Glomerulonephritis classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Glomerulonephritis classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Glomerulonephritis classification US Medical PG Question 1: A 21-year-old male presents to your office with hematuria 3 days after the onset of a productive cough and fever. Following renal biopsy, immunofluorescence shows granular IgA deposits in the glomerular mesangium. Which of the following do you suspect in this patient?
- A. Lipoid nephrosis
- B. Berger’s disease (Correct Answer)
- C. HIV infection
- D. Systemic lupus erythematosus
- E. Poststreptococcal glomerulonephritis
Glomerulonephritis classification Explanation: ***Berger’s disease***
- The presentation of **hematuria occurring 3 days after a respiratory infection** (productive cough and fever) is characteristic of **IgA nephropathy** or Berger's disease, showing a synpharyngitic pattern.
- **Immunofluorescence showing granular IgA deposits in the glomerular mesangium** is the histological hallmark of IgA nephropathy.
*Lipoid nephrosis*
- This condition is also known as **minimal change disease** and typically presents with **nephrotic syndrome** (heavy proteinuria, edema, hypoalbuminemia), not primarily hematuria.
- Renal biopsy would reveal **effacement of foot processes** on electron microscopy with normal light microscopy and negative immunofluorescence, unlike the IgA deposits described.
*HIV infection*
- HIV can lead to **HIV-associated nephropathy (HIVAN)**, which typically presents as **focal segmental glomerulosclerosis** (FSGS) and can include proteinuria and progressive renal failure.
- While hematuria can occur, the characteristic **IgA deposits in the mesangium** described are not typical for HIVAN.
*Systemic lupus erythematosus*
- **Lupus nephritis** is a common complication of SLE, and can present with hematuria, proteinuria, and various patterns of glomerulonephritis.
- However, immunofluorescence in lupus nephritis usually shows **IgG, IgM, IgA, C3, and C1q deposits** (full-house staining), not isolated IgA deposits.
*Poststreptococcal glomerulonephritis*
- This condition typically presents with **hematuria 10-14 days after a streptococcal infection** (post-infectious glomerulonephritis), a longer latency period than seen in this patient.
- Immunofluorescence would show unique **"lumpy-bumpy" granular deposits of C3 and IgG** along the glomerular basement membrane, often with characteristic subepithelial humps on electron microscopy, rather than mesangial IgA.
Glomerulonephritis classification US Medical PG Question 2: A 12-year-old boy is brought to an outpatient clinic by his mother, who noticed that her son’s urine has been dark for the past 4 days. She initially attributed this to inadequate hydration, so she monitored her son’s fluid intake and encouraged him to drink more water. However, she noticed that the color of the urine kept getting darker until it began to resemble cola. The boy’s medical history is significant for a sore throat approx. 2 weeks ago, which resolved without medication or treatment. The boy has also been complaining of pain in his ankles, which he first noticed shortly after soccer practice 1 week ago. He has had no pain during urination or urethral discharge, however, and does not have any history of previous episodes of cola-colored urine or passage of blood in the urine. However, the boy has been experiencing intermittent episodes of abdominal pain for the past 3 days. The boy also has wheals on his torso, legs, and buttocks, which his mother attributes to seasonal allergies. Physical examination reveals an alert child who is not in obvious distress but who has a mild conjunctival pallor. Vital signs include: respiratory rate is 22/min, temperature is 36.7°C (98.0°F), and blood pressure is 130/90 mm Hg. Examination of the musculoskeletal system reveals multiple skin lesions (see image). Which of the following laboratory findings is most likely associated with this patient’s clinical presentation?
- A. Elevated level of serum IgA (Correct Answer)
- B. Elevated IgM-IgG immune complex rheumatoid factor
- C. 24-hour urinary protein of more than 4 g
- D. Elevated levels of serum IgG and C3 protein
- E. Low C-reactive protein level
Glomerulonephritis classification Explanation: ***Elevated level of serum IgA***
- The patient's presentation with **cola-colored urine** (hematuria), recent **sore throat**, **abdominal pain**, **arthralgia**, and a **purpuric rash** is highly suggestive of **Henoch-Schönlein purpura (HSP)**, now known as **IgA vasculitis**.
- HSP is characterized by **IgA-dominant immune complex deposition** in small vessels, leading to **elevated serum IgA levels** in 50-90% of cases.
