CKD complications management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for CKD complications management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
CKD complications management US Medical PG Question 1: You are called to a hemodialysis suite. The patient is a 61-year-old man with a history of hypertension, hypercholesterolemia, and type-2 diabetes mellitus-induced end-stage renal disease who has required hemodialysis for the past year. His current hemodialysis session is nearing the end when the nurse notices that his blood pressure has dropped to 88/60 mm Hg from his normal of 142/90 mm Hg. The patient denies any shortness of breath or chest pain. He took his daily bisoprolol, metformin, and insulin this morning before coming to the hospital. On examination, the patient’s blood pressure is 92/60 mm Hg, and his heart rate is 119/min. Chest auscultation is unremarkable. What is the most appropriate next management step?
- A. Infuse 1 liter of 0.9% saline
- B. Administer intravenous calcium gluconate
- C. Transfuse the patient with 1 unit of packed red blood cells
- D. Stop ultrafiltration and decrease blood flow into the machine (Correct Answer)
- E. Start the patient on an epinephrine drip
CKD complications management Explanation: ***Stop ultrafiltration and decrease blood flow into the machine***
- The patient's **hypotension** and **tachycardia** during hemodialysis strongly suggest **intradialytic hypotension**, which is often caused by excessive fluid removal (ultrafiltration) or rapid fluid shifts.
- **Stopping ultrafiltration** and **reducing blood flow** allows for gradual re-equilibration of fluid and helps stabilize blood pressure without adding more fluid to a patient with end-stage renal disease.
*Infuse 1 liter of 0.9% saline*
- Administering a large volume of saline is generally **contraindicated in ESRD patients** given their inability to excrete fluid, which could lead to **fluid overload** and pulmonary edema.
- While fluid resuscitation might be considered for severe hypotension, the initial step in intradialytic hypotension is to adjust the dialysis settings.
*Administer intravenous calcium gluconate*
- **Calcium gluconate** is primarily used to stabilize the cardiac membrane in cases of **severe hyperkalemia**, which is not indicated by the current clinical picture.
- There is no mention of ECG changes or lab results to suggest hyperkalemia.
*Transfuse the patient with 1 unit of packed red blood cells*
- There is no clinical evidence of **acute blood loss** or **severe anemia** presenting with hypovolemic shock.
- Transfusion is an intervention for significant blood loss or severe anemia, not for intradialytic hypotension caused by fluid shifts.
*Start the patient on an epinephrine drip*
- **Vasopressors** like epinephrine are typically reserved for **refractory hypotension** after more conservative measures have failed, or in cases of **septic shock** or **anaphylaxis**.
- Initiating a powerful vasopressor as a first step without addressing the potential underlying cause related to dialysis is inappropriate.
CKD complications management US Medical PG Question 2: A 42-year-old man presents to his primary care physician for a wellness checkup. The patient has a past medical history of obesity, constipation, and depression. His current medications include metformin, lactulose, and fluoxetine. His temperature is 99.5°F (37.5°C), blood pressure is 157/102 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 5,500/mm^3 with normal differential
Platelet count: 190,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 105 mEq/L
K+: 3.5 mEq/L
HCO3-: 21 mEq/L
BUN: 20 mg/dL
Glucose: 129 mg/dL
Creatinine: 1.1 mg/dL
AST: 12 U/L
ALT: 10 U/L
Urine:
Appearance: Yellow
Bacteria: Absent
Red blood cells: 0/hpf
pH: 6.8
Nitrite: Absent
Which of the following is the next best step in management?
- A. Administer ammonium chloride and repeat lab studies (Correct Answer)
- B. Administer bicarbonate and repeat lab studies
- C. Administer high dose bicarbonate
- D. Obtain urine sodium level
- E. Administer hydrochlorothiazide
CKD complications management Explanation: ***Administer ammonium chloride and repeat lab studies***
- The patient has **hypertension** (157/102 mmHg), **mild metabolic acidosis** (HCO3- 21 mEq/L), and **inappropriately alkaline urine pH (6.8)** despite systemic acidosis, suggesting **distal renal tubular acidosis (Type 1 RTA)**.
- In Type 1 RTA, the distal tubule cannot adequately secrete H+ ions, resulting in inability to acidify urine below pH 5.5 even in the presence of systemic acidosis.
