Renal replacement therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal replacement therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Renal replacement therapy US Medical PG Question 1: A 23-year-old man comes to his primary care provider after having severe abdominal cramping and diarrhea beginning the previous night. He denies any fevers or vomiting. Of note, he reports that he works in a nursing home and that several residents of the nursing home exhibited similar symptoms this morning. On exam, his temperature is 99.7°F (37.6°C), blood pressure is 116/80 mmHg, pulse is 88/min, and respirations are 13/min. His stool is cultured on blood agar and it is notable for a double zone of hemolysis. Which of the following organisms is the most likely cause?
- A. Clostridium difficile
- B. Listeria monocytogenes
- C. Clostridium perfringens (Correct Answer)
- D. Enterococcus faecalis
- E. Streptococcus pneumoniae
Renal replacement therapy Explanation: ***Clostridium perfringens***
- The patient's symptoms of **abdominal cramping** and **diarrhea** without fever or vomiting, along with the rapid onset and the presence of similar symptoms in others at the nursing home, are classic for **food poisoning** caused by *Clostridium perfringens*.
- The **double zone of hemolysis** on blood agar is a characteristic laboratory finding for this bacterium, produced by its alpha-toxin and theta-toxin.
*Clostridium difficile*
- This organism primarily causes **pseudomembranous colitis** and is typically associated with **antibiotic use** or in hospitalized patients, causing severe watery diarrhea, often with fever.
- It does not typically present with the acute, self-limiting food poisoning symptoms described, and its detection usually involves toxin assays, not characteristic hemolytic patterns on blood agar.
*Listeria monocytogenes*
- *Listeria monocytogenes* is associated with **meningitis** in immunocompromised individuals, pregnant women, and neonates, and can cause mild gastroenteritis, but less commonly epidemic outbreaks of diarrhea in this setting.
- It does not produce a double zone of hemolysis on blood agar.
*Enterococcus faecalis*
- *Enterococcus faecalis* is a common cause of **urinary tract infections** and endocarditis, and can occasionally be associated with diarrheal diseases, but it is not typically associated with food poisoning outbreaks of this nature.
- It does not produce a double zone of hemolysis on blood agar.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a common cause of **pneumonia**, otitis media, and meningitis, and is not associated with gastrointestinal symptoms like diarrhea or food poisoning.
- It typically exhibits alpha-hemolysis on blood agar (partial hemolysis), not a double zone of hemolysis.
Renal replacement therapy US Medical PG Question 2: A 19-year-old man presents to the emergency department after a motor vehicle accident. The patient reports left shoulder pain that worsens with deep inspiration. Medical history is significant for a recent diagnosis of infectious mononucleosis. His temperature is 99°F (37.2°C), blood pressure is 80/55 mmHg, pulse is 115/min, and respiratory rate is 22/min. On physical exam, there is abdominal guarding, abdominal tenderness in the left upper quadrant, and rebound tenderness. The patient’s mucous membranes are dry and skin turgor is reduced. Which of the following most likely represents the acute changes in renal plasma flow (RPF) and glomerular filtration rate (GFR) in this patient?
- A. No change in RPF and decreased GFR
- B. Decreased RPF and decreased GFR (Correct Answer)
- C. No change in RPF and increased GFR
- D. Decreased RPF and no change in GFR
- E. No change in RPF and GFR
Renal replacement therapy Explanation: ***Decreased RPF and decreased GFR***
- This patient presents with signs of **hypovolemic shock** (hypotension with BP 80/55 mmHg, tachycardia, dry mucous membranes, reduced skin turgor) likely due to **splenic rupture** from the motor vehicle accident, exacerbated by splenomegaly from **infectious mononucleosis**.
- With a blood pressure of 80/55 mmHg (MAP ~73 mmHg), the patient is at or below the **lower limit of renal autoregulation** (~80 mmHg MAP).
- In acute hypovolemic shock, **renal blood flow and RPF decrease** due to systemic hypotension and **sympathetic vasoconstriction**.
- Although **angiotensin II-mediated efferent arteriolar constriction** attempts to preserve GFR by maintaining glomerular capillary pressure, this compensation is **insufficient** when MAP falls below the autoregulatory range.
