Diabetic nephropathy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diabetic nephropathy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diabetic nephropathy US Medical PG Question 1: A 52-year-old man comes to the physician for a routine health maintenance examination. He feels well. His blood pressure is 125/70 mm Hg. His glomerular filtration rate is calculated to be 105 mL/min/1.73 m2 and glucose clearance is calculated to be 103 mL/min. This patient is most likely being treated with which of the following agents?
- A. Ifosfamide
- B. Acarbose
- C. Canagliflozin (Correct Answer)
- D. Glipizide
- E. Metformin
Diabetic nephropathy Explanation: ***Canagliflozin***
- The key finding is that **glucose clearance (103 mL/min) approximately equals GFR (105 mL/min)**, indicating nearly complete failure of glucose reabsorption.
- **Canagliflozin** is an **SGLT2 inhibitor** that blocks the sodium-glucose cotransporter 2 in the proximal tubule, preventing glucose reabsorption.
- This causes filtered glucose to be excreted in urine, resulting in **glucose clearance approaching GFR** - exactly what is seen in this patient.
- SGLT2 inhibitors are increasingly used as first-line agents in Type 2 Diabetes, especially with cardiovascular or renal benefits.
*Metformin*
- **Metformin** is a biguanide that decreases hepatic gluconeogenesis and increases peripheral insulin sensitivity.
- It does **NOT affect renal glucose handling** or glucose clearance, which would remain near zero in patients on metformin.
- The elevated glucose clearance in this patient rules out metformin monotherapy.
*Ifosfamide*
- **Ifosfamide** is an alkylating chemotherapy agent used for cancer treatment, not diabetes management.
- It can cause **Fanconi syndrome** (proximal tubule dysfunction) leading to glycosuria, but this would also cause decreased GFR, proteinuria, and electrolyte abnormalities.
- This patient's normal GFR and otherwise normal presentation makes ifosfamide-induced toxicity unlikely.
*Acarbose*
- **Acarbose** is an alpha-glucosidase inhibitor that slows carbohydrate absorption in the intestine.
- It works in the **GI tract**, not the kidneys, and does not affect glucose clearance.
- It would not explain the elevated renal glucose excretion seen here.
*Glipizide*
- **Glipizide** is a sulfonylurea that stimulates pancreatic insulin release.
- It does **NOT affect renal glucose handling** and would not cause elevated glucose clearance.
- The patient's glucose clearance pattern is inconsistent with sulfonylurea therapy.
Diabetic nephropathy US Medical PG Question 2: A 62-year-old woman with type 2 diabetes mellitus comes to the physician because of a 3-month history of fatigue and weakness. Her hemoglobin A1c concentration was 13.5% 12 weeks ago. Her blood pressure is 152/92 mm Hg. Examination shows lower extremity edema. Serum studies show:
K+ 5.1 mEq/L
Phosphorus 5.0 mg/dL
Ca2+ 7.8 mg/dL
Urea nitrogen 60 mg/dL
Creatinine 2.2 mg/dL
Which of the following is the best parameter for early detection of this patient’s renal condition?
- A. Serum total protein
- B. Serum creatinine
- C. Urinary red blood cell casts
- D. Serum urea nitrogen
- E. Urinary albumin (Correct Answer)
Diabetic nephropathy Explanation: ***Urinary albumin***
- **Microalbuminuria** is often the earliest detectable sign of **diabetic nephropathy**, occurring before changes in GFR or serum creatinine become apparent.
- Regular screening for urinary albumin in diabetic patients allows for early intervention to slow the progression of **renal damage**.
*Serum total protein*
- **Hypoalbuminemia** can be seen in advanced renal disease due to significant proteinuria, but it is not an early marker.
- Other conditions like **liver disease** or **malnutrition** can also cause altered serum total protein, making it less specific for early renal damage.
*Serum creatinine*
- **Serum creatinine** levels rise significantly only after a substantial portion of kidney function (around 50%) has been lost.
