Primary glomerular diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Primary glomerular diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Primary glomerular diseases US Medical PG Question 1: A 41-year-old man presents at an office for a regular health check-up. He has no complaints. He has no history of significant illnesses. He currently takes omeprazole for gastroesophageal reflux disease. He occasionally smokes cigarettes and drinks alcohol. The family history is unremarkable. The vital signs include: blood pressure 133/67 mm Hg, pulse 67/min, respiratory rate 15/min, and temperature 36.7°C (98.0°F). The physical examination was within normal limits. A complete blood count reveals normal values. A urinalysis was ordered which shows the following:
pH 6.7
Color light yellow
RBC none
WBC none
Protein absent
Cast hyaline casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
Which of the following is the likely etiology for hyaline casts in this patient?
- A. End-stage renal disease/chronic kidney disease (CKD)
- B. Acute interstitial nephritis
- C. Non-specific; can be a normal finding (Correct Answer)
- D. Post-streptococcal glomerulonephritis
- E. Nephrotic syndrome
Primary glomerular diseases Explanation: ***Non-specific; can be a normal finding***
- **Hyaline casts** are formed from precipitated **Tamm-Horsfall mucoprotein** and can be seen in small numbers even in **healthy individuals**, particularly with concentrated urine, dehydration, or strenuous exercise.
- In this patient, the absence of other red flags (normal vitals, normal CBC, no symptoms, and other clear urinalysis findings) makes the presence of hyaline casts a **non-specific finding** and likely benign.
*End-stage renal disease/chronic kidney disease (CKD)*
- While CKD can feature various casts, **broad waxy casts** are more characteristic of advanced and chronic kidney damage, indicating significant tubular dilation.
- The patient's **normal vital signs** and **absence of symptoms or other lab abnormalities** make advanced renal disease unlikely.
*Acute interstitial nephritis*
- **Acute interstitial nephritis** is typically associated with a history of **drug exposure** (e.g., penicillin, NSAIDs, PPIs) and presents with **eosinophiluria**, **white blood cell casts**, and systemic symptoms like fever or rash, none of which are present here.
- The patient is on omeprazole, which can rarely cause AIN, but the **lack of symptoms** (e.g., fever, rash, eosinophilia) and typical findings (e.g. WBC casts) makes it less likely.
*Post-streptococcal glomerulonephritis*
- This condition typically follows a **streptococcal infection** and presents with signs of acute nephritis, including **hematuria**, **red blood cell casts**, and **proteinuria**, which are absent in this urinalysis.
- The patient has **no history of recent infection** or associated symptoms like edema or hypertension.
*Nephrotic syndrome*
- **Nephrotic syndrome** is characterized by **massive proteinuria** (>3.5 g/day), **hypoalbuminemia**, edema, and hyperlipidemia.
- The urinalysis shows **absent protein**, ruling out nephrotic syndrome.
Primary glomerular diseases US Medical PG Question 2: A 12-year-old girl is presented to the office by her mother with complaints of cola-colored urine and mild facial puffiness that began 5 days ago. According to her mother, she had a sore throat 3 weeks ago. Her immunization records are up to date. The mother denies fever and any change in bowel habits. The vital signs include blood pressure 138/78 mm Hg, pulse 88/min, temperature 36.8°C (98.2°F), and respiratory rate 11/min. On physical examination, there is pitting edema of the upper and lower extremities bilaterally. An oropharyngeal examination is normal. Urinalysis shows the following results:
pH 6.2
Color dark brown
Red blood cell (RBC) count 18–20/HPF
White blood cell (WBC) count 3–4/HPF
Protein 1+
Cast RBC casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
24 h urine protein excretion 0.6 g
HPF: high-power field
Which of the following would best describe the light microscopy findings in this case?