- Result: **Both RPF and GFR decrease**, though GFR may be relatively preserved compared to the magnitude of RPF decrease initially.
*No change in RPF and decreased GFR*
- This scenario would suggest decreased filtration despite normal renal perfusion, implying a primary glomerular barrier problem.
- In hypovolemic shock, **RPF is always decreased** due to reduced systemic blood flow and renal vasoconstriction.
*Decreased RPF and no change in GFR*
- While renal autoregulation attempts to maintain stable GFR despite changes in blood pressure, this mechanism works only within the **autoregulatory range (MAP 80-180 mmHg)**.
- At BP 80/55 mmHg, autoregulation is overwhelmed, and **GFR will decrease** along with RPF.
*No change in RPF and increased GFR*
- An **increased GFR** is inconsistent with hypovolemic shock and would require either increased RPF or enhanced glomerular filtration pressure.
- Maintaining normal RPF during severe hypotension is physiologically implausible.
*No change in RPF and GFR*
- This suggests normal renal function despite **severe hypotension and hypovolemia**, which contradicts basic renal physiology.
- The body's compensatory mechanisms cannot fully maintain both RPF and GFR when systemic blood pressure falls below the autoregulatory threshold.
Renal replacement therapy US Medical PG Question 3: A 33-year-old man presents to the emergency department because of an episode of bloody emesis. He has had increasing dyspnea over the past 2 days. He was diagnosed with peptic ulcer disease last year. He has been on regular hemodialysis for the past 2 years because of end-stage renal disease. He skipped his last dialysis session because of an unexpected business trip. He has no history of liver disease. His supine blood pressure is 110/80 mm Hg and upright is 90/70, pulse is 110/min, respirations are 22/min, and temperature is 36.2°C (97.2°F). The distal extremities are cold to touch, and the outstretched hand shows flapping tremor. A bloody nasogastric lavage is also noted, which eventually clears after saline irrigation. Intravenous isotonic saline and high-dose proton pump inhibitors are initiated, and the patient is admitted into the intensive care unit. Which of the following is the most appropriate next step in the management of this patient?
- A. Observation in the intensive care unit
- B. Double-balloon tamponade
- C. Hemodialysis (Correct Answer)
- D. Transfusion of packed red blood cells
- E. Esophagogastroduodenoscopy
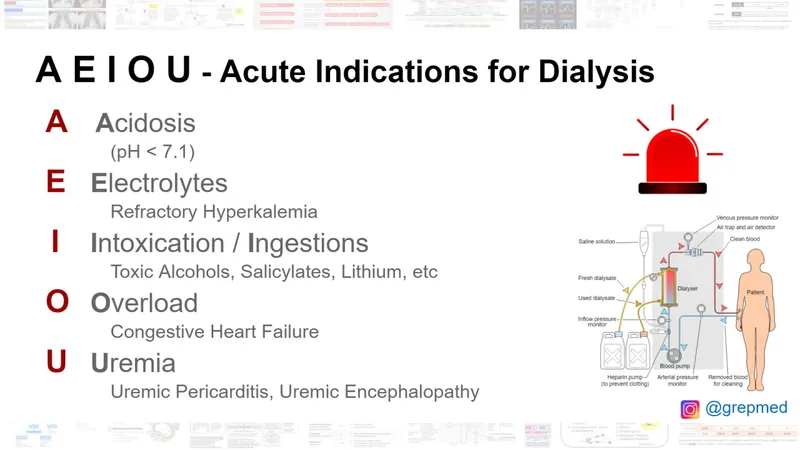
Renal replacement therapy Explanation: ***Hemodialysis***
- The patient has **end-stage renal disease** and missed his last dialysis session, leading to **uremic crisis** with **dyspnea** (fluid overload) and **asterixis** (uremic encephalopathy).
- **Uremic platelet dysfunction** also contributes to the GI bleeding, making dialysis essential to correct coagulopathy.
- Emergency hemodialysis is the most critical intervention to remove accumulated toxins, correct fluid overload, and improve hemostasis before any invasive procedures.
*Observation in the intensive care unit*
- While ICU admission is appropriate for monitoring, passive observation without addressing the underlying **uremia** will not resolve the critical issues of **fluid overload**, **uremic encephalopathy**, and **uremic coagulopathy**.