- Therefore, it is a marker of established renal dysfunction rather than an early indicator.
*Urinary red blood cell casts*
- The presence of **red blood cell casts** in urine indicates **glomerulonephritis** or other inflammatory conditions affecting the glomeruli.
- While concerning, it is not the typical or earliest presentation of **diabetic nephropathy**, which primarily involves proteinuria.
*Serum urea nitrogen*
- **Blood urea nitrogen (BUN)** levels, like creatinine, increase with declining kidney function and are used to assess the severity of **renal impairment**.
- However, BUN levels can also be influenced by factors like **hydration status** and **protein intake**, and they are not an early marker of nascent renal disease.
Diabetic nephropathy US Medical PG Question 3: A 44-year-old man presents for a checkup. The patient says he has to urinate quite frequently but denies any dysuria or pain on urination. Past medical history is significant for diabetes mellitus type 2 and hypertension, both managed medically, as well as a chronic mild cough for the past several years. Current medications are metformin, aspirin, rosuvastatin, captopril, and furosemide. His vital signs are an irregular pulse of 74/min, a respiratory rate of 14/min, a blood pressure of 130/80 mm Hg, and a temperature of 36.7°C (98.0°F). His BMI is 32 kg/m2. On physical examination, there are visible jugular pulsations present in the neck bilaterally. Laboratory findings are significant for the following:
Glycated Hemoglobin (Hb A1c) 7.5%
Fasting Blood Glucose 120 mg/dL
Serum Electrolytes
Sodium 138 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum Creatinine 1.3 mg/dL
Blood Urea Nitrogen 18 mg/dL
Which of the following is the next best step in the management of this patient?
- A. Replace captopril with valsartan.
- B. Stop furosemide.
- C. Stop metformin.
- D. Start rosiglitazone.
- E. Start exenatide. (Correct Answer)
Diabetic nephropathy Explanation: ***Correct: Start exenatide.***
* The patient has **diabetes mellitus type 2** with an **HbA1c of 7.5%**, indicating suboptimal glycemic control despite being on metformin. Exenatide, a **GLP-1 receptor agonist**, helps improve glycemic control by increasing insulin secretion, decreasing glucagon secretion, and slowing gastric emptying.
* Given his BMI of **32 kg/m²**, exenatide is particularly beneficial as it also promotes **weight loss**, addressing an important comorbidity.
*Incorrect: Replace captopril with valsartan.*
* The patient is currently on captopril, an **ACE inhibitor**, for hypertension. Replacing it with valsartan, an **ARB**, is generally considered if the patient develops an ACE inhibitor-induced cough or angioedema.
* While the patient has a chronic cough, it's been present for several years, making a **long-standing smoker's cough or COPD more likely** than an ACE-inhibitor-induced cough, which usually resolves within a few weeks of stopping the drug. His blood pressure and renal function are stable on captopril.
*Incorrect: Stop furosemide.*
* The presence of **visible jugular pulsations** in the neck suggests **elevated central venous pressure**, which could indicate **fluid overload** or heart failure. Stopping a diuretic like furosemide in this context would likely worsen fluid retention.
* Furosemide is currently helping to manage the patient's fluid status, and discontinuing it could lead to **decompensation**, especially given the potential cardiac involvement hinted at by the jugular pulsations and irregular pulse.
*Incorrect: Stop metformin.*
* The patient's **HbA1c of 7.5%** indicates that his diabetes is **not well-controlled** on metformin alone, but this does not warrant stopping metformin, which is a first-line agent.
* Metformin should only be stopped in cases of severe renal impairment (eGFR <30 mL/min/1.73m²), which is not indicated by his **creatinine of 1.3 mg/dL**, or other contraindications such as metabolic acidosis.
