Hypertensive nephrosclerosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypertensive nephrosclerosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypertensive nephrosclerosis US Medical PG Question 1: A 50-year-old man presents with headache, chest discomfort, and blurred vision. His headache started 2 days ago and has not improved. He describes it as severe, throbbing, localized to the occipital part of the head and worse at the end of the day. He says he has associated nausea but denies any vomiting. Past medical history is significant for hypertension diagnosed 15 years ago, managed with beta-blockers until the patient self d/c’ed them a month ago. He has not seen a physician for the past 2 years. Family history is significant for hypertension and an ST-elevation myocardial infarction in his father and diabetes mellitus in his mother. Vitals signs are a blood pressure of 200/110 mm Hg, a pulse rate of 100/min and respiratory rate of 18/min Ophthalmoscopy reveals arteriolar nicking and papilledema. His ECG is normal. Laboratory findings are significant for a serum creatinine of 1.4 mg/dL and a blood urea nitrogen of 25 mg/dL. Urinalysis has 2+ protein. He is started on intravenous nitroprusside. Which of the following best explains the pathophysiology responsible for the neovascular changes present in this patient?
- A. Protein deposition in the vascular lumen
- B. Transmural calcification of arterial walls
- C. Smooth muscle hyperplasia and duplication of the basement membrane (Correct Answer)
- D. Weakening of vessel wall following endothelial injury
- E. Cholesterol deposition in the vascular lumen
Hypertensive nephrosclerosis Explanation: ***Smooth muscle hyperplasia and duplication of the basement membrane***
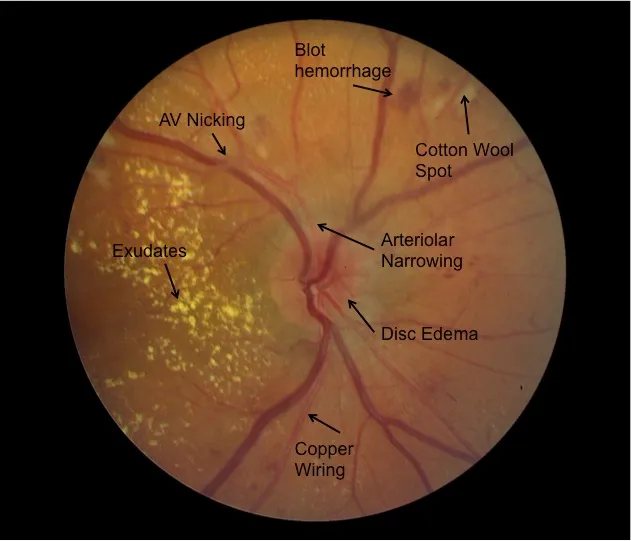
- This patient is experiencing a **hypertensive emergency**, evidenced by symptoms of end-organ damage (blurred vision, papilledema, acute kidney injury) in the presence of severe hypertension (BP 200/110 mmHg).
- In a hypertensive emergency, the extreme pressure leads to arterial and arteriolar damage characterized by **smooth muscle cell proliferation** and **duplication of the basement membrane**, resulting in **hyperplastic arteriosclerosis** which is responsible for the neovascular changes, particularly in the retinal vessels observed with papilledema [1].
*Protein deposition in the vascular lumen*
- While protein deposition can occur in certain vascular pathologies, such as **amyloidosis**, it is not the primary mechanism for the neovascular changes seen in severe hypertension [1].
- Hypertensive emergencies primarily involve direct structural changes to the vessel walls due to high pressure, not protein accumulation in the lumen.
*Transmural calcification of arterial walls*
- **Calcification of arterial walls** is more typical of **atherosclerosis** or **arteriosclerosis** in its chronic forms, particularly Mönckeberg arteriosclerosis, but does not explain the acute neovascular changes or papilledema in a hypertensive crisis.
- This process is gradual and contributes to vessel stiffness rather than the proliferative changes seen in malignant hypertension [1].
*Weakening of vessel wall following endothelial injury*
- Endothelial injury is a component of hypertensive damage, but the primary acute consequence in a hypertensive emergency is often **fibrinoid necrosis** and subsequent **hyperplastic changes* rather than simple weakening leading to neovascularization [2].
