Nephritic syndrome US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nephritic syndrome. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nephritic syndrome US Medical PG Question 1: A 41-year-old man presents at an office for a regular health check-up. He has no complaints. He has no history of significant illnesses. He currently takes omeprazole for gastroesophageal reflux disease. He occasionally smokes cigarettes and drinks alcohol. The family history is unremarkable. The vital signs include: blood pressure 133/67 mm Hg, pulse 67/min, respiratory rate 15/min, and temperature 36.7°C (98.0°F). The physical examination was within normal limits. A complete blood count reveals normal values. A urinalysis was ordered which shows the following:
pH 6.7
Color light yellow
RBC none
WBC none
Protein absent
Cast hyaline casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
Which of the following is the likely etiology for hyaline casts in this patient?
- A. End-stage renal disease/chronic kidney disease (CKD)
- B. Acute interstitial nephritis
- C. Non-specific; can be a normal finding (Correct Answer)
- D. Post-streptococcal glomerulonephritis
- E. Nephrotic syndrome
Nephritic syndrome Explanation: ***Non-specific; can be a normal finding***
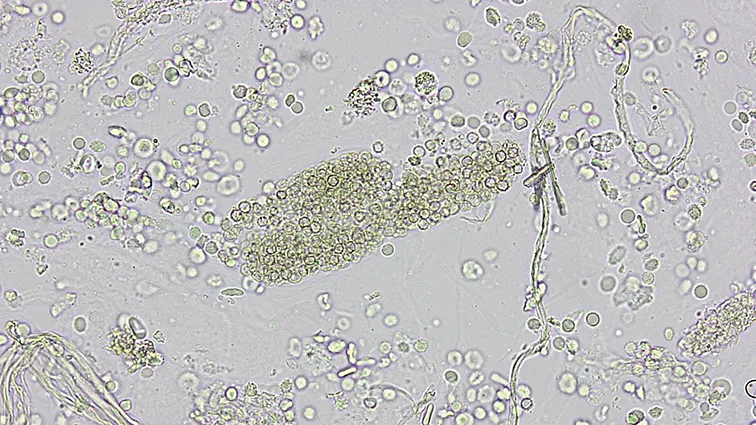
- **Hyaline casts** are formed from precipitated **Tamm-Horsfall mucoprotein** and can be seen in small numbers even in **healthy individuals**, particularly with concentrated urine, dehydration, or strenuous exercise.
- In this patient, the absence of other red flags (normal vitals, normal CBC, no symptoms, and other clear urinalysis findings) makes the presence of hyaline casts a **non-specific finding** and likely benign.
*End-stage renal disease/chronic kidney disease (CKD)*
- While CKD can feature various casts, **broad waxy casts** are more characteristic of advanced and chronic kidney damage, indicating significant tubular dilation.
- The patient's **normal vital signs** and **absence of symptoms or other lab abnormalities** make advanced renal disease unlikely.
*Acute interstitial nephritis*
- **Acute interstitial nephritis** is typically associated with a history of **drug exposure** (e.g., penicillin, NSAIDs, PPIs) and presents with **eosinophiluria**, **white blood cell casts**, and systemic symptoms like fever or rash, none of which are present here.
- The patient is on omeprazole, which can rarely cause AIN, but the **lack of symptoms** (e.g., fever, rash, eosinophilia) and typical findings (e.g. WBC casts) makes it less likely.
*Post-streptococcal glomerulonephritis*
- This condition typically follows a **streptococcal infection** and presents with signs of acute nephritis, including **hematuria**, **red blood cell casts**, and **proteinuria**, which are absent in this urinalysis.
- The patient has **no history of recent infection** or associated symptoms like edema or hypertension.
