Viral hepatitis (A, B, C, D, E) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Viral hepatitis (A, B, C, D, E). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 1: A 28-year-old woman with a history of intravenous drug use is brought to the emergency department because of a 1-day history of fatigue, yellow eyes, confusion, and blood in her stools. She appears ill. Her temperature is 38.1°C (100.6°F). Physical examination shows pain in the right upper quadrant, diffuse jaundice with scleral icterus, and bright red blood in the rectal vault. Further evaluation demonstrates virions in her blood, some of which have a partially double-stranded DNA genome while others have a single-stranded RNA genome. They are found to share an identical lipoprotein envelope. This patient is most likely infected with which of the following pathogens?
- A. Deltavirus (Correct Answer)
- B. Filovirus
- C. Calicivirus
- D. Hepevirus
- E. Herpesvirus
Viral hepatitis (A, B, C, D, E) Explanation: ***Deltavirus***
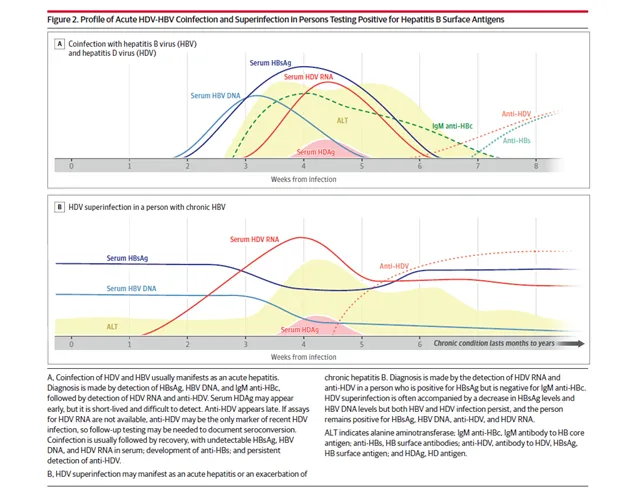
- The presence of both **partially double-stranded DNA virions** (Hepatitis B virus) and **single-stranded RNA virions** (Hepatitis D virus) sharing an identical lipoprotein envelope is pathognomonic for **coinfection with Hepatitis B and Deltavirus (HDV)** [1].
- **Hepatitis D (Deltavirus)** is a **defective RNA virus** that is obligately dependent on **Hepatitis B surface antigen (HBsAg)** for its replication, assembly, and transmission—explaining why both viruses share the same lipoprotein envelope [1].
- This coinfection or superinfection with HDV causes **more severe acute hepatitis** and higher rates of **fulminant hepatic failure** compared to HBV alone, consistent with the patient's presentation of jaundice, confusion (hepatic encephalopathy), and GI bleeding [1].
- The patient's **IV drug use** is a key risk factor for both HBV and HDV transmission [1].
*Filovirus*
- **Filoviruses** (e.g., Ebola, Marburg) cause **viral hemorrhagic fever** with severe bleeding manifestations and can present with bloody stools.
- However, they are **single-stranded RNA viruses** only and do not involve coinfection with a DNA virus, nor do they share envelopes with DNA viruses.
- Geographic exposure and clinical context (African hemorrhagic fever outbreaks) would be expected.
*Calicivirus*
- **Caliciviruses** (e.g., Norovirus, Sapovirus) are **non-enveloped, single-stranded RNA viruses** that cause acute **gastroenteritis** with vomiting and diarrhea.
- They do not cause hepatitis with jaundice and hepatic encephalopathy, nor do they involve DNA virus coinfection or envelope sharing.
*Hepevirus*
- **Hepatitis E virus (Hepevirus)** is a **non-enveloped, single-stranded RNA virus** that causes acute hepatitis, primarily through **fecal-oral transmission** (contaminated water).
- While it causes liver disease, it does not involve coinfection with a DNA virus or envelope sharing, and it is not typically associated with IV drug use.
- It can cause severe disease in pregnant women but does not explain the dual genome findings.