- Weakening of vessel walls is more characteristic of aneurysm formation [1].
*Cholesterol deposition in the vascular lumen*
- **Cholesterol deposition** is the hallmark of **atherosclerosis**, a chronic process leading to plaque formation and arterial narrowing [1].
- While this patient has hypertension, a risk factor for atherosclerosis, cholesterol deposition does not explain the acute neovascular changes or papilledema observed in the context of a hypertensive emergency.
Hypertensive nephrosclerosis US Medical PG Question 2: A 41-year-old man presents at an office for a regular health check-up. He has no complaints. He has no history of significant illnesses. He currently takes omeprazole for gastroesophageal reflux disease. He occasionally smokes cigarettes and drinks alcohol. The family history is unremarkable. The vital signs include: blood pressure 133/67 mm Hg, pulse 67/min, respiratory rate 15/min, and temperature 36.7°C (98.0°F). The physical examination was within normal limits. A complete blood count reveals normal values. A urinalysis was ordered which shows the following:
pH 6.7
Color light yellow
RBC none
WBC none
Protein absent
Cast hyaline casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
Which of the following is the likely etiology for hyaline casts in this patient?
- A. End-stage renal disease/chronic kidney disease (CKD)
- B. Acute interstitial nephritis
- C. Non-specific; can be a normal finding (Correct Answer)
- D. Post-streptococcal glomerulonephritis
- E. Nephrotic syndrome
Hypertensive nephrosclerosis Explanation: ***Non-specific; can be a normal finding***
- **Hyaline casts** are formed from precipitated **Tamm-Horsfall mucoprotein** and can be seen in small numbers even in **healthy individuals**, particularly with concentrated urine, dehydration, or strenuous exercise.
- In this patient, the absence of other red flags (normal vitals, normal CBC, no symptoms, and other clear urinalysis findings) makes the presence of hyaline casts a **non-specific finding** and likely benign.
*End-stage renal disease/chronic kidney disease (CKD)*
- While CKD can feature various casts, **broad waxy casts** are more characteristic of advanced and chronic kidney damage, indicating significant tubular dilation.
- The patient's **normal vital signs** and **absence of symptoms or other lab abnormalities** make advanced renal disease unlikely.
*Acute interstitial nephritis*
- **Acute interstitial nephritis** is typically associated with a history of **drug exposure** (e.g., penicillin, NSAIDs, PPIs) and presents with **eosinophiluria**, **white blood cell casts**, and systemic symptoms like fever or rash, none of which are present here.
- The patient is on omeprazole, which can rarely cause AIN, but the **lack of symptoms** (e.g., fever, rash, eosinophilia) and typical findings (e.g. WBC casts) makes it less likely.
*Post-streptococcal glomerulonephritis*
- This condition typically follows a **streptococcal infection** and presents with signs of acute nephritis, including **hematuria**, **red blood cell casts**, and **proteinuria**, which are absent in this urinalysis.
- The patient has **no history of recent infection** or associated symptoms like edema or hypertension.
*Nephrotic syndrome*
- **Nephrotic syndrome** is characterized by **massive proteinuria** (>3.5 g/day), **hypoalbuminemia**, edema, and hyperlipidemia.
- The urinalysis shows **absent protein**, ruling out nephrotic syndrome.
Hypertensive nephrosclerosis US Medical PG Question 3: A 54-year-old African American man presents to the clinic for his first annual well-check. He was unemployed for years but recently received health insurance from a new job. He reports feeling healthy and has no complaints. His blood pressure is 157/90 mmHg, pulse is 86/min, and respirations are 12/min. Routine urinalysis demonstrated a mild increase in albumin and creatinine. What medication is indicated at this time?
- A. Hydrochlorothiazide
- B. Metoprolol
- C. Furosemide
- D. Lisinopril (Correct Answer)
- E. Amlodipine
Hypertensive nephrosclerosis Explanation: ***Lisinopril***
- This patient presents with **hypertension (157/90 mmHg)** and **mild albuminuria with elevated creatinine**, indicating early chronic kidney disease (CKD). An **ACE inhibitor (e.g., lisinopril)** is the first-line treatment for hypertension in **any patient with CKD or proteinuria**, regardless of race or ethnicity.