*Nephrotic syndrome*
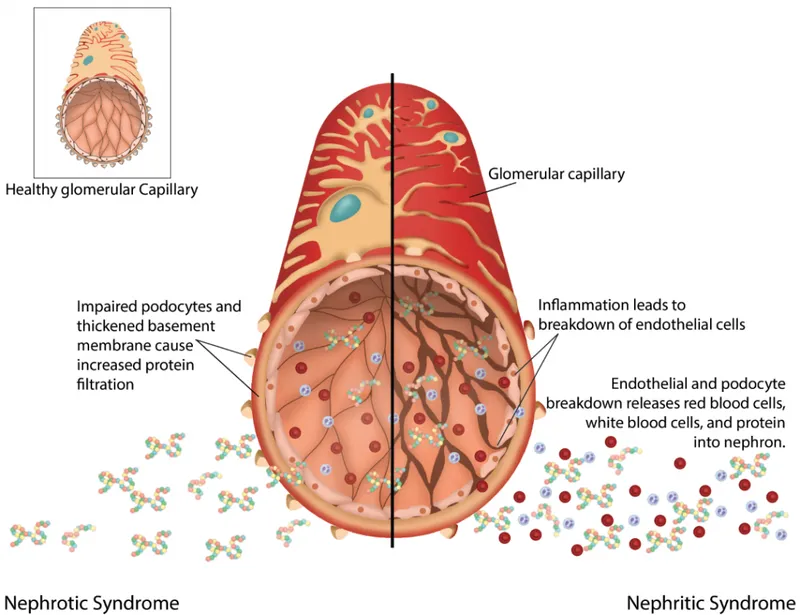
- **Nephrotic syndrome** is characterized by **massive proteinuria** (>3.5 g/day), **hypoalbuminemia**, edema, and hyperlipidemia.
- The urinalysis shows **absent protein**, ruling out nephrotic syndrome.
Nephritic syndrome US Medical PG Question 2: A 43-year-old man comes to the physician for a 1-week history of swelling around his eyes and decreased urination. His pulse is 87/min, and blood pressure is 152/95 mm Hg. Physical examination shows 1+ periorbital and pretibial edema. Serum studies show a urea nitrogen concentration of 21 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows 3+ blood and 1+ protein. Further evaluation of this patient is most likely to show which of the following?
- A. Urinary rhomboid crystals
- B. Renal interstitial inflammation
- C. Hypoalbuminemia
- D. Detached renal tubular epithelial cells
- E. Red blood cell casts (Correct Answer)
Nephritic syndrome Explanation: ***Red blood cell casts***
- The patient's presentation with **periorbital and pretibial edema**, **hypertension**, elevated **creatinine**, **hematuria** (3+ blood), and mild **proteinuria** (1+ protein) is highly suggestive of **acute glomerulonephritis**.
- **Red blood cell casts** are pathognomonic for **glomerulonephritis**, indicating that red blood cells are leaking from the glomeruli and congealing in the renal tubules.
*Urinary rhomboid crystals*
- **Urinary rhomboid crystals** are typically associated with conditions like **uric acid nephrolithiasis** or gout, which are not suggested by the patient's symptoms or lab findings.
- Their presence would indicate a risk for **kidney stones**, not evidence of glomerular inflammation.
*Renal interstitial inflammation*
- **Renal interstitial inflammation** is characteristic of **acute interstitial nephritis**, which often presents with fever, rash, eosinophilia, and flank pain, usually due to drug reactions or infections.
- While kidney injury can occur, the primary findings of **hematuria** and **proteinuria** in this context strongly point away from an interstitial process as the initial diagnosis.
*Hypoalbuminemia*
- **Hypoalbuminemia** is a hallmark of **nephrotic syndrome**, characterized by severe proteinuria (>3.5 g/day), significant edema, and hyperlipidemia.
- This patient has only 1+ proteinuria, which is not severe enough to cause significant hypoalbuminemia or the full nephrotic picture.
*Detached renal tubular epithelial cells*
- **Detached renal tubular epithelial cells** and **tubular cell casts** are characteristic findings in **acute tubular necrosis (ATN)**, usually resulting from ischemia or nephrotoxins.
