Acute kidney injury US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute kidney injury. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
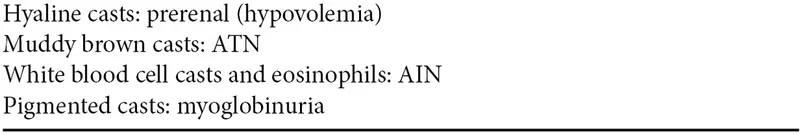
Acute kidney injury US Medical PG Question 1: A 53-year-old woman presents to the emergency room with severe chest pain radiating to the back. She was diagnosed with acute aortic dissection. A few hours into the resuscitation, she was having oliguria. Laboratory findings show a serum creatinine level of 5.3 mg/dL. Which of the following casts are most likely to be seen on urinalysis?
- A. RBC casts
- B. Fatty casts
- C. Muddy brown casts (Correct Answer)
- D. Waxy casts
- E. Hyaline casts
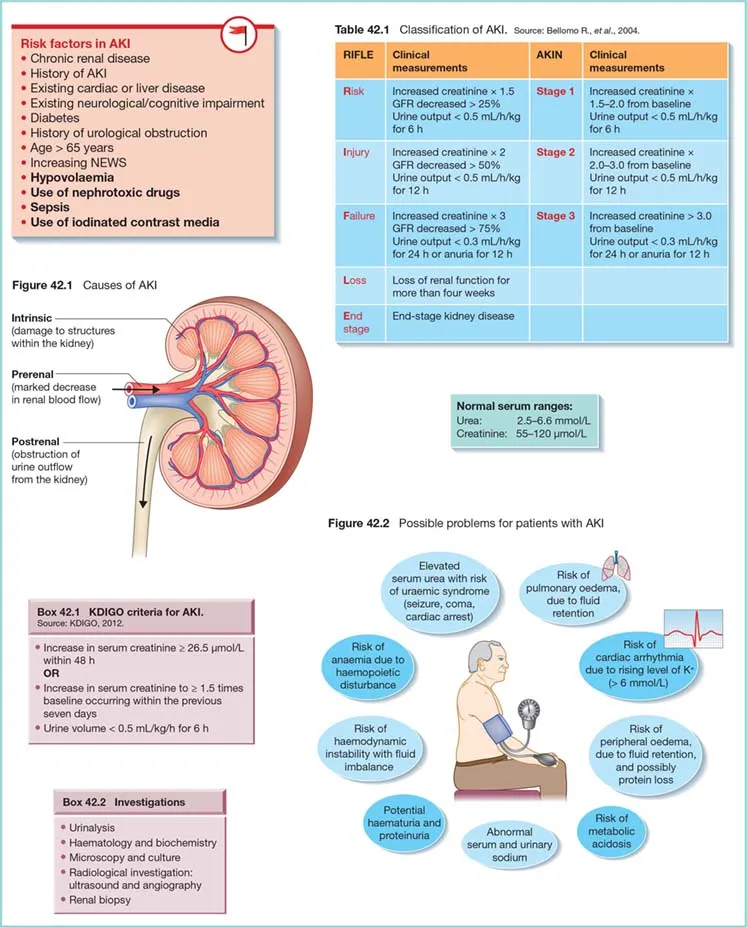
Acute kidney injury Explanation: ***Muddy brown casts***
- **Acute tubular necrosis (ATN)**, likely caused by **renal hypoperfusion** in the context of an aortic dissection, is characterized by the presence of **muddy brown granular casts** in urinalysis. The significantly elevated **creatinine (5.3 mg/dL)** and **oliguria** support a diagnosis of acute kidney injury with ATN.
- These casts are pathognomonic for ATN and are formed from shed **epithelial cells** and debris accumulating in the renal tubules.
*RBC casts*
- **Red blood cell (RBC) casts** are indicative of **glomerulonephritis** or other causes of **glomerular injury**, which are not directly suggested by the presentation of aortic dissection and subsequent oliguria.
- While hematuria can occur in various renal conditions, the presence of **RBC casts** points to bleeding originating from the glomerulus, which is a different pathology than ATN.
*Fatty casts*
- **Fatty casts** are typically associated with **nephrotic syndrome**, a condition characterized by significant proteinuria, hypoalbuminemia, and edema.
- There is no clinical information to suggest nephrotic syndrome in this patient, whose acute renal failure is likely due to hypoperfusion.
*Waxy casts*
- **Waxy casts** are generally indicative of **chronic kidney disease** and highly advanced, severe tubular damage, representing a later stage of kidney injury.