- This is the most specific laboratory finding for this patient's clinical presentation.
*Elevated IgM-IgG immune complex rheumatoid factor*
- **Rheumatoid factor (RF)** is an autoantibody (typically IgM against IgG Fc) primarily associated with **rheumatoid arthritis** and other rheumatologic conditions.
- This patient's symptoms are more consistent with a **small vessel vasculitis** (HSP) rather than rheumatoid arthritis.
- The arthralgia in HSP is due to vasculitis, not synovitis.
*24-hour urinary protein of more than 4 g*
- A **24-hour urinary protein excretion** exceeding 3.5 g/day defines **nephrotic-range proteinuria**.
- While HSP can involve the kidneys (**IgA nephropathy**), the typical presentation features **hematuria with mild-to-moderate proteinuria**.
- Nephrotic-range proteinuria (>4 g/24hr) is uncommon in HSP and less characteristic than elevated serum IgA.
*Elevated levels of serum IgG and C3 protein*
- Elevated serum IgG is a nonspecific marker of immune activation and is not characteristic of HSP.
- **Complement levels (C3, C4) are typically normal in HSP**, as it is not a complement-mediated vasculitis.
- Low C3 levels would suggest **post-streptococcal glomerulonephritis** (low C3, normal C4) or **lupus nephritis** (low C3 and C4), not HSP.
*Low C-reactive protein level*
- **C-reactive protein (CRP)** is an **acute phase reactant** that is typically **elevated** during inflammatory and vasculitic processes, including HSP.
- A **low CRP level** would be inconsistent with the active systemic inflammation indicated by this patient's symptoms (arthralgia, abdominal pain, rash, and renal involvement).
Glomerulonephritis classification US Medical PG Question 3: A 61-year-old man comes to the physician because of progressively worsening swelling of his ankles. He says he has felt exhausted lately. Over the past 3 months, he has gained 5 kg. He has smoked one pack of cigarettes daily for 30 years. His pulse is 75/min and his blood pressure is 140/90 mmHg. Examination shows 2+ pitting edema in the lower extremities. Neurologic exam shows diminished two-point discrimination in the fingers and toes. A urine sample is noted to be foamy. Laboratory studies show a hemoglobin A1c of 7.9% and creatinine of 1.9 mg/dL. A biopsy specimen of the kidney is most likely to show which of the following?
- A. Nodular glomerulosclerosis (Correct Answer)
- B. Wire looping of capillaries
- C. Immune complex deposition
- D. Split glomerular basement membrane
- E. Interstitial inflammation
Glomerulonephritis classification Explanation: ***Nodular glomerulosclerosis***
- The patient's history of **elevated HbA1c (7.9%)**, **pitting edema**, **foamy urine**, and **elevated creatinine (1.9 mg/dL)** strongly indicates **diabetic nephropathy**. Nodular glomerulosclerosis (**Kimmelstiel-Wilson lesions**) is a characteristic pathological finding in advanced diabetic nephropathy.
- The **diminished two-point discrimination** also points to **peripheral neuropathy**, a common complication of diabetes, further supporting the diagnosis of diabetes-related end-organ damage.
*Wire looping of capillaries*
- **Wire looping** of capillaries, along with **subendothelial immune complex deposits**, is characteristic of **diffuse proliferative glomerulonephritis**, often associated with **lupus nephritis (Class III or IV)**.
- While this patient has renal involvement, the clinical picture (diabetes, neuropathy) does not suggest a systemic autoimmune disease like lupus.
*Immune complex deposition*
- **Immune complex deposition** is a general feature of many forms of **glomerulonephritis**, including post-infectious glomerulonephritis or lupus nephritis.
- However, the specific clinical context of uncontrolled diabetes makes **diabetic nephropathy** the most likely cause, which is primarily a metabolic rather than immune-mediated injury.
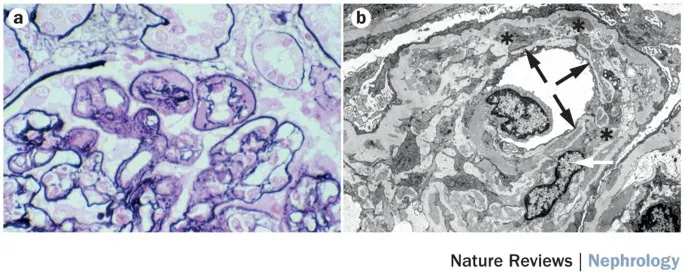
*Split glomerular basement membrane*
- A **split glomerular basement membrane** (often described as duplication or tram-track appearance) is characteristic of **membranoproliferative glomerulonephritis (MPGN)** types I and II.