- A. Segmental sclerosis and hyalinosis
- B. Wire looping of capillaries
- C. Mesangial proliferation
- D. Hypercellular and enlarged glomeruli (Correct Answer)
- E. Crescentic proliferation consisting of glomerular parietal cells, macrophage, and fibrin
Primary glomerular diseases Explanation: ***Hypercellular and enlarged glomeruli***
- The patient's presentation with **cola-colored urine**, facial puffiness, edema, hypertension, and a recent history of sore throat points to **post-streptococcal glomerulonephritis (PSGN)**.
- Light microscopy in PSGN typically reveals **diffuse hypercellularity** due to proliferation of mesangial and endothelial cells, and infiltration by inflammatory cells, leading to enlarged glomeruli.
*Segmental sclerosis and hyalinosis*
- This finding is characteristic of **focal segmental glomerulosclerosis (FSGS)**, which typically presents with **nephrotic syndrome** (heavy proteinuria, hypoalbuminemia, severe edema).
- While there is proteinuria in this case, it is not in the nephrotic range, and other clinical features do not support FSGS.
*Wire looping of capillaries*
- **Wire looping** is a classic feature of **diffuse proliferative glomerulonephritis (DPGN)**, often seen in **lupus nephritis (Class III or IV)**.
- The patient’s clinical picture, particularly the antecedent sore throat and acute presentation, is not consistent with lupus nephritis.
*Mesangial proliferation*
- While mesangial proliferation occurs in PSGN, it is usually accompanied by **endocapillary proliferation** and inflammatory cell infiltration, making the glomeruli appear diffusely hypercellular and enlarged.
- Isolated mesangial proliferation is more characteristic of **IgA nephropathy**, which typically presents with recurrent episodes of gross hematuria, sometimes concurrent with or shortly after an upper respiratory infection.
*Crescentic proliferation consisting of glomerular parietal cells, macrophage, and fibrin*
- **Crescents** are pathognomonic of **rapidly progressive glomerulonephritis (RPGN)**, which involves severe and rapid loss of renal function.
- While PSGN can occasionally progress to RPGN, the typical presentation of PSGN usually does not involve prominent crescent formation unless severe.
Primary glomerular diseases US Medical PG Question 3: A 20-year-old man comes to the clinic complaining of fever and a sore throat for 5 days. He receives oral penicillin from his primary doctor. After a day of antibiotic treatment, he developed gross hematuria. As a child, he recalls having multiple episodes of hematuria. The vital signs are within normal limits. On physical examination, pharyngeal edema and cervical lymphadenopathy are present. His laboratory examination reveals the following:
WBC 11,000/mm3
Neutrophils 76%
Lymphocytes 23%
Eosinophils 1%
Platelets 150,000/mm3
Hemoglobin 14 g/dL
Hct 41.2%
BUN 16 mg/dL
Creatinine 0.9 mg/dL
ASO titer 100
Urinalysis shows hematuria but no proteinuria. Immunofluorescence shows granular IgA immune complex deposits in the mesangium. Hepatitis B, hepatitis C, and HIV serology are negative. ASO titers and C3 levels are within normal limits. What is the most likely diagnosis?
- A. Berger’s disease (Correct Answer)
- B. Penicillin-induced hypersensitivity reaction
- C. Celiac disease
- D. Hemolytic uremic syndrome
- E. Post-streptococcal glomerulonephritis
Primary glomerular diseases Explanation: ***Berger's disease***
- The co-occurrence of **gross hematuria with an upper respiratory tract infection** (sore throat), the history of **recurrent hematuria**, and the urinalysis showing **hematuria without proteinuria** strongly suggest Berger's disease.
- The definitive diagnostic finding is the **granular IgA immune complex deposits in the mesangium** on immunofluorescence of renal biopsy, which is pathognomonic for IgA nephropathy (Berger's disease).
- The timing is classic for IgA nephropathy: hematuria occurring **concurrently or within 1-2 days** of the upper respiratory infection (synpharyngitic hematuria).
*Penicillin-induced hypersensitivity reaction*
- This condition typically presents with a **rash, fever, and eosinophilia**, not primarily with gross hematuria. While some drug-induced kidney injuries can occur, the specific IgA deposits and recurrent history point away from this.