- While the patient has acute kidney injury, the timeline and acute nature of the insult make muddy brown casts more likely than waxy casts.
*Hyaline casts*
- **Hyaline casts** are composed primarily of Tamm-Horsfall mucoprotein, a normal protein secreted by renal tubule cells.
- These casts can be seen in normal urine, especially after exercise or dehydration, and are not specific for any particular kidney pathology or acute kidney injury.
Acute kidney injury US Medical PG Question 2: A 32-year-old man is brought to the emergency department after a car accident; he was extricated after 4 hours. He did not lose consciousness and does not have headache or nausea. He is in severe pain. He sustained severe injuries to both arms and the trauma team determines that surgical intervention is needed. Urinary catheterization shows dark colored urine. His temperature is 38°C (100.4°F), pulse is 110/min, and blood pressure is 90/60 mm Hg. The patient is alert and oriented. Examination shows multiple injuries to the upper extremities, contusions on the trunk, and abdominal tenderness. Laboratory studies show:
Hemoglobin 9.2 g/dL
Leukocyte count 10,900/mm3
Platelet count 310,000/mm3
Serum
Na+ 137 mEq/L
K+ 6.8 mEq/L
Cl- 97 mEq/L
Glucose 168 mg/dL
Creatinine 1.7 mg/dL
Calcium 7.7 mg/dL
Arterial blood gas analysis on room air shows a pH of 7.30 and a serum bicarbonate of 14 mEq/L. An ECG shows peaked T waves. A FAST scan of the abdomen is negative. Two large bore cannulas are inserted and intravenous fluids are administered. Which of the following is the most appropriate next step in management?
- A. Intravenous mannitol
- B. Intravenous sodium bicarbonate
- C. Packed red blood cell transfusion
- D. Intravenous calcium gluconate (Correct Answer)
- E. Intravenous insulin
Acute kidney injury Explanation: ***Intravenous calcium gluconate***
- The patient presents with severe **hyperkalemia** (K+ 6.8 mEq/L) and ECG changes (peaked T waves), indicating immediate cardiotoxicity risk. **Calcium gluconate** stabilizes the cardiac cell membranes, protecting the heart from the effects of high potassium.
- While other options address other issues, stabilizing the heart takes precedence in cases of extreme hyperkalemia with ECG changes.
*Intravenous mannitol*
- **Mannitol** is an osmotic diuretic used to reduce intracranial pressure or acute cerebral edema. The patient does not show signs or symptoms requiring this intervention (no consciousness loss, headache, or nausea).
- Its use here would not address the life-threatening hyperkalemia or cardiologic findings.
*Intravenous sodium bicarbonate*
- **Sodium bicarbonate** can help shift potassium intracellularly and correct metabolic acidosis, but its effect is slower and less reliable than calcium for immediate cardiac stabilization in severe hyperkalemia.
- The primary concern here is the acute cardiac risk, which calcium directly addresses.
*Packed red blood cell transfusion*
- The patient has a hemoglobin of 9.2 g/dL, indicating **anemia**, likely due to trauma. However, his blood pressure is 90/60 mm Hg despite intravenous fluids, suggesting ongoing hypovolemia or other shock.
- While addressing blood loss is important, the immediate life threat is the **cardiac instability due to hyperkalemia**, which must be managed first.
*Intravenous insulin*
- Insulin, often given with dextrose, helps shift potassium into cells. This is an effective treatment for hyperkalemia but does not provide immediate **cardiac membrane stabilization** like calcium gluconate.
- Given the peaked T waves, protecting the heart from arrhythmias is the most critical first step.
Acute kidney injury US Medical PG Question 3: A 52-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He was an unrestrained passenger who was ejected from the vehicle. On presentation, he is found to be actively bleeding from numerous wounds. His blood pressure is 76/42 mmHg and pulse is 152/min. Attempts at resuscitation fail, and he dies 25 minutes later. Autopsy shows blood in the peritoneal cavity, and histology of the kidney reveals swelling of the proximal convoluted tubule epithelial cells. Which of the following is most likely the mechanism underlying the renal cell findings?
- A. Decreased activity of caspase 7
- B. Increased activity of caspase 9
- C. Increased function of the Na+/K+-ATPase
- D. Increased activity of caspase 8
- E. Decreased function of the Na+/K+-ATPase (Correct Answer)
Acute kidney injury Explanation: ***Decreased function of the Na+/K+-ATPase***
- The patient experienced **hypovolemic shock** due to severe blood loss, leading to a significant drop in blood pressure and organ perfusion. This results in **ischemia** of the renal cells.