- This finding is not typically associated with diabetic nephropathy, which involves thickening of the basement membrane and mesangial expansion but not splitting.
*Interstitial inflammation*
- **Interstitial inflammation** is a prominent feature of **interstitial nephritis**, often caused by drug reactions (e.g., NSAIDs, antibiotics) or certain systemic diseases.
- While renal damage in diabetes can lead to some interstitial fibrosis and inflammation, it is not the primary histological hallmark, and the prominent glomerular changes are more specific.
Glomerulonephritis classification US Medical PG Question 4: A 22-year-old man comes to the emergency department because of several episodes of blood in his urine and decreased urine output for 5 days. His blood pressure is 158/94 mm Hg. Examination shows bilateral lower extremity edema. Urinalysis shows 3+ protein and red blood cell casts. Mass spectrometry analysis of the urinary protein detects albumin, transferrin, and IgG. Which of the following best describes this type of proteinuria?
- A. Tubular
- B. Selective glomerular
- C. Nonselective glomerular (Correct Answer)
- D. Postrenal
- E. Overflow
Glomerulonephritis classification Explanation: ***Nonselective glomerular***
- The presence of **albumin**, **transferrin**, and **IgG** indicates a loss of molecular control by the glomerulus, allowing both small and larger proteins to pass.
- This pattern, particularly with significant proteinuria (3+ protein) and **red blood cell casts**, is characteristic of a severe **glomerular injury** leading to nonselective filtration.
*Tubular*
- **Tubular proteinuria** results from impaired reabsorption of low-molecular-weight proteins by the renal tubules, typically due to **tubulointerstitial damage**.
- It would primarily involve smaller proteins like **beta-2 microglobulin** or **retinol-binding protein**, not significant amounts of albumin and IgG.
*Selective glomerular*
- **Selective glomerular proteinuria** involves the loss of smaller proteins, primarily **albumin**, due to damage to the glomerular charge barrier, while larger proteins like IgG are retained.
- The detection of **IgG** in the urine indicates a loss of both charge and size selectivity, ruling out selective proteinuria.
*Postrenal*
- **Postrenal proteinuria** is due to inflammation or bleeding in the urinary tract below the kidneys, such as the ureters, bladder, or urethra.
- It is typically associated with conditions like **urinary tract infections** or **stones** and would not cause the significant systemic symptoms (hypertension, edema) or protein profile seen here.
*Overflow*
- **Overflow proteinuria** occurs when there is an overproduction of low-molecular-weight proteins (e.g., **Bence Jones proteins** in multiple myeloma) that overwhelm the reabsorptive capacity of the tubules.
- This patient presents with **glomerular injury** features (red blood cell casts, hypertension, edema) and the presence of albumin and IgG, not an overproduction of single-type low-molecular-weight proteins.
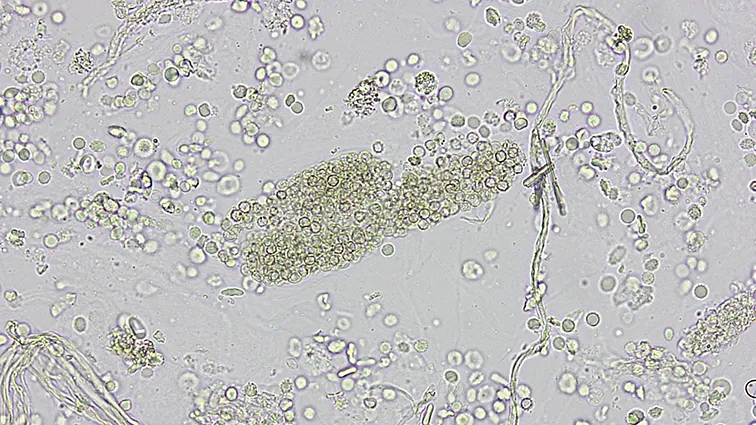
Glomerulonephritis classification US Medical PG Question 5: A 62-year-old man comes to the physician because of fatigue and decreased urine output for 2 weeks. He has not been to the physician for many years and takes no medications. Serum studies show a urea nitrogen concentration of 42 mg/dL and a creatinine concentration of 2.3 mg/dL. Urinalysis shows heavy proteinuria. A photomicrograph of a section of a kidney biopsy specimen is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Amyloidosis
- B. Diabetes mellitus (Correct Answer)
- C. Dyslipidemia
- D. Fibromuscular dysplasia
- E. Severe hypertension
Glomerulonephritis classification Explanation: ***Diabetes mellitus***
- The kidney biopsy shows **diffuse glomerulosclerosis** with **Kimmelstiel-Wilson nodules** (nodular mesangial sclerosis), which are pathognomonic for **diabetic nephropathy**.
