CKD etiology and pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for CKD etiology and pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
CKD etiology and pathophysiology US Medical PG Question 1: A 62-year-old woman with type 2 diabetes mellitus comes to the physician because of a 3-month history of fatigue and weakness. Her hemoglobin A1c concentration was 13.5% 12 weeks ago. Her blood pressure is 152/92 mm Hg. Examination shows lower extremity edema. Serum studies show:
K+ 5.1 mEq/L
Phosphorus 5.0 mg/dL
Ca2+ 7.8 mg/dL
Urea nitrogen 60 mg/dL
Creatinine 2.2 mg/dL
Which of the following is the best parameter for early detection of this patient’s renal condition?
- A. Serum total protein
- B. Serum creatinine
- C. Urinary red blood cell casts
- D. Serum urea nitrogen
- E. Urinary albumin (Correct Answer)
CKD etiology and pathophysiology Explanation: ***Urinary albumin***
- **Microalbuminuria** is often the earliest detectable sign of **diabetic nephropathy**, occurring before changes in GFR or serum creatinine become apparent.
- Regular screening for urinary albumin in diabetic patients allows for early intervention to slow the progression of **renal damage**.
*Serum total protein*
- **Hypoalbuminemia** can be seen in advanced renal disease due to significant proteinuria, but it is not an early marker.
- Other conditions like **liver disease** or **malnutrition** can also cause altered serum total protein, making it less specific for early renal damage.
*Serum creatinine*
- **Serum creatinine** levels rise significantly only after a substantial portion of kidney function (around 50%) has been lost.
- Therefore, it is a marker of established renal dysfunction rather than an early indicator.
*Urinary red blood cell casts*
- The presence of **red blood cell casts** in urine indicates **glomerulonephritis** or other inflammatory conditions affecting the glomeruli.
- While concerning, it is not the typical or earliest presentation of **diabetic nephropathy**, which primarily involves proteinuria.
*Serum urea nitrogen*
- **Blood urea nitrogen (BUN)** levels, like creatinine, increase with declining kidney function and are used to assess the severity of **renal impairment**.
- However, BUN levels can also be influenced by factors like **hydration status** and **protein intake**, and they are not an early marker of nascent renal disease.
CKD etiology and pathophysiology US Medical PG Question 2: Which factor most strongly influences protein filtration at the glomerulus?
- A. Electrical charge
- B. Molecular size (Correct Answer)
- C. Shape
- D. Temperature
CKD etiology and pathophysiology Explanation: ***Molecular size***
- The glomerular filtration barrier, particularly the **slit diaphragms** between podocytes, acts as a size-selective filter, restricting the passage of larger molecules.
- Proteins like **albumin** (molecular radius ~36 Å, molecular weight ~69 kDa) are significantly large, making them difficult to pass through the filtration barrier.
- Size selectivity is the **primary and most important** factor in protein filtration.
*Electrical charge*
- The glomerular basement membrane contains **negatively charged proteoglycans** (heparan sulfate), which repel negatively charged proteins like albumin, contributing to their retention.
- While important, the role of electrical charge is **secondary** to molecular size in preventing the bulk passage of most proteins.
*Shape*
- While abnormal protein shapes (e.g., **amyloid fibrils**) can impact filtration in specific disease states, the typical physiological filtration of most proteins is primarily governed by size and charge.
- The inherent shape of normal globular proteins plays a less direct role compared to their overall size.
*Temperature*
- **Physiological temperature** is relatively constant in the body and does not directly influence the molecular interactions and physical properties of the glomerular filtration barrier in a way that significantly alters protein filtration.
- Temperature changes would lead to denaturation or aggregation, which are not the primary determinants of normal protein filtration.