*Incorrect: Start rosiglitazone.*
* Rosiglitazone is a **thiazolidinedione (TZD)** that can improve insulin sensitivity and lower blood glucose. However, it is associated with side effects such as **weight gain** and **fluid retention**, which would be undesirable in this patient given his obesity and potential signs of fluid overload (jugular pulsations).
* Additionally, TZDs have been linked to an increased risk of **congestive heart failure**, a concern given his irregular pulse and jugular pulsations suggesting potential cardiac issues.
Diabetic nephropathy US Medical PG Question 4: A 67-year-old man presents to his primary care provider because of fatigue and loss of appetite. He is also concerned that his legs are swollen below the knee. He has had type 2 diabetes for 35 years, for which he takes metformin and glyburide. Today his temperature is 36.5°C (97.7°F), the blood pressure is 165/82 mm Hg, and the pulse is 88/min. Presence of which of the following would make diabetic kidney disease less likely in this patient?
- A. Normal-to-large kidneys on ultrasound
- B. Gradual reduction of glomerular filtration rate (GFR)
- C. Diabetic retinopathy
- D. Nephrotic range proteinuria
- E. Cellular casts in urinalysis (Correct Answer)
Diabetic nephropathy Explanation: ***Cellular casts in urinalysis***
- The presence of **cellular casts**, especially **red blood cell casts** or **white blood cell casts**, suggests an active glomerular inflammatory disease (e.g., glomerulonephritis) or an interstitial nephritis, which are atypical for uncomplicated diabetic kidney disease.
- Diabetic kidney disease typically presents with bland urine sediment without significant cellular casts.
*Normal-to-large kidneys on ultrasound*
- In the early stages of diabetic kidney disease, the kidneys can be **normal in size or even enlarged** due to compensatory hypertrophy and increased renal blood flow.
- Only in **advanced stages** of chronic kidney disease from diabetes do the kidneys become atrophic and shrunken.
*Gradual reduction of glomerular filtration rate (GFR)*
- Diabetic kidney disease is characterized by a **progressive decline in GFR** over time, often correlating with the duration and control of diabetes.
- This gradual decline is a hallmark differentiating it from acute kidney injury or rapidly progressive glomerulonephritis.
*Diabetic retinopathy*
- The presence of **diabetic retinopathy** is a strong indicator of **microvascular complications** of diabetes and is highly correlated with the presence and severity of diabetic kidney disease.
- This co-occurrence supports a diagnosis of diabetic kidney disease, not ruling it out.
*Nephrotic range proteinuria*
- **Nephrotic range proteinuria** (protein excretion > 3.5 g/day) is a common manifestation of diabetic kidney disease, especially as the disease progresses to more advanced stages.
- This level of proteinuria suggests significant glomerular damage, consistent with diabetic nephropathy.
Diabetic nephropathy US Medical PG Question 5: A 51-year-old African American man presents to his primary care physician’s office for an annual visit. He has no major concerns and says that he has been healthy for the last year. His past medical history is significant for diabetes as well as long standing hypertension that has developed gradually since his 30's; however, he has refused to take any medications. Physical exam shows no abnormal findings. Routine laboratory testing reveals the following:
Serum creatinine concentration: 1.5 mg/dL
Blood urea nitrogen: 31 mg/dL
Based on these results, urine studies are conducted that reveal mild proteinuria of less than 1 g/day and no casts.
Which of the following is most likely associated with the cause of this patient's elevated creatinine?
- A. String of beads on angiography
- B. Kimmelstiel-Wilson lesions (Correct Answer)
- C. Apple-green birefringent lesions
- D. Renal cortex necrosis
- E. Flea-bitten kidney
Diabetic nephropathy Explanation: **Kimmelstiel-Wilson lesions**
- The patient has a history of long-standing diabetes and hypertension, which are the primary risk factors for **diabetic nephropathy**.
- **Kimmelstiel-Wilson lesions** are nodular glomerulosclerosis pathognomonic for **diabetic nephropathy**, characterized by hyaline nodules in the mesangium.