- **Heavy proteinuria**, elevated BUN (42 mg/dL) and creatinine (2.3 mg/dL), along with the patient's age, are consistent with long-standing diabetes mellitus, even if previously undiagnosed.
- Diabetic nephropathy is the leading cause of end-stage renal disease in the United States.
*Amyloidosis*
- While amyloidosis can cause nephrotic syndrome and renal failure, the characteristic histology shows **extracellular amorphous deposits** that stain with **Congo red** and demonstrate apple-green birefringence under polarized light.
- The mesangial nodular pattern seen in diabetic nephropathy is distinct from the amyloid deposits seen in amyloidosis.
- Systemic amyloidosis typically presents with other organ involvement such as **cardiomyopathy**, **hepatosplenomegaly**, or **macroglossia**.
*Dyslipidemia*
- **Dyslipidemia** is a common comorbidity of nephrotic syndrome and diabetic nephropathy, but it is not a direct cause of the structural glomerular damage.
- It represents a metabolic consequence rather than the underlying etiology of the renal pathology.
*Fibromuscular dysplasia*
- **Fibromuscular dysplasia** affects the **renal arteries**, causing **renovascular hypertension** and renal ischemia.
- It typically presents with hypertension in young to middle-aged women and an abdominal bruit, not with heavy proteinuria and glomerular nodular sclerosis.
- The histology would show arterial wall changes, not glomerular pathology.
*Severe hypertension*
- **Severe hypertension** causes hypertensive nephrosclerosis with arteriolosclerosis and global glomerulosclerosis, but not the characteristic **nodular mesangial expansion** (Kimmelstiel-Wilson nodules) seen in diabetic nephropathy.
- While hypertension commonly accompanies diabetic nephropathy, the specific histological findings of nodular glomerulosclerosis are pathognomonic for diabetes mellitus.
- Hypertensive nephrosclerosis shows arteriolar hyalinosis and ischemic changes, which differ from diabetic glomerular changes.
Glomerulonephritis classification US Medical PG Question 6: A 47-year-old woman comes to the physician because of a 2-week history of gradually worsening facial and lower extremity swelling. She has had a 4-kg (8.8-lb) weight gain during this time. Her blood pressure is 150/88 mm Hg. Examination shows periorbital edema and 2+ pretibial edema bilaterally. A 24-hour collection of urine shows 4.0 g of proteinuria. Microscopic examination of a kidney biopsy specimen shows thickening of the glomerular basement membrane. Electron microscopy shows dense subepithelial deposits. Further evaluation is most likely to show which of the following?
- A. Anti-myeloperoxidase antibodies
- B. Anti-streptolysin O antibodies
- C. Anti-phospholipase A2 receptor antibodies (Correct Answer)
- D. Anti-C3 convertase antibodies
- E. Anti-collagen type IV antibodies
Glomerulonephritis classification Explanation: ***Anti-phospholipase A2 receptor antibodies***
- This patient's presentation with **nephrotic syndrome** (edema, hypertension, significant proteinuria) and kidney biopsy findings of **thickened glomerular basement membrane** with **subepithelial deposits** points to **membranous nephropathy**.
- **Anti-PLA2R antibodies** are a highly specific and common marker (found in 70-80% of cases) for **primary membranous nephropathy**, which is an autoimmune disease.
*Anti-myeloperoxidase antibodies*
- These antibodies are associated with **ANCA-associated vasculitides**, such as **microscopic polyangiitis** and **eosinophilic granulomatosis with polyangiitis (Churg-Strauss)**.