- **Ischemic injury** impairs ATP production, which is essential for the function of the **Na+/K+-ATPase pump**. Failure of this pump leads to intracellular accumulation of sodium and water, causing **cellular swelling**, particularly noticeable in the proximal convoluted tubules.
*Decreased activity of caspase 7*
- **Caspases**, including caspase 7, are involved in **apoptosis** (programmed cell death), which involves cell shrinkage and fragmentation, not the swelling observed here.
- Decreased caspase activity would generally *reduce* apoptosis, which is not the primary mechanism of acute cell injury in shock.
*Increased activity of caspase 9*
- Increased activity of **caspase 9** is indicative of the **intrinsic apoptotic pathway**, typically initiated by mitochondrial damage.
- While prolonged ischemia can eventually lead to apoptotic changes, the acute finding of **cellular swelling** points more directly to immediate membrane pump dysfunction due to ATP depletion.
*Increased function of the Na+/K+-ATPase*
- **Increased function** of the Na+/K+-ATPase would actively pump sodium out of the cell and potassium in, *preventing* intracellular swelling.
- This option contradicts the observed finding of proximal convoluted tubule epithelial cell swelling, which is characteristic of acute cellular injury due to pump failure.
*Increased activity of caspase 8*
- **Caspase 8** is a key initiator caspase in the **extrinsic apoptotic pathway**, often triggered by death receptor signaling.
- Similar to caspase 9, increased caspase 8 activity would lead to apoptosis, characterized by cell shrinkage, not the **cellular swelling** seen in acute ischemic injury.
Acute kidney injury US Medical PG Question 4: A 58-year-old man presents to the emergency department following a motor vehicle accident where he was an unrestrained passenger. On initial presentation in the field, he had diffuse abdominal tenderness and his blood pressure is 70/50 mmHg and pulse is 129/min. Following administration of 2 L of normal saline, his blood pressure is 74/58 mmHg. He undergoes emergency laparotomy and the source of the bleeding is controlled. On the second post-operative day, his blood pressure is 110/71 mmHg and pulse is 90/min. There is a midline abdominal scar with no erythema and mild tenderness. Cardiopulmonary examination is unremarkable. He has had 300 mL of urine output over the last 24 hours. Urinalysis shows 12-15 RBC/hpf, 2-5 WBC/hpf, and trace protein. What additional finding would you expect to see on urinalysis?
- A. WBC casts
- B. RBC casts
- C. Fatty casts
- D. Hyaline casts
- E. Muddy brown casts (Correct Answer)
Acute kidney injury Explanation: ***Muddy brown casts***
- The patient's history of **post-traumatic hypovolemic shock** leading to prolonged hypotension, coupled with **oliguria** and an elevated blood pressure on post-operative day 2, are highly suggestive of **acute tubular necrosis (ATN)**.
- **Muddy brown granular casts** are a hallmark finding of ATN, representing sloughed renal tubular cells and heme pigments.
*WBC casts*
- **WBC casts** are characteristic of **pyelonephritis** or **interstitial nephritis**, often accompanied by fever, flank pain, and significant pyuria, none of which are the primary presentation here.
- While there are some WBCs in the urine, the overall clinical picture does not point towards an infectious or inflammatory renal process as the primary cause of renal dysfunction.
*RBC casts*
- **RBC casts** indicate **glomerulonephritis** or severe tubular damage with hemorrhage, suggesting glomerular inflammation or a vasculitic process.
- While the urinalysis shows 12-15 RBC/hpf, the absence of other strong indicators of glomerular disease and the prominent history of shock make ATN a more likely diagnosis than glomerulonephritis.
*Fatty casts*
- **Fatty casts** are typically seen in **nephrotic syndrome**, associated with significant proteinuria (>3.5g/day), hyperlipidemia, and edema.
- The patient's trace proteinuria and the absence of other nephrotic syndrome features make this finding unlikely.
*Hyaline casts*
- **Hyaline casts** are composed of Tamm-Horsfall mucoprotein and can be found in **healthy individuals** as well as in states of **dehydration** or mild renal injury.
- While the patient was likely dehydrated, hyaline casts are non-specific and do not explain the degree of renal dysfunction and oliguria observed in this case.