- The patient's lab results do not show **eosinophilia** (1%), which would be expected in a hypersensitivity reaction.
*Celiac disease*
- Celiac disease is an **autoimmune disorder of the small intestine** triggered by gluten; it primarily causes gastrointestinal symptoms like diarrhea, weight loss, and malabsorption.
- While IgA nephropathy can be associated with celiac disease, celiac disease itself would not cause the presented acute onset of **gross hematuria** or the specific renal biopsy findings.
*Hemolytic uremic syndrome*
- HUS is characterized by the triad of **microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury**.
- This patient does not have **anemia** (Hb 14 g/dL), **thrombocytopenia** (platelets 150,000/mm3), or an elevated **BUN/Creatinine** indicative of acute kidney injury.
*Post-streptococcal glomerulonephritis*
- PSGN typically occurs **1-3 weeks after a streptococcal infection**, presenting with hematuria, proteinuria, edema, and hypertension. In this case, the hematuria occurred **within days of the URI onset**, which is the typical timing for IgA nephropathy, not PSGN.
- Key lab findings for PSGN include **low C3 levels** and significantly elevated **ASO titers**, neither of which (ASO titer 100, C3 within normal limits) were present in this patient.
Primary glomerular diseases US Medical PG Question 4: A 6-year-old boy is brought to the physician because of increasing swelling around his eyes for the past 3 days. During this period, he has had frothy light yellow urine. He had a sore throat 12 days ago. He appears tired. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 105/65 mm Hg. Examination shows periorbital edema and pitting edema of the lower extremities. Cardiopulmonary examination shows no abnormalities. Which of the following findings on urinalysis is most likely associated with this patient's condition?
- A. WBC casts
- B. Fatty casts (Correct Answer)
- C. Hyaline casts
- D. RBC casts
- E. Muddy brown casts
Primary glomerular diseases Explanation: ***Fatty casts***
- The patient's symptoms of **periorbital edema**, **pitting edema of lower extremities**, and **frothy urine** are classic for **nephrotic syndrome**, characterized by massive **proteinuria** (>3.5 g/day), **hypoalbuminemia**, **hyperlipidemia**, and **edema**.
- **Fatty casts** (also called **oval fat bodies** when in tubular cells) are **pathognomonic for nephrotic syndrome** and result from hyperlipidemia and lipiduria associated with severe proteinuria.
- In a **6-year-old child**, the most common cause of nephrotic syndrome is **minimal change disease**.
*WBC casts*
- **WBC casts** indicate **renal parenchymal inflammation** or **infection**, such as **pyelonephritis**, **acute interstitial nephritis**, or **tubulointerstitial disease**.
- These are not characteristic findings in **nephrotic syndrome**, which primarily affects the **glomerular filtration barrier** leading to protein loss rather than inflammatory cell infiltration.
*Hyaline casts*
- **Hyaline casts** are composed of **Tamm-Horsfall protein** and can be found in **normal urine**, especially with **dehydration**, **exercise**, or **concentrated urine**.
- They are **non-specific** and do not indicate significant kidney pathology or nephrotic syndrome.
*RBC casts*
- **RBC casts** are characteristic of **glomerulonephritis** and **nephritic syndrome** (such as **post-streptococcal glomerulonephritis**), where patients present with **hematuria**, **hypertension**, **mild edema**, and **oliguria**.
- While this patient had a **sore throat 12 days ago** (typical timing for post-streptococcal disease), his clinical presentation is clearly **nephrotic** (massive edema, frothy urine, normal blood pressure) rather than **nephritic**, making RBC casts unlikely.
- The **frothy urine** indicates significant **proteinuria**, not hematuria.
*Muddy brown casts*
- **Muddy brown casts** (granular casts with epithelial cell debris) are highly suggestive of **acute tubular necrosis (ATN)**, typically resulting from **ischemic** or **nephrotoxic injury**.