- While ATN can cause acute kidney injury, the prominent **hematuria** and **hypertension** in this case are more indicative of a glomerular process than tubular damage.
Nephritic syndrome US Medical PG Question 3: A 62-year-old woman with type 2 diabetes mellitus comes to the physician because of a 3-month history of fatigue and weakness. Her hemoglobin A1c concentration was 13.5% 12 weeks ago. Her blood pressure is 152/92 mm Hg. Examination shows lower extremity edema. Serum studies show:
K+ 5.1 mEq/L
Phosphorus 5.0 mg/dL
Ca2+ 7.8 mg/dL
Urea nitrogen 60 mg/dL
Creatinine 2.2 mg/dL
Which of the following is the best parameter for early detection of this patient’s renal condition?
- A. Serum total protein
- B. Serum creatinine
- C. Urinary red blood cell casts
- D. Serum urea nitrogen
- E. Urinary albumin (Correct Answer)
Nephritic syndrome Explanation: ***Urinary albumin***
- **Microalbuminuria** is often the earliest detectable sign of **diabetic nephropathy**, occurring before changes in GFR or serum creatinine become apparent.
- Regular screening for urinary albumin in diabetic patients allows for early intervention to slow the progression of **renal damage**.
*Serum total protein*
- **Hypoalbuminemia** can be seen in advanced renal disease due to significant proteinuria, but it is not an early marker.
- Other conditions like **liver disease** or **malnutrition** can also cause altered serum total protein, making it less specific for early renal damage.
*Serum creatinine*
- **Serum creatinine** levels rise significantly only after a substantial portion of kidney function (around 50%) has been lost.
- Therefore, it is a marker of established renal dysfunction rather than an early indicator.
*Urinary red blood cell casts*
- The presence of **red blood cell casts** in urine indicates **glomerulonephritis** or other inflammatory conditions affecting the glomeruli.
- While concerning, it is not the typical or earliest presentation of **diabetic nephropathy**, which primarily involves proteinuria.
*Serum urea nitrogen*
- **Blood urea nitrogen (BUN)** levels, like creatinine, increase with declining kidney function and are used to assess the severity of **renal impairment**.
- However, BUN levels can also be influenced by factors like **hydration status** and **protein intake**, and they are not an early marker of nascent renal disease.
Nephritic syndrome US Medical PG Question 4: A 54-year-old African American man presents to the clinic for his first annual well-check. He was unemployed for years but recently received health insurance from a new job. He reports feeling healthy and has no complaints. His blood pressure is 157/90 mmHg, pulse is 86/min, and respirations are 12/min. Routine urinalysis demonstrated a mild increase in albumin and creatinine. What medication is indicated at this time?
- A. Hydrochlorothiazide
- B. Metoprolol
- C. Furosemide
- D. Lisinopril (Correct Answer)
- E. Amlodipine
Nephritic syndrome Explanation: ***Lisinopril***
- This patient presents with **hypertension (157/90 mmHg)** and **mild albuminuria with elevated creatinine**, indicating early chronic kidney disease (CKD). An **ACE inhibitor (e.g., lisinopril)** is the first-line treatment for hypertension in **any patient with CKD or proteinuria**, regardless of race or ethnicity.
- ACE inhibitors are **renoprotective** by reducing intraglomerular pressure and slowing progression of kidney disease. The presence of albuminuria represents a **compelling indication** that overrides other considerations for initial antihypertensive selection.
- Note: While ACE inhibitors are typically **less effective** as monotherapy in African Americans without compelling indications, the presence of CKD/proteinuria makes them the preferred agent.