- **Ammonium chloride loading test** is used to confirm Type 1 RTA by inducing metabolic acidosis and demonstrating the kidney's inability to lower urine pH below 5.5, establishing the diagnosis before initiating chronic alkali therapy.
*Administer hydrochlorothiazide*
- While the patient does have hypertension requiring treatment, hydrochlorothiazide is **not first-line therapy for Type 1 RTA** and can actually worsen hypokalemia, which is common in Type 1 RTA.
- Thiazide diuretics can exacerbate metabolic acidosis and do not address the underlying tubular defect in acid excretion.
- Treating hypertension is important but should occur after establishing the diagnosis of the acid-base disorder.
*Administer high dose bicarbonate*
- High-dose bicarbonate is the **chronic treatment** for Type 1 RTA, but the diagnosis must first be confirmed.
- Starting empiric bicarbonate therapy without diagnostic confirmation would obscure the diagnosis and prevent appropriate long-term management planning.
- The degree of acidosis is mild (HCO3- 21 mEq/L), so urgent bicarbonate administration is not required.
*Obtain urine sodium level*
- Urine sodium is useful for evaluating volume status, prerenal azotemia, or differentiating causes of acute kidney injury.
- It does not help diagnose or confirm renal tubular acidosis, which is the primary concern given the alkaline urine pH in the setting of metabolic acidosis.
*Administer bicarbonate and repeat lab studies*
- Simply administering bicarbonate and rechecking labs does not establish a diagnosis and would temporarily mask the acid-base abnormality.
- This approach would delay definitive diagnosis of Type 1 RTA and is not a systematic diagnostic strategy.
- Repeating labs without a diagnostic intervention provides no additional useful information.
CKD complications management US Medical PG Question 3: A 54-year-old African American man presents to the clinic for his first annual well-check. He was unemployed for years but recently received health insurance from a new job. He reports feeling healthy and has no complaints. His blood pressure is 157/90 mmHg, pulse is 86/min, and respirations are 12/min. Routine urinalysis demonstrated a mild increase in albumin and creatinine. What medication is indicated at this time?
- A. Hydrochlorothiazide
- B. Metoprolol
- C. Furosemide
- D. Lisinopril (Correct Answer)
- E. Amlodipine
CKD complications management Explanation: ***Lisinopril***
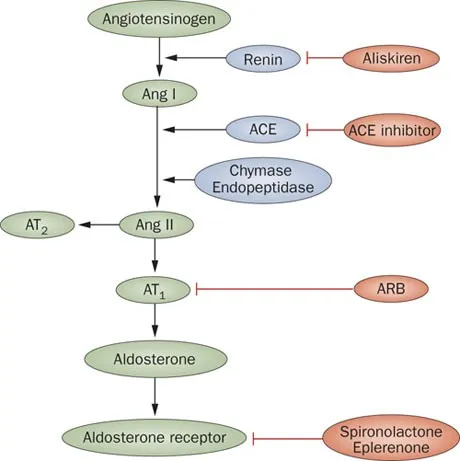
- This patient presents with **hypertension (157/90 mmHg)** and **mild albuminuria with elevated creatinine**, indicating early chronic kidney disease (CKD). An **ACE inhibitor (e.g., lisinopril)** is the first-line treatment for hypertension in **any patient with CKD or proteinuria**, regardless of race or ethnicity.
- ACE inhibitors are **renoprotective** by reducing intraglomerular pressure and slowing progression of kidney disease. The presence of albuminuria represents a **compelling indication** that overrides other considerations for initial antihypertensive selection.
- Note: While ACE inhibitors are typically **less effective** as monotherapy in African Americans without compelling indications, the presence of CKD/proteinuria makes them the preferred agent.
*Hydrochlorothiazide*
- While a **thiazide diuretic** like hydrochlorothiazide would be an appropriate first-line agent for this African American patient with uncomplicated hypertension, it is **less effective** than an ACE inhibitor in patients with **proteinuria or kidney disease**.
- It does not offer the same degree of **renoprotection** as an ACE inhibitor in this clinical scenario with documented albuminuria.
*Metoprolol*
- **Beta-blockers** like metoprolol are effective antihypertensives but are generally **not considered first-line** for uncomplicated hypertension unless there are compelling indications like heart failure, angina, or history of myocardial infarction.
