Spontaneous bacterial peritonitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spontaneous bacterial peritonitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spontaneous bacterial peritonitis US Medical PG Question 1: A 42-year-old man with chronic hepatitis C is admitted to the hospital because of jaundice and abdominal distention. He is diagnosed with decompensated liver cirrhosis, and treatment with diuretics is begun. Two days after admission, he develops abdominal pain and fever. Physical examination shows tense ascites and diffuse abdominal tenderness. Paracentesis yields cloudy fluid with elevated polymorphonuclear (PMN) leukocyte count. A drug with which of the following mechanisms is most appropriate for this patient's condition?
- A. Free radical creation within bacterial cell
- B. Inhibition of bacterial 50S subunit
- C. Inhibition of bacterial RNA polymerase
- D. Inhibition of bacterial peptidoglycan crosslinking (Correct Answer)
- E. Inhibition of bacterial DNA gyrase
Spontaneous bacterial peritonitis Explanation: ***Inhibition of bacterial peptidoglycan crosslinking***
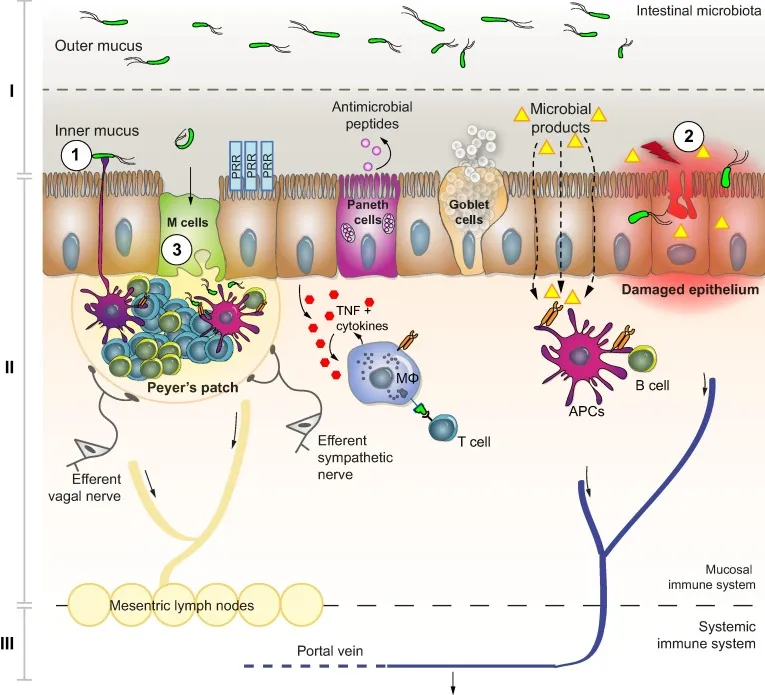
- The patient's symptoms (fever, abdominal pain, diffuse tenderness, cloudy ascitic fluid with elevated PMN count) are highly suggestive of **spontaneous bacterial peritonitis (SBP)**, a common complication of decompensated cirrhosis.
- The most appropriate treatment for SBP is **broad-spectrum antibiotics**, typically a third-generation cephalosporin like **cefotaxime** or **ceftriaxone**, which work by inhibiting bacterial peptidoglycan crosslinking in the cell wall (beta-lactam mechanism).
- These agents provide excellent coverage against the common gram-negative enteric pathogens (especially *E. coli*) that cause SBP.
*Free radical creation within bacterial cell*
- This mechanism is characteristic of **nitroimidazoles** (e.g., metronidazole), which are effective against anaerobic bacteria and certain protozoa.
- While anaerobes can occasionally be involved in secondary peritonitis, empiric treatment for SBP typically targets gram-negative enteric bacteria, for which nitroimidazoles are not first-line choices.
*Inhibition of bacterial 50S subunit*
- This mechanism is common to **macrolides** (e.g., azithromycin) and **lincosamides** (e.g., clindamycin).
- These antibiotics are generally not first-line empiric treatment for SBP, which primarily requires coverage of gram-negative aerobes.
*Inhibition of bacterial RNA polymerase*
- This is the mechanism of action for **rifampin**, which is primarily used for tuberculosis and prophylaxis against certain bacterial meningitis (e.g., *N. meningitidis*).