- These conditions typically present with **rapidly progressive glomerulonephritis** and rarely with isolated nephrotic syndrome or subepithelial deposits.
*Anti-streptolysin O antibodies*
- These antibodies are elevated after a **streptococcal infection** and are associated with **post-streptococcal glomerulonephritis**.
- This disease typically causes **nephritic syndrome** (hematuria, hypertension, mild proteinuria) and on biopsy shows **subepithelial humps** (immune complex deposits), but not a thick basement membrane as the primary finding.
*Anti-C3 convertase antibodies*
- These antibodies are characteristic of **C3 glomerulopathy**, which includes **dense deposit disease** (MPGN type II) and C3 glomerulonephritis.
- While C3 glomerulopathy can cause nephrotic syndrome, the characteristic electron microscopy findings are **intramembranous dense deposits**, not subepithelial deposits, and the primary defect is dysregulation of the alternative complement pathway.
*Anti-collagen type IV antibodies*
- These antibodies are characteristic of **Goodpasture syndrome** (anti-glomerular basement membrane disease).
- This condition typically presents with **rapidly progressive glomerulonephritis** and often **pulmonary hemorrhage**, and biopsy shows **linear deposition of IgG** along the glomerular basement membrane, not subepithelial deposits.
Glomerulonephritis classification US Medical PG Question 7: A 57-year-old woman presents to her family physician because of sinusitis and nasal drainage for 3 months. The nasal drainage is purulent and occasionally hemorrhagic. She has only temporary improvement after trying multiple over the counter medications. Over the last 2 weeks, she also has fatigue and joint pain, mainly affecting the ankles, knees, and wrists. Vital signs include: temperature 36.9°C (98.4°F), blood pressure 142/91 mm Hg, and pulse 82/min. On examination, there is inflammation and bleeding of the nasal mucosa, along with tenderness to percussion over the maxillary sinuses. Urine dipstick reveals 4+ microscopic hematuria and 2+ proteinuria. Which of the following is the most likely diagnosis?
- A. Granulomatosis with polyangiitis (Correct Answer)
- B. Polyarteritis nodosa
- C. Churg-Strauss syndrome
- D. Immunoglobulin A nephropathy
- E. Sarcoidosis
Glomerulonephritis classification Explanation: ***Granulomatosis with polyangiitis***
- This patient presents with **upper airway inflammation** (chronic sinusitis, hemorrhagic purulent nasal drainage, inflamed nasal mucosa), **joint pain**, and **renal involvement** (hematuria, proteinuria), which are classic features of granulomatosis with polyangiitis (GPA), formerly known as Wegener's granulomatosis.
- GPA is a **small vessel vasculitis** often associated with **ANCA** (specifically PR3-ANCA/c-ANCA) and characterized by granulomatous inflammation of the respiratory tract and glomerulonephritis.
*Polyarteritis nodosa*
- **Polyarteritis nodosa (PAN)** typically involves **medium-sized arteries** and presents with systemic symptoms, but it **spares the lungs** and **kidneys initially**, unlike the prominent renal and upper respiratory manifestations seen here.
- PAN is **not associated with ANCA** and does not typically involve the upper respiratory tract with granulomatous inflammation.
*Churg-Strauss syndrome*
- Also known as **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**, this condition is characterized by **asthma**, **eosinophilia**, and **allergic rhinitis**, which are not the primary features in this patient.
- While it can involve the upper respiratory tract and kidneys, the absence of **asthma** and **high eosinophil count** makes it less likely.
*Immunoglobulin A nephropathy*
- This is a **primary glomerular disease** characterized by **IgA deposition** in the mesangium, presenting often with recurrent macroscopic hematuria following an upper respiratory or gastrointestinal infection.
- It does **not cause systemic vasculitis** with prominent upper airway inflammation, granulomas, or destructive sinusitis.
*Sarcoidosis*
- **Sarcoidosis** is a multi-system granulomatous disease, often affecting the lungs and lymph nodes, and sometimes the skin, eyes, and joints.
- While it can cause some nasal symptoms, it generally **does not cause destructive sinonasal disease** with purulent and hemorrhagic drainage or severe glomerulonephritis with 4+ hematuria, and it is **not a vasculitis**.