- ACE inhibitors are **renoprotective** by reducing intraglomerular pressure and slowing progression of kidney disease. The presence of albuminuria represents a **compelling indication** that overrides other considerations for initial antihypertensive selection.
- Note: While ACE inhibitors are typically **less effective** as monotherapy in African Americans without compelling indications, the presence of CKD/proteinuria makes them the preferred agent.
*Hydrochlorothiazide*
- While a **thiazide diuretic** like hydrochlorothiazide would be an appropriate first-line agent for this African American patient with uncomplicated hypertension, it is **less effective** than an ACE inhibitor in patients with **proteinuria or kidney disease**.
- It does not offer the same degree of **renoprotection** as an ACE inhibitor in this clinical scenario with documented albuminuria.
*Metoprolol*
- **Beta-blockers** like metoprolol are effective antihypertensives but are generally **not considered first-line** for uncomplicated hypertension unless there are compelling indications like heart failure, angina, or history of myocardial infarction.
- They also do not provide the specific **renoprotective benefits** seen with ACE inhibitors in patients with albuminuria.
*Furosemide*
- **Loop diuretics** such as furosemide are potent diuretics primarily used for managing **symptoms of fluid overload** (e.g., heart failure, severe edema) and are not typically the first choice for chronic hypertension without such indications.
- For patients with **mild kidney impairment and hypertension without volume overload**, an ACE inhibitor is preferred for its renoprotective effects.
*Amlodipine*
- **Calcium channel blockers** like amlodipine are effective antihypertensives and would typically be an excellent first-line choice for an African American patient with hypertension.
- However, for this patient with **documented albuminuria**, an ACE inhibitor is preferred due to its **specific renoprotective effects** and proven benefit in slowing CKD progression, which amlodipine does not provide.
Hypertensive nephrosclerosis US Medical PG Question 4: A 56-year-old Caucasian male presents to the clinic to establish care. He has never seen a physician and denies any known medical problems. Physical examination is notable for central obesity, but the patient has regular heart and lung sounds. He has a blood pressure of 157/95 mm Hg and heart rate of 92/min. He follows up 2 weeks later, and his blood pressure continues to be elevated. At this time, you diagnose him with essential hypertension and decide to initiate antihypertensive therapy. Per the Joint National Committee 8 guidelines for treatment of high blood pressure, of the following combinations of drugs, which can be considered for first-line treatment of high blood pressure in the Caucasian population?
- A. ACE inhibitor, ARB, CCB, or thiazide (Correct Answer)
- B. ACE inhibitor, angiotensin receptor blocker (ARB), beta-blocker (BB), or thiazide
- C. ACE inhibitor, ARB, CCB, or loop diuretic
- D. ACE inhibitor, ARB, alpha-blocker, or loop diuretic
- E. ACE inhibitor, ARB, alpha-blocker, or direct vasodilator
Hypertensive nephrosclerosis Explanation: **ACE inhibitor, ARB, CCB, or thiazide**
- The **JNC 8 guidelines** recommend **ACE inhibitors**, **ARBs**, **calcium channel blockers (CCBs)**, and **thiazide diuretics** as first-line agents for essential hypertension in the general non-Black population.
- These drug classes have demonstrated efficacy in reducing cardiovascular events and are generally well-tolerated.
*ACE inhibitor, angiotensin receptor blocker (ARB), beta-blocker (BB), or thiazide*
- While **ACE inhibitors**, **ARBs**, and **thiazides** are first-line, **beta-blockers** are generally not considered first-line for uncomplicated hypertension unless there are specific compelling indications (e.g., post-MI, heart failure).
- **Beta-blockers** are less effective than other first-line agents in preventing stroke in the elderly and may have more side effects in some populations.
*ACE inhibitor, ARB, CCB or loop diuretic*
- **ACE inhibitors**, **ARBs**, and **CCBs** are first-line options, but **loop diuretics** are typically reserved for patients with fluid overload or chronic kidney disease, not for initial management of essential hypertension.
- **Loop diuretics** have a shorter duration of action and a greater electrolyte-wasting effect compared to thiazide diuretics, making them less suitable for long-term monotherapy.