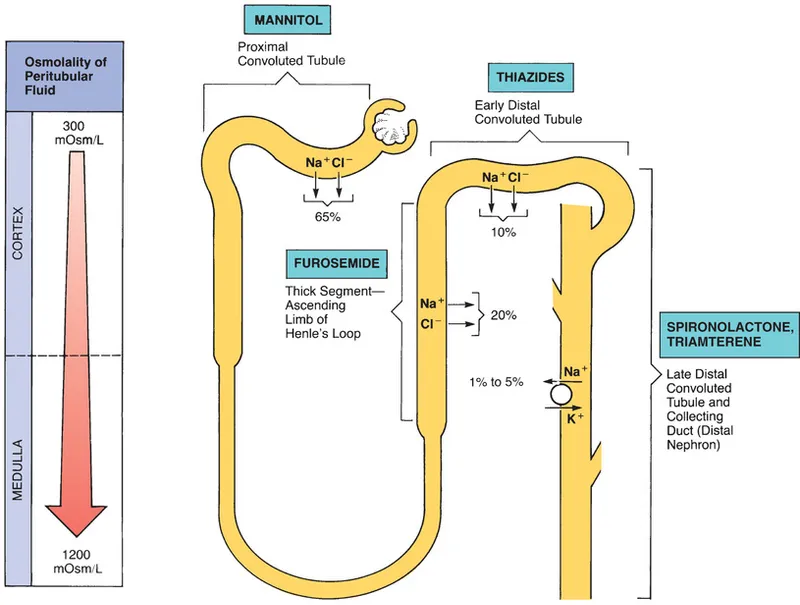
*Hydrochlorothiazide*
- While a **thiazide diuretic** like hydrochlorothiazide would be an appropriate first-line agent for this African American patient with uncomplicated hypertension, it is **less effective** than an ACE inhibitor in patients with **proteinuria or kidney disease**.
- It does not offer the same degree of **renoprotection** as an ACE inhibitor in this clinical scenario with documented albuminuria.
*Metoprolol*
- **Beta-blockers** like metoprolol are effective antihypertensives but are generally **not considered first-line** for uncomplicated hypertension unless there are compelling indications like heart failure, angina, or history of myocardial infarction.
- They also do not provide the specific **renoprotective benefits** seen with ACE inhibitors in patients with albuminuria.
*Furosemide*
- **Loop diuretics** such as furosemide are potent diuretics primarily used for managing **symptoms of fluid overload** (e.g., heart failure, severe edema) and are not typically the first choice for chronic hypertension without such indications.
- For patients with **mild kidney impairment and hypertension without volume overload**, an ACE inhibitor is preferred for its renoprotective effects.
*Amlodipine*
- **Calcium channel blockers** like amlodipine are effective antihypertensives and would typically be an excellent first-line choice for an African American patient with hypertension.
- However, for this patient with **documented albuminuria**, an ACE inhibitor is preferred due to its **specific renoprotective effects** and proven benefit in slowing CKD progression, which amlodipine does not provide.
Nephritic syndrome US Medical PG Question 5: A 45-year-old woman comes to the physician because of a 2-week history of fatigue and excessive thirst. During this period, she has not been able to sleep through the night because of the frequent urge to urinate. She also urinates more than usual during the day. She drinks 4–5 liters of water and 1–2 beers daily. She has autosomal dominant polycystic kidney disease, hypertension treated with lisinopril, and bipolar disorder. Therapy with valproic acid was begun after a manic episode 3 months ago. Vital signs are within normal limits. Irregular flank masses are palpated bilaterally. The remainder of the examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 152 mEq/L
K+ 4.1 mEq/L
Cl− 100 mEq/L
HCO3− 25 mEq/L
Creatinine 1.8 mg/dL
Osmolality 312 mOsmol/kg
Glucose 98 mg/dL
Urine osmolality 190 mOsmol/kg
The urine osmolality does not change after 3 hours despite no fluid intake or after administration of desmopressin. Which of the following is the most appropriate next step in management?
- A. Further water restriction
- B. Begin infusion of 3% saline
- C. Desmopressin therapy
- D. Hydrochlorothiazide therapy (Correct Answer)
- E. Amiloride therapy
Nephritic syndrome Explanation: ***Hydrochlorothiazide therapy***
- The patient's presentation of polyuria, polydipsia, hypernatremia, and inappropriately low urine osmolality, unresponsive to **desmopressin**, indicates **nephrogenic diabetes insipidus (NDI)**.