- They also do not provide the specific **renoprotective benefits** seen with ACE inhibitors in patients with albuminuria.
*Furosemide*
- **Loop diuretics** such as furosemide are potent diuretics primarily used for managing **symptoms of fluid overload** (e.g., heart failure, severe edema) and are not typically the first choice for chronic hypertension without such indications.
- For patients with **mild kidney impairment and hypertension without volume overload**, an ACE inhibitor is preferred for its renoprotective effects.
*Amlodipine*
- **Calcium channel blockers** like amlodipine are effective antihypertensives and would typically be an excellent first-line choice for an African American patient with hypertension.
- However, for this patient with **documented albuminuria**, an ACE inhibitor is preferred due to its **specific renoprotective effects** and proven benefit in slowing CKD progression, which amlodipine does not provide.
CKD complications management US Medical PG Question 4: A 39-year-old woman presents to the clinic with complaints of constipation for the past 2 weeks. She reports that it has been getting increasingly difficult to pass stool to the point that she would go for 2-3 days without going to the bathroom. Prior to this, she passed stool every day without difficulty. She denies weight changes, headaches, chest pain, or abdominal pain but endorses fatigue. Her past medical history is significant for 2 episodes of kidney stones within the past 3 months. A physical examination is unremarkable. Laboratory studies are done and the results are shown below:
Serum:
Na+: 138 mEq/L
Cl-: 97 mEq/L
K+: 3.9 mEq/L
HCO3-: 24 mEq/L
BUN: 10 mg/dL
Glucose: 103 mg/dL
Creatinine: 1.1 mg/dL
Thyroid-stimulating hormone: 3.1 uU/mL
Ca2+: 12.1 mg/dL
Phosphate: 1.2 mg/dL (Normal: 2.5-4.5 mg/dL)
What is the most likely explanation for this patient’s low phosphate levels?
- A. Defective G-coupled calcium-sensing receptors in multiple tissues
- B. Increased calcium reabsorption at the distal convoluted tubule due to enhanced TRPV5 channel activity
- C. Hereditary malfunction of phosphate absorption at the small brush border
- D. Chronic renal disease caused by recurrent renal stones
- E. Inhibition of sodium-phosphate cotransporter at the proximal convoluted tubule (PCT) (Correct Answer)
CKD complications management Explanation: ***Inhibition of sodium-phosphate cotransporter at the proximal convoluted tubule (PCT)***
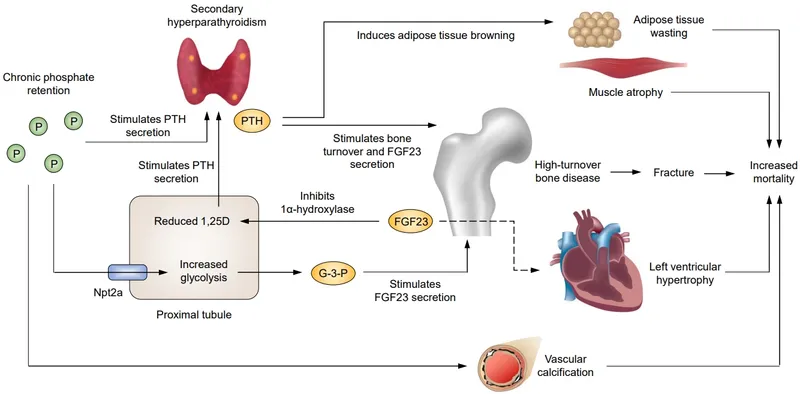
- The patient presents with **hypercalcemia (Ca2+ 12.1 mg/dL)** and **hypophosphatemia (Phosphate 1.2 mg/dL)**, along with a history of recurrent kidney stones and constipation, which are classic signs of **primary hyperparathyroidism**.
- In primary hyperparathyroidism, elevated **parathyroid hormone (PTH)** directly inhibits the **sodium-phosphate cotransporter** in the PCT, leading to decreased phosphate reabsorption and increased renal phosphate excretion.
*Defective G-coupled calcium-sensing receptors in multiple tissues*
- This describes **familial hypocalciuric hypercalcemia (FHH)**, where defective **calcium-sensing receptors (CaSRs)** in the parathyroid glands and kidneys cause a higher set point for calcium, leading to hypercalcemia.