*ACE inhibitor, ARB, alpha-blocker, or loop diuretic*
- **Alpha-blockers** and **loop diuretics** are not considered first-line agents for essential hypertension. **Alpha-blockers** are typically used for benign prostatic hyperplasia or as add-on therapy for resistant hypertension.
- **Alpha-blockers** can cause significant orthostatic hypotension, particularly with the first dose, and have not shown the same cardiovascular protective benefits as true first-line agents.
*ACE inhibitor, ARB, alpha-blocker, or direct vasodilator*
- **Alpha-blockers** and **direct vasodilators** (e.g., hydralazine, minoxidil) are not first-line treatments for essential hypertension.
- **Direct vasodilators** are potent but often cause reflex tachycardia and fluid retention, requiring co-administration with other agents, and are typically reserved for severe or resistant hypertension.
Hypertensive nephrosclerosis US Medical PG Question 5: A 27-year-old woman presents to her primary care physician because of headaches that she has had over the last three weeks. She has not had any significant past medical history though she does recall that various types of cancer run in her family. She has also noticed that she has been gaining some weight, and her feet no longer fit into her favorite shoes. On presentation, her temperature is 98.6°F (37°C), blood pressure is 159/92 mmHg, pulse is 75/min, and respirations are 16/min. Physical exam reveals 1+ edema in her lower extremities bilaterally. She is placed on captopril and presents to the emergency department two weeks later after a minor motor vehicle accident. She is cleared of any serious injuries, and as part of her workup, labs are drawn with the following results:
BUN: 47 mg/dL
Creatinine: 1.4 mg/dL
Which of the following findings would most likely also be seen in this patient?
- A. Mass present in adrenal cortex
- B. Atherosclerotic plaques blocking blood flow
- C. Mass present in adrenal medulla
- D. No lesions present
- E. String-of-beads appearance on angiography (Correct Answer)
Hypertensive nephrosclerosis Explanation: ***String-of-beads appearance on angiography***
- The patient's symptoms of **headaches**, **weight gain**, **bilateral lower extremity edema**, and **hypertension** (159/92 mmHg) in a young woman, especially with the presentation of acute kidney injury after beginning an ACE inhibitor (captopril), are highly suggestive of **renovascular hypertension** due to **fibromuscular dysplasia (FMD)**.
- FMD characteristically presents as a **"string-of-beads"** appearance on renal angiography due to areas of stenosis alternating with aneurysmal dilations in the renal arteries.
*Mass present in adrenal cortex*
- A mass in the adrenal cortex typically causes **hyperaldosteronism (Conn syndrome)** or **Cushing's syndrome**. While hyperaldosteronism can cause hypertension and hypokalemia, it does not explain the acute kidney injury with ACE inhibitor treatment.
- Cushing's syndrome involves **central obesity**, **moon facies**, and **striae**, which are not described.
*Atherosclerotic plaques blocking blood flow*
- **Atherosclerotic renovascular disease** typically affects older individuals with a history of cardiovascular risk factors (diabetes, hyperlipidemia, smoking). This patient is young and has no such history.
- While it can cause renal artery stenosis and acute kidney injury with ACE inhibitors, the demographic profile does not fit.
*Mass present in adrenal medulla*
- A mass in the adrenal medulla suggests a **pheochromocytoma**, which causes **episodic hypertension**, **palpitations**, **sweating**, and **anxiety**.
- The patient's hypertension is sustained, and she does not present with classic symptoms of a pheochromocytoma.
*No lesions present*
- The patient's clinical presentation, including the development of acute kidney injury after starting captopril, strongly indicates an underlying renovascular pathology.
- The absence of lesions would not explain the severe, sustained hypertension and the adverse reaction to captopril.