- This is the most likely cause given the combination of diabetes, mild proteinuria (<1 g/day), and chronic renal insufficiency.
*String of beads on angiography*
- This finding is characteristic of **fibromuscular dysplasia**, a non-inflammatory vascular disease that can cause **renal artery stenosis**.
- While renal artery stenosis can cause hypertension and renal impairment, the patient's long-standing diabetes and gradual progression make diabetic nephropathy a more probable cause.
*Apple-green birefringent lesions*
- This describes the characteristic staining of **amyloid deposits** with **Congo red stain** under polarized light.
- While amyloidosis can cause renal failure with proteinuria, it is less common than diabetic nephropathy in a patient with long-standing diabetes and the typical presentation described.
*Renal cortex necrosis*
- This is a rare and severe form of **acute kidney injury** often associated with conditions like severe sepsis, obstetric complications, or disseminated intravascular coagulation.
- The patient's history of gradual onset hypertension and diabetes, along with mild proteinuria and elevated creatinine, points to a chronic rather than acute process.
*Flea-bitten kidney*
- This describes the gross appearance of kidneys in **malignant hypertension**, showing petechial hemorrhages on the renal surface.
- While the patient has long-standing hypertension, the presentation suggests chronic kidney disease from diabetic nephropathy rather than acute malignant hypertension, which would present with markedly elevated blood pressure and acute kidney injury.
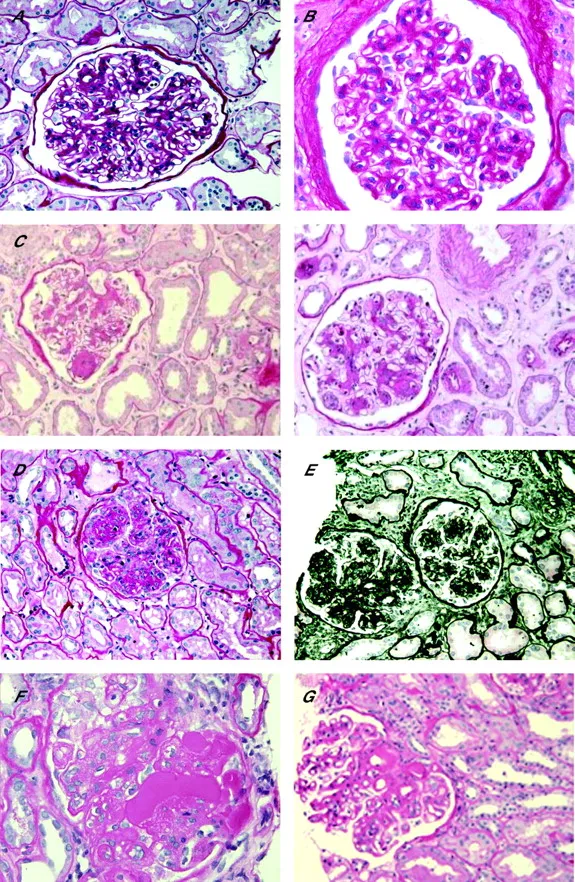
Diabetic nephropathy US Medical PG Question 6: A 62-year-old man comes to the physician because of fatigue and decreased urine output for 2 weeks. He has not been to the physician for many years and takes no medications. Serum studies show a urea nitrogen concentration of 42 mg/dL and a creatinine concentration of 2.3 mg/dL. Urinalysis shows heavy proteinuria. A photomicrograph of a section of a kidney biopsy specimen is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Amyloidosis
- B. Diabetes mellitus (Correct Answer)
- C. Dyslipidemia
- D. Fibromuscular dysplasia
- E. Severe hypertension
Diabetic nephropathy Explanation: ***Diabetes mellitus***
- The kidney biopsy shows **diffuse glomerulosclerosis** with **Kimmelstiel-Wilson nodules** (nodular mesangial sclerosis), which are pathognomonic for **diabetic nephropathy**.