- **Thiazide diuretics**, such as hydrochlorothiazide, induce mild volume depletion, which stimulates proximal tubular water and solute reabsorption, effectively reducing water delivery to the collecting duct and ameliorating symptoms of NDI.
- This is the first-line treatment for NDI regardless of underlying etiology.
*Further water restriction*
- While the patient exhibits polydipsia, further water restriction would exacerbate her **hypernatremia** and dehydration without addressing the underlying inability to concentrate urine.
- This would lead to increased thirst and potentially more severe electrolyte imbalances.
*Begin infusion of 3% saline*
- The patient already has **hypernatremia (Na+ 152 mEq/L)**; infusing **hypertonic saline** would dangerously worsen this condition and increase serum osmolality.
- This intervention is used for severe hyponatremia, not hypernatremia.
*Desmopressin therapy*
- The diagnostic test showed that the urine osmolality did not change after **desmopressin administration**, indicating a lack of renal response to ADH.
- This confirms **nephrogenic diabetes insipidus**, making exogenous ADH (desmopressin) ineffective as a treatment.
*Amiloride therapy*
- **Amiloride**, a potassium-sparing diuretic, is specifically used to treat **lithium-induced NDI** by blocking ENaC channels and reducing lithium uptake in principal cells.
- This patient is on **valproic acid** (not lithium) for bipolar disorder, making amiloride inappropriate.
- Her NDI is likely multifactorial, related to her ADPKD with chronic kidney disease (creatinine 1.8 mg/dL) and possibly valproic acid, but **thiazide diuretics remain first-line regardless of etiology**.
Nephritic syndrome US Medical PG Question 6: A 6-year-old boy presents to your office with hematuria. Two weeks ago the patient had symptoms of a sore throat and fever. Although physical exam is unremarkable, laboratory results show a decreased serum C3 level and an elevated anti-DNAse B titer. Which of the following would you most expect to see on renal biopsy?
- A. Immune complex deposits with a "spike and dome" appearance on electron microscopy
- B. Large, hypercellular glomeruli on light microscopy (Correct Answer)
- C. Wirelooping and hyaline thrombi on light microscopy
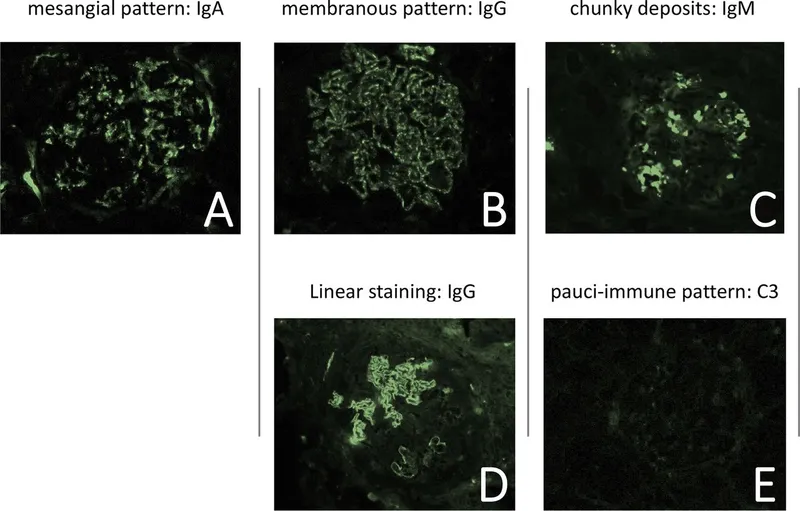
- D. Polyclonal IgA deposition on immunofluorescence
- E. Antibodies to GBM resulting in a linear immunofluorescence pattern
Nephritic syndrome Explanation: ***Large, hypercellular glomeruli on light microscopy***
- The clinical presentation, including recent **sore throat**, **hematuria**, decreased **C3**, and elevated **anti-DNAse B titer**, is highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- On light microscopy, PSGN characteristically shows **diffuse proliferative glomerulonephritis** with **enlarged, hypercellular glomeruli** due to inflammatory cell infiltration and proliferation of intrinsic glomerular cells.