CKD etiology and pathophysiology US Medical PG Question 3: A 50-year-old morbidly obese woman presents to a primary care clinic for the first time. She states that her father recently died due to kidney failure and wants to make sure she is healthy. She works as an accountant, is not married or sexually active, and drinks alcohol occasionally. She currently does not take any medications. She does not know if she snores at night but frequently feels fatigued. She denies any headaches but reports occasional visual difficulties driving at night. She further denies any blood in her urine or increased urinary frequency. She does not engage in any fitness program. She has her period every 2 months with heavy flows. Her initial vital signs reveal that her blood pressure is 180/100 mmHg and heart rate is 70/min. Her body weight is 150 kg (330 lb). On physical exam, the patient has droopy eyelids, a thick neck with a large tongue, no murmurs or clicks on cardiac auscultation, clear lungs, a soft nontender, albeit large abdomen, and palpable pulses in her distal extremities. She can walk without difficulty. A repeat measurement of her blood pressure shows 155/105 mmHg. Which among the following is part of the most appropriate next step in management?
- A. Renal artery doppler ultrasonography
- B. Polysomnography
- C. Urinalysis (Correct Answer)
- D. Thyroid-stimulating hormone
- E. Cortisol levels
CKD etiology and pathophysiology Explanation: ***Urinalysis***
- Given the patient's strong family history of **kidney failure**, current presentation with **hypertension (BP 180/100 mmHg, confirmed at 155/105 mmHg)**, and concern for her health, a urinalysis is a crucial initial step to look for signs of kidney damage or disease.
- Urinalysis can detect **proteinuria**, **hematuria**, or other abnormalities indicative of renal pathology, helping to assess her kidney health.
*Renal artery doppler ultrasonography*
- While **renal artery stenosis** can cause hypertension, it is usually considered after initial non-invasive tests and if there are specific signs of secondary hypertension like a **renal bruit** or **unexplained renal insufficiency**, which are not explicitly described here as a first step.
- This is a more advanced diagnostic test and not typically the *most appropriate next step* before basic screening like urinalysis.
*Polysomnography*
- The patient's **morbid obesity**, **fatigue**, and physical exam findings like a **thick neck with a large tongue** suggest **obstructive sleep apnea (OSA)**, for which polysomnography is the diagnostic test.
- However, while important, addressing the immediate concern of **hypertension** and assessing **kidney health** (given the family history) is a higher priority in the *initial* workup.
*Thyroid-stimulating hormone*
- Symptoms like **fatigue**, **heavy menstrual periods (menorrhagia)**, and features like a **thick tongue** could suggest **hypothyroidism**.
- However, **hypertension** and the urgent need to evaluate **kidney function** (due to family history and current high blood pressure) make urinalysis a more immediate and critical step before an extensive endocrine workup.
*Cortisol levels*
- Elevated blood pressure, obesity, and menstrual irregularities could, in some contexts, raise suspicion for **Cushing's syndrome**.
- However, there are no classic features like **buffalo hump**, **moon facies**, or **striae** mentioned, and assessing renal involvement given the family history and current hypertension is a more direct next step.
CKD etiology and pathophysiology US Medical PG Question 4: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
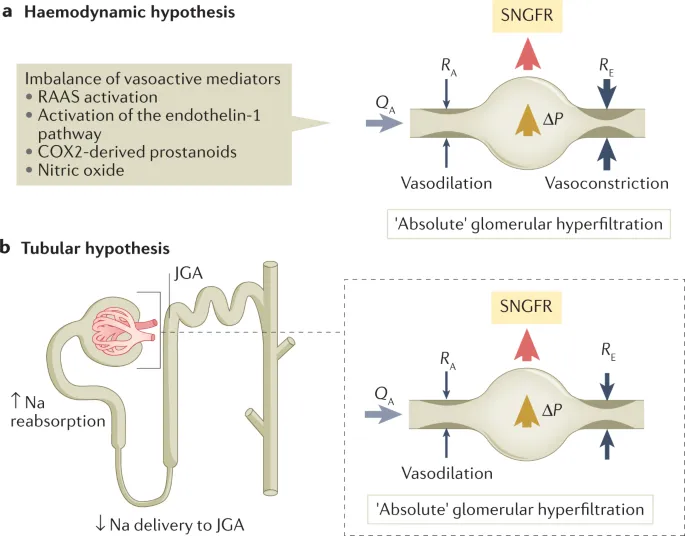
CKD etiology and pathophysiology Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
CKD etiology and pathophysiology US Medical PG Question 5: A 22-year-old man comes to the emergency department because of several episodes of blood in his urine and decreased urine output for 5 days. His blood pressure is 158/94 mm Hg. Examination shows bilateral lower extremity edema. Urinalysis shows 3+ protein and red blood cell casts. Mass spectrometry analysis of the urinary protein detects albumin, transferrin, and IgG. Which of the following best describes this type of proteinuria?