Acute kidney injury US Medical PG Question 5: A 67-year-old man comes to the emergency department for the evaluation of two episodes of red urine since this morning. He has no pain with urination. He reports lower back pain and fever. Six months ago, he was diagnosed with osteoarthritis of the right knee that he manages with 1–2 tablets of ibuprofen per day. He has smoked one pack of cigarettes daily for the past 45 years. He does not drink alcohol. His temperature is 38.5°C (101.3°F), pulse is 95/min, and blood pressure is 130/80 mm Hg. Physical examination shows faint, diffuse maculopapular rash, and bilateral flank pain. The remainder of the examination shows no abnormalities. Urinalysis shows:
Blood +3
Protein +1
RBC 10–12/hpf
RBC cast negative
Eosinophils numerous
Which of the following is the most likely diagnosis?
- A. Acute glomerulonephritis
- B. Renal cell carcinoma
- C. Acute tubular necrosis
- D. Acute tubulointerstitial nephritis (Correct Answer)
- E. Crystal-induced acute kidney injury
Acute kidney injury Explanation: ***Acute tubulointerstitial nephritis***
- The patient's history of daily **ibuprofen use**, along with **fever**, **rash**, **flank pain**, and **eosinophilia** in the urine, is highly suggestive of **acute tubulointerstitial nephritis (ATIN)**, often drug-induced.
- The urinalysis showing **hematuria** (+3 blood, 10-12 RBCs/hpf), **proteinuria** (+1 protein), and significantly **numerous eosinophils** further supports this diagnosis, as ATIN is characterized by inflammation of the renal tubules and interstitium.
*Acute glomerulonephritis*
- While acute glomerulonephritis can present with hematuria and proteinuria, it typically involves the presence of **RBC casts**, which are noted as negative in this patient's urinalysis.
- The significant eosinophilia and response to ibuprofen are not characteristic features of acute glomerulonephritis.
*Renal cell carcinoma*
- Renal cell carcinoma can cause painless hematuria and flank pain, but it is less likely to present with acute symptoms such as **fever**, **rash**, and **eosinophilia**.
- This condition does not typically cause the diffuse maculopapular rash or the specific urinalysis findings of numerous eosinophils.
*Acute tubular necrosis*
- Acute tubular necrosis (ATN) is often associated with ischemia or nephrotoxic agents and typically presents with muddy brown casts in the urine, not red blood cell casts or numerous eosinophils.
- While ATN can cause acute kidney injury, the rash, fever, and eosinophils point away from this diagnosis.
*Crystal-induced acute kidney injury*
- Crystal-induced AKI might occur with certain drugs or metabolic conditions and would typically show evidence of crystals in the urine (e.g., uric acid, oxalate), which are not mentioned here.
- The presence of fever, rash, and marked eosinophilia is not typical for crystal-induced injury.
Acute kidney injury US Medical PG Question 6: A 48-year-old man is brought to the emergency department by his wife because of a 3-day history of increasing confusion and lethargy. He complains of decreased urine output and abdominal pain for the past month. Two months ago, he was hospitalized for pyelonephritis and treated with ceftriaxone. He has a history of chronic hepatitis C. He does not take any medications. He appears pale and irritable. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 98/60 mm Hg. On mental status examination, he is oriented to person but not to time or place. Physical examination shows scleral icterus and jaundice. There is 2+ pitting edema of the lower extremities. The abdomen is distended with a positive fluid wave. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 4300/mm3
Platelet count 89,000/mm3
Prothrombin time 19 sec
Serum
Urea nitrogen 71 mg/dL
Glucose 99 mg/dL
Creatinine 3.5 mg/dL
ALT 137 mg/dL
AST 154 mg/dL
Urinalysis shows no abnormalities. The FeNa is < 1%. Ultrasound of the kidneys is unremarkable. Intravenous fluids are administered for 36 hours but do not improve urine output. Which of the following is the most likely cause of the kidney dysfunction in this patient?