Hypertensive nephrosclerosis US Medical PG Question 6: A 62-year-old man comes to the physician because of fatigue and swelling of the lower legs for 3 weeks. One year ago, he had an 85% stenosis in the left anterior descending artery, for which he received 2 stents. He was diagnosed with hepatitis C 5 years ago. He has type 2 diabetes mellitus and arterial hypertension. Current medications include aspirin, metformin, and ramipril. He does not smoke or drink alcohol. His temperature is 37°C (98.6°F), pulse is 92/min, and blood pressure is 142/95 mm Hg. Examination shows 2+ pretibial edema bilaterally. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.2 g/dL
Leukocyte count 6500/mm3
Platelet count 188,000/mm3
Serum
Na+ 137 mEq/L
Cl− 105 mEq/L
K+ 5.2 mEq/L
Urea nitrogen 60 mg/dL
Glucose 110 mg/dL
Creatinine 3.9 mg/dL
Albumin 3.6 g/dL
HbA1C 6.8%
Urine
Blood negative
Glucose 1+
Protein 3+
WBC 0–1/hpf
A renal biopsy shows sclerosis in the capillary tufts and arterial hyalinosis. Which of the following is the most likely underlying mechanism of this patient's findings?
- A. Diabetes mellitus
- B. Arterial hypertension (Correct Answer)
- C. Amyloidosis
- D. Membranoproliferative glomerulonephritis
- E. Membranous nephropathy
Hypertensive nephrosclerosis Explanation: ***Arterial hypertension***
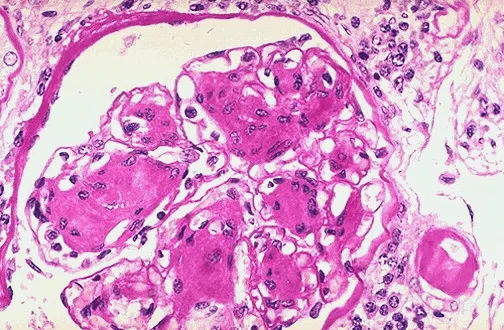
- The patient's **blood pressure of 142/95 mm Hg** and history of arterial hypertension, coupled with **arterial hyalinosis** and **glomerulosclerosis (sclerosis in the capillary tufts)** seen on biopsy, strongly indicate hypertensive nephrosclerosis as the primary cause of renal damage. **Arterial hyalinosis** is the pathognomonic finding of hypertensive nephropathy, resulting from chronic endothelial injury and plasma protein deposition in vessel walls.
- The elevated **urea nitrogen (60 mg/dL)** and **creatinine (3.9 mg/dL)**, along with significant **proteinuria (3+)**, indicate substantial kidney damage, consistent with chronic hypertensive nephrosclerosis.
- The inadequate blood pressure control despite ACE inhibitor therapy (ramipril) demonstrates ongoing hypertensive injury.
*Diabetes mellitus*
- While the patient has diabetes, the biopsy finding of **arterial hyalinosis** and **glomerulosclerosis** is more characteristic of hypertensive nephrosclerosis rather than diabetic nephropathy.
- Diabetic nephropathy typically presents with **glomerular basement membrane thickening**, **mesangial expansion**, and **Kimmelstiel-Wilson nodules** (nodular glomerulosclerosis), which are not the primary biopsy findings described here.
- Additionally, the patient's **good glycemic control (HbA1C 6.8%)** makes advanced diabetic nephropathy less likely.
*Amyloidosis*
- Amyloidosis would typically show characteristic **amyloid deposits** in the glomeruli and interstitium, which stain positive with **Congo red** and exhibit apple-green birefringence under polarized light, findings not reported.
- Presentation usually includes significant proteinuria, often in the nephrotic range, and can affect multiple organs, but the specific biopsy findings of **arterial hyalinosis** point away from amyloidosis as the primary cause.
*Membranoproliferative glomerulonephritis*
- This condition is typically characterized by **mesangial and endothelial proliferation**, **glomerular basement membrane thickening** with a "tram-track" appearance (due to mesangial interposition), and often immune complex deposits.
- While the patient has hepatitis C (a known risk factor for MPGN), the biopsy findings of **glomerulosclerosis** and **arterial hyalinosis** are not specific for MPGN, and the characteristic proliferative changes are not described.
*Membranous nephropathy*
- Membranous nephropathy is primarily characterized by **subepithelial immune complex deposits** and **diffuse thickening of the glomerular basement membrane** (spike and dome appearance on silver stain).
- It is a common cause of nephrotic syndrome in adults, but the biopsy describes **glomerulosclerosis** and **arterial hyalinosis** which are not the hallmark features of membranous nephropathy.