- **Heavy proteinuria**, elevated BUN (42 mg/dL) and creatinine (2.3 mg/dL), along with the patient's age, are consistent with long-standing diabetes mellitus, even if previously undiagnosed.
- Diabetic nephropathy is the leading cause of end-stage renal disease in the United States.
*Amyloidosis*
- While amyloidosis can cause nephrotic syndrome and renal failure, the characteristic histology shows **extracellular amorphous deposits** that stain with **Congo red** and demonstrate apple-green birefringence under polarized light.
- The mesangial nodular pattern seen in diabetic nephropathy is distinct from the amyloid deposits seen in amyloidosis.
- Systemic amyloidosis typically presents with other organ involvement such as **cardiomyopathy**, **hepatosplenomegaly**, or **macroglossia**.
*Dyslipidemia*
- **Dyslipidemia** is a common comorbidity of nephrotic syndrome and diabetic nephropathy, but it is not a direct cause of the structural glomerular damage.
- It represents a metabolic consequence rather than the underlying etiology of the renal pathology.
*Fibromuscular dysplasia*
- **Fibromuscular dysplasia** affects the **renal arteries**, causing **renovascular hypertension** and renal ischemia.
- It typically presents with hypertension in young to middle-aged women and an abdominal bruit, not with heavy proteinuria and glomerular nodular sclerosis.
- The histology would show arterial wall changes, not glomerular pathology.
*Severe hypertension*
- **Severe hypertension** causes hypertensive nephrosclerosis with arteriolosclerosis and global glomerulosclerosis, but not the characteristic **nodular mesangial expansion** (Kimmelstiel-Wilson nodules) seen in diabetic nephropathy.
- While hypertension commonly accompanies diabetic nephropathy, the specific histological findings of nodular glomerulosclerosis are pathognomonic for diabetes mellitus.
- Hypertensive nephrosclerosis shows arteriolar hyalinosis and ischemic changes, which differ from diabetic glomerular changes.
Diabetic nephropathy US Medical PG Question 7: A 76-year-old woman comes in for a routine checkup with her doctor. She is concerned that she feels tired most days and has difficulty doing her household chores. She complains that she gets fatigued and breathless with mild exertion. Past medical history is significant for diabetes mellitus, chronic kidney disease from prolonged elevated blood sugar, and primary biliary cirrhosis. Medications include lisinopril, insulin, and metformin. Family medicine is noncontributory. She drinks one beer every day. Today, she has a heart rate of 98/min, respiratory rate of 17/min, blood pressure of 110/65 mm Hg, and a temperature of 37.0°C (98.6°F). General examination shows that she is pale and haggard looking. She has a heartbeat with a regular rate and rhythm and her lungs are clear to auscultation bilaterally. A complete blood count (CBC) is as follows:
Leukocyte count: 12,000/mm3
Red blood cell count: 3.1 million/mm3
Hemoglobin: 11.0 g/dL
MCV: 85 fL
MCH: 27 pg/cell
Platelet count: 450,000/mm3
Fecal occult blood test is negative. What is the most likely cause of her anemia?
- A. Chronic kidney disease (Correct Answer)
- B. Acute bleeding
- C. Alcoholism
- D. Liver disease
- E. Colorectal cancer
Diabetic nephropathy Explanation: ***Chronic kidney disease***
- **Chronic kidney disease (CKD)** is a common cause of **normocytic, normochromic anemia** due to decreased production of **erythropoietin** by the kidneys.
- This patient's history of CKD, alongside her **normocytic anemia (MCV 85 fL)**, makes this the most likely cause.
*Acute bleeding*
- Acute bleeding would typically present with signs of **hypovolemia** (e.g., hypotension, tachycardia) and potentially a **reticulocytosis** as the bone marrow compensates, neither of which are seen here.