Glomerulonephritis classification US Medical PG Question 8: A 62-year-old man presents to the emergency department with hematuria and hemoptysis that started in the morning. He notes that he has had frequent lung infections throughout his adult life, the most recent being 2 weeks ago. He also mentions that he has had hematuria twice before but never as severe as he is having currently. His medical history is otherwise non-significant, and his only medication is acetaminophen as needed. His blood pressure is 136/92 mm Hg, heart rate is 86/min, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). Chest radiography shows a resolving right middle lobe airspace opacity. His initial laboratory tests are notable for elevated erythrocyte sedimentation rate and C-reactive protein level. While in the examination room, the patient develops a spontaneous nosebleed. What is the most likely diagnosis?
- A. Goodpasture syndrome
- B. IgA nephropathy
- C. Minimal change disease
- D. Post-streptococcal glomerulonephritis
- E. Granulomatosis with polyangiitis (Correct Answer)
Glomerulonephritis classification Explanation: ***Granulomatosis with polyangiitis***
- This patient presents with a **triad of upper airway (nosebleed), lower airway (hemoptysis, recurrent lung infections), and renal involvement (hematuria)**, which is classic for granulomatosis with polyangiitis (GPA), a form of ANCA-associated vasculitis.
- The elevated **ESR and CRP** indicate systemic inflammation, which is common in vasculitic conditions.
*Goodpasture syndrome*
- Characterized by **glomerulonephritis and pulmonary hemorrhage (hemoptysis)**, but typically does not involve the upper airways (e.g., nosebleeds).
- Diagnosis is confirmed by the presence of **anti-glomerular basement membrane antibodies**, which often presents more acutely.
*IgA nephropathy*
- Often presents with **recurrent episodes of gross hematuria**, frequently following an upper respiratory tract infection.
- While it involves the kidneys, it **does not typically cause pulmonary or upper airway symptoms** such as hemoptysis or recurrent lung opacities.
*Minimal change disease*
- Characterized by **nephrotic syndrome (proteinuria, hypoalbuminemia, edema)** and rarely presents with hematuria.
- **Does not cause pulmonary or upper airway manifestations** like hemoptysis or nosebleeds.
*Post-streptococcal glomerulonephritis*
- Typically occurs **1-3 weeks after a streptococcal infection** and presents with acute nephritic syndrome (hematuria, proteinuria, edema, hypertension).
- **Does not involve recurrent lung infections or hemoptysis** and is less likely in an adult with recurrent hematuria episodes.
Glomerulonephritis classification US Medical PG Question 9: A 50-year-old woman comes to the emergency department because of fever and productive cough with blood in the sputum for 1 day. She also reports a sharp pain under her ribs that is worsened on taking deep breaths. Over the past 2 years, she has had repeated episodes of sinusitis, for which she used over the counter medication. She has recently started a new job at a wire-mesh factory. Her temperature is 38.3°C (100.9 °F), pulse is 72/min, respirations are 16/min, and blood pressure is 120/80 mm Hg. Physical examination shows palpable nonblanching skin lesions over her hands and feet. Examination of the nasal cavity shows ulcerations of the nasopharyngeal mucosa and a small septal perforation. Pulmonary examination shows stridor on inspiration. Laboratory studies show:
Hemoglobin 13.2 g/dL
Leukocyte count 10,300/mm3
Platelet count 205,000/mm3
Serum
Urea nitrogen 24 mg/dL
Creatinine 2.4 mg/dL
Urine
Protein 2+
RBC 70/hpf
RBC casts numerous
WBC 1–2/hpf
A chest x-ray shows multiple cavitating, nodular lesions bilaterally. Which of the following additional findings is most likely to be present in this patient?
- A. Increased p-ANCA titers
- B. Increased anti-Smith titers
- C. Increased anti-GBM titers
- D. Increased c-ANCA titers (Correct Answer)
- E. Decreased ADAMTS13 activity
Glomerulonephritis classification Explanation: ### ***Increased c-ANCA titers***
- The patient's presentation with **sinusitis**, **nasal ulcerations**, **pulmonary cavitating nodules** with hemoptysis, and **rapidly progressive glomerulonephritis** (elevated creatinine, proteinuria, RBC casts) is highly indicative of **Granulomatosis with Polyangiitis (GPA)**.