- However, FHH typically presents with **normal to slightly elevated PTH levels** and **hypocalciuria**, whereas this patient's presentation with hypophosphatemia and recurrent kidney stones is more consistent with elevated PTH from primary hyperparathyroidism.
*Increased calcium reabsorption at the distal convoluted tubule due to enhanced TRPV5 channel activity*
- While **PTH** does increase calcium reabsorption, this occurs primarily in the **distal convoluted tubule (DCT)** via activation of **TRPV5 channels**.
- This mechanism explains the **hypercalcemia** but does not directly account for the observed **hypophosphatemia**, which is primarily due to PTH's action on phosphate excretion in the PCT.
*Hereditary malfunction of phosphate absorption at the small brush border*
- This describes conditions like **hereditary hypophosphatemic rickets**, which are characterized by isolated renal phosphate wasting and usually present earlier in life.
- This patient's acute onset of symptoms, hypercalcemia, and history of kidney stones point away from a primary hereditary defect in intestinal phosphate absorption.
*Chronic renal disease caused by recurrent renal stones*
- While recurrent kidney stones can lead to chronic kidney disease (CKD), CKD typically causes **hyperphosphatemia** due to reduced glomerular filtration of phosphate, especially in later stages.
- The patient's creatinine and BUN are within normal limits, indicating no significant chronic kidney disease that would explain the hypophosphatemia.
CKD complications management US Medical PG Question 5: A 66-year-old man with congestive heart failure presents to the emergency department complaining of worsening shortness of breath. These symptoms have worsened over the last 3 days. He has a blood pressure of 126/85 mm Hg and heart rate of 82/min. Physical examination is notable for bibasilar crackles. A chest X-ray reveals bilateral pulmonary edema. His current medications include metoprolol succinate and captopril. You wish to add an additional medication targeted towards his symptoms. Of the following, which statement is correct regarding loop diuretics?
- A. Loop diuretics can cause metabolic acidosis
- B. Loop diuretics can cause ammonia toxicity
- C. Loop diuretics can cause hyperlipidemia
- D. Loop diuretics decrease sodium, magnesium, and chloride but increase calcium
- E. Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter (Correct Answer)
CKD complications management Explanation: ***Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter***
- Loop diuretics, like furosemide, directly block the **Na+/K+/2Cl- cotransporter** in the **thick ascending limb of the loop of Henle**, preventing the reabsorption of these ions.
- This inhibition leads to increased excretion of water, sodium, potassium, and chloride, which is beneficial in conditions like **pulmonary edema** due to **congestive heart failure**.
*Loop diuretics can cause metabolic acidosis*
- Loop diuretics typically cause **metabolic alkalosis**, not acidosis, because they increase the excretion of hydrogen ions and potassium, leading to a compensatory increase in bicarbonate.
- The increased delivery of sodium to the collecting duct can also stimulate potassium and hydrogen secretion, contributing to alkalosis.
*Loop diuretics can cause ammonia toxicity*
- Loop diuretics do not directly cause **ammonia toxicity**; this is more commonly associated with conditions like **hepatic encephalopathy** or certain other medications.
- Their primary mechanism of action is on renal ion transport, not ammonia metabolism.
*Loop diuretics can cause hyperlipidemia*
- While some diuretics like **thiazide diuretics** can cause mild increases in **lipid levels**, loop diuretics are not typically associated with significant **hyperlipidemia**.
- The most common metabolic side effects of loop diuretics include electrolyte imbalances.
*Loop diuretics decrease sodium, magnesium, and chloride but increase calcium*
- Loop diuretics decrease the reabsorption of **sodium**, **magnesium**, and **chloride**, leading to their increased excretion.
- They also increase **calcium excretion** (cause hypocalcemia), rather than increasing serum calcium levels, by inhibiting its reabsorption in the thick ascending limb of the loop of Henle.