- A. Tubular
- B. Selective glomerular
- C. Nonselective glomerular (Correct Answer)
- D. Postrenal
- E. Overflow
CKD etiology and pathophysiology Explanation: ***Nonselective glomerular***
- The presence of **albumin**, **transferrin**, and **IgG** indicates a loss of molecular control by the glomerulus, allowing both small and larger proteins to pass.
- This pattern, particularly with significant proteinuria (3+ protein) and **red blood cell casts**, is characteristic of a severe **glomerular injury** leading to nonselective filtration.
*Tubular*
- **Tubular proteinuria** results from impaired reabsorption of low-molecular-weight proteins by the renal tubules, typically due to **tubulointerstitial damage**.
- It would primarily involve smaller proteins like **beta-2 microglobulin** or **retinol-binding protein**, not significant amounts of albumin and IgG.
*Selective glomerular*
- **Selective glomerular proteinuria** involves the loss of smaller proteins, primarily **albumin**, due to damage to the glomerular charge barrier, while larger proteins like IgG are retained.
- The detection of **IgG** in the urine indicates a loss of both charge and size selectivity, ruling out selective proteinuria.
*Postrenal*
- **Postrenal proteinuria** is due to inflammation or bleeding in the urinary tract below the kidneys, such as the ureters, bladder, or urethra.
- It is typically associated with conditions like **urinary tract infections** or **stones** and would not cause the significant systemic symptoms (hypertension, edema) or protein profile seen here.
*Overflow*
- **Overflow proteinuria** occurs when there is an overproduction of low-molecular-weight proteins (e.g., **Bence Jones proteins** in multiple myeloma) that overwhelm the reabsorptive capacity of the tubules.
- This patient presents with **glomerular injury** features (red blood cell casts, hypertension, edema) and the presence of albumin and IgG, not an overproduction of single-type low-molecular-weight proteins.
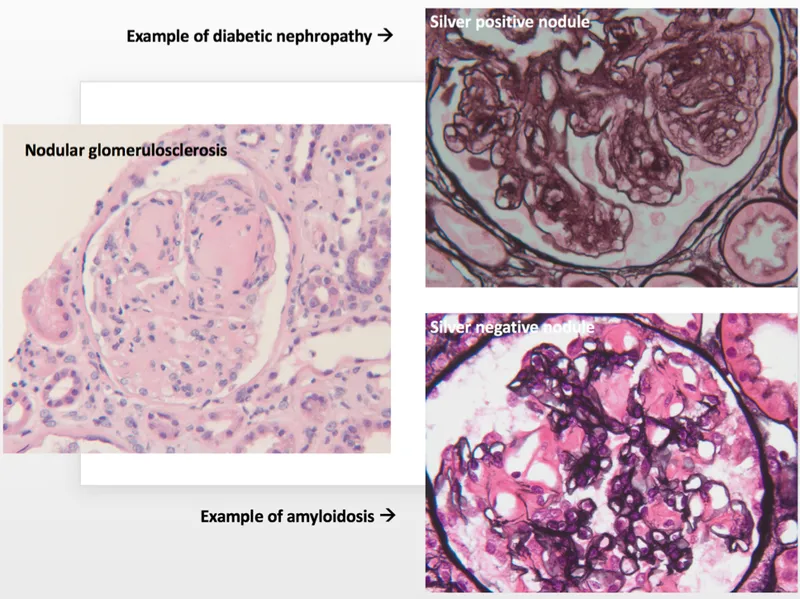
CKD etiology and pathophysiology US Medical PG Question 6: A 62-year-old man comes to the physician because of fatigue and decreased urine output for 2 weeks. He has not been to the physician for many years and takes no medications. Serum studies show a urea nitrogen concentration of 42 mg/dL and a creatinine concentration of 2.3 mg/dL. Urinalysis shows heavy proteinuria. A photomicrograph of a section of a kidney biopsy specimen is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Amyloidosis
- B. Diabetes mellitus (Correct Answer)
- C. Dyslipidemia
- D. Fibromuscular dysplasia
- E. Severe hypertension
CKD etiology and pathophysiology Explanation: ***Diabetes mellitus***
- The kidney biopsy shows **diffuse glomerulosclerosis** with **Kimmelstiel-Wilson nodules** (nodular mesangial sclerosis), which are pathognomonic for **diabetic nephropathy**.