*Herpesvirus*
- **Herpesviruses** are **enveloped, double-stranded DNA viruses** that cause various infections (HSV, VZV, EBV, CMV).
- While they have DNA genomes and envelopes, they do not coinfect with RNA viruses sharing the same envelope structure, nor are they typically associated with acute severe hepatitis in IV drug users.
- Hepatitis from CMV or EBV would have different serologic and molecular findings.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 2: A 52-year-old male patient with chronic alcoholism presents to an ambulatory medical clinic, where the hepatologist elects to perform comprehensive hepatitis B screening, in addition to several other screening and preventative measures. Given the following choices, which serologic marker, if positive, would indicate the patient’s immunity to the hepatitis B virus?
- A. HBeAb
- B. HBeAg
- C. HBsAb (Correct Answer)
- D. HBsAg
- E. HBcAb
Viral hepatitis (A, B, C, D, E) Explanation: ***HBsAb***
- A positive **HBsAb** (Hepatitis B surface antibody) indicates immunity to hepatitis B virus, either from successful **vaccination** or **recovery from past infection**.
- This antibody provides **protective immunity** against future HBV infection and is the definitive marker of immunity.
*HBeAb*
- **HBeAb** (Hepatitis B e antibody) indicates **seroconversion** from HBeAg during chronic HBV infection, suggesting lower viral replication.
- It does **not confer immunity** against the virus itself and only reflects a phase of chronic infection.
*HBeAg*
- **HBeAg** (Hepatitis B e antigen) indicates **active viral replication** with high infectivity during ongoing hepatitis B infection.
- Its presence signifies a **replicative phase** of infection and increased risk of transmission to others.
*HBsAg*
- **HBsAg** (Hepatitis B surface antigen) indicates **active hepatitis B infection**, whether acute or chronic.
- This antigen is the **first serologic marker** to appear following exposure and confirms presence of the virus.
*HBcAb*
- **HBcAb** (Hepatitis B core antibody) indicates **previous or current exposure** to hepatitis B virus.
- It does **not differentiate** between acute, chronic, or resolved infection and does not confer protective immunity.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 3: A 28-year-old woman comes to the emergency department for a 1-week history of jaundice and nausea. She recalls eating some seafood last weekend at a cookout. She lives at home with her 2-year-old son who attends a daycare center. The child's immunizations are up-to-date, and his last hepatitis A vaccine was administered 6 weeks ago. The woman's temperature is 37.5°C (99.5°F), pulse is 82/min, and blood pressure is 134/84 mm Hg. Examination shows scleral icterus. The liver is palpated 2-cm below the right costal margin and is tender. Her serum studies show:
Total bilirubin 3.4 mg/dL
Alkaline phosphatase 89 U/L
AST 185 U/L
ALT 723 U/L
Hepatitis A IgM antibody positive
Hepatitis B surface antibody positive
Hepatitis B surface antigen negative
Hepatitis B core IgM antibody negative
Hepatitis C antibody negative
Which of the following health maintenance recommendations is most appropriate for the child at this time?
- A. Isolate the child
- B. Administer hepatitis B immunoglobulin and hepatitis B vaccine
- C. No additional steps are needed (Correct Answer)
- D. Administer hepatitis B immunoglobulin only
- E. Administer hepatitis A vaccine and hepatitis A immunoglobulin
Viral hepatitis (A, B, C, D, E) Explanation: ***No additional steps are needed***
- The child received his **last hepatitis A vaccine 6 weeks ago**, which provides adequate protection against hepatitis A infection.
- According to **CDC/ACIP guidelines**, children who have received **at least one dose** of hepatitis A vaccine do **not require post-exposure prophylaxis** (neither additional vaccine nor immunoglobulin) after exposure to hepatitis A.
- One dose of hepatitis A vaccine provides protection within **2-4 weeks**, and since 6 weeks have elapsed, the child is already immune.
- The child's **immunizations are up-to-date**, confirming he is on the appropriate hepatitis A vaccination schedule (2-dose series).