- Rifampin is not suitable as empiric monotherapy for SBP given the typical causative pathogens.
*Inhibition of bacterial DNA gyrase*
- This is the mechanism of **fluoroquinolones** (e.g., ciprofloxacin, levofloxacin), which inhibit DNA gyrase (topoisomerase II) and topoisomerase IV, preventing bacterial DNA replication.
- Fluoroquinolones can be used for SBP treatment and prophylaxis, but third-generation cephalosporins remain the preferred first-line empiric therapy for acute SBP in most clinical guidelines.
Spontaneous bacterial peritonitis US Medical PG Question 2: A 47-year-old man presents to the emergency department with jaundice and extreme fatigue for the past 4 days. He also noticed that his stool is very pale and urine is dark. Past medical history is unremarkable. The review of systems is significant for a 23 kg (50 lb) weight loss over the last 3 months which he says is due to decreased appetite. He is afebrile and the vital signs are within normal limits. A contrast computed tomography (CT) scan of the abdomen reveals a mass in the pancreatic head. A blood test for carbohydrate antigen (CA19-9) is positive. The patient is admitted to the intensive care unit (ICU) and undergoes surgical decompression of the biliary tract. He is placed on total parenteral nutrition (TPN). On day 4 after admission, his intravenous access site is found to be erythematous and edematous. Which of the following microorganisms is most likely responsible for this patient’s intravenous (IV) site infection?
- A. Candida parapsilosis (Correct Answer)
- B. E. coli
- C. Hepatitis B virus
- D. Pseudomonas aeruginosa
- E. Malassezia furfur
Spontaneous bacterial peritonitis Explanation: ***Candida parapsilosis***
- This yeast is a common cause of **catheter-related bloodstream infections** in patients receiving **total parenteral nutrition (TPN)**, as it can readily grow on lipid emulsions.
- The patient's presentation with an erythematous and edematous intravenous access site, coupled with a history of TPN, strongly points towards a fungal infection, with *C. parapsilosis* being a primary suspect due to its affinity for TPN.
*E. coli*
- While *E. coli* is a common cause of **urinary tract infections** and can cause **bloodstream infections**, it is not a typical cause of IV site infections specifically associated with TPN.
- Its presence at an IV site would usually indicate a more generalized sepsis or contamination, rather than the specific affinity *C. parapsilosis* has for TPN lines.
*Hepatitis B virus*
- **Hepatitis B virus** causes **viral hepatitis** and liver damage, but it does not directly cause localized IV site infections with erythema and edema.
- It is typically spread through blood and body fluids and its clinical manifestations are systemic, primarily involving the liver, rather than local skin signs at an IV access site.
*Pseudomonas aeruginosa*
- **Pseudomonas aeruginosa** is a common opportunistic pathogen, particularly in **immunocompromised patients** and those with medical devices, but it is typically associated with infections in burn wounds, cystic fibrosis, or ventilator-associated pneumonia.
- While it can cause catheter-related infections, it is not as uniquely linked to TPN-associated IV site infections as *Candida parapsilosis*.
*Malassezia furfur*
- *Malassezia furfur* is known to cause **catheter-related infections** in patients receiving **lipid emulsions** via central lines, similar to *C. parapsilosis*.
- However, *C. parapsilosis* is statistically a more common cause of TPN-associated fungemia and IV site infections than *M. furfur*.
Spontaneous bacterial peritonitis US Medical PG Question 3: A 50-year-old woman presents with esophageal varices, alcoholic cirrhosis, hepatic encephalopathy, portal hypertension, and recent onset confusion. The patient’s husband does not recall her past medical history but knows her current medications and states that she is quite disciplined about taking them. Current medications are spironolactone, labetalol, lactulose, and furosemide. Her temperature is 38.3°C (100.9°F), heart rate is 115/min, blood pressure is 105/62 mm Hg, respiratory rate is 12/min, and oxygen saturation is 96% on room air. On physical examination, the patient is disoriented, lethargic, and poorly responsive to commands. A cardiac examination is unremarkable. Lungs are clear to auscultation. The abdomen is distended, tense, and mildly tender. Mild asterixis is present. Neurologic examination is normal. The digital rectal examination reveals guaiac negative stool. Laboratory findings are significant for the following:
Basic metabolic panel Unremarkable
Platelet count 95,500/µL
Leukocyte count 14,790/µL
Hematocrit 33% (baseline is 30%)
Which of the following would most likely be of diagnostic value in this patient?