*Immune complex deposits with a "spike and dome" appearance on electron microscopy*
- This "spike and dome" appearance refers to **subepithelial deposits** with new basement membrane formation, which is characteristic of **membranous nephropathy**, not PSGN.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults, which is different from the child's presentation here.
*Wirelooping and hyaline thrombi on light microscopy*
- These features, particularly **"wire-loop" lesions** and **hyaline thrombi**, suggest severe **lupus nephritis**, a manifestation of **systemic lupus erythematosus**.
- Lupus nephritis often presents with a range of kidney pathologies and systemic symptoms not seen in this patient.
*Polyclonal IgA deposition on immunofluorescence*
- **IgA deposition** in the mesangium is the hallmark of **IgA nephropathy (Berger's disease)**, which typically presents with recurrent hematuria, often after an upper respiratory infection.
- While there is hematuria and a recent infection, the decreased C3 and elevated anti-DNAse B titer point away from IgA nephropathy.
*Antibodies to GBM resulting in a linear immunofluorescence pattern*
- A **linear pattern** of IgG deposits along the glomerular basement membrane (GBM) is characteristic of **Goodpasture syndrome (anti-GBM disease)**.
- This condition involves antibodies specifically targeting the GBM and often presents with rapidly progressive glomerulonephritis and pulmonary hemorrhage, which are not described here.
Nephritic syndrome US Medical PG Question 7: A 31-year-old woman presents to her primary care provider to discuss the results from a previous urine analysis. She has no new complaints and feels well. Past medical history is significant for systemic lupus erythematosus. She was diagnosed 5 years ago and takes hydroxychloroquine every day and prednisone when her condition flares. Her previous urine analysis shows elevated protein levels (4+) and blood (3+). The urine sediment contained red blood cells (6 RBCs/high-power field). The treating physician would like to perform a renal biopsy to rule out lupus nephritis. What type of hypersensitivity is suggestive of lupus nephritis?
- A. Type IV, mediated by IgG and IgM antibodies
- B. Type IV, mediated by CD4+ T cells
- C. Type III, mediated by IgG antibodies (Correct Answer)
- D. Type I, mediated by IgE antibodies
- E. Type II, mediated by IgG and IgM antibodies
Nephritic syndrome Explanation: ***Type III, mediated by IgG antibodies***
- Lupus nephritis is a classic example of a **Type III hypersensitivity reaction**, characterized by the formation of **immune complexes** (combinations of antibodies and antigens) in the circulation.
- These circulating **autoantibody-antigen complexes** deposit in the glomeruli of the kidneys, activating complement and initiating an inflammatory response that damages renal tissue.
*Type IV, mediated by IgG and IgM antibodies*
- **Type IV hypersensitivity** is a **delayed-type reaction** mediated by T cells, not antibodies.
- IgG and IgM antibodies are involved in Type II and Type III hypersensitivity, not Type IV.
*Type IV, mediated by CD4+ T cells*
- While **Type IV hypersensitivity** is indeed mediated by **CD4+ T cells** (and CD8+ T cells), lupus nephritis is primarily an **immune complex-mediated (Type III)** disease.
- T cells do play a role in the pathogenesis of SLE, but the direct kidney damage in lupus nephritis is driven by antibody-antigen complex deposition.
*Type I, mediated by IgE antibodies*
- **Type I hypersensitivity** is an **immediate allergic reaction** mediated by **IgE antibodies** binding to mast cells and basophils, leading to histamine release.
- This type of reaction is responsible for conditions like asthma, allergies, and anaphylaxis, and is not involved in lupus nephritis.
*Type II, mediated by IgG and IgM antibodies*
- **Type II hypersensitivity** involves **antibodies directly targeting antigens on cell surfaces or extracellular matrix components**, leading to cell lysis or dysfunction.