- The patient's missed dialysis session and severe symptoms necessitate active intervention, not just observation.
*Double-balloon tamponade*
- This procedure is reserved for **life-threatening variceal bleeding** that is refractory to endoscopic treatment.
- The patient's history of **peptic ulcer disease** (not cirrhosis) and the clearing of bloody lavage with saline irrigation suggest non-variceal bleeding, making tamponade inappropriate.
*Transfusion of packed red blood cells*
- While the patient shows signs of **orthostatic hypotension** and **tachycardia** suggesting hypovolemia, the GI bleeding has **stabilized** (NG lavage cleared with irrigation).
- Transfusion may be needed based on hemoglobin levels, but it does not address the **immediately life-threatening uremic crisis** with encephalopathy and platelet dysfunction.
- The most urgent priority is dialysis to stabilize the patient for subsequent procedures.
*Esophagogastroduodenoscopy*
- EGD is indicated to identify and potentially treat the source of **upper GI bleeding** in a patient with **peptic ulcer disease**.
- However, the patient's severe **uremic symptoms**, **encephalopathy**, and **coagulopathy** must be addressed first to safely perform this invasive procedure and optimize outcomes.
Renal replacement therapy US Medical PG Question 4: A 50-year-old man with a history of stage 4 kidney disease was admitted to the hospital for an elective hemicolectomy. His past medical history is significant for severe diverticulitis. After the procedure he becomes septic and was placed on broad spectrum antibiotics. On morning rounds, he appear weak and complains of fatigue and nausea. His words are soft and he has difficulty answering questions. His temperature is 38.9°C (102.1°F), heart rate is 110/min, respiratory rate is 15/min, blood pressure 90/65 mm Hg, and saturation is 89% on room air. On physical exam, his mental status appears altered. He has a bruise on his left arm that spontaneously appeared overnight. His cardiac exam is positive for a weak friction rub. Blood specimens are collected and sent for evaluation. An ECG is performed (see image). What therapy will this patient most likely receive next?
- A. Send the patient for hemodialysis (Correct Answer)
- B. Perform a STAT pericardiocentesis
- C. Prepare the patient for renal transplant
- D. Treat the patient with aspirin
- E. Treat the patient with cyclophosphamide and prednisone
Renal replacement therapy Explanation: ***Send the patient for hemodialysis***
- This patient presents with symptoms of **uremic encephalopathy** and **uremic pericarditis** in the context of **stage 4 kidney disease**. The altered mental status, weakness, fatigue, nausea, and the development of a bruise (which could indicate uremic coagulopathy) are suggestive of severe uremia. The ECG shows widespread **ST elevation and PR depression**, particularly noticeable in leads like II, V2-V6, which is a classic finding for pericarditis. The **weak friction rub** confirms this clinical suspicion. Hemodialysis is crucial to rapidly remove uremic toxins and resolve both uremic encephalopathy and pericarditis.
- The ECG findings, including diffuse **ST elevation** with **PR depression**, are characteristic of **pericarditis**. In a patient with end-stage renal disease, **uremia** is a common cause of pericarditis, which can be life-threatening if not promptly treated with dialysis.
*Perform a STAT pericardiocentesis*
- While the patient has pericarditis, there are no immediate signs of **cardiac tamponade**, such as muffled heart sounds, jugular venous distension, or pulsus paradoxus, that would necessitate an emergency pericardiocentesis.
- The primary treatment for **uremic pericarditis** is typically **hemodialysis** to resolve the underlying uremic state, not direct fluid removal unless tamponade is present.
*Prepare the patient for renal transplant*
- **Renal transplant** is a long-term solution for end-stage renal disease, but it is not an acute intervention for immediate life-threatening uremic complications like uremic pericarditis and encephalopathy.
- The patient needs urgent stabilization and treatment of his current acute medical issues before transplant consideration.
*Treat the patient with aspirin*
- While aspirin can be used for some forms of pericarditis, it is generally **contraindicated** in patients with **uremic pericarditis** due to the increased risk of **gastric bleeding** and potential exacerbation of uremic coagulopathy.
- The primary treatment for uremic pericarditis is **dialysis**, not anti-inflammatory medications, as the inflammation is driven by uremic toxins.