Hypertensive nephrosclerosis US Medical PG Question 7: A 30-year-old African American woman comes to the physician because of fatigue and muscle weakness for the past 5 weeks. During this period, she has had recurrent headaches and palpitations. She has hypertension and major depressive disorder. She works as a nurse at a local hospital. She has smoked about 6–8 cigarettes daily for the past 10 years and drinks 1–2 glasses of wine on weekends. Current medications include enalapril, metoprolol, and fluoxetine. She is 168 cm (5 ft 6 in) tall and weighs 60 kg (132 lb); BMI is 21.3 kg/m2. Her temperature is 37°C (98.6°F), pulse is 75/min, and blood pressure is 155/85 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender; bowel sounds are normal. Her skin is dry and there is no edema in the lower extremities. Laboratory studies show:
Hemoglobin 13.3 g/dL
Serum
Na+ 146 mEq/L
Cl- 105 mEq/L
K+ 3.0 mEq/L
HCO3- 30 mEq/L
Urea nitrogen 10 mg/dL
Glucose 95 mg/dL
Creatinine 0.8 mg/dL
Urine
Blood negative
Glucose negative
Protein negative
RBC 0–1/hpf
WBC none
Which of the following is the most likely diagnosis in this patient?
- A. Cushing syndrome
- B. Aldosteronoma (Correct Answer)
- C. Laxative abuse
- D. Pheochromocytoma
- E. Renal artery stenosis
Hypertensive nephrosclerosis Explanation: ***Aldosteronoma***
- This patient presents with **hypertension**, **muscle weakness**, fatigue, **hypokalemia** (K+ 3.0 mEq/L), and **metabolic alkalosis** (HCO3- 30 mEq/L), which are classic signs of **primary hyperaldosteronism**.
- **Aldosteronomas** are a common cause of primary hyperaldosteronism due to autonomous aldosterone production, leading to sodium retention, potassium excretion, and subsequent hypertension and hypokalemia.
*Cushing syndrome*
- While Cushing syndrome can cause hypertension and muscle weakness, it typically presents with features like **central obesity**, **moon facies**, **buffalo hump**, **striae**, and **hyperglycemia**, which are not described in this patient.
- Although it can cause hypokalemia, the overall clinical picture is more suggestive of primary hyperaldosteronism given the constellation of symptoms.
*Laxative abuse*
- Laxative abuse can cause hypokalemia and metabolic alkalosis, but it typically presents with **diarrhea**, **abdominal pain**, and potentially features of **dehydration**, which are absent here.
- Chronic laxative abuse would not typically be the primary cause of sustained hypertension in this context without other tell-tale signs.
*Pheochromocytoma*
- **Pheochromocytoma** causes episodic or sustained hypertension, often accompanied by **palpitations**, **headaches**, and **sweating** due to excessive catecholamine release.
- However, it does not typically cause hypokalemia or metabolic alkalosis unless there is co-secretion of other hormones, making it less likely than aldosteronoma with the presented lab abnormalities.
*Renal artery stenosis*
- **Renal artery stenosis** can cause hypertension and sometimes hypokalemia due to increased renin secretion, leading to secondary hyperaldosteronism.
- However, the primary cause would be renal ischemia, and the hyperaldosteronism would be reactive, whereas in this case, the hypokalemia and metabolic alkalosis strongly point towards autonomous aldosterone production.
Hypertensive nephrosclerosis US Medical PG Question 8: A 42-year-old man comes to the physician because of a 2-month history of fatigue and increased urination. The patient reports that he has been drinking more than usual because he is constantly thirsty. He has avoided driving for the past 8 weeks because of intermittent episodes of blurred vision. He had elevated blood pressure at his previous visit but is otherwise healthy. Because of his busy work schedule, his diet consists primarily of fast food. He does not smoke or drink alcohol. He is 178 cm (5 ft 10 in) tall and weighs 109 kg (240 lb); BMI is 34 kg/m2. His pulse is 75/min and his blood pressure is 148/95 mm Hg. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin A1c 6.8%
Serum
Glucose 180 mg/dL
Creatinine 1.0 mg/dL
Total cholesterol 220 mg/dL
HDL cholesterol 50 mg/dL
Triglycerides 140 mg/dL
Urine
Blood negative
Glucose 2+
Protein 1+
Ketones negative
Which of the following is the most appropriate next step in management?