- A. Therapeutic trial of lactulose
- B. Abdominal paracentesis (Correct Answer)
- C. Noncontrast CT of the head
- D. Serum ammonia level
- E. Esophagogastroduodenoscopy
Spontaneous bacterial peritonitis Explanation: ***Abdominal paracentesis***
- The patient presents with **fever, abdominal tenderness, distension, and new-onset confusion** in the setting of **cirrhosis and ascites**, which are highly suggestive of **spontaneous bacterial peritonitis (SBP)**.
- An **abdominal paracentesis** with analysis of ascitic fluid (cell count with differential, culture) is necessary to diagnose SBP and guide appropriate antibiotic treatment.
*Therapeutic trial of lactulose*
- While the patient has **hepatic encephalopathy** and is on lactulose, her current presentation with **fever and abdominal tenderness** suggests an acute infectious process rather than worsening encephalopathy unresponsive to current therapy.
- A therapeutic trial of lactulose alone would delay the diagnosis of a potentially life-threatening infection like SBP.
*Noncontrast CT of the head*
- Although the patient has new-onset confusion, her presentation also includes **fever, abdominal tenderness, and signs of infection** in a patient with cirrhosis.
- A CT head would be more appropriate if there were focal neurological deficits, acute head trauma, or if SBP was ruled out and other causes of altered mental status were suspected.
*Serum ammonia level*
- The patient has known **hepatic encephalopathy**, and her current confusion is likely multifactorial.
- While an elevated ammonia level supports the diagnosis of hepatic encephalopathy, it is not diagnostic for the *cause* of her acute deterioration and would not rule out SBP, which requires urgent diagnosis and treatment.
*Esophagogastroduodenoscopy*
- The patient has a history of esophageal varices, but there is no evidence of active gastrointestinal bleeding (e.g., melena, hematemesis, guaiac positive stool).
- An **EGD** would be indicated for acute variceal bleeding, but it is not the most immediate or relevant diagnostic step for her current acute presentation of fever, abdominal pain, and confusion.
Spontaneous bacterial peritonitis US Medical PG Question 4: A 15-year-old boy presents with his father to the urgent care department with a 5-day history of frequent diarrhea, occasionally mixed with streaks of blood. Stool cultures are pending, but preliminary stool samples demonstrate fecal leukocytes and erythrocytes. The patient's vital signs are within normal limits, and he is started on outpatient therapy for presumed Shigella infection. Which of the following was the young man most likely started on?
- A. Oral vancomycin
- B. Oral erythromycin
- C. Oral metronidazole
- D. An oral quinolone
- E. Oral trimethoprim-sulfamethoxazole (TMP-SMX) (Correct Answer)
Spontaneous bacterial peritonitis Explanation: **Oral trimethoprim-sulfamethoxazole (TMP-SMX)**
- **TMP-SMX** is a traditional first-line treatment for **Shigella infection** in settings where susceptibility is expected or confirmed.
- The patient's presentation with **bloody diarrhea**, **fecal leukocytes**, and **erythrocytes** is classic for **Shigella dysentery**.
- While **resistance rates vary by region**, TMP-SMX remains an appropriate choice when local susceptibility patterns support its use.
- It is cost-effective, well-tolerated, and appropriate for outpatient management of uncomplicated cases.
*Oral vancomycin*
- Vancomycin is specifically used for **Clostridioides difficile infection** and does not treat Shigella.
- It has **poor oral absorption** and no activity against Gram-negative enteric pathogens like Shigella.
*Oral erythromycin*
- Erythromycin is primarily effective against **Campylobacter jejuni** and respiratory pathogens.
- It has **limited activity against Shigella** and resistance rates are high, making it an inappropriate choice.
*Oral metronidazole*
- Metronidazole treats **anaerobic bacteria** and protozoal infections (*Giardia*, *Entamoeba histolytica*).