- **Heavy proteinuria**, elevated BUN (42 mg/dL) and creatinine (2.3 mg/dL), along with the patient's age, are consistent with long-standing diabetes mellitus, even if previously undiagnosed.
- Diabetic nephropathy is the leading cause of end-stage renal disease in the United States.
*Amyloidosis*
- While amyloidosis can cause nephrotic syndrome and renal failure, the characteristic histology shows **extracellular amorphous deposits** that stain with **Congo red** and demonstrate apple-green birefringence under polarized light.
- The mesangial nodular pattern seen in diabetic nephropathy is distinct from the amyloid deposits seen in amyloidosis.
- Systemic amyloidosis typically presents with other organ involvement such as **cardiomyopathy**, **hepatosplenomegaly**, or **macroglossia**.
*Dyslipidemia*
- **Dyslipidemia** is a common comorbidity of nephrotic syndrome and diabetic nephropathy, but it is not a direct cause of the structural glomerular damage.
- It represents a metabolic consequence rather than the underlying etiology of the renal pathology.
*Fibromuscular dysplasia*
- **Fibromuscular dysplasia** affects the **renal arteries**, causing **renovascular hypertension** and renal ischemia.
- It typically presents with hypertension in young to middle-aged women and an abdominal bruit, not with heavy proteinuria and glomerular nodular sclerosis.
- The histology would show arterial wall changes, not glomerular pathology.
*Severe hypertension*
- **Severe hypertension** causes hypertensive nephrosclerosis with arteriolosclerosis and global glomerulosclerosis, but not the characteristic **nodular mesangial expansion** (Kimmelstiel-Wilson nodules) seen in diabetic nephropathy.
- While hypertension commonly accompanies diabetic nephropathy, the specific histological findings of nodular glomerulosclerosis are pathognomonic for diabetes mellitus.
- Hypertensive nephrosclerosis shows arteriolar hyalinosis and ischemic changes, which differ from diabetic glomerular changes.
CKD etiology and pathophysiology US Medical PG Question 7: A 72-year-old woman with a medical history significant for chronic kidney disease stage 4, hypertension, and type 2 diabetes mellitus, presents to the office for a scheduled visit. During her last visit, the physician started discussing with her the possibility of starting her on dialysis for her chronic kidney disease. The patient has no complaints about her health and enjoys spending time with her family. At presentation, she is afebrile; the blood pressure is 139/89 mm Hg and the heart rate is 80/min. On physical examination, her pulses are bounding, the complexion is pale, she has a grade ⅙ holosystolic murmur, breath sounds remain clear, and 2+ pedal edema to the knee. The measurement of which of the following laboratory values is most appropriate to screen for renal osteodystrophy in this patient?
- A. Erythrocyte sedimentation rate
- B. Serum vitamin B-12 level
- C. Serum C-reactive protein level
- D. Serum thyroid-stimulating hormone level
- E. Serum intact parathyroid hormone level (Correct Answer)
CKD etiology and pathophysiology Explanation: ***Serum intact parathyroid hormone level***
- **Renal osteodystrophy**, a common complication of **chronic kidney disease (CKD)** stage 4 and 5, is primarily caused by secondary hyperparathyroidism.