- A. Renal vein thrombosis
- B. Renal tubular injury
- C. Renal microvascular thrombi
- D. Decreased renal perfusion (Correct Answer)
- E. Renal interstitial inflammation
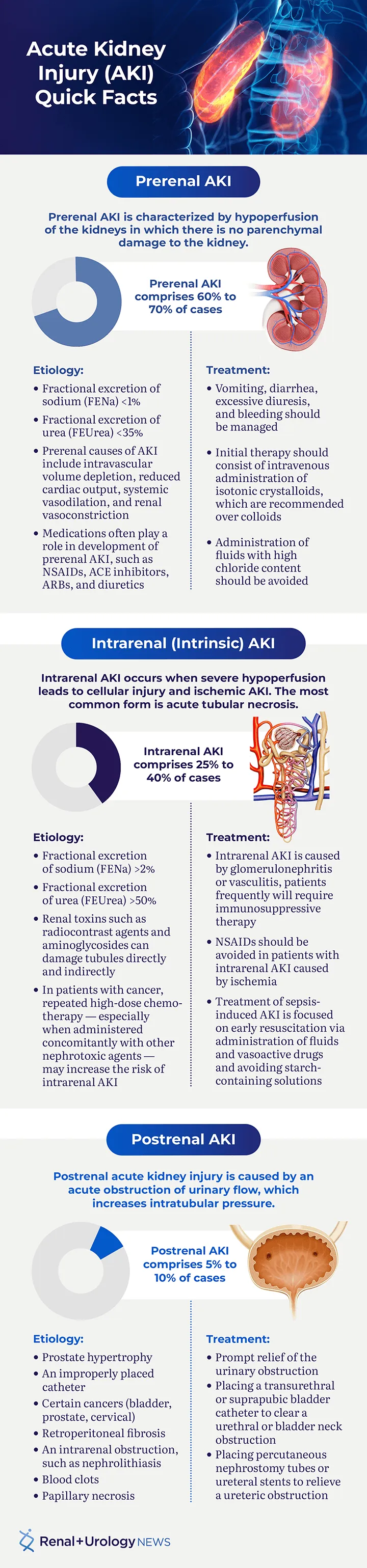
Acute kidney injury Explanation: ***Decreased renal perfusion***
- The patient's history of **chronic hepatitis C** with signs of **liver dysfunction** (jaundice, scleral icterus, distended abdomen with fluid wave, prolonged PT, thrombocytopenia, confusion) suggests **cirrhosis** and portal hypertension, leading to **hepatorenal syndrome (HRS)**.
- **HRS** is characterized by severe **renal vasoconstriction** due to systemic vasodilation and decreased effective arterial blood volume, leading to impaired renal perfusion and function that does **not respond to fluid resuscitation**, as seen in this patient.
- The **low FeNa (<1%)** reflects avid sodium retention, **unremarkable urinalysis** excludes intrinsic renal disease, and **lack of improvement with 36 hours of IV fluids** confirms the diagnosis.
*Renal vein thrombosis*
- This condition is often associated with **nephrotic syndrome** or hypercoagulable states, typically presenting with **flank pain**, hematuria, and a sudden decline in renal function.
- The patient's clinical picture and laboratory findings (e.g., **negative urinalysis**, **low FeNa**, **no response to volume expansion**) are not typical for renal vein thrombosis, which would show abnormal imaging findings.
*Renal tubular injury*
- **Acute tubular necrosis (ATN)**, a form of renal tubular injury, typically occurs after **ischemic or nephrotoxic insults** and is characterized by muddy brown granular casts on urinalysis and a **high FeNa (>2%)**.
- In this case, the **unremarkable urinalysis** and **FeNa <1%** argue against ATN or other primary tubular injury as the cause of acute kidney injury.
*Renal microvascular thrombi*
- Conditions involving renal microvascular thrombi, such as **thrombotic microangiopathy**, often present with **thrombocytopenia**, microangiopathic hemolytic anemia (schistocytes), and severe hypertension.
- While the patient has thrombocytopenia, there is **no evidence of hemolysis** or other features typical of primary microvascular thrombi, and the clinical context points to liver disease as the primary etiology.
*Renal interstitial inflammation*
- **Acute interstitial nephritis (AIN)** is usually drug-induced (e.g., antibiotics, NSAIDs) and presents with **eosinophilia**, rash, fever, and white blood cell casts in the urine.
- The patient's presentation does not include these findings, and the **unremarkable urinalysis** makes AIN less likely. The recent ceftriaxone treatment was 2 months ago, making drug-induced AIN temporally unlikely.
Acute kidney injury US Medical PG Question 7: A 32-year-old man is brought to the Emergency Department after 3 consecutive days of diarrhea, fatigue and weakness. His stool has been soft and mucoid, with no blood stains. The patient just came back from a volunteer mission in Guatemala, where he remained asymptomatic. His personal medical history is unremarkable. Today his blood pressure is 98/60 mm Hg, pulse is 110/min, respiratory rate is 19/min, and his body temperature is 36.7°C (98.1°F). On physical exam, he has sunken eyes, dry mucosa, mild diffuse abdominal tenderness, and hyperactive bowel sounds. Initial laboratory tests are shown below:
Serum creatinine (SCr) 1.8 mg/dL
Blood urea nitrogen (BUN) 50 mg/dL
Serum sodium 132 mEq/L
Serum potassium 3.5 mEq/L
Serum chloride 102 mEq/L
Which of the following phenomena would you expect in this patient?