CKD complications management US Medical PG Question 6: A 69-year-old male with past medical history of hypertension, hyperlipidemia, and diabetes mellitus complicated by end stage renal disease on dialysis presents to his nephrologist for a follow-up appointment. A few weeks ago, the patient saw his nephrologist because he had been feeling tired despite efforts to get enough sleep, eat a well-balanced diet, and exercise. At the time, laboratory studies revealed a hemoglobin of 9.7 g/dL, and the patient’s nephrologist suggested starting recombinant human erythropoietin (EPO). Since then, the patient has been receiving EPO intravenously three times per week. The patient reports today that he continues to feel tired despite the new treatment. His temperature is 98.0°F (36.7°C), blood pressure is 134/83 mmHg, pulse is 65/min, and respirations are 12/min. On physical exam, he has conjunctival pallor, and laboratory studies show a hemoglobin of 9.8 g/dL.
Which of the following laboratory findings would currently be seen in this patient?
- A. Normal MCV, increased RDW, increased ferritin, increased transferrin saturation
- B. Low MCV, increased RDW, increased ferritin, decreased transferrin saturation
- C. Low MCV, increased RDW, normal ferritin, normal transferrin saturation
- D. Normal MCV, normal RDW, increased ferritin, increased transferrin saturation
- E. Low MCV, increased RDW, decreased ferritin, decreased transferrin saturation (Correct Answer)
CKD complications management Explanation: ***Low MCV, increased RDW, decreased ferritin, decreased transferrin saturation***
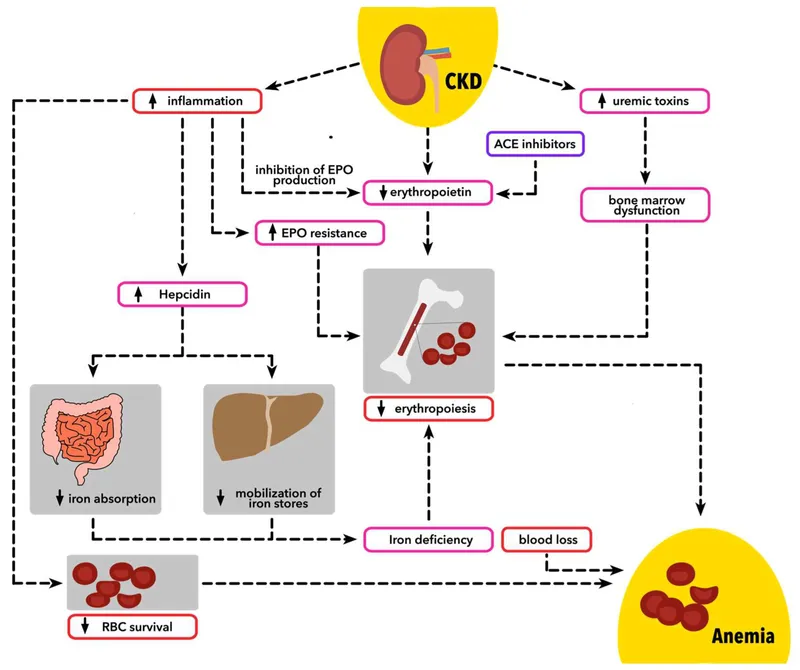
- The patient's persistent anemia despite **erythropoietin (EPO)** treatment, along with conjunctival pallor and an unchanged hemoglobin level, points towards an underlying **iron deficiency**.
- **Iron deficiency** is characterized by **microcytic (low MCV)**, **hypochromic** red blood cells, often with an **increased red cell distribution width (RDW)** due to varying cell sizes, and labs showing **decreased ferritin** (iron stores) and **decreased transferrin saturation** (iron transport).
*Normal MCV, increased RDW, increased ferritin, increased transferrin saturation*
- This profile (**increased ferritin** and **transferrin saturation**) is inconsistent with **iron deficiency**, which is the likely cause of the patient's persistent anemia despite EPO.
- While an **increased RDW** can be seen in some anemias, the other markers do not fit the clinical picture of uncorrected anemia.
*Low MCV, increased RDW, increased ferritin, decreased transferrin saturation*
- The presence of **increased ferritin** suggests sufficient or even elevated iron stores, which contradicts the classic picture of **iron deficiency anemia**.
- **Decreased transferrin saturation** with **increased ferritin** can occur in **anemia of chronic disease (ACD)**, but the primary issue here is likely iron deficiency given the patient's ESRD and lack of response to EPO.
*Low MCV, increased RDW, normal ferritin, normal transferrin saturation*
- **Normal ferritin** and **normal transferrin saturation** would typically rule out **iron deficiency anemia** as the cause of microcytic anemia.