- **Intact parathyroid hormone (iPTH)** is critical in diagnosing and monitoring this condition, as elevated levels indicate impaired mineral and bone metabolism due to failing kidneys.
*Erythrocyte sedimentation rate*
- **Erythrocyte sedimentation rate (ESR)** is a general marker of inflammation and is not specific for renal osteodystrophy.
- While CKD can be associated with inflammation, ESR does not directly assess mineral and bone disorders.
*Serum vitamin B-12 level*
- **Vitamin B-12** deficiency can cause anemia and neurological symptoms, but it is not directly involved in the pathogenesis or diagnosis of renal osteodystrophy.
- This test would be more relevant if the patient presented with symptoms of **pernicious anemia** or neuropathy.
*Serum C-reactive protein level*
- **C-reactive protein (CRP)**, like ESR, is a general **inflammatory marker** and does not provide specific information about bone health or mineral metabolism in CKD.
- High CRP levels might indicate infection or systemic inflammation but are not used to screen for renal osteodystrophy.
*Serum thyroid-stimulating hormone level*
- **Thyroid-stimulating hormone (TSH)** assesses **thyroid function**, which is distinct from renal osteodystrophy.
- Thyroid disorders can impact bone health, but TSH is not the primary screening test for bone disease related to CKD.
CKD etiology and pathophysiology US Medical PG Question 8: A 60-year-old man with a long-standing history of type 2 diabetes and hypertension managed with lisinopril and metformin presents with itchy skin. He also describes moderate nausea, vomiting, muscle weakness, and fatigue. The vital signs include: temperature 36.8°C (98.2°F), heart rate 98/min, respiratory rate 15/min, blood pressure 135/85 mm Hg, oxygen saturation 100% on room air. Physical exam is notable for pale conjunctivae, pitting edema, and ascites. Laboratory findings are shown below:
BUN 78 mg/dL
pCO2 25 mm Hg
Creatinine 7.2 mg/dL
Glucose 125 mg/dL
Serum chloride 102 mmol/L
Serum potassium 6.3 mEq/L
Serum sodium 130 mEq/L
Total calcium 1.3 mmol/L
Magnesium 1.2 mEq/L
Phosphate 1.9 mmol/L
Hemoglobin 9.5 g/dL
MCV 86 μm3
Bicarbonate (HCO3) 10 mmol/L
Shrunken kidneys are identified on renal ultrasound. The doctor explains to the patient that he will likely need dialysis due to his significant renal failure until a renal transplant can be performed. The patient is concerned because he is very busy and traveling a lot for work. Given his lifestyle requirements, what is a potential complication of the most appropriate dialysis modality for this patient?
- A. Excessive bleeding
- B. Muscle cramping
- C. Hypotension
- D. Hypertriglyceridemia (Correct Answer)
- E. Hypoglycemia
CKD etiology and pathophysiology Explanation: ***Hypertriglyceridemia***
- The patient's **lifestyle requirements** (busy, traveling a lot) suggest **peritoneal dialysis (PD)** as the most appropriate modality due to its flexibility and home-based nature.
- **Hypertriglyceridemia** is a common complication of PD due to the absorption of glucose from the dialysate, which stimulates hepatic triglyceride synthesis.
*Excessive bleeding*
- This is a rare complication in both hemodialysis and peritoneal dialysis.
- While **anti-coagulation** is used in hemodialysis, it's carefully monitored, and significant bleeding is not a typical long-term complication of the chosen modality (PD).
*Muscle cramping*
- **Muscle cramps** can occur with hemodialysis, typically due to rapid fluid and electrolyte shifts.
- This is less common in peritoneal dialysis, which involves a slower and more continuous exchange process.
*Hypotension*
- **Hypotension** can be a complication of hemodialysis due to rapid fluid removal.
- Peritoneal dialysis, with its gradual fluid exchange, is generally less associated with significant hypotensive episodes.