- A. Low urine osmolality, high FeNa+, high urine Na+
- B. High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+
- C. Low urine osmolality, high FeNa+, low urine Na+
- D. High urine osmolality, low FeNa+, low urine Na+ (Correct Answer)
- E. Low urine osmolality, low FeNa+, high urine Na+
Acute kidney injury Explanation: ***High urine osmolality, low FeNa+, low urine Na+***
- The patient exhibits signs of **dehydration** (hypotension, tachycardia, sunken eyes, dry mucosa) and **acute kidney injury (AKI)** with elevated BUN and creatinine, particularly a **BUN/creatinine ratio of 27.8** (50/1.8). These findings point to **prerenal AKI** due to hypovolemia from diarrhea.
- In prerenal AKI, the kidneys attempt to conserve water and sodium to restore intravascular volume. This leads to **increased ADH** secretion and **aldosterone**, resulting in **high urine osmolality** (concentrated urine), **low fractional excretion of sodium (FeNa+)** (<1%), and **low urine sodium concentration** (<20 mEq/L).
*Low urine osmolality, high FeNa+, high urine Na+*
- This pattern is typical of **acute tubular necrosis (ATN)**, an intrinsic cause of AKI, where tubular damage impairs the kidney's ability to concentrate urine and reabsorb sodium.
- The context of dehydration and prerenal state makes ATN less likely as the initial primary pathology compared to the body's compensatory mechanisms during hypovolemia.
*High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+*
- This combination is generally contradictory. High urine osmolality suggests water conservation, while high FeNa+ and urine Na+ indicate sodium wasting, which would typically be seen in diuretic use or specific renal tubular disorders, not uncompensated hypovolemia.
- In prerenal AKI, the body actively reabsorbs sodium to expand volume, leading to low rather than high FeNa+ and urine Na+.
*Low urine osmolality, high FeNa+, low urine Na+*
- This combination is inconsistent. High FeNa+ and low urine Na+ do not usually occur together in a state of hypovolemia. If FeNa+ is high, it implies significant sodium excretion, which would typically be accompanied by higher urine Na+.
- Low urine osmolality also suggests impaired concentrating ability, which is not characteristic of the compensatory mechanisms in prerenal AKI.
*Low urine osmolality, low FeNa+, high urine Na+*
- This combination is also contradictory. Low urine osmolality with low FeNa+ and high urine Na+ does not align with typical kidney responses to dehydration or specific AKI etiologies.
- Low FeNa+ and high urine Na+ are conflicting, as low FeNa+ implies sodium conservation, while high urine Na+ indicates sodium excretion.
Acute kidney injury US Medical PG Question 8: A 63-year-old man undergoes uncomplicated laparoscopic cholecystectomy for acute cholecystitis and is admitted to the surgical ward for postoperative management. On postoperative day 1, routine laboratory studies reveal an increase in serum creatinine to 1.46 mg/dL from 0.98 mg/dL before the operation; BUN is 37 mg/dL, increased from 18 mg/dL on prior measurement; K is 4.8 mEq/L and CO2 is 19 mEq/L. The patient has an indwelling urinary catheter in place, draining minimal urine over the last few hours. Which of the following is the most appropriate next step in management?
- A. Initiate emergent hemodialysis
- B. Obtain bilateral renal ultrasonography
- C. Obtain urinalysis
- D. Evaluate urinary catheter for obstruction (Correct Answer)
- E. Administer IV fluid bolus
Acute kidney injury Explanation: ***Evaluate urinary catheter for obstruction***
- The patient presents with **acute kidney injury (AKI)** evidenced by elevated BUN and creatinine, along with minimal urine output, raising suspicion for a **post-renal obstruction**.
- Given the presence of an indwelling urinary catheter, a **mechanical obstruction** (e.g., kink, clot) is the most immediate and easily reversible cause to investigate.
*Initiate emergent hemodialysis*
- While the patient has AKI, there are no immediate life-threatening indications for **emergent hemodialysis** such as severe hyperkalemia, refractory acidosis, or pulmonary edema.
- Furthermore, investigating and potentially reversing the cause of AKI should precede considering dialysis.
