. Additionally, damaged kidneys cannot convert vitamin D into its active form, which further reduces calcium absorption from the gut and bone, contributing to hypocalcemia. This persistent hypocalcemia stimulates the parathyroid glands to produce more **parathyroid hormone (PTH)**, resulting in **secondary hyperparathyroidism**.
*Increased PTH, decreased calcium, decreased phosphate*
- This pattern of laboratory findings is characteristic of **primary hyperparathyroidism**, where an adenoma or hyperplasia of the parathyroid glands leads to excessive PTH production.
- In primary hyperparathyroidism, elevated PTH causes increased bone resorption and renal phosphate excretion, typically resulting in **hypercalcemia** and **hypophosphatemia**.
*Normal PTH, increased calcium, normal phosphate*
- This combination is not typically seen in CKD-related mineral and bone disorder.
- While hypercalcemia can occur in some conditions, normal PTH with increased calcium often points toward conditions like **paraneoplastic syndromes** or **granulomatous diseases** producing PTH-related protein, or **vitamin D intoxication**.
*Increased PTH, increased calcium, decreased phosphate*
- This specific combination (high PTH, high calcium, low phosphate) is the classic hallmark of **primary hyperparathyroidism**.
- In contrast, secondary hyperparathyroidism due to CKD typically presents with **hypocalcemia** and **hyperphosphatemia** due to impaired renal function.
*Increased PTH, increased calcium, increased phosphate*
- This pattern is highly unusual and not characteristic of any common parathyroid or kidney disorder.
- While both PTH and phosphate can be increased in certain advanced stages of CKD, calcium levels are typically low or normal, not elevated in secondary hyperparathyroidism.
More Secondary glomerular diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.