*Administer hepatitis A vaccine and hepatitis A immunoglobulin*
- This would be appropriate for **previously unvaccinated** individuals exposed to hepatitis A, immunocompromised patients, or infants under 12 months.
- However, this child has **already been vaccinated** 6 weeks ago and therefore has adequate protection.
- Administering both vaccine and immunoglobulin is **unnecessary** and not indicated per current guidelines when prior vaccination has occurred.
*Isolate the child*
- Isolation is not the primary recommendation for hepatitis A post-exposure management in household contacts.
- The focus should be on **prevention through immunization**, but this child is already protected by prior vaccination.
- Standard hygiene measures (handwashing) are recommended but formal isolation is not necessary.
*Administer hepatitis B immunoglobulin and hepatitis B vaccine*
- The mother's serology shows **HBsAg negative** and **HBsAb positive**, indicating she is **immune to hepatitis B** (likely from prior vaccination) and not currently infected.
- There is **no risk of hepatitis B transmission** from the mother to the child.
- This intervention addresses the wrong infection entirely.
*Administer hepatitis B immunoglobulin only*
- This is inappropriate because the mother does **not have active hepatitis B infection** (HBsAg negative).
- This option does not address the **hepatitis A exposure**, which is the relevant concern in this scenario.
- Hepatitis B immunoglobulin is indicated only for exposure to hepatitis B, not hepatitis A.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 4: A 28-year-old man presents to the office with complaints of malaise, anorexia, and vomiting for the past 2 weeks. He also says that his urine is dark. The past medical history is unremarkable. The temperature is 36.8°C (98.2°F), the pulse is 72/min, the blood pressure is 118/63 mm Hg, and the respiratory rate is 15/min. The physical examination reveals a slightly enlarged, tender liver. No edema or spider angiomata are noted. Laboratory testing showed the following:
HBsAg Positive
IgM anti-HBc < 1:1,000
Anti-HBs Negative
HBeAg Positive
Anti-HBe Negative
HBV DNA 2.65 × 10⁹ IU/L
Alpha-fetoprotein 125 ng/mL
What is the most likely cause of this patient's condition?
- A. Acute HBV infection
- B. Passive immunity
- C. Acute resolving infection
- D. Resolved HBV infection (innate immunity)
- E. Acute exacerbation of chronic HBV infection (Correct Answer)
Viral hepatitis (A, B, C, D, E) Explanation: ***Acute exacerbation of chronic HBV infection***
- The combination of **HBsAg positive** (indicating extant infection) and **IgM anti-HBc < 1:1,000** (a low titer consistent with chronic infection, not acute) points towards a pre-existing chronic hepatitis B infection.
- The elevated **HBV DNA (2.65 × 109 IU/L)**, along with clinical symptoms like malaise, anorexia, vomiting, dark urine, and a tender liver, suggests an **acute exacerbation** of this chronic condition.
*Acute HBV infection*
- An acute HBV infection would typically present with a **high titer of IgM anti-HBc** and often **HBeAg positive** initially, but this patient's low IgM anti-HBc titer rules out a new acute infection.
- While symptoms align with acute hepatitis, the serology (low IgM anti-HBc) is not characteristic of primary acute infection.
*Passive immunity*
- Passive immunity would be characterized by the presence of **Anti-HBs without HBsAg**, which is not seen here.
- This scenario usually occurs after receiving hepatitis B immunoglobulin or transplacental transfer of antibodies.
*Acute resolving infection*
- A resolving acute infection would typically show a **decrease in HBsAg** and the **presence of Anti-HBs**, neither of which are observed in this patient.
- The **high viral load (HBV DNA)** and persistent HBsAg also contradict a resolving infection.
*Resolved HBV infection (innate immunity)*
- A resolved HBV infection is defined by the **absence of HBsAg** and the **presence of Anti-HBs**, along with anti-HBc.