- This patient's presentation with **gradual onset edema** and **frothy urine** points to a **glomerular disorder** (nephrotic syndrome), not **acute tubular injury**.
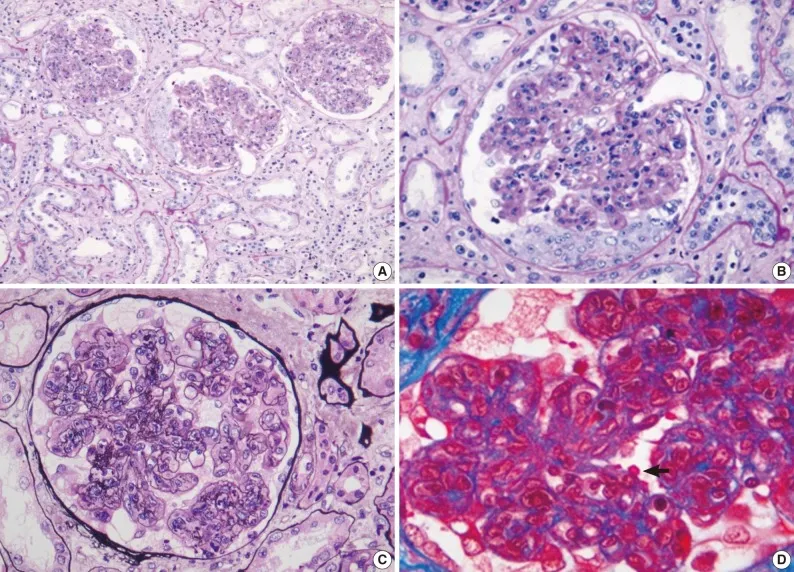
Primary glomerular diseases US Medical PG Question 5: A 62-year-old man comes to the physician because of fatigue and decreased urine output for 2 weeks. He has not been to the physician for many years and takes no medications. Serum studies show a urea nitrogen concentration of 42 mg/dL and a creatinine concentration of 2.3 mg/dL. Urinalysis shows heavy proteinuria. A photomicrograph of a section of a kidney biopsy specimen is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Amyloidosis
- B. Diabetes mellitus (Correct Answer)
- C. Dyslipidemia
- D. Fibromuscular dysplasia
- E. Severe hypertension
Primary glomerular diseases Explanation: ***Diabetes mellitus***
- The kidney biopsy shows **diffuse glomerulosclerosis** with **Kimmelstiel-Wilson nodules** (nodular mesangial sclerosis), which are pathognomonic for **diabetic nephropathy**.
- **Heavy proteinuria**, elevated BUN (42 mg/dL) and creatinine (2.3 mg/dL), along with the patient's age, are consistent with long-standing diabetes mellitus, even if previously undiagnosed.
- Diabetic nephropathy is the leading cause of end-stage renal disease in the United States.
*Amyloidosis*
- While amyloidosis can cause nephrotic syndrome and renal failure, the characteristic histology shows **extracellular amorphous deposits** that stain with **Congo red** and demonstrate apple-green birefringence under polarized light.
- The mesangial nodular pattern seen in diabetic nephropathy is distinct from the amyloid deposits seen in amyloidosis.
- Systemic amyloidosis typically presents with other organ involvement such as **cardiomyopathy**, **hepatosplenomegaly**, or **macroglossia**.
*Dyslipidemia*
- **Dyslipidemia** is a common comorbidity of nephrotic syndrome and diabetic nephropathy, but it is not a direct cause of the structural glomerular damage.
- It represents a metabolic consequence rather than the underlying etiology of the renal pathology.
*Fibromuscular dysplasia*
- **Fibromuscular dysplasia** affects the **renal arteries**, causing **renovascular hypertension** and renal ischemia.
- It typically presents with hypertension in young to middle-aged women and an abdominal bruit, not with heavy proteinuria and glomerular nodular sclerosis.
- The histology would show arterial wall changes, not glomerular pathology.