*Obtain bilateral renal ultrasonography*
- **Renal ultrasonography** is appropriate for evaluating post-renal causes after simpler causes of obstruction, such as a catheter issue, have been ruled out.
- It would be used to assess for hydronephrosis, which indicates **ureteral or bladder outlet obstruction**.
*Obtain urinalysis*
- A **urinalysis** can help characterize intrinsic renal causes of AKI (e.g., ATN, interstitial nephritis) but is less helpful in initial assessment of a suspected acute obstruction related to a catheter.
- The immediate priority is to rule out a mechanical issue with the indwelling catheter.
*Administer IV fluid bolus*
- The patient's BUN/creatinine ratio (approximately 25:1) suggests a potential **pre-renal etiology** (volume depletion), but the minimal urine output with an indwelling catheter warrants ruling out obstruction first.
- Administering fluids without addressing a potential obstruction could worsen patient outcome if the obstruction is present.
Acute kidney injury US Medical PG Question 9: A 49-year-old woman presents to the emergency room with bloody stool and malaise. She developed a fever and acute left lower quadrant abdominal pain earlier in the day. She has had 2 bowel movements with bright red blood. Her past medical history is notable for hyperlipidemia, hypertension, and diabetes mellitus. She takes lovastatin, hydrochlorothiazide, metformin, glyburide, and aspirin. Her temperature is 102.9°F (39.4°C), blood pressure is 101/61 mmHg, pulse is 110/min, and respirations are 22/min. On exam, she is fully alert and oriented. She is tender in the left lower quadrant. A computerized tomography (CT) scan is performed demonstrating acute diverticulitis. She is admitted and started on broad-spectrum antibiotics. 48 hours later, her urine output is significantly decreased. Her abdominal pain has improved but she has started vomiting and appears confused. She has new bilateral lower extremity edema and decreased breath sounds at the lung bases. Laboratory analysis upon admission and 48 hours later is shown below:
Admission:
Hemoglobin: 11.9 g/dl
Hematocrit: 34%
Leukocyte count: 11,500/mm^3
Platelet count: 180,000/ mm^3
Serum:
Na+: 141 mEq/L
Cl-: 103 mEq/L
K+: 4.5 mEq/L
HCO3-: 23 mEq/L
BUN: 21 mg/dL
Glucose: 110 mg/dL
Creatinine: 0.9 mg/dL
48 hours later:
Hemoglobin: 10.1 g/dl
Hematocrit: 28%
Leukocyte count: 11,500 cells/mm^3
Platelet count: 195,000/ mm^3
Serum:
Na+: 138 mEq/L
Cl-: 100 mEq/L
K+: 5.1 mEq/L
HCO3-: 24 mEq/L
BUN: 30 mg/dL
Glucose: 120 mg/dL
Creatinine: 2.1 mg/dL
Which of the following findings would most likely be seen on urine microscopy?
- A. Waxy casts
- B. Muddy brown casts (Correct Answer)
- C. White blood cell casts
- D. Fatty casts
- E. Hyaline casts
Acute kidney injury Explanation: ***Muddy brown casts***
- The patient's presentation with **acute kidney injury** (creatinine rising from 0.9 to 2.1 mg/dL in 48 hours) along with signs of **sepsis** (fever, hypotension, altered mental status, decreased urine output) strongly suggests **acute tubular necrosis (ATN)**, a common cause of intrinsic renal failure.
- **Muddy brown casts** composed of degenerating renal tubular epithelial cells and granular material are pathognomonic for **acute tubular necrosis** and indicate significant tubular damage.
*Waxy casts*
- **Waxy casts** are typically associated with **chronic renal failure** and advanced renal disease, indicating prolonged tubular stasis and severe urine flow reduction.
- While the patient has acute kidney injury, her history does not suggest pre-existing chronic kidney disease to this extent.
*White blood cell casts*
- **White blood cell casts** are characteristic of **interstitial nephritis** or **pyelonephritis**, indicating inflammation or infection within the kidney parenchyma.
- Although the patient has a possible infection (diverticulitis, sepsis), the rapid decline in renal function with a clear rise in creatinine points more directly to ATN rather than primarily interstitial inflammation.
*Fatty casts*
- **Fatty casts** are typically seen in **nephrotic syndrome**, a condition characterized by massive proteinuria, hypoalbuminemia, and significant edema.
- The patient's symptoms are more consistent with acute kidney injury due to sepsis, and there is no information to suggest nephrotic-range proteinuria.