- This patient still has **HBsAg present** and **Anti-HBs negative**, ruling out a resolved infection.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 5: A 35-year-old man with no known past medical history presents to his physician because he is applying for a job as a healthcare worker, which requires screening for the hepatitis B virus (HBV). The patient states that he is in good health and denies any symptoms. His vital signs and physical exam are unremarkable. Labs are drawn, and the patient's HBV serology shows the following:
HBsAg: positive
anti-HBsAg antibody: negative
anti-HBcAg IgM: negative
anti-HBcAg IgG: positive
HBeAg: negative
anti-HBeAg antibody: positive
Which of the following best describes this patient's results?
- A. Immune due to previous infection
- B. Chronically infected, low infectivity (Correct Answer)
- C. Immune due to previous vaccination
- D. Acutely infected
- E. Chronically infected, high infectivity
Viral hepatitis (A, B, C, D, E) Explanation: ***Chronically infected, low infectivity***
- The presence of **HBsAg positive** for more than 6 months indicates **chronic HBV infection**. The presence of **anti-HBeAg antibody** and **negative HBeAg** suggests **low viral replication activity** and thus low infectivity.
- **HBeAg negativity** along with positivity for **HBV DNA** (if tested, though not provided here) would further differentiate this state as **"HBeAg-negative chronic hepatitis B,"** which typically implies lower, but still present, infectivity compared to HBeAg-positive chronic infection.
*Immune due to previous infection*
- Immunity due to previous infection is characterized by **negative HBsAg** and **positive anti-HBsAg antibody**, along with **positive anti-HBcAg IgG**.
- This patient, however, is **HBsAg positive** and **anti-HBsAg antibody negative**, ruling out resolved infection.
*Immune due to previous vaccination*
- Immunity due to vaccination is characterized by **negative HBsAg**, **positive anti-HBsAg antibody**, and **negative anti-HBcAg antibody** (both IgM and IgG).
- This patient has **positive HBsAg** and **positive anti-HBcAg IgG**, indicating either current or past infection, not vaccination-induced immunity.
*Acutely infected*
- **Acute infection** is characterized by **positive HBsAg**, **negative anti-HBsAg antibody**, and typically **positive anti-HBcAg IgM**.
- This patient has **negative anti-HBcAg IgM**, which makes acute infection unlikely, as IgM antibodies are present early in acute infection.
*Chronically infected, high infectivity*
- **High infectivity** in chronic HBV infection is typically indicated by **positive HBsAg** and **positive HBeAg**, often with high levels of HBV DNA.
- This patient is **HBeAg negative** and **anti-HBeAg antibody positive**, indicating a lower level of viral replication and thus lower infectivity.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 6: A 25-year-old man presents to the office for a 3-day history of fever and fatigue. Upon further questioning, he says that he also had constant muscular pain, headaches, and fever during these days. He adds additional information by giving a history of regular unprotected sexual relationship with multiple partners. He is a non-smoker and drinks alcohol occasionally. The heart rate is 102/min, respiratory rate is 18/min, temperature is 38.0°C (100.4°F), and blood pressure is 120/80 mm Hg. On physical examination, he is icteric and hepatosplenomegaly is evident with diffuse muscular and abdominal tenderness particularly in the right upper quadrant. The serologic markers show the following pattern:
Anti-HAV IgM negative
HBsAg positive
Anti-HBs negative
IgM anti-HBc positive
Anti-HCV negative
Anti-HDV negative
What is the most likely diagnosis?
- A. Viral hepatitis D
- B. Viral hepatitis C
- C. Viral hepatitis A
- D. Viral hepatitis E
- E. Viral hepatitis B (Correct Answer)
Viral hepatitis (A, B, C, D, E) Explanation: ***Viral hepatitis B***
- The combination of **HBsAg positive** and **IgM anti-HBc positive** indicates an **acute hepatitis B infection**.
- Symptoms like **fever**, **fatigue**, **muscular pain**, **icterus**, and **hepatosplenomegaly** are consistent with acute viral hepatitis.