*Severe hypertension*
- **Severe hypertension** causes hypertensive nephrosclerosis with arteriolosclerosis and global glomerulosclerosis, but not the characteristic **nodular mesangial expansion** (Kimmelstiel-Wilson nodules) seen in diabetic nephropathy.
- While hypertension commonly accompanies diabetic nephropathy, the specific histological findings of nodular glomerulosclerosis are pathognomonic for diabetes mellitus.
- Hypertensive nephrosclerosis shows arteriolar hyalinosis and ischemic changes, which differ from diabetic glomerular changes.
Primary glomerular diseases US Medical PG Question 6: A 4-year-old girl is brought to the physician because of increasing swelling around her eyes and over both her feet for the past 4 days. During this period, she has had frothy light yellow urine. Her vital signs are within normal limits. Physical examination shows periorbital edema and 2+ pitting edema of the lower legs and ankles. A urinalysis of this patient is most likely to show which of the following findings?
- A. Fatty casts (Correct Answer)
- B. Epithelial casts
- C. WBC casts
- D. Waxy casts
- E. Muddy brown casts
Primary glomerular diseases Explanation: ***Fatty casts***
- The presence of **periorbital edema**, **pitting edema** of the lower legs and ankles, and **frothy urine** in a child is highly suggestive of **nephrotic syndrome**.
- **Fatty casts** are formed when lipid-laden renal tubular epithelial cells (oval fat bodies) aggregate and are expelled into the urine, and are characteristically associated with **nephrotic syndrome** due to massive proteinuria and lipiduria.
- Among the cast types listed, fatty casts are the most specific finding for nephrotic syndrome.
*Epithelial casts*
- **Epithelial cell casts** indicate **acute tubular necrosis (ATN)** or other conditions involving damage to the renal tubular epithelium.
- While ATN can cause edema, the clinical presentation here (frothy urine, periorbital edema, absence of oliguria or acute kidney injury) is more classic for nephrotic syndrome.
*WBC casts*
- **White blood cell (WBC) casts** are indicative of **renal parenchymal inflammation** or **infection**, such as pyelonephritis or interstitial nephritis.
- The patient's symptoms do not suggest infection, and there is no mention of fever, dysuria, or flank pain.
*Waxy casts*
- **Waxy casts** typically indicate **chronic kidney disease** and advanced renal failure, representing severe urinary stasis and dilated, damaged tubules.
- The acute onset of symptoms (4 days) in a 4-year-old child makes chronic kidney disease less likely as the primary diagnosis.
*Muddy brown casts*
- **Muddy brown casts** are pathognomonic for **acute tubular necrosis (ATN)**, often seen in cases of ischemia or nephrotoxic injury.
- While ATN is a severe renal injury, the patient's presentation with frothy urine and prominent edema without signs of acute kidney injury points more specifically to nephrotic syndrome.
Primary glomerular diseases US Medical PG Question 7: A 43-year-old man is referred by his family physician because his urine dipstick reveals 3+ protein and urinalysis reveals 1-2 red cells/high power field, but is otherwise negative. He does not have any current complaints. His family history is irrelevant. He denies smoking and alcohol use. His temperature is 36.7°C (98.06°F), blood pressure is 130/82 mm Hg, and pulse is 78/min. Physical examination is unremarkable. Which of the following is the best next step in the management of this patient’s condition?
- A. Reassurance
- B. Repeat the urine dipstick test
- C. 24-hour urine collection (Correct Answer)
- D. Start captopril
- E. Urine culture
Primary glomerular diseases Explanation: ***24-hour urine collection***
- The presence of **3+ proteinuria on dipstick** (approximately ≥300 mg/dL) is significant and requires **quantification** to assess the degree of proteinuria and guide further management.
- A **24-hour urine collection** is the traditional gold standard method to quantify total protein excretion and determine if the patient has clinically significant proteinuria (>150 mg/day is abnormal; >3.5 g/day indicates nephrotic-range proteinuria).