*Treat the patient with cyclophosphamide and prednisone*
- **Immunosuppressants** like cyclophosphamide and prednisone are used for autoimmune or inflammatory conditions causing pericarditis, such as systemic lupus erythematosus.
- This patient's pericarditis is clearly linked to **uremia** from kidney disease, not an autoimmune condition, making immunosuppressive therapy inappropriate and potentially harmful.
Renal replacement therapy US Medical PG Question 5: A 63-year-old woman comes to the physician for a routine health maintenance examination. She reports feeling tired sometimes and having itchy skin. Over the past 2 years, the amount of urine she passes has been slowly decreasing. She has hypertension and type 2 diabetes mellitus complicated with diabetic nephropathy. Her current medications include insulin, furosemide, amlodipine, and a multivitamin. Her nephrologist recently added erythropoietin to her medication regimen. She follows a diet low in salt, protein, potassium, and phosphorus. Her temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 145/87 mm Hg. Physical examination shows 1+ edema around the ankles bilaterally. Laboratory studies show:
Hemoglobin 9.8 g/dL
Serum
Glucose 98 mg/dL
Albumin 4 g/dL
Na+ 145 mEq/L
Cl– 100 mEq/L
K+ 5.1 mEq/L
Urea nitrogen 46 mg/dL
Creatinine 3.1 mg/dL
Which of the following complications is the most common cause of death in patients receiving long-term treatment for this patient's renal condition?
- A. Malignancy
- B. Anemia
- C. Cardiovascular disease (Correct Answer)
- D. Discontinuation of treatment
- E. Gastrointestinal bleeding
Renal replacement therapy Explanation: ***Cardiovascular disease***
- Patients with **end-stage renal disease (ESRD)**, particularly those on dialysis, have a significantly increased risk of cardiovascular events, including **heart failure**, **myocardial infarction**, and stroke. This is due to accelerated **atherosclerosis**, hypertension, volume overload, and chronic inflammation prevalent in ESRD.
- The patient's history of **hypertension** and **type 2 diabetes mellitus** with **diabetic nephropathy** further exacerbates the risk of cardiovascular complications, making it the leading cause of mortality.
*Malignancy*
- While patients with ESRD do have an increased risk of certain **malignancies** (e.g., kidney, bladder cancer), it is not the most common cause of death compared to cardiovascular disease.
- The immune dysregulation in uremia contributes to this increased risk, but **cardiovascular disease** remains a more significant factor in mortality.
*Anemia*
- **Anemia** is a common complication of ESRD due to decreased **erythropoietin production**, as evidenced by the patient's low hemoglobin and erythropoietin prescription.
- While anemia contributes to fatigue and can worsen cardiovascular outcomes, it is a modifiable risk factor and generally not the direct cause of death; rather, the underlying cardiovascular issues it exacerbates are.
*Discontinuation of treatment*
- While **non-compliance** or discontinuation of treatment can lead to poor outcomes and mortality, it is not considered the most common *medical* cause of death in patients receiving long-term treatment for ESRD.
- The question asks for a medical complication, and cardiovascular disease is a direct physiological consequence of chronic kidney disease and its treatments.
*Gastrointestinal bleeding*
- **Gastrointestinal bleeding** can occur in ESRD patients due to uremic coagulopathy, angiodysplasia, and peptic ulcers, and it can be severe.
- However, while a serious complication, it is **less common** as a cause of death compared to the overwhelming burden of cardiovascular disease in this patient population.
Renal replacement therapy US Medical PG Question 6: A 56-year-old woman presents to the emergency department with muscle weakness. She reports her symptoms have progressively worsened over the course of 2 weeks and are most significant in her lower extremities. She also notices increased urinary frequency. Approximately 1 month ago she was diagnosed with a calcium phosphate nephrolithiasis. Medical history is significant for rheumatoid arthritis diagnosed approximately 10 years ago treated with methotrexate, and type II diabetes mellitus treated with metformin. Her temperature is 98.6°F (37°C), blood pressure is 138/92 mmHg, pulse is 92/min, and respirations are 17/min. On physical exam, there is mild tenderness to palpation of the metacarpophalangeal and proximal interphalangeal joints. There is 4/5 power throughout the lower extremity. Laboratory testing is shown.