*Viral hepatitis D*
- This is ruled out by the **negative Anti-HDV** marker, as hepatitis D requires co-infection with hepatitis B.
- While patients can be co-infected with HBV and HDV, the serology explicitly excludes HDV in this case.
*Viral hepatitis C*
- This is excluded by the **negative Anti-HCV** marker, which would be positive in hepatitis C infection.
- Though sexually transmitted, the serological markers point away from HCV.
*Viral hepatitis A*
- This is ruled out by the **negative Anti-HAV IgM** marker.
- Hepatitis A is typically transmitted via the **fecal-oral route**, which is less consistent with the patient's sexual history.
*Viral hepatitis E*
- While hepatitis E can cause acute hepatitis, it is typically diagnosed by **IgM anti-HEV** antibodies, which are not provided as positive here.
- Transmission is usually **fecal-oral**, which is not the primary risk factor suggested by the patient's history.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 7: In a previous experiment infecting hepatocytes, it was shown that viable HDV virions were only produced in the presence of a co-infection with HBV. To better understand which HBV particle was necessary for the production of viable HDV virions, the scientist encoded in separate plasmids the various antigens/proteins of HBV and co-infected the hepatocytes with HDV. In which of the experiments would viable HDV virions be produced in conjunction with the appropriate HBV antigen/protein?
- A. HBV DNA polymerase
- B. HBV RNA polymerase
- C. HBsAg (Correct Answer)
- D. HBcAg
- E. HBeAg
Viral hepatitis (A, B, C, D, E) Explanation: ***HBsAg***
- **Hepatitis D virus (HDV)** is a **defective virus** that requires co-infection with **hepatitis B virus (HBV)** to complete its replication cycle.
- Specifically, HDV uses the **hepatitis B surface antigen (HBsAg)**, encoded by HBV, to form its **outer envelope** and assemble viable virions.
*HBV DNA polymerase*
- HBV DNA polymerase is essential for **HBV DNA replication**, converting the viral pregenomic RNA into DNA.
- It plays no direct role in the **packaging or formation of the HDV envelope**.
*HBV RNA polymerase*
- HBV, like other DNA viruses, utilizes the **host cell's RNA polymerase** for transcription of its RNA templates, not its own.
- HBV itself does not encode an RNA polymerase, and even if it did, it would not be relevant for HDV virion packaging.
*HBcAg*
- **Hepatitis B core antigen (HBcAg)** forms the **capsid** of the HBV virion, encapsulating the viral genome.
- While critical for HBV replication, it is **not incorporated into the HDV virion outer envelope**.
*HBeAg*
- **Hepatitis B e-antigen (HBeAg)** is a soluble protein derived from **HBcAg** that is secreted into the blood.
- It plays a role in **immune modulation** and is a marker of HBV replication but does not contribute to HDV virion assembly.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 8: A 72-year-old man comes to the emergency department for progressively worsening abdominal pain. The pain began 2 weeks ago and is localized to the right upper quadrant. He feels sick and fatigued. He also reports breathlessness when climbing the stairs to his first-floor apartment. He is a retired painter. He has hypertension and type 2 diabetes mellitus. He is sexually active with one female partner and does not use condoms consistently. He began having sexual relations with his most recent partner 2 months ago. He smoked 1 pack of cigarettes daily for 40 years but quit 10 years ago. He does not drink alcohol. Current medications include insulin and enalapril. He is 181 cm (5 ft 11 in) tall and weighs 110 kg (264 lb); BMI is 33.5 kg/m2. His vital signs are within normal limits. Physical examination shows jaundice, a distended abdomen, and tender hepatomegaly. There is no jugular venous distention. A grade 2/6 systolic ejection murmur is heard along the right upper sternal border. Laboratory studies show:
Hemoglobin 18.9 g/dL
Aspartate aminotransferase 450 U/L
Alanine aminotransferase 335 U/L
Total bilirubin 2.1 mg/dL
Which of the following is the most likely cause of his symptoms?