*Hyaline casts*
- **Hyaline casts** can be found in **healthy individuals** from concentrated urine or after exercise and are non-specific, indicating only mild tubular protein aggregation.
- They are not indicative of significant renal pathology like ATN and would not explain the patient's acute and severe renal deterioration.
Acute kidney injury US Medical PG Question 10: A 45-year-old homeless man is brought to the emergency department by the police. He was found intoxicated and passed out in a library. The patient has a past medical history of IV drug abuse, diabetes, alcohol abuse, and malnutrition. The patient has been hospitalized previously for multiple episodes of pancreatitis and sepsis. Currently, the patient is minimally responsive and only withdraws his extremities in response to painful stimuli. His temperature is 99.5°F (37.5°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam is notable for tachycardia, a diastolic murmur at the left lower sternal border, and bilateral crackles on pulmonary exam. The patient is started on IV fluids, vancomycin, and piperacillin-tazobactam. Laboratory values are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 30%
Leukocyte count: 11,500/mm^3 with normal differential
Platelet count: 297,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.0 mEq/L
HCO3-: 28 mEq/L
BUN: 33 mg/dL
Glucose: 60 mg/dL
Creatinine: 1.7 mg/dL
Ca2+: 9.7 mg/dL
PT: 20 seconds
aPTT: 60 seconds
AST: 1,010 U/L
ALT: 950 U/L
The patient is admitted to the medical floor. Five days later, the patient's neurological status has improved. His temperature is 99.5°F (37.5°C), blood pressure is 130/90 mmHg, pulse is 90/min, respirations are 11/min, and oxygen saturation is 99% on room air. Laboratory values are repeated as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 32%
Leukocyte count: 9,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 102 mEq/L
K+: 4.3 mEq/L
HCO3-: 24 mEq/L
BUN: 31 mg/dL
Glucose: 100 mg/dL
Creatinine: 1.6 mg/dL
Ca2+: 9.0 mg/dL
PT: 40 seconds
aPTT: 90 seconds
AST: 150 U/L
ALT: 90 U/L
Which of the following is the best description of this patient’s current status?
- A. Recovery from acute renal failure
- B. Acute renal failure
- C. Recovery from ischemic liver disease
- D. Fulminant liver failure (Correct Answer)
- E. Recovery from acute alcoholic liver disease
Acute kidney injury Explanation: ***Fulminant liver failure***
- The patient's **prolonged PT (40 seconds)** and **aPTT (90 seconds)** after 5 days, despite improvements in other parameters, indicate a severe impairment in hepatic synthesis of clotting factors, which is a hallmark of **fulminant liver failure**.
- The initial presentation with **elevated AST/ALT (over 1000 U/L)** coupled with **encephalopathy (minimally responsive)** and subsequent worsening coagulopathy points towards acute liver failure, even if transaminases are improving.
*Recovery from acute renal failure*
- While the initial **creatinine (1.7 mg/dL)** was mildly elevated, it remained largely unchanged (1.6 mg/dL) after 5 days, indicating no significant acute renal failure or subsequent recovery.
- The patient’s fluid resuscitation and improved hemodynamics would likely lead to a more pronounced improvement in creatinine if significant acute renal failure had occurred and was recovering.
*Acute renal failure*
- The creatinine level, while slightly elevated, does not meet the criteria for significant **acute renal failure** (e.g., a >50% increase from baseline or a >0.3 mg/dL increase within 48 hours relative to his baseline, which is unknown but likely lower than 1.7 mg/dL given his other conditions).
- Furthermore, if true acute renal failure was present on admission, 5 days later with improved vitals, we would expect a clearer trend of either worsening or recovering creatinine, neither of which is strongly evident here.
*Recovery from ischemic liver disease*
- While the initial very high transaminases (AST 1010, ALT 950) could suggest **ischemic liver injury**, the subsequent significant prolongation of **PT and aPTT** (from 20 to 40 seconds and 60 to 90 seconds, respectively) indicates worsening synthetic dysfunction, not recovery.
- Recovery from ischemic liver disease would typically show improving coagulation parameters alongside decreasing transaminases.
*Recovery from acute alcoholic liver disease*
- Similar to recovery from ischemic liver disease, recovery from **acute alcoholic liver disease** would involve an improvement in liver synthetic function, reflected by a **shortening of PT/aPTT**, not a progressive prolongation as seen here.
- The patient's initial presentation is consistent with acute alcoholic hepatitis or other acute liver injury given his history and high LFTs, but the subsequent worsening coagulopathy rules out recovery.
More Acute kidney injury US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.