*Hypoglycemia*
- The **glucose-rich dialysate** used in peritoneal dialysis can actually lead to **hyperglycemia**, not hypoglycemia, especially in diabetic patients.
- Regular insulin adjustments are often required for diabetic patients on PD.
CKD etiology and pathophysiology US Medical PG Question 9: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
CKD etiology and pathophysiology Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
CKD etiology and pathophysiology US Medical PG Question 10: A 42-year-old man comes to the physician because of a 2-month history of fatigue and increased urination. The patient reports that he has been drinking more than usual because he is constantly thirsty. He has avoided driving for the past 8 weeks because of intermittent episodes of blurred vision. He had elevated blood pressure at his previous visit but is otherwise healthy. Because of his busy work schedule, his diet consists primarily of fast food. He does not smoke or drink alcohol. He is 178 cm (5 ft 10 in) tall and weighs 109 kg (240 lb); BMI is 34 kg/m2. His pulse is 75/min and his blood pressure is 148/95 mm Hg. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin A1c 6.8%
Serum
Glucose 180 mg/dL
Creatinine 1.0 mg/dL
Total cholesterol 220 mg/dL
HDL cholesterol 50 mg/dL
Triglycerides 140 mg/dL
Urine
Blood negative
Glucose 2+
Protein 1+
Ketones negative
Which of the following is the most appropriate next step in management?
- A. Metformin therapy (Correct Answer)
- B. Low-carbohydrate diet
- C. Aspirin therapy
- D. ACE inhibitor therapy
- E. Insulin therapy
CKD etiology and pathophysiology Explanation: ***Metformin therapy***
- This patient has **newly diagnosed type 2 diabetes mellitus** with classic symptoms (polyuria, polydipsia, blurred vision) and laboratory confirmation (HbA1c 6.8%, glucose 180 mg/dL, glucosuria).
- **Metformin is the first-line pharmacologic therapy** for type 2 diabetes according to current guidelines (ADA, AACE) due to its efficacy, safety profile, cardiovascular benefits, and low risk of hypoglycemia.
- The patient's creatinine is normal (1.0 mg/dL), so metformin is not contraindicated.
- Addressing the **symptomatic hyperglycemia** is the most appropriate next step in management.
*ACE inhibitor therapy*
- ACE inhibitors are indicated for diabetic patients with **hypertension and albuminuria** to provide renoprotection and slow progression of diabetic nephropathy.
- While this patient has both hypertension (148/95 mm Hg) and proteinuria (1+), ACE inhibitor therapy should be initiated **after or concurrent with diabetes management**, not as the sole initial intervention.
- The patient needs **glycemic control first** given symptomatic hyperglycemia, though ACE inhibitor would be an appropriate addition to the treatment regimen.
*Low-carbohydrate diet*
- **Lifestyle modifications** including medical nutrition therapy and exercise are foundational for managing type 2 diabetes and should be recommended.
- However, given the patient's **symptomatic hyperglycemia** (HbA1c 6.8%, glucose 180 mg/dL with classic symptoms), lifestyle changes alone are **insufficient as the initial management**.
- Pharmacologic therapy with metformin should be initiated immediately alongside lifestyle counseling.
*Insulin therapy*
- Insulin therapy is indicated for patients with **very high HbA1c** (typically >9-10%), **severe symptoms of hyperglycemia**, evidence of catabolism, or failure of oral agents.
- This patient's HbA1c of 6.8% represents **relatively mild hyperglycemia** that is appropriately managed with metformin as first-line therapy.
- Insulin is **not indicated** at this stage of disease.
*Aspirin therapy*
- **Aspirin for primary prevention** in diabetes is controversial; current guidelines suggest shared decision-making for patients at increased cardiovascular risk without high bleeding risk.
- While this patient has cardiovascular risk factors (diabetes, hypertension, obesity, dyslipidemia), aspirin would be a **secondary priority** after addressing the acute metabolic derangements.
- **Glycemic control takes precedence** over aspirin initiation in newly diagnosed diabetes.
More CKD etiology and pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.