- A. Hepatotropic viral infection
- B. Increased iron absorption
- C. Hepatic steatosis
- D. Hepatic vein obstruction (Correct Answer)
- E. Thickened pericardium
Viral hepatitis (A, B, C, D, E) Explanation: ***Hepatic vein obstruction***
- The patient's **acute liver injury** (elevated AST, ALT, bilirubin) with **right upper quadrant pain**, **tender hepatomegaly**, and **distended abdomen** are classic signs of hepatic vein obstruction (Budd-Chiari syndrome).
- The elevated **hemoglobin (18.9 g/dL)** suggests **polycythemia**, a common predisposing factor for thrombotic events, including hepatic vein thrombosis.
*Hepatotropic viral infection*
- While **hepatotropic viral infections** can cause acute liver injury, the patient's **polycythemia** and the specific presentation of **tender hepatomegaly** and **abdominal distention** are less indicative of this cause alone.
- Though he reports unprotected sex, acute viral hepatitis would generally present with more pronounced acute symptoms and specific markers on serology, which are not provided.
*Increased iron absorption*
- **Hemochromatosis**, due to increased iron absorption, causes liver damage but typically presents with **bronze skin**, diabetes, and joint pain, and the liver injury is usually insidious rather than acute with marked abdominal symptoms.
- The extremely high hemoglobin level in this acute setting is not characteristic of iron overload alone as a primary etiology for acute liver injury mimicking Budd-Chiari.
*Hepatic steatosis*
- **Hepatic steatosis** (fatty liver) is common in patients with **diabetes** and **obesity**; however, it usually presents as asymptomatic elevation of liver enzymes or chronic liver disease, not acute, severe right upper quadrant pain, marked tender hepatomegaly, and abdominal distension, especially with concurrent polycythemia.
- The degree of liver enzyme elevation and bilirubin is more pronounced than typically seen in uncomplicated hepatic steatosis.
*Thickened pericardium*
- A **thickened pericardium** (constrictive pericarditis) can cause **hepatomegaly** and **abdominal distension** due to right-sided heart failure. However, this is characteristically associated with **jugular venous distention** and often **ascites**, which are not noted here.
- The prominent **acute right upper quadrant pain** and **marked liver enzyme elevation** are less typical of cardiac causes of liver congestion compared to thrombotic occlusion.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 9: A 44-year-old woman presents to the emergency department with jaundice and diffuse abdominal pain. She denies any previous medical problems and says she does not take any medications, drugs, or supplements. Her temperature is 97.6°F (36.4°C), blood pressure is 133/87 mmHg, pulse is 86/min, respirations are 22/min, and oxygen saturation is 100% on room air. Physical exam is notable for sclera which are icteric and there is tenderness to palpation over the right upper quadrant. Laboratory studies are ordered as seen below.
Hepatitis B surface antigen: Positive
Hepatitis B surface antibody: Negative
Hepatitis B core antibody IgM: Negative
Hepatitis B core antibody IgG: Positive
Hepatitis B E antigen: Positive
Hepatitis B E antibody (anti-HBe): Negative
Which of the following is the most likely diagnosis?
- A. Chronic hepatitis B infection (Correct Answer)
- B. Hepatitis B vaccination
- C. Acute hepatitis B infection
- D. Resolved hepatitis B infection
- E. No hepatitis B vaccination or infection
Viral hepatitis (A, B, C, D, E) Explanation: ### ***Chronic hepatitis B infection***
- The presence of **Hepatitis B surface antigen (HBsAg) positive** combined with **Hepatitis B core antibody IgG (anti-HBc IgG) positive** indicates infection that has persisted beyond 6 months.
- **Hepatitis B core antibody IgM (anti-HBc IgM) negative** rules out acute infection, as IgM antibodies appear early in acute hepatitis B.
- **Hepatitis B e antigen (HBeAg) positive** indicates active viral replication and high infectivity, consistent with HBeAg-positive chronic hepatitis B.