Serum:
Na+: 137 mEq/L
Cl-: 106 mEq/L
K+: 2.9 mEq/L
HCO3-: 18 mEq/L
Glucose: 115 mg/dL
Creatinine: 1.0 mg/dL
Urine pH: 5.6
Which of the following is the best next step in management?
- A. Administer intravenous sodium bicarbonate
- B. Increase the methotrexate dose
- C. Administer intravenous insulin
- D. Begin potassium replacement therapy with dextrose (Correct Answer)
- E. Administer hydrochlorothiazide
Renal replacement therapy Explanation: ***Begin potassium replacement therapy with dextrose***
- The patient presents with **muscle weakness**, **hypokalemia** (2.9 mEq/L), and **metabolic acidosis** (HCO3- 18 mEq/L, normal anion gap since Na - Cl - HCO3 = 137 - 106 - 18 = 13). These findings, along with a history of calcium phosphate nephrolithiasis and relatively alkaline urine (pH 5.6) in the presence of acidosis, point to **distal renal tubular acidosis (Type 1 RTA)**.
- **Potassium replacement** is crucial given the severe hypokalemia, which is likely contributing to the muscle weakness. Potassium is typically administered in dextrose-containing fluids to provide a vehicle for safe intravenous administration and prevent venous irritation from concentrated potassium solutions.
*Administer intravenous sodium bicarbonate*
- While the patient has **metabolic acidosis**, sodium bicarbonate is not the immediate priority and could worsen hypokalemia by driving potassium intracellularly through alkalinization.
- The primary issue is the **renal inability to excrete acid** *and* conserve potassium. Both potassium repletion and bicarbonate therapy will ultimately be needed for Type 1 RTA, but **potassium repletion is the immediate priority** given the severe hypokalemia and muscle weakness.
*Increase the methotrexate dose*
- The patient's **rheumatoid arthritis** is treated with methotrexate, but there is no indication that her current symptoms are related to RA flare or that her methotrexate dose is insufficient.
- Increasing methotrexate would not address the **hypokalemia**, **metabolic acidosis**, or **muscle weakness**.
*Administer intravenous insulin*
- The patient has type II diabetes, but her **blood glucose** (115 mg/dL) is well-controlled and does not warrant immediate intravenous insulin.
- **Insulin would be contraindicated** in this setting as it drives potassium into cells, which would worsen the patient's life-threatening hypokalemia.
*Administer hydrochlorothiazide*
- **Hydrochlorothiazide** is a thiazide diuretic that causes **hypokalemia** and **metabolic alkalosis**.
- Administering hydrochlorothiazide would be contraindicated in this patient as it would exacerbate her existing hypokalemia and would not address the underlying **Type 1 RTA** or metabolic acidosis.