- The **negative fecal occult blood test** and stable vital signs also argue against acute or chronic gastrointestinal bleeding.
*Alcoholism*
- Chronic alcoholism can lead to anemia, often **macrocytic** due to **folate deficiency**, or less commonly microcytic if associated with iron deficiency from GI bleeding.
- While she drinks one beer daily, this amount is unlikely to directly cause significant anemia, especially given her **normocytic MCV**.
*Liver disease*
- **Primary biliary cirrhosis (PBC)** can cause anemia through various mechanisms, including **hemolysis**, **folate deficiency**, or bleeding from **portal hypertension**.
- However, PBC-related anemia is often microcytic or macrocytic, and her **normocytic MCV** and the more direct link to CKD make it less likely to be the primary cause.
*Colorectal cancer*
- **Colorectal cancer** can cause anemia due to **chronic blood loss**, which would typically lead to **iron deficiency anemia** (microcytic anemia).
- The patient has a **normocytic anemia (MCV 85 fL)** and a **negative fecal occult blood test**, making this diagnosis highly unlikely.
Diabetic nephropathy US Medical PG Question 8: A 55-year-old Caucasian woman visits her family physician for a checkup and to discuss her laboratory results from a previous visit. The medical history is significant for obesity, hypothyroidism, and chronic venous insufficiency. The medications include thyroxine and a multivitamin. In her previous visit, she complained about being hungry all the time, urinating multiple times a day, and craving water for most of the day. Blood and urine samples were obtained. Today her blood pressure is 120/70 mm Hg, the pulse is 80/min, the respiratory rate is 18/min, and the body temperature is 36.4°C (97.5°F). The physical examination reveals clear lungs with regular heart sounds and no abdominal tenderness. There is mild pitting edema of the bilateral lower extremities. The laboratory results are as follows:
Elevated SCr for an eGFR of 60 mL/min/1.73 m²
Spot urine albumin-to-creatinine ratio 250 mg/g
Urinalysis
Specific gravity 1.070
Proteins (++)
Glucose (+++)
Nitrites (-)
Microscopy
Red blood cells none
White blood cells none
Hyaline casts few
A bedside renal ultrasound revealed enlarged kidneys bilaterally without hydronephrosis. Which of the following kidney-related test should be ordered next?
- A. Renal computed tomography
- B. No further renal tests are required
- C. Urine protein electrophoresis (Correct Answer)
- D. Renal arteriography
- E. Renal biopsy
Diabetic nephropathy Explanation: ***Urine protein electrophoresis***
- The patient's symptoms (polyuria, polydipsia, hunger) along with **significant proteinuria** (++ on urinalysis, **albumin-to-creatinine ratio of 250 mg/g**) and **glucosuria** (+++) suggest possible **diabetes mellitus** and associated **diabetic nephropathy**.
- While diabetic nephropathy is likely, other proteinuric kidney diseases, such as **monoclonal gammopathy** (e.g., related to multiple myeloma), can also present with proteinuria and enlarged kidneys. Urine protein electrophoresis helps to **differentiate albuminuria from other proteinurias**, such as light chains, which is crucial for diagnosis and treatment.
*Renal computed tomography*
- This imaging study would be considered if there was suspicion of **renal masses**, stones, or other structural abnormalities not clearly defined by ultrasound, or if **hydronephrosis** was present, which is not the case here.
- Given the primary concern is proteinuria with symptoms suggestive of diabetes, a CT scan is not the most immediate next step for characterizing the type of proteinuria.
*No further renal tests are required*
- This is incorrect because the patient has significant proteinuria and symptoms suggesting a systemic disease that involves the kidneys, requiring further investigation to **confirm the etiology of the kidney damage** and guide management.
- The elevated specific gravity, proteinuria, and glucosuria, along with enlarged kidneys, warrant **further diagnostic workup** beyond an eGFR and ACR.
*Renal arteriography*
- This invasive procedure is used to visualize the **renal arteries** and assess for conditions like **renal artery stenosis** or vasculitis.