- Alternatively, a **spot urine protein-to-creatinine ratio (PCR)** or **albumin-to-creatinine ratio (ACR)** can be used, but among the given options, 24-hour collection is the appropriate next step.
- The concurrent finding of **microscopic hematuria (1-2 RBCs/hpf)** further supports the need for evaluation of possible **glomerular disease** or other renal pathology.
*Repeat the urine dipstick test*
- Repeating a dipstick is appropriate for **trace or 1+ proteinuria** to rule out transient causes (exercise, fever, orthostatic proteinuria, concentrated urine).
- However, **3+ proteinuria is too significant** to simply repeat the dipstick; it requires quantification to determine the severity and guide further diagnostic workup (e.g., renal biopsy if nephrotic-range).
*Urine culture*
- While infection can cause proteinuria and hematuria, the urinalysis is described as "otherwise negative," suggesting an absence of **leukocytes, nitrites, or bacteria** typical of a urinary tract infection.
- The patient is **asymptomatic** without dysuria, frequency, or fever, making infection unlikely.
- A urine culture would be appropriate if there were clinical signs of UTI.
*Reassurance*
- Giving reassurance would be **inappropriate and potentially harmful** given the finding of **3+ proteinuria**, which is a significant indicator of potential renal pathology.
- Proteinuria of this magnitude can indicate **glomerulonephritis, diabetic nephropathy, hypertensive nephrosclerosis**, or other kidney diseases requiring further evaluation.
- The presence of concurrent **microscopic hematuria** raises additional concern for glomerular disease.
*Start captopril*
- Captopril, an **ACE inhibitor**, is used to reduce proteinuria and provide renoprotection in patients with **confirmed chronic kidney disease**, particularly in the setting of **diabetes or hypertension**.
- Initiating treatment is **premature** without first quantifying the proteinuria, establishing a diagnosis, and ruling out secondary causes.
- The patient's blood pressure (130/82 mm Hg) is at the upper limit of normal but does not mandate immediate antihypertensive therapy before completing the diagnostic evaluation.
Primary glomerular diseases US Medical PG Question 8: A 14-year-old boy is brought to the emergency department from school after falling in gym class. He was unable to stand after the accident and has a painful and swollen knee. On presentation he says that he has never had an incident like this before; however, he does suffer from hard to control nosebleeds and prolonged bleeding after minor cuts. Based on his presentation a panel of bleeding tests is obtained with the following results:
Bleeding time: Prolonged
Prothrombin time: Normal
Partial thromboplastin time: Prolonged
Which of the following describes the function of the component that is defective in the most likely cause of this patient's symptoms?
- A. Binds to a nucleotide derivative
- B. Binds to fibrinogen
- C. Binds to subendothelial collagen (Correct Answer)
- D. It is a cofactor for an epoxide reductase
- E. Catalyzes the conversion of factor X
Primary glomerular diseases Explanation: ***Binds to subendothelial collagen***
- The patient's history of **nosebleeds**, **prolonged bleeding**, and a knee injury suggests a **primary hemostasis** defect. The lab results (prolonged bleeding time, normal PT, prolonged PTT) point to **von Willebrand disease** (vWD).
- The most important function of **von Willebrand factor** (vWF), which is deficient or dysfunctional in vWD, is to mediate platelet adhesion to the **subendothelial collagen** at sites of vascular injury.
*Binds to a nucleotide derivative*
- This option refers to the function of **P2Y12 receptors** on platelets, which bind to ADP (a nucleotide derivative) to promote platelet aggregation.
- While important for platelet function, this is not the primary defect in von Willebrand disease, which is an issue with **platelet adhesion**.
*Binds to fibrinogen*
- **Glycoprotein IIb/IIIa receptors** on platelets bind to **fibrinogen** to mediate platelet aggregation and form a platelet plug.
- This is a secondary step in hemostasis, and while affected by vWF's indirect role in stabilizing FVIII, it's not the direct primary defect.