Renal replacement therapy US Medical PG Question 7: A 60-year-old man with a long-standing history of type 2 diabetes and hypertension managed with lisinopril and metformin presents with itchy skin. He also describes moderate nausea, vomiting, muscle weakness, and fatigue. The vital signs include: temperature 36.8°C (98.2°F), heart rate 98/min, respiratory rate 15/min, blood pressure 135/85 mm Hg, oxygen saturation 100% on room air. Physical exam is notable for pale conjunctivae, pitting edema, and ascites. Laboratory findings are shown below:
BUN 78 mg/dL
pCO2 25 mm Hg
Creatinine 7.2 mg/dL
Glucose 125 mg/dL
Serum chloride 102 mmol/L
Serum potassium 6.3 mEq/L
Serum sodium 130 mEq/L
Total calcium 1.3 mmol/L
Magnesium 1.2 mEq/L
Phosphate 1.9 mmol/L
Hemoglobin 9.5 g/dL
MCV 86 μm3
Bicarbonate (HCO3) 10 mmol/L
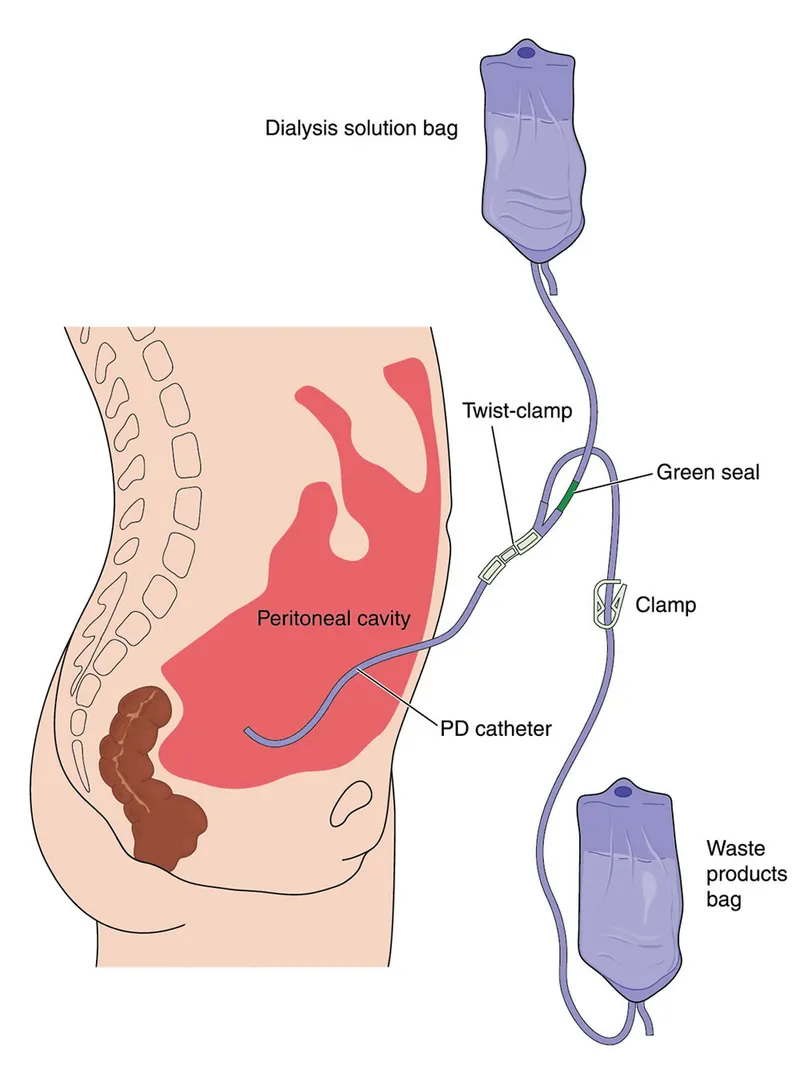
Shrunken kidneys are identified on renal ultrasound. The doctor explains to the patient that he will likely need dialysis due to his significant renal failure until a renal transplant can be performed. The patient is concerned because he is very busy and traveling a lot for work. Given his lifestyle requirements, what is a potential complication of the most appropriate dialysis modality for this patient?
- A. Excessive bleeding
- B. Muscle cramping
- C. Hypotension
- D. Hypertriglyceridemia (Correct Answer)
- E. Hypoglycemia
Renal replacement therapy Explanation: ***Hypertriglyceridemia***
- The patient's **lifestyle requirements** (busy, traveling a lot) suggest **peritoneal dialysis (PD)** as the most appropriate modality due to its flexibility and home-based nature.
- **Hypertriglyceridemia** is a common complication of PD due to the absorption of glucose from the dialysate, which stimulates hepatic triglyceride synthesis.
*Excessive bleeding*
- This is a rare complication in both hemodialysis and peritoneal dialysis.
- While **anti-coagulation** is used in hemodialysis, it's carefully monitored, and significant bleeding is not a typical long-term complication of the chosen modality (PD).
*Muscle cramping*
- **Muscle cramps** can occur with hemodialysis, typically due to rapid fluid and electrolyte shifts.
- This is less common in peritoneal dialysis, which involves a slower and more continuous exchange process.
*Hypotension*
- **Hypotension** can be a complication of hemodialysis due to rapid fluid removal.
- Peritoneal dialysis, with its gradual fluid exchange, is generally less associated with significant hypotensive episodes.
*Hypoglycemia*
- The **glucose-rich dialysate** used in peritoneal dialysis can actually lead to **hyperglycemia**, not hypoglycemia, especially in diabetic patients.