- While IgG and IgM are involved, the defining feature is direct binding to fixed tissue antigens rather than deposition of circulating immune complexes as seen in lupus nephritis.
Nephritic syndrome US Medical PG Question 8: A 7-year-old girl is brought to the physician because of generalized fatigue and dark urine for 1 week. Four weeks ago, she was treated with topical mupirocin for a skin infection. Her 5-year-old brother has steroid-resistant nephrotic syndrome. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 14/min, and blood pressure is 132/89 mm Hg. Examination shows periorbital and 1+ pretibial edema bilaterally. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12.9 g/dL
Leukocyte count 7,200/mm3
Platelet count 230,000/mm3
Serum
Urea nitrogen 32 mg/dL
Creatinine 1.8 mg/dL
Urine
Blood 2+
Protein 2+
Glucose negative
RBC 12–14/hpf with dysmorphic features
RBC casts numerous
Which of the following is the most likely cause of these findings?
- A. Antibodies against type IV collagen
- B. Subepithelial immune complex deposition (Correct Answer)
- C. Defective circulating IgA antibodies
- D. Antibodies against cell nucleus proteins
- E. Inflammation of small-sized blood vessels
Nephritic syndrome Explanation: ***Subepithelial immune complex deposition***
- The history of a recent **skin infection** treated with mupirocin, followed by symptoms of **fatigue**, **dark urine**, **edema**, and **hypertension**, strongly suggests **post-streptococcal glomerulonephritis (PSGN)**.
- PSGN is characterized by the deposition of **immune complexes** (containing streptococcal antigens and antibodies) in the subepithelial space of the glomeruli, leading to inflammation and kidney injury.
*Antibodies against type IV collagen*
- This is characteristic of **Goodpasture syndrome**, which presents with rapidly progressive glomerulonephritis and often pulmonary hemorrhage.
- The patient's age and history of a preceding skin infection do not fit the typical presentation of Goodpasture syndrome, and there is no mention of hemoptysis.
*Defective circulating IgA antibodies*
- This describes **IgA nephropathy** (Berger's disease), which is typically characterized by recurrent episodes of gross hematuria, often triggered by a respiratory or gastrointestinal infection.
- While there is hematuria, the timing of symptoms (4 weeks after skin infection) and the presence of significant edema and hypertension differentiate it from typical IgA nephropathy.
*Antibodies against cell nucleus proteins*
- This is characteristic of **systemic lupus erythematosus (SLE)**, which can cause lupus nephritis.
- While lupus nephritis can present with proteinuria, hematuria, and renal failure, the patient's age (7 years old) and the clear history of a preceding streptococcal skin infection without other systemic lupus symptoms make PSGN a more likely diagnosis.
*Inflammation of small-sized blood vessels*
- This describes **vasculitis**, which can affect the kidney (e.g., ANCA-associated vasculitis).
- While vasculitis can cause glomerulonephritis, the specific clinical picture here, especially the recent skin infection and laboratory findings, points more directly to an immune complex-mediated process like PSGN rather than primary small vessel vasculitis.
Nephritic syndrome US Medical PG Question 9: Multiple patients present to your office with hematuria following an outbreak of Group A Streptococcus. Biopsy reveals that all of the patients have the same disease, characterized by large, hypercellular glomeruli with neutrophil infiltration. Which patient has the best prognosis?
- A. 38-year-old man with sickle cell trait
- B. 65-year-old nulliparous woman
- C. 18-year-old man treated with corticosteroids
- D. 50-year-old man with a history of strep infection
- E. 8-year-old boy who undergoes no treatment (Correct Answer)
Nephritic syndrome Explanation: **8-year-old boy who undergoes no treatment**
- **Post-streptococcal glomerulonephritis (PSGN)** has an excellent prognosis in children, with over 95% making a full recovery, regardless of treatment.
- Children are known to spontaneously resolve the condition, often without long-term renal complications.