*It is a cofactor for an epoxide reductase*
- This describes the role of **Vitamin K** in the carboxylation of clotting factors; specifically, its role as a cofactor for **gamma-glutamyl carboxylase**, which is then reduced by **epoxide reductase**.
- Deficiencies in Vitamin K activity affect the **extrinsic** and **common pathways** (factors II, VII, IX, X), which would typically present with a **prolonged PT** in addition to PTT, unlike this patient.
*Catalyzes the conversion of factor X*
- This describes the function of **Factor IXa** (in complex with Factor VIIIa) and **Factor VIIa** (with Tissue Factor), which activate Factor X to Factor Xa.
- While vWF stabilizes **Factor VIII**, leading to prolonged PTT, the direct catalytic conversion of Factor X is not the primary function of vWF itself.
Primary glomerular diseases US Medical PG Question 9: A 44-year-old woman comes to the physician with increasingly yellow sclera and pruritus over the past 3 months. She has intermittent right-upper-quadrant pain and discomfort. She has no history of any serious illnesses and takes no medications. Her vital signs are within normal limits. Her sclera are icteric. Skin examination shows linear scratch marks on the trunk and limbs. The remainder of the physical examination is unremarkable. Laboratory studies show:
Complete blood count
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
Leukocyte count 6,000/mm3 with a normal differential
Serum
Alkaline phosphatase 470 U/L
Aspartate aminotransferase (AST, GOT) 38 U/L
Alanine aminotransferase (ALT, GPT) 45 U/L
γ-Glutamyltransferase (GGT) 83 U/L (N=5–50 U/L)
Bilirubin, total 2.7 mg/dL
Bilirubin, direct 1.4 mg/dL
Magnetic resonance cholangiopancreatography (MRCP) shows a multifocal and diffuse beaded appearance of the intrahepatic and extrahepatic biliary ducts. Which of the following is the most appropriate diagnostic study at this time?
- A. No further testing is indicated
- B. Colonoscopy (Correct Answer)
- C. Liver biopsy
- D. Upper endoscopy
- E. Endoscopic retrograde cholangiopancreatography (ERCP)
Primary glomerular diseases Explanation: ***Colonoscopy***
- The patient's presentation with **pruritus**, **jaundice**, elevated **alkaline phosphatase**, and characteristic **beaded appearance of biliary ducts** on MRCP is highly suggestive of **Primary Sclerosing Cholangitis (PSC)**.
- Approximately **60-80% of patients with PSC** have concomitant **inflammatory bowel disease (IBD)**, particularly **ulcerative colitis**.
- **Colonoscopy with biopsies** is the most appropriate next step to screen for IBD, as it allows visualization of the entire colon and can detect pancolitis or right-sided disease that would be missed by sigmoidoscopy.
- Early detection of IBD is important for management and colorectal cancer surveillance, as PSC-IBD patients have increased risk of colorectal malignancy.
*No further testing is indicated*
- This is incorrect because the patient has clear signs of PSC, and further evaluation is necessary to screen for **associated IBD**, which occurs in the majority of PSC patients.
- Identifying concurrent IBD affects prognosis, management, and surveillance strategies for colorectal cancer.
*Liver biopsy*
- While liver biopsy can provide histological confirmation and staging information, the **MRCP findings of multifocal beaded strictures** are highly specific for PSC and are generally considered **diagnostic**.
- Biopsy carries risks and is typically reserved for cases where imaging is equivocal or when assessing fibrosis stage is critical for management decisions.
- Given the classic MRCP findings, screening for IBD takes priority over liver biopsy.
*Upper endoscopy*
- **Upper endoscopy** evaluates the esophagus, stomach, and duodenum.
- It is not appropriate for screening inflammatory bowel disease or evaluating the biliary tree in the context of suspected PSC.
- Upper endoscopy would be indicated if the patient had upper GI symptoms or if screening for varices was needed in cirrhotic patients.