- Regular insulin adjustments are often required for diabetic patients on PD.
Renal replacement therapy US Medical PG Question 8: A 58-year-old man is brought to the Emergency Department after 2 days of shortness of breath, orthopnea, and lower limb edema. His past medical history is significant for hypertension and a myocardial infarction 3 years ago that required a coronary arterial bypass graft. He has not been able to take prescribed medicine in several months due to recent unemployment and issues with insurance. On admission, his blood pressure is 155/92 mmHg, heart rate is 102/min, respiratory rate is 24/min, and temperature is 36.4°C (97.5°F). On physical examination there are fine rales in both lungs, regular and rhythmic cardiac sounds with an S3 gallop and a grade II/VI holosystolic murmur. Initial laboratory tests are shown below:
Na+ 140 mEq/L
K+ 4.2 mEq/L
Cl- 105 mEq/L
BUN 20 mg/dL
Creatinine 0.8 mg/dL
The patient is stabilized and admitted to the hospital. The next day his blood pressure is 110/60 mmHg, heart rate is 110/min, respiratory rate is 18/min, and temperature is 36.4°C (97.5°F). This morning's laboratory tests are shown below:
Na+ 135 mEq/L
K+ 3.2 mEq/L
Cl- 102 mEq/L
BUN 45 mg/dL
Creatinine 1.7 mg/dL
Which of the following best explains the changes seen in this patient?
- A. Urinary tract obstruction
- B. Diuretic therapy (Correct Answer)
- C. Chronic renal failure
- D. Glomerular basement membrane damage
- E. Cholesterol emboli
Renal replacement therapy Explanation: ***Diuretic therapy***
- The patient's initial presentation is consistent with **acute decompensated heart failure**, characterized by shortness of breath, orthopnea, lower limb edema, rales, S3 gallop, and a holosystolic murmur (likely mitral regurgitation due to ventricle dilation). The initial normal kidney function (BUN 20, creatinine 0.8) and electrolyte values support acute heart failure.
- The subsequent drop in blood pressure (155/92 to 110/60 mmHg), increase in heart rate (102 to 110/min), and significant rises in BUN (20 to 45 mg/dL) and creatinine (0.8 to 1.7 mg/dL) with a decrease in potassium (4.2 to 3.2 mEq/L) strongly suggest **diuretic-induced volume depletion** leading to worsened renal function (prerenal azotemia) and hypokalemia.
*Urinary tract obstruction*
- This would typically present with symptoms like **dysuria**, frequency, or hesitancy, and acute kidney injury with a more prominent rise in creatinine relative to BUN, none of which are described.
- Obstruction would be less likely to cause a significant drop in blood pressure and hypokalemia, as seen in this patient.
*Chronic renal failure*
- While kidney function has worsened, the initial labs showed normal kidney function, ruling out **chronic disease** as the cause of the acute deterioration.
- Chronic renal failure would typically present with elevated BUN and creatinine for an extended period, which is not the case here.
*Glomerular basement membrane damage*
- Conditions involving **glomerular damage**, such as glomerulonephritis, typically present with proteinuria, hematuria, and often hypertension, which are not detailed in this scenario.
- The acute changes in electrolytes and BUN/creatinine are more indicative of a **hemodynamic issue** rather than a primary glomerular pathology.
*Cholesterol emboli*
- While a patient with a history of CABG is at risk for **cholesterol emboli**, this condition typically causes acute kidney injury, livedo reticularis, eosinophilia, and digital ischemia, which are not described.
- It would not explain the rapid electrolyte shifts and clear signs of volume depletion seen in this patient.
Renal replacement therapy US Medical PG Question 9: You are called to a hemodialysis suite. The patient is a 61-year-old man with a history of hypertension, hypercholesterolemia, and type-2 diabetes mellitus-induced end-stage renal disease who has required hemodialysis for the past year. His current hemodialysis session is nearing the end when the nurse notices that his blood pressure has dropped to 88/60 mm Hg from his normal of 142/90 mm Hg. The patient denies any shortness of breath or chest pain. He took his daily bisoprolol, metformin, and insulin this morning before coming to the hospital. On examination, the patient’s blood pressure is 92/60 mm Hg, and his heart rate is 119/min. Chest auscultation is unremarkable. What is the most appropriate next management step?