- It has **no significant activity against Shigella**, a facultative anaerobic Gram-negative bacillus.
*An oral quinolone*
- **Fluoroquinolones** (e.g., ciprofloxacin) are highly effective against Shigella and often used as first-line therapy, particularly in areas with high TMP-SMX resistance.
- They are increasingly preferred in current guidelines due to rising resistance to TMP-SMX.
- However, in the context of empiric outpatient treatment where susceptibility is presumed, **TMP-SMX** may still be chosen initially as a narrower-spectrum, cost-effective option, with fluoroquinolones reserved based on culture results or treatment failure.
Spontaneous bacterial peritonitis US Medical PG Question 5: A 49-year-old woman with a history of hepatitis C cirrhosis complicated by esophageal varices, ascites, and hepatic encephalopathy presents with 1 week of increasing abdominal discomfort. Currently, she takes lactulose, rifaximin, furosemide, and spironolactone. On physical examination, she has mild asterixis, generalized jaundice, and a distended abdomen with positive fluid wave. Diagnostic paracentesis yields a WBC count of 1196/uL with 85% neutrophils. Which of the following is the most appropriate treatment?
- A. Cefotaxime (Correct Answer)
- B. Transjugular intrahepatic portosystemic shunt placement
- C. Large volume paracentesis with albumin
- D. Increased furosemide and spironolactone
- E. Metronidazole
Spontaneous bacterial peritonitis Explanation: ***Cefotaxime***
- The patient presents with classic signs of **spontaneous bacterial peritonitis (SBP)**: increasing abdominal discomfort in a cirrhotic patient with ascites, and a diagnostic paracentesis showing **ascitic fluid neutrophil count >250 cells/mm³** (1196 × 0.85 = 1016 neutrophils/μL).
- **Third-generation cephalosporins** like cefotaxime or ceftriaxone are the **first-line treatment** for SBP due to their broad-spectrum coverage against common enteric gram-negative bacteria (especially E. coli and Klebsiella).
- Treatment should be initiated promptly once SBP is diagnosed to reduce mortality.
*Transjugular intrahepatic portosystemic shunt placement*
- TIPS is primarily used for **refractory ascites** or **recurrent variceal bleeding** that is not responsive to medical management.
- It is **not indicated** for the acute treatment of SBP and would be inappropriate in the setting of active infection.
*Large volume paracentesis with albumin*
- Large volume paracentesis is used to relieve symptoms of **tense ascites** causing respiratory compromise or severe discomfort, not as a primary treatment for SBP.
- While albumin is often given with large volume paracentesis (>5L removed) to prevent post-paracentesis circulatory dysfunction, it does not treat the underlying bacterial infection.
*Increased furosemide and spironolactone*
- Diuretics like furosemide and spironolactone are used to manage **chronic ascites** by promoting fluid excretion.
- Increasing their dose will not address the active bacterial infection causing SBP and may worsen renal function in an acutely ill patient.
*Metronidazole*
- Metronidazole is primarily effective against **anaerobic bacteria** and some protozoa.
- While it might be considered in specific polymicrobial intra-abdominal infections, it is **not sufficient as monotherapy** for SBP, which commonly involves gram-negative aerobic bacteria like E. coli and Klebsiella species.
Spontaneous bacterial peritonitis US Medical PG Question 6: A 45-year-old homeless man is brought to the emergency department. He was found unconscious at the park. The patient has a past medical history of IV drug abuse, hepatitis C, alcohol abuse, schizophrenia, and depression. He does not receive normal medical follow up or care. His temperature is 102°F (38.9°C), blood pressure is 97/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam demonstrates a diffusely distended abdomen that is dull to percussion with a notable fluid wave. The abdominal exam causes the patient to contract his extremities. Cardiac and pulmonary exam are within normal limits. The patient responds to painful stimuli and smells heavily of alcohol. Which of the following is the best next step in management?
- A. Ceftriaxone
- B. CT abdomen
- C. Paracentesis (Correct Answer)
- D. Cefotaxime
- E. Ultrasound
Spontaneous bacterial peritonitis Explanation: ***Paracentesis***
- The patient's **distended abdomen**, **dullness to percussion**, and **fluid wave** are classic signs of **ascites**. Given his history of **alcohol abuse** and **hepatitis C**, he is at high risk for cirrhosis-related ascites, which can become infected (spontaneous bacterial peritonitis, or **SBP**).