*Endoscopic retrograde cholangiopancreatography (ERCP)*
- While **ERCP** can visualize the biliary tree, it is an **invasive procedure** with significant risks including **pancreatitis** (3-5% risk), cholangitis, and perforation.
- Given that **MRCP has already demonstrated the characteristic findings** of PSC non-invasively, ERCP is reserved for **therapeutic interventions** (e.g., balloon dilation of dominant strictures, stent placement, or bile duct brushings if cholangiocarcinoma is suspected).
- ERCP is not appropriate as a diagnostic study when MRCP has already established the diagnosis.
Primary glomerular diseases US Medical PG Question 10: A 32-year-old man comes to the emergency department because of recurrent episodes of vomiting for 1 day. He has had over 15 episodes of bilious vomiting. During this period he has had cramping abdominal pain but has not had a bowel movement or passed flatus. He does not have fever or diarrhea. He was diagnosed with Crohn disease at the age of 28 years which has been well controlled with oral mesalamine. He underwent a partial small bowel resection for midgut volvulus at birth. His other medications include vitamin B12, folic acid, loperamide, ferrous sulfate, and vitamin D3. He appears uncomfortable and his lips are parched. His temperature is 37.1°C (99.3°F), pulse is 103/min, and blood pressure is 104/70 mm Hg. The abdomen is distended, tympanitic, and tender to palpation over the periumbilical area and the right lower quadrant. Rectal examination is unremarkable. A CT scan of the abdomen shows multiple dilated loops of small bowel with a transition zone in the mid to distal ileum. After 24 hours of conservative management with IV fluid resuscitation, nasogastric bowel decompression, promethazine, and analgesia, his condition does not improve and a laparotomy is scheduled. During the laparotomy, two discrete strictures are noted in the mid-ileum, around 20 cm apart. Which of the following is the most appropriate next step in management?
- A. Small bowel resection with ileostomy
- B. Abdominal closure and start palliative care
- C. Small bowel resection and primary anastomosis
- D. Strictureplasty of individual strictures (Correct Answer)
- E. Ileocolectomy
Primary glomerular diseases Explanation: ***Strictureplasty of individual strictures***
- This patient presents with **multiple strictures** in the mid-ileum causing a small bowel obstruction in the setting of **Crohn's disease**. Strictureplasty is the preferred surgical approach for *short, multiple (up to four), or recurrent Crohn's disease strictures* as it preserves bowel length.
- While small bowel resection is an option, **strictureplasty** is favored in Crohn's disease to *avoid short bowel syndrome*, especially if multiple strictures are present, as seen here.
*Small bowel resection with ileostomy*
- An ileostomy is typically created when a primary anastomosis is not safe due to high risk of leak (e.g., severe inflammation, peritonitis, patient instability) or when there is extensive disease not amenable to strictureplasty with primary anastomosis.
- Performing an ileostomy when primary anastomosis is possible unnecessarily creates a stoma, which can lead to complications and impact quality of life.
*Abdominal closure and start palliative care*
- This patient, while acutely unwell, has a surgically correctable cause for his obstruction and is not described as having an incurable or end-stage condition necessitating only palliative care.
- Palliative care would be considered for patients with widespread untreatable disease or severe comorbidities, which is not indicated here given the localized, treatable strictures.
*Small bowel resection and primary anastomosis*
- While small bowel resection is a valid treatment for isolated, non-recurrent strictures, strictureplasty is generally preferred in Crohn's disease when multiple strictures are present.
- **Resection of multiple segments** can lead to significant **short bowel syndrome**, especially in a patient with a history of prior small bowel resection, making strictureplasty a more bowel-sparing and appropriate choice.
*Ileocolectomy*
- **Ileocolectomy** involves resection of the terminal ileum and a portion of the colon. This would be indicated if the disease involves the *ileocecal valve region* or the *colon*, which is not the case in this patient, whose strictures are in the mid-ileum.
- This procedure is excessive for mid-ileal strictures and would result in unnecessary removal of healthy bowel given the location of the strictures.
More Primary glomerular diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.