- A. Metformin therapy (Correct Answer)
- B. Low-carbohydrate diet
- C. Aspirin therapy
- D. ACE inhibitor therapy
- E. Insulin therapy
Hypertensive nephrosclerosis Explanation: ***Metformin therapy***
- This patient has **newly diagnosed type 2 diabetes mellitus** with classic symptoms (polyuria, polydipsia, blurred vision) and laboratory confirmation (HbA1c 6.8%, glucose 180 mg/dL, glucosuria).
- **Metformin is the first-line pharmacologic therapy** for type 2 diabetes according to current guidelines (ADA, AACE) due to its efficacy, safety profile, cardiovascular benefits, and low risk of hypoglycemia.
- The patient's creatinine is normal (1.0 mg/dL), so metformin is not contraindicated.
- Addressing the **symptomatic hyperglycemia** is the most appropriate next step in management.
*ACE inhibitor therapy*
- ACE inhibitors are indicated for diabetic patients with **hypertension and albuminuria** to provide renoprotection and slow progression of diabetic nephropathy.
- While this patient has both hypertension (148/95 mm Hg) and proteinuria (1+), ACE inhibitor therapy should be initiated **after or concurrent with diabetes management**, not as the sole initial intervention.
- The patient needs **glycemic control first** given symptomatic hyperglycemia, though ACE inhibitor would be an appropriate addition to the treatment regimen.
*Low-carbohydrate diet*
- **Lifestyle modifications** including medical nutrition therapy and exercise are foundational for managing type 2 diabetes and should be recommended.
- However, given the patient's **symptomatic hyperglycemia** (HbA1c 6.8%, glucose 180 mg/dL with classic symptoms), lifestyle changes alone are **insufficient as the initial management**.
- Pharmacologic therapy with metformin should be initiated immediately alongside lifestyle counseling.
*Insulin therapy*
- Insulin therapy is indicated for patients with **very high HbA1c** (typically >9-10%), **severe symptoms of hyperglycemia**, evidence of catabolism, or failure of oral agents.
- This patient's HbA1c of 6.8% represents **relatively mild hyperglycemia** that is appropriately managed with metformin as first-line therapy.
- Insulin is **not indicated** at this stage of disease.
*Aspirin therapy*
- **Aspirin for primary prevention** in diabetes is controversial; current guidelines suggest shared decision-making for patients at increased cardiovascular risk without high bleeding risk.
- While this patient has cardiovascular risk factors (diabetes, hypertension, obesity, dyslipidemia), aspirin would be a **secondary priority** after addressing the acute metabolic derangements.
- **Glycemic control takes precedence** over aspirin initiation in newly diagnosed diabetes.
Hypertensive nephrosclerosis US Medical PG Question 9: A 59-year-old man presents to his primary care provider with the complaint of daytime fatigue. He often has a headache that is worse in the morning and feels tired when he awakes. He perpetually feels fatigued even when he sleeps in. The patient lives alone, drinks 2-3 beers daily, drinks coffee regularly, and has a 10 pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 180/110 mm Hg, pulse is 80/min, respirations are 13/min, and oxygen saturation is 98% on room air. Physical exam is notable for a BMI of 39 kg/m^2. The rest of the patient's pulmonary and neurological exams are unremarkable. Which of the following is the best next step in management?
- A. Caffeine avoidance
- B. Screening for depression
- C. Alcohol avoidance in the evening
- D. CT head
- E. Weight loss (Correct Answer)
Hypertensive nephrosclerosis Explanation: ***Weight Loss***
- The patient's **BMI of 39 kg/m²** indicates **class III obesity**, which is the strongest modifiable risk factor for **obstructive sleep apnea (OSA)**. The clinical presentation—**daytime fatigue**, morning headaches, unrefreshing sleep despite adequate sleep duration, and hypertension—strongly suggests OSA.
- While **polysomnography** is the gold standard for confirming OSA, the clinical diagnosis is evident in this case. **Weight loss** is the most important initial therapeutic intervention, as even modest weight reduction (10% of body weight) can significantly improve or resolve OSA in obese patients.