- A **paracentesis** is crucial for diagnosing SBP by analyzing the ascitic fluid for **cell count (especially PMNs)**, culture, and other parameters. It's the most appropriate first step in a patient with new-onset ascites or suspected SBP, especially if they are febrile.
*Ceftriaxone*
- While **antibiotics** are indicated for **spontaneous bacterial peritonitis (SBP)**, initiating empiric antibiotics like **ceftriaxone** before diagnostic paracentesis could mask the causative organism and make diagnosis difficult.
- Paracentesis is necessary to confirm SBP and guide specific antibiotic therapy, though empiric antibiotics should be started promptly after fluid collection if SBP is highly suspected.
*CT abdomen*
- A **CT scan** would provide detailed anatomical information but is not the most urgent or appropriate first step for diagnosing **SBP** or guiding immediate management in this setting.
- While it can confirm ascites, it cannot establish the diagnosis of infection or determine the fluid's cellular content, which is critical for treatment decisions.
*Cefotaxime*
- Similar to ceftriaxone, **cefotaxime** is an appropriate **antibiotic** for treating **spontaneous bacterial peritonitis (SBP)**.
- However, performing a **diagnostic paracentesis** to confirm SBP and obtain fluid for analysis is the priority before initiating empiric antibiotic therapy, just as with ceftriaxone.
*Ultrasound*
- An **ultrasound** can confirm the presence of **ascites** and rule out other causes of abdominal distension, and can also guide paracentesis.
- However, in a patient with suspected **spontaneous bacterial peritonitis (SBP)** and clear signs of ascites, performing the **diagnostic paracentesis** is the most direct and urgent next step to identify infection, making it more critical than just imaging.
Spontaneous bacterial peritonitis US Medical PG Question 7: A 67-year-old man is brought to the emergency department when he was found obtunded at the homeless shelter. The patient is currently not responsive and smells of alcohol. The patient has a past medical history of alcohol use, IV drug use, and hepatitis C. His temperature is 99°F (37.2°C), blood pressure is 95/65 mmHg, pulse is 95/min, respirations are 13/min, and oxygen saturation is 95% on room air. The patient is started on IV fluids, and his pulse decreases to 70/min. On physical exam, the patient has an abdominal exam notable for distension and a positive fluid wave. The patient displays mild yellow discoloration of his skin. The patient has notable poor dentition and poor hygiene overall. A systolic murmur is heard along the left sternal border on cardiac exam. Pulmonary exam is notable for mild bibasilar crackles. Laboratory values are ordered, and return as below:
Hemoglobin: 10 g/dL
Hematocrit: 32%
Leukocyte count: 7,500 cells/mm^3 with normal differential
Platelet count: 227,000/mm^3
Serum:
Na+: 125 mEq/L
Cl-: 100 mEq/L
K+: 5.0 mEq/L
HCO3-: 24 mEq/L
BUN: 51 mg/dL
Glucose: 89 mg/dL
Creatinine: 2.2 mg/dL
Ca2+: 10.0 mg/dL
AST: 22 U/L
ALT: 19 U/L
Urine:
Color: Amber
Nitrites: Negative
Sodium: 12 mmol/24 hours
Red blood cells: 0/hpf
Over the next 24 hours, the patient produces very little urine. Which of the following best explains this patient’s renal findings?
- A. Liver failure (Correct Answer)
- B. Nephrotoxic agent
- C. Dehydration
- D. Postrenal azotemia
- E. Congestive heart failure
Spontaneous bacterial peritonitis Explanation: ***Liver failure***
- The patient's history of **alcohol use**, **hepatitis C**, **ascites** (abdominal distension with fluid wave), and **jaundice** (yellow skin discoloration) are all signs of severe liver disease/cirrhosis.
- In the context of advanced liver failure, this patient has developed **hepatorenal syndrome (HRS)**, a critical complication characterized by **functional renal failure** due to severe renal vasoconstriction without intrinsic kidney damage.