- There is no clinical indication (e.g., uncontrolled hypertension despite medication, abdominal bruits, flash pulmonary edema) to suggest renal artery stenosis, and the current presentation points toward a primary glomerular issue.
*Renal biopsy*
- While a **renal biopsy** might eventually be necessary, it is an **invasive procedure** and usually performed after less invasive tests (like urine protein electrophoresis) have been conducted and if the diagnosis remains unclear or if there's a need for precise histological classification, especially if non-diabetic kidney disease is suspected.
- In this case, characterizing the type of proteinuria is important first, as **diabetic nephropathy** can often be diagnosed clinically without a biopsy if typical features are present and other causes are ruled out.
Diabetic nephropathy US Medical PG Question 9: A 75-year-old man presents to his primary care physician for foot pain. The patient states that he has had chronic foot pain, which has finally caused him to come and see the doctor. The patient's past medical history is unknown and he has not seen a doctor in over 50 years. The patient states he has led a healthy lifestyle, consumes a plant-based diet, exercised regularly, and avoided smoking, thus his lack of checkups with a physician. The patient lives alone as his wife died recently. His temperature is 98.1°F (36.7°C), blood pressure is 128/64 mmHg, pulse is 80/min, respirations are 13/min, and oxygen saturation is 98% on room air. The patient's BMI is 19 kg/m^2 and he appears healthy. Physical exam demonstrates a right foot that is diffusely swollen, mildly tender, and deformed. The patient's gait is abnormal. Which of the following is associated with the underlying cause of this patient's presentation?
- A. Methicillin-resistant bacterial agent
- B. Unprotected sexual intercourse
- C. Megaloblastic anemia
- D. High-impact trauma to the foot
- E. Hyperfiltration damage of the kidney (Correct Answer)
Diabetic nephropathy Explanation: ***Hyperfiltration damage of the kidney***
- The patient's presentation of a **deformed and diffusely swollen, mildly tender foot** in a 75-year-old, alongside his self-reported healthy lifestyle (plant-based diet, exercise), points toward **Charcot arthropathy (diabetic foot)**, which is typically a complication of **diabetes mellitus**.
- **Hyperfiltration damage of the kidney** is a key early sign of **diabetic nephropathy**, occurring during stages 1 and 2, where the kidneys compensate for damage by increasing the glomerular filtration rate, eventually leading to proteinuria and chronic kidney disease. This is a common association with long-standing, undiagnosed diabetes.
*Methicillin-resistant bacterial agent*
- This typically causes **acute infections**, often with signs of severe inflammation, warmth, erythema, and possibly purulence. The patient's presentation is of **chronic foot pain** and **deformity**, less suggestive of an acute bacterial infection.
- While foot ulcers related to diabetes can become infected with MRSA, the primary underlying cause of the foot deformity and pain is not MRSA itself, but rather the neuropathic and vascular complications of diabetes.
*Unprotected sexual intercourse*
- **Unprotected sexual intercourse** is a risk factor for sexually transmitted infections (STIs) and their sequelae, such as **reactive arthritis**.
- Reactive arthritis typically presents with acute, asymmetric oligoarthritis, often affecting the lower extremities, and usually has associated urethritis or conjunctivitis, which are not mentioned in this chronic, deforming condition.
*Megaloblastic anemia*
- **Megaloblastic anemia** is primarily caused by **vitamin B12 or folate deficiency** and can lead to neurological symptoms like **peripheral neuropathy** (e.g., paresthesias, gait disturbance).
- While peripheral neuropathy can contribute to foot problems, megaloblastic anemia itself does not directly cause the severe **bone and joint destruction** seen in Charcot arthropathy; it's a consequence of diabetic neuropathy.
*High-impact trauma to the foot*
- **High-impact trauma** can cause fractures, dislocations, or acute soft tissue injuries to the foot, leading to pain and swelling.