- **c-ANCA (cytoplasmic antineutrophil cytoplasmic antibodies)**, primarily targeting **proteinase 3 (PR3)**, are serological markers commonly elevated in GPA and help confirm the diagnosis.
### *Increased p-ANCA titers*
- **p-ANCA (perinuclear antineutrophil cytoplasmic antibodies)**, typically targeting **myeloperoxidase (MPO)**, are more commonly associated with **microscopic polyangiitis** or **eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)**.
- While both GPA and microscopic polyangiitis can present with kidney and lung involvement, the prominent upper airway disease (sinusitis, nasal ulcerations, septal perforation) in this patient points more strongly towards GPA and c-ANCA positivity.
### *Increased anti-Smith titers*
- **Anti-Smith antibodies** are highly specific for **Systemic Lupus Erythematosus (SLE)**.
- The clinical presentation of **upper airway destruction**, **cavitating lung lesions**, and **glomerulonephritis with RBC casts** is not typical for SLE, which more commonly presents with malar rash, arthritis, serositis, and other systemic symptoms.
### *Increased anti-GBM titers*
- **Anti-GBM (anti-glomerular basement membrane) antibodies** are characteristic of **Goodpasture syndrome**, which causes a **rapidly progressive glomerulonephritis** and often **pulmonary hemorrhage**.
- However, Goodpasture syndrome does not typically involve **upper airway disease** (sinusitis, nasal ulcerations, septal perforation) or **palpable skin lesions**, which are prominent features in this patient.
### *Decreased ADAMTS13 activity*
- **Decreased ADAMTS13 activity** is diagnostic of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is characterized by the pentad of **thrombocytopenia**, **microangiopathic hemolytic anemia**, **neurological symptoms**, **renal insufficiency**, and **fever**, but it does not involve the prominent **destructive upper airway disease** or **cavitating lung lesions** seen in this patient.
Glomerulonephritis classification US Medical PG Question 10: A 12-year-old boy presents with a 3-day history of frothy brown urine. He does not complain of any other symptoms. He notes that 3 weeks ago he had a fever with a sore throat, but he did not receive any treatment at the time. His blood pressure is 152/94 mm Hg, heart rate is 72/min, respiratory rate is 15/min, and temperature is 37.0°C (98.6°F). Review of his medical record shows that his blood pressure was 118/74 mm Hg just 4 weeks ago. Laboratory analysis reveals elevated serum creatinine, hematuria with RBC casts, and elevated urine protein without frank proteinuria. What laboratory test can confirm the most likely diagnosis in this patient?
- A. Antistreptolysin O (ASO) titer (Correct Answer)
- B. Urine Gram stain
- C. Urine electrolytes
- D. Stool sample
- E. Urine catecholamine assessment
Glomerulonephritis classification Explanation: ***Antistreptolysin O (ASO) titer***
- A 3-week history of a sore throat followed by frothy brown urine, **hematuria with RBC casts**, and **hypertension** in a 12-year-old boy is highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- An elevated **ASO titer** indicates recent exposure to *Streptococcus pyogenes*, the causative agent of PSGN, confirming the diagnosis.
*Urine Gram stain*
- This test is used to detect bacterial infections in the urinary tract, which typically present with symptoms like **dysuria, frequency, and fever**, and often show bacteriuria rather than hematuria with RBC casts.
- While a urinary tract infection can cause hematuria, the presence of **RBC casts** and the preceding sore throat point away from a simple bacterial UTI.
*Urine electrolytes*
- While renal dysfunction can affect electrolyte balance, **urine electrolytes** are not a primary diagnostic tool for glomerulonephritis like PSGN.
- This test is more useful for assessing **fluid balance disorders** or specific tubular dysfunctions.
*Stool sample*
- A **stool sample** is primarily used to diagnose gastrointestinal infections or conditions affecting the bowel.
- There is no clinical indication in this patient's presentation (sore throat, frothy brown urine, hypertension, hematuria with RBC casts) that would suggest a gastrointestinal pathology as the cause of his renal symptoms.
*Urine catecholamine assessment*
- This test is used to screen for **pheochromocytoma**, a rare tumor of the adrenal glands that can cause hypertension.
- While the patient has new-onset hypertension, the history of a preceding sore throat and the presence of **hematuria with RBC casts** strongly argue against pheochromocytoma as the primary diagnosis.
More Glomerulonephritis classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.