- Key diagnostic features of HRS include: elevated **BUN** and **creatinine**, markedly **low urine sodium (<20 mEq/L)**, **oliguria** that does not improve with volume expansion, and absence of other causes of renal failure.
- The urine sodium of **12 mmol/24 hours** is pathognomonic for HRS, indicating maximal sodium retention by the kidneys in response to decreased effective arterial blood volume.
*Nephrotoxic agent*
- While IV drug use can be associated with certain nephrotoxic exposures, there is no direct evidence in the clinical presentation (e.g., specific drug use leading to toxicity, muddy brown casts on urinalysis) to support this.
- **Acute tubular necrosis (ATN)** from nephrotoxins typically presents with urine sodium **>40 mEq/L** and granular casts, which are absent here.
- The patient's underlying liver disease with characteristic low urine sodium provides a more comprehensive explanation for the renal dysfunction.
*Dehydration*
- The patient's **blood pressure** is low, but he responded to IV fluids with a decreased pulse, suggesting some improvement in volume status, yet his renal function worsened with persistent oliguria.
- While dehydration can cause **prerenal azotemia**, the lack of improvement after IV fluid resuscitation, extreme oliguria, very low urine sodium in the context of advanced cirrhosis with ascites point strongly towards hepatorenal syndrome rather than simple hypovolemia.
- True prerenal azotemia from dehydration typically improves with fluid administration, which did not occur here.
*Postrenal azotemia*
- This condition is caused by an **obstruction** to urine outflow, such as a kidney stone, enlarged prostate, or tumor.
- There are no clinical signs or symptoms (e.g., flank pain, difficulty urinating, hydronephrosis on imaging) in the patient's presentation to suggest an obstructive cause.
- Postrenal obstruction typically requires **bilateral** obstruction or obstruction in a single functioning kidney to cause significant azotemia.
*Congestive heart failure*
- While the patient has **bibasilar crackles** and a cardiac murmur, these are non-specific findings that might be related to volume overload from liver disease or endocarditis from IV drug use.
- **Cardiorenal syndrome** can cause renal dysfunction, but typically presents with more prominent signs of heart failure and urine sodium is often higher (>40 mEq/L) when diuretics are used.
- The patient's profound liver failure with ascites, jaundice, and the characteristic very low urine sodium provide a much stronger and more direct explanation for the progressive renal dysfunction as hepatorenal syndrome.
Spontaneous bacterial peritonitis US Medical PG Question 8: A 52-year-old man comes to the physician because his skin has been progressively yellowing for the past 4 weeks. He also reports low appetite and difficulty fitting into his pants because of his swollen legs over the past several months. There is no personal or family history of serious illness. He does not smoke and drinks 1 to 2 beers on special occasions. He used to be sexually active with multiple female partners but has lost interest in sexual intercourse recently. He is 178 cm (5 ft 10 in) tall and weighs 68 kg (150 lb); his BMI is 22 kg/m2. Vital signs are within normal limits. Physical examination shows yellowing of the skin and sclera as well as erythema of the palms. There is bilateral enlargement of breast tissue. Cardiopulmonary examinations show no abnormalities. The abdomen is distended. The liver is palpated 2 to 3 cm below the right costal margin. On percussion of the left abdomen, a thrill can be felt on the right side. Hepatojugular reflux is absent. There is bilateral edema below the knees. Which of the following is the most likely underlying cause of this patient's condition?
- A. Autoimmune hepatitis
- B. Congestive hepatopathy
- C. Primary biliary cirrhosis
- D. Chronic viral hepatitis (Correct Answer)
- E. Non-alcoholic steatohepatitis
Spontaneous bacterial peritonitis Explanation: ***Chronic viral hepatitis***
- The patient's history of **multiple sexual partners** and subsequent development of **jaundice**, **ascites** (distended abdomen with thrill on percussion), **palmar erythema**, **gynecomastia** (bilateral enlarged breast tissue), and **peripheral edema** are highly suggestive of **decompensated chronic liver disease**, such as **cirrhosis**.
- **Chronic viral hepatitis** (e.g., Hepatitis B or C) is a very common cause of cirrhosis, especially in patients with a history of risky behaviors like unprotected sexual intercourse.
*Autoimmune hepatitis*
- While