- However, the patient's presentation is of **chronic pain and progressive deformity**, indicating a degenerative process rather than an acute traumatic injury. While trauma can exacerbate Charcot foot, it's not the underlying cause.
Diabetic nephropathy US Medical PG Question 10: A 42-year-old man comes to the physician because of a 2-month history of fatigue and increased urination. The patient reports that he has been drinking more than usual because he is constantly thirsty. He has avoided driving for the past 8 weeks because of intermittent episodes of blurred vision. He had elevated blood pressure at his previous visit but is otherwise healthy. Because of his busy work schedule, his diet consists primarily of fast food. He does not smoke or drink alcohol. He is 178 cm (5 ft 10 in) tall and weighs 109 kg (240 lb); BMI is 34 kg/m2. His pulse is 75/min and his blood pressure is 148/95 mm Hg. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin A1c 6.8%
Serum
Glucose 180 mg/dL
Creatinine 1.0 mg/dL
Total cholesterol 220 mg/dL
HDL cholesterol 50 mg/dL
Triglycerides 140 mg/dL
Urine
Blood negative
Glucose 2+
Protein 1+
Ketones negative
Which of the following is the most appropriate next step in management?
- A. Metformin therapy (Correct Answer)
- B. Low-carbohydrate diet
- C. Aspirin therapy
- D. ACE inhibitor therapy
- E. Insulin therapy
Diabetic nephropathy Explanation: ***Metformin therapy***
- This patient has **newly diagnosed type 2 diabetes mellitus** with classic symptoms (polyuria, polydipsia, blurred vision) and laboratory confirmation (HbA1c 6.8%, glucose 180 mg/dL, glucosuria).
- **Metformin is the first-line pharmacologic therapy** for type 2 diabetes according to current guidelines (ADA, AACE) due to its efficacy, safety profile, cardiovascular benefits, and low risk of hypoglycemia.
- The patient's creatinine is normal (1.0 mg/dL), so metformin is not contraindicated.
- Addressing the **symptomatic hyperglycemia** is the most appropriate next step in management.
*ACE inhibitor therapy*
- ACE inhibitors are indicated for diabetic patients with **hypertension and albuminuria** to provide renoprotection and slow progression of diabetic nephropathy.
- While this patient has both hypertension (148/95 mm Hg) and proteinuria (1+), ACE inhibitor therapy should be initiated **after or concurrent with diabetes management**, not as the sole initial intervention.
- The patient needs **glycemic control first** given symptomatic hyperglycemia, though ACE inhibitor would be an appropriate addition to the treatment regimen.
*Low-carbohydrate diet*
- **Lifestyle modifications** including medical nutrition therapy and exercise are foundational for managing type 2 diabetes and should be recommended.
- However, given the patient's **symptomatic hyperglycemia** (HbA1c 6.8%, glucose 180 mg/dL with classic symptoms), lifestyle changes alone are **insufficient as the initial management**.
- Pharmacologic therapy with metformin should be initiated immediately alongside lifestyle counseling.
*Insulin therapy*
- Insulin therapy is indicated for patients with **very high HbA1c** (typically >9-10%), **severe symptoms of hyperglycemia**, evidence of catabolism, or failure of oral agents.
- This patient's HbA1c of 6.8% represents **relatively mild hyperglycemia** that is appropriately managed with metformin as first-line therapy.
- Insulin is **not indicated** at this stage of disease.
*Aspirin therapy*
- **Aspirin for primary prevention** in diabetes is controversial; current guidelines suggest shared decision-making for patients at increased cardiovascular risk without high bleeding risk.
- While this patient has cardiovascular risk factors (diabetes, hypertension, obesity, dyslipidemia), aspirin would be a **secondary priority** after addressing the acute metabolic derangements.
- **Glycemic control takes precedence** over aspirin initiation in newly diagnosed diabetes.
More Diabetic nephropathy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.