- A. Infuse 1 liter of 0.9% saline
- B. Administer intravenous calcium gluconate
- C. Transfuse the patient with 1 unit of packed red blood cells
- D. Stop ultrafiltration and decrease blood flow into the machine (Correct Answer)
- E. Start the patient on an epinephrine drip
Renal replacement therapy Explanation: ***Stop ultrafiltration and decrease blood flow into the machine***
- The patient's **hypotension** and **tachycardia** during hemodialysis strongly suggest **intradialytic hypotension**, which is often caused by excessive fluid removal (ultrafiltration) or rapid fluid shifts.
- **Stopping ultrafiltration** and **reducing blood flow** allows for gradual re-equilibration of fluid and helps stabilize blood pressure without adding more fluid to a patient with end-stage renal disease.
*Infuse 1 liter of 0.9% saline*
- Administering a large volume of saline is generally **contraindicated in ESRD patients** given their inability to excrete fluid, which could lead to **fluid overload** and pulmonary edema.
- While fluid resuscitation might be considered for severe hypotension, the initial step in intradialytic hypotension is to adjust the dialysis settings.
*Administer intravenous calcium gluconate*
- **Calcium gluconate** is primarily used to stabilize the cardiac membrane in cases of **severe hyperkalemia**, which is not indicated by the current clinical picture.
- There is no mention of ECG changes or lab results to suggest hyperkalemia.
*Transfuse the patient with 1 unit of packed red blood cells*
- There is no clinical evidence of **acute blood loss** or **severe anemia** presenting with hypovolemic shock.
- Transfusion is an intervention for significant blood loss or severe anemia, not for intradialytic hypotension caused by fluid shifts.
*Start the patient on an epinephrine drip*
- **Vasopressors** like epinephrine are typically reserved for **refractory hypotension** after more conservative measures have failed, or in cases of **septic shock** or **anaphylaxis**.
- Initiating a powerful vasopressor as a first step without addressing the potential underlying cause related to dialysis is inappropriate.
Renal replacement therapy US Medical PG Question 10: A 29-year-old man presents to the emergency department with a sharp pain in the center of his chest. The pain is knife-like and constant. Sitting alleviates the pain and lying supine aggravates it. He denies the use of nicotine, alcohol or illicit drugs. Vital signs include: temperature 37.0°C (98.6°F), blood pressure 135/92 mm Hg, and pulse 97/min. On examination, a friction rub is heard at the left sternal border while the patient is leaning forward. His ECG is shown in the image. Which of the following can prevent recurrence of this patient’s condition?
- A. Ibuprofen
- B. Aspirin
- C. Colchicine (Correct Answer)
- D. Glucocorticoids
- E. Systemic antibiotics
Renal replacement therapy Explanation: ***Colchicine***
- Colchicine is an **anti-inflammatory agent** that is highly effective in preventing recurrences of pericarditis, especially when used in conjunction with NSAIDs.
- It is recommended for initial treatment and for several months to reduce the risk of future episodes in cases of acute and recurrent pericarditis.
*Ibuprofen*
- Ibuprofen, a **NSAID**, is a first-line treatment for acute pericarditis to manage pain and inflammation.
- While effective for acute symptom relief, it is not primarily used for long-term prevention of recurrent pericarditis without an additional agent like colchicine.
*Aspirin*
- Aspirin, like other **NSAIDs**, is used to treat the acute inflammation and pain of pericarditis, particularly in patients with acute myocardial infarction.
- It does not offer superior anti-recurrent properties compared to other NSAIDs or colchicine for pericarditis.
*Glucocorticoids*
- Glucocorticoids are generally **reserved for refractory cases** of pericarditis or when NSAIDs and colchicine are contraindicated due to potential side effects and an increased risk of recurrence.
- Their use as a primary agent can actually **increase the risk of recurrence** once tapered, making them a less desirable option for prevention.
*Systemic antibiotics*
- Pericarditis is most commonly **viral or idiopathic**; therefore, systemic antibiotics are not indicated unless there is clear evidence of a bacterial infection.
- The presented symptoms and ECG findings are not suggestive of bacterial pericarditis, which is rare.
More Renal replacement therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.