- In a patient with end-stage renal disease (ESRD) and uncorrected anemia, **iron deficiency** is a common and often co-existing issue, making normal iron studies unlikely if iron deficiency is the problem.
*Normal MCV, normal RDW, increased ferritin, increased transferrin saturation*
- This profile suggests **adequate iron stores** and typically indicates a **normocytic anemia** (normal MCV) without significant variation in red cell size (normal RDW).
- Given the patient's uncorrected anemia and the need for EPO, this laboratory picture does not align with the most likely cause of continued fatigue, which is an **iron deficiency**.
CKD complications management US Medical PG Question 7: A 35-year-old woman is involved in a car accident and presents with an open fracture of the left femur and severe bleeding from the left femoral artery. No past medical history or current medications. Her blood pressure is 90/60 mm Hg, pulse is 110/min, and respirations are 21/min. On physical examination, the patient is lethargic, confused, and poorly responds to commands. Peripheral pulses are 1+ in the left lower extremity below the level of the knee and 2+ elsewhere. When she arrives at the hospital, a stat hemoglobin level shows 6 g/dL. Which of the following is most correct about the patient’s condition?
- A. This patient’s laboratory findings will likely demonstrate a normocytic anemia (Correct Answer)
- B. Hemoglobin concentration will be significantly decreased immediately after the acute bleeding begins
- C. This patient will likely be diagnosed with iron deficiency anemia
- D. Hematocrit is expected to accurately reflect the degree of blood loss immediately after acute hemorrhage
- E. Her reticulocyte count is expected to be elevated at this time
CKD complications management Explanation: ***This patient's laboratory findings will likely demonstrate a normocytic anemia***
- In cases of **acute blood loss**, both plasma and red blood cells are lost proportionally, leading to **normocytic, normochromic anemia** as the body has not yet had time to alter red blood cell production
- The MCV (mean corpuscular volume) remains **normal (80-100 fL)** until chronic compensatory mechanisms develop
- This distinguishes acute hemorrhage from chronic blood loss, which can eventually lead to **microcytic anemia** due to iron depletion
*Hematocrit is expected to accurately reflect the degree of blood loss immediately after acute hemorrhage*
- **Immediately after acute hemorrhage**, both red blood cells and plasma are lost proportionally, so the **hematocrit initially remains relatively unchanged** despite significant blood volume loss
- The hematocrit **drops hours later** as fluid shifts from the interstitial space into the vascular compartment to restore blood volume, diluting the remaining red blood cells
- This patient's low hemoglobin at hospital arrival reflects this compensatory hemodilution process
*Hemoglobin concentration will be significantly decreased immediately after the acute bleeding begins*
- While the patient is actively bleeding, the **hemoglobin concentration may not immediately decrease** because red blood cells and plasma are lost together in proportion
- The apparent drop in hemoglobin becomes more pronounced as the body **replenishes plasma volume** through fluid shifts or after **intravenous fluid administration**, diluting the remaining red cell mass
- The hemoglobin of 6 g/dL at hospital arrival reflects fluid shifts that have already occurred
*Her reticulocyte count is expected to be elevated at this time*
- The bone marrow requires **3-5 days to mount a reticulocytosis** in response to acute blood loss and increased erythropoietin production
- At hospital arrival shortly after the accident, the **reticulocyte count will be normal** as insufficient time has passed for bone marrow response
- An elevated reticulocyte count would be expected **several days after the hemorrhage**, not acutely
*This patient will likely be diagnosed with iron deficiency anemia*
- **Iron deficiency anemia** is a **chronic condition** characterized by **microcytic, hypochromic red blood cells** due to prolonged iron loss or inadequate dietary intake
- Acute blood loss, as seen in this trauma case, causes **normocytic anemia** with normal MCV and MCH
- Iron deficiency could develop weeks to months later if iron stores become depleted without supplementation
CKD complications management US Medical PG Question 8: A 57-year-old man is brought to the emergency department 2 hours after the onset of severe nausea and vomiting. He also has cramping abdominal pain and feels fatigued. Two months ago, he injured his lumbar spine in a car accident and lost complete motor and sensory function below the level of injury. He has been bedridden ever since and is cared for at home. He has type 2 diabetes mellitus and renal insufficiency. Examination shows dry mucosal membranes and sensory impairment with flaccid paralysis in both lower limbs that is consistent with prior examinations. Laboratory studies show:
Serum
Calcium 12.8 mg/dL
Parathyroid hormone, N-terminal 180 pg/mL
Thyroid-stimulating hormone 2.5 μU/mL
Thyroxine 8 μg/dL
Calcitriol Decreased
Creatinine 2.6 mg/dL
Urine
Calcium 550 mg/24 h
In addition to administration of intravenous 0.9% saline and calcitonin, which of the following is the most appropriate next step in management?