- Weight loss reduces upper airway collapse by decreasing fatty tissue deposition around the pharynx and improving lung volumes. This addresses the underlying pathophysiology rather than just treating symptoms.
- This intervention also addresses his **hypertension** (180/110 mm Hg), which is commonly associated with and exacerbated by OSA.
*Caffeine avoidance*
- While excessive caffeine can disrupt sleep architecture, the patient's symptoms—particularly **morning headaches** and **unrefreshing sleep despite sleeping in**—are not characteristic of caffeine-induced insomnia, which typically presents with difficulty initiating sleep.
- These symptoms, combined with obesity and hypertension, point strongly to a sleep-related breathing disorder rather than a stimulant effect.
*Screening for depression*
- Fatigue is indeed a cardinal symptom of major depressive disorder, but the specific pattern here—**morning headaches** (from nocturnal hypercapnia/hypoxemia), **unrefreshing sleep**, and **obesity with hypertension**—is far more consistent with OSA.
- Depression screening could be considered if symptoms persist after addressing the sleep disorder, as untreated OSA can contribute to or worsen mood disorders.
*Alcohol avoidance in the evening*
- **Alcohol consumption** (2-3 beers daily) does worsen OSA by relaxing upper airway dilator muscles and suppressing arousal responses to hypoxemia. Evening alcohol avoidance would be a beneficial **adjunctive measure**.
- However, while helpful, this intervention is less impactful than weight loss. The patient's **severe obesity** (BMI 39 kg/m²) is the predominant and most modifiable risk factor, making weight loss the priority intervention that will have the greatest effect on reducing OSA severity.
*CT head*
- CT head would be indicated if there were focal neurological deficits, papilledema, or features suggesting increased intracranial pressure or structural brain pathology.
- This patient's **neurological exam is unremarkable**, and his headaches are characteristic of OSA (worse in the morning due to nocturnal CO₂ retention, improving throughout the day). Imaging is not warranted.
Hypertensive nephrosclerosis US Medical PG Question 10: A 63-year-old woman presents to your outpatient clinic complaining of headaches, blurred vision, and fatigue. She has a blood pressure of 171/91 mm Hg and heart rate of 84/min. Physical examination is unremarkable. Her lab results include K+ of 3.1mEq/L and a serum pH of 7.51. Of the following, which is the most likely diagnosis for this patient?
- A. Pheochromocytoma
- B. Renal artery stenosis
- C. Cushing’s syndrome
- D. Primary hyperaldosteronism (Conn’s syndrome) (Correct Answer)
- E. Addison’s disease
Hypertensive nephrosclerosis Explanation: ***Primary hyperaldosteronism (Conn’s syndrome)***
- The combination of **hypertension**, **hypokalemia (K+ 3.1 mEq/L)**, and **metabolic alkalosis (pH 7.51)** is highly characteristic of primary hyperaldosteronism.
- Excess aldosterone leads to increased sodium reabsorption and potassium/hydrogen ion excretion, causing these electrolyte imbalances.
*Pheochromocytoma*
- This condition involves episodic **hypertension**, palpitations, sweating, and anxiety due to catecholamine excess.
- While hypertension is present, the absence of paroxysmal symptoms and the specific electrolyte abnormalities (hypokalemia, alkalosis) make it less likely.
*Renal artery stenosis*
- This can cause **secondary hypertension** and occasionally hypokalemia, but it typically presents with **renal bruits**, and the metabolic alkalosis is not a direct or prominent feature.
- The elevated renin-angiotensin-aldosterone axis would lead to secondary hyperaldosteronism, but primary hyperaldosteronism is suggested by the overall clinical picture.
*Cushing’s syndrome*
- Cushing's syndrome is characterized by **central obesity**, striae, moon facies, and **hyperglycemia**, among other symptoms.
- While hypertension and hypokalemia can occur in severe cases, the predominant clinical features are not aligned with this patient's presentation.
*Addison’s disease*
- This condition is characterized by **adrenal insufficiency**, leading to hypoglycemia, **hyponatremia**, **hyperkalemia**, and **hypotension**.
- The patient's hypertension and hypokalemia directly contradict the typical presentation of Addison’s disease.
More Hypertensive nephrosclerosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.