- The clinical presentation with jaundice and RUQ pain suggests an acute flare of chronic hepatitis B infection.
### *Hepatitis B vaccination*
- Successful hepatitis B vaccination produces **anti-HBs positive** with **HBsAg negative** and **anti-HBc negative**.
- This patient has **HBsAg positive** and **anti-HBc IgG positive**, indicating actual infection rather than vaccine-induced immunity.
### *Acute hepatitis B infection*
- Acute hepatitis B is characterized by **HBsAg positive** with **anti-HBc IgM positive** (IgM appears first in acute infection).
- This patient has **anti-HBc IgM negative** and **anti-HBc IgG positive**, indicating the infection occurred more than 6 months ago, consistent with chronic rather than acute infection.
### *Resolved hepatitis B infection*
- Resolved infection shows **HBsAg negative**, **anti-HBs positive**, and **anti-HBc IgG positive**.
- This patient's **HBsAg positive** status directly indicates ongoing infection, not resolution.
### *No hepatitis B vaccination or infection*
- Complete absence of exposure would show **HBsAg negative**, **anti-HBs negative**, and **anti-HBc negative** (all markers negative).
- This patient has multiple positive markers including **HBsAg** and **anti-HBc IgG**, confirming hepatitis B infection.
Viral hepatitis (A, B, C, D, E) US Medical PG Question 10: A 38-year-old woman comes to the physician because of a 3-month history of moderate abdominal pain that is unresponsive to medication. She has a history of two spontaneous abortions at 11 and 12 weeks' gestation. Ultrasound examination of the abdomen shows normal liver parenchyma, a dilated portal vein, and splenic enlargement. Upper endoscopy shows dilated submucosal veins in the lower esophagus. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased serum bilirubin levels
- B. Increased prothrombin time
- C. Thrombocytopenia (Correct Answer)
- D. Hepatic venous congestion
- E. Councilman bodies
Viral hepatitis (A, B, C, D, E) Explanation: ***Thrombocytopenia***
- The patient's **recurrent spontaneous abortions** suggest **antiphospholipid syndrome (APS)**, a hypercoagulable state that predisposes to both arterial and venous thrombosis.
- APS likely caused **portal vein thrombosis**, leading to **prehepatic portal hypertension** (dilated portal vein, esophageal varices, and splenomegaly) with **normal liver parenchyma**.
- The **splenomegaly** causes **hypersplenism**, resulting in **thrombocytopenia** due to splenic sequestration and increased destruction of platelets.
- While APS can also cause immune-mediated thrombocytopenia directly, the primary mechanism here is hypersplenism secondary to portal hypertension.
*Increased serum bilirubin levels*
- Elevated bilirubin indicates **hepatocellular dysfunction** or **biliary obstruction**.
- The ultrasound shows **normal liver parenchyma**, making significant hepatocellular damage unlikely.
- Portal vein thrombosis without liver parenchymal disease does not typically cause hyperbilirubinemia.
*Increased prothrombin time*
- Prolonged PT reflects impaired **hepatic synthesis of coagulation factors** (II, VII, IX, X).
- With **normal liver parenchyma** on imaging, synthetic liver function should be preserved.
- Portal vein thrombosis alone does not impair hepatocyte function or coagulation factor synthesis.
*Hepatic venous congestion*
- This finding is characteristic of **Budd-Chiari syndrome** (hepatic vein thrombosis), which presents with hepatomegaly, ascites, and signs of hepatic outflow obstruction.
- The patient's findings (dilated **portal vein**, normal liver parenchyma) indicate **portal vein thrombosis** causing **prehepatic portal hypertension**, not posthepatic venous congestion.
*Councilman bodies*
- These are **eosinophilic apoptotic hepatocytes** seen in acute liver injury (viral hepatitis, yellow fever, toxic injury).
- **Normal liver parenchyma** on ultrasound excludes significant hepatocellular necrosis.
- This finding is unrelated to thrombotic disorders or portal hypertension.
More Viral hepatitis (A, B, C, D, E) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.