- A. Thiazide diuretics
- B. Reduced calcium intake
- C. Bisphosphonates (Correct Answer)
- D. Hemodialysis
- E. Glucocorticoids
CKD complications management Explanation: ***Bisphosphonates***
- This patient presents with **severe hypercalcemia** (12.8 mg/dL) with symptoms of nausea, vomiting, and abdominal pain. Given his prolonged immobilization due to a spinal cord injury, **immobilization-induced hypercalcemia** is highly likely.
- After initial rehydration with 0.9% saline and calcitonin to rapidly lower calcium, **bisphosphonates** (e.g., zoledronic acid) are the most appropriate next step to inhibit osteoclast activity and **reduce bone resorption**, which is the primary driver of hypercalcemia in immobilized patients.
*Thiazide diuretics*
- Thiazide diuretics **increase calcium reabsorption** in the renal tubules, which would worsen hypercalcemia.
- These are typically used to treat hypercalciuria (and prevent kidney stones) in normocalcemic patients, not hypercalcemia.
*Reduced calcium intake*
- While reducing dietary calcium is a general recommendation for hypercalcemia, it is **insufficient** as the primary treatment for acute, severe hypercalcemia driven by **increased bone resorption**.
- The main problem here is bone breakdown, not excessive intake.
*Hemodialysis*
- Hemodialysis is reserved for **severe, refractory hypercalcemia** that does not respond to intravenous fluids, calcitonin, and bisphosphonates, especially in patients with severe renal failure.
- While this patient has renal insufficiency (Cr 2.6 mg/dL), other less invasive and highly effective treatments should be tried first.
*Glucocorticoids*
- Glucocorticoids are effective in treating hypercalcemia associated with certain conditions like **granulomatous diseases** (e.g., sarcoidosis) or **hematologic malignancies** (e.g., multiple myeloma).
- They work by reducing intestinal calcium absorption and decreasing production of calcitriol. They are **not indicated** for immobilization-induced hypercalcemia.
CKD complications management US Medical PG Question 9: A 32-year-old woman is hospitalized after developing an allergic reaction to the contrast medium used for a cerebral angiography. The study was initially ordered as part of the diagnostic approach of a suspected case of pseudotumor cerebri. Her medical history is unremarkable. On physical examination she has stable vital signs, a diffuse maculopapular rash over her neck and chest, and a mild fever. She is started on hydrocortisone and monitored for the next 8 hours. After the monitoring period, a laboratory test shows significant azotemia. The patient complains of generalized weakness and palpitations. Tall-peaked T waves are observed on ECG. Which of the following explains this clinical manifestation?
- A. Anemia
- B. Platelet dysfunction
- C. Uremic pericarditis
- D. Metabolic acidosis
- E. Hyperkalemia (Correct Answer)
CKD complications management Explanation: ***Hyperkalemia***
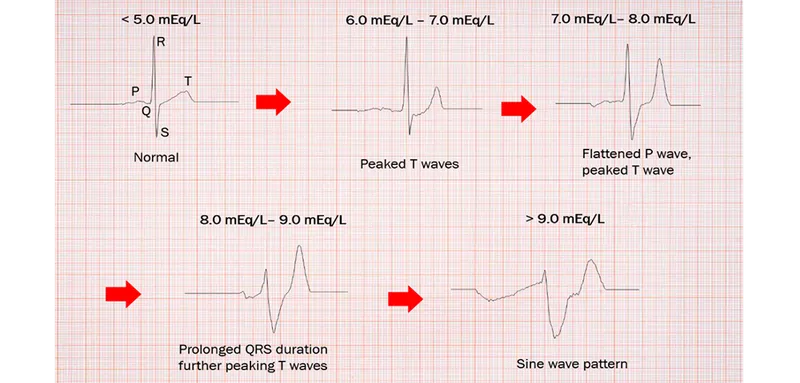
- The combination of **significant azotemia** (indicating acute kidney injury), **generalized weakness**, and **peaked T waves on ECG** are classic signs of hyperkalemia.