- **Age is the single most important prognostic factor** in PSGN, and pediatric patients have significantly better outcomes than adults.
*38-year-old man with sickle cell trait*
- While sickle cell trait is generally asymptomatic, it is not a factor that improves the prognosis of PSGN.
- Adult patients typically have a worse prognosis for PSGN compared to children, with only ~50% achieving complete recovery and higher risk of developing chronic kidney disease.
*65-year-old nulliparous woman*
- **Older age** is a significant risk factor for worse prognosis in PSGN, with elderly patients having the highest likelihood of progressing to chronic renal failure.
- Gender and parity status do not directly influence the prognosis of PSGN.
*18-year-old man treated with corticosteroids*
- Corticosteroids are **not indicated** for the routine treatment of PSGN and do not improve its prognosis, as the disease is typically self-limiting.
- This patient's age (18 years old) places him at the transition between pediatric and adult outcomes, generally with a less favorable prognosis than younger children.
*50-year-old man with a history of strep infection*
- A history of strep infection is the **etiological cause** of PSGN but provides no prognostic advantage.
- Middle-aged and older adults have significantly worse outcomes in PSGN compared to children, with increased risk of progression to chronic kidney disease.
Nephritic syndrome US Medical PG Question 10: A 65-year old man comes to the emergency department because of altered mental status for 1 day. He has had headaches, severe nausea, vomiting, and diarrhea for 2 days. He has a history of hypertension, insomnia, and bipolar disorder. His medications include lisinopril, fluoxetine, atorvastatin, lithium, olanzapine, and alprazolam. His temperature is 37.2 °C (99.0 °F), pulse is 90/min, respirations are 22/min, and blood pressure is 102/68 mm Hg. He is somnolent and confused. His mucous membranes are dry. Neurological examination shows dysarthria, decreased muscle strength throughout, and a coarse tremor of the hands bilaterally. The remainder of the examination shows no abnormalities. In addition to IV hydration and electrolyte supplementation, which of the following is the next best step in management?
- A. Bowel irrigation
- B. Intravenous diazepam
- C. Oral cyproheptadine
- D. Intravenous dantrolene
- E. Hemodialysis (Correct Answer)
Nephritic syndrome Explanation: ***Hemodialysis***
- This patient presents with symptoms consistent with **severe lithium toxicity** (altered mental status, somnolence, confusion, dysarthria, decreased muscle strength, coarse tremor) likely exacerbated by dehydration due to nausea, vomiting, and diarrhea.
- **Hemodialysis** is indicated for severe lithium toxicity, especially when plasma lithium levels are very high (>4.0 mEq/L), there are signs of cerebellar toxicity or seizures, or if renal impairment prevents adequate lithium excretion.
*Bowel irrigation*
- **Whole-bowel irrigation** is primarily used for large ingestions of sustained-release or enteric-coated medications, or substances not adsorbed by activated charcoal.
- It is generally *not* effective for removing lithium, as lithium is rapidly and completely absorbed from the gastrointestinal tract.
*Intravenous diazepam*
- **Benzodiazepines** like diazepam are useful for managing seizures or severe agitation associated with drug toxicities but do not address the underlying cause of lithium toxicity by removing the drug from the body.
- While agitation and seizures might occur in severe lithium toxicity, the primary initial step in severe cases is to remove the excess lithium.
*Oral cyproheptadine*
- **Cyproheptadine** is an antihistamine with antiserotonergic properties, used in the treatment of **serotonin syndrome**.
- This patient's clinical presentation is classic for **lithium toxicity**, not serotonin syndrome, although fluoxetine can contribute to serotonin syndrome, the tremor and neurological picture coupled with lithium use points to lithium toxicity.
*Intravenous dantrolene*
- **Dantrolene** is a muscle relaxant primarily used for conditions like **neuroleptic malignant syndrome** (NMS) or malignant hyperthermia due to its direct action on skeletal muscle.
- It is not indicated for treating the central nervous system effects or removal of lithium in lithium toxicity.
More Nephritic syndrome US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.