- The allergic reaction and subsequent treatment may have exacerbated kidney dysfunction, leading to impaired potassium excretion and subsequent elevated serum potassium levels.
*Anemia*
- While anemia can cause weakness and palpitations, it does not typically manifest with **peaked T waves** on ECG or directly explain the presence of **azotemia**.
- Anemia is common in chronic kidney disease but is not the primary cause of acute symptoms and ECG changes described here.
*Platelet dysfunction*
- Uremia can lead to **platelet dysfunction**, causing bleeding tendencies, but it does not account for the **generalized weakness**, **azotemia**, or the characteristic **peaked T waves** on ECG.
- Platelet dysfunction is typically associated with bruising or prolonged bleeding, not the cardiovascular and neurological symptoms observed.
*Uremic pericarditis*
- **Uremic pericarditis** can cause chest pain, a friction rub, and sometimes palpitations, but it does not directly explain the **peaked T waves** or generalized weakness in the context of acute azotemia.
- The primary symptoms of pericarditis are often related to inflammation of the pericardium rather than electrolyte imbalances.
*Metabolic acidosis*
- **Metabolic acidosis** is common in acute kidney injury and can contribute to weakness and dyspnea, but it does not directly cause **peaked T waves** on ECG.
- While clinically important, acidosis itself doesn't explain the specific ECG findings, which are more indicative of hyperkalemia.
CKD complications management US Medical PG Question 10: A 72-year-old woman with a medical history significant for chronic kidney disease stage 4, hypertension, and type 2 diabetes mellitus, presents to the office for a scheduled visit. During her last visit, the physician started discussing with her the possibility of starting her on dialysis for her chronic kidney disease. The patient has no complaints about her health and enjoys spending time with her family. At presentation, she is afebrile; the blood pressure is 139/89 mm Hg and the heart rate is 80/min. On physical examination, her pulses are bounding, the complexion is pale, she has a grade ⅙ holosystolic murmur, breath sounds remain clear, and 2+ pedal edema to the knee. The measurement of which of the following laboratory values is most appropriate to screen for renal osteodystrophy in this patient?
- A. Erythrocyte sedimentation rate
- B. Serum vitamin B-12 level
- C. Serum C-reactive protein level
- D. Serum thyroid-stimulating hormone level
- E. Serum intact parathyroid hormone level (Correct Answer)
CKD complications management Explanation: ***Serum intact parathyroid hormone level***
- **Renal osteodystrophy**, a common complication of **chronic kidney disease (CKD)** stage 4 and 5, is primarily caused by secondary hyperparathyroidism.
- **Intact parathyroid hormone (iPTH)** is critical in diagnosing and monitoring this condition, as elevated levels indicate impaired mineral and bone metabolism due to failing kidneys.
*Erythrocyte sedimentation rate*
- **Erythrocyte sedimentation rate (ESR)** is a general marker of inflammation and is not specific for renal osteodystrophy.
- While CKD can be associated with inflammation, ESR does not directly assess mineral and bone disorders.
*Serum vitamin B-12 level*
- **Vitamin B-12** deficiency can cause anemia and neurological symptoms, but it is not directly involved in the pathogenesis or diagnosis of renal osteodystrophy.
- This test would be more relevant if the patient presented with symptoms of **pernicious anemia** or neuropathy.
*Serum C-reactive protein level*
- **C-reactive protein (CRP)**, like ESR, is a general **inflammatory marker** and does not provide specific information about bone health or mineral metabolism in CKD.
- High CRP levels might indicate infection or systemic inflammation but are not used to screen for renal osteodystrophy.
*Serum thyroid-stimulating hormone level*
- **Thyroid-stimulating hormone (TSH)** assesses **thyroid function**, which is distinct from renal osteodystrophy.
- Thyroid disorders can impact bone health, but TSH is not the primary screening test for bone disease related to CKD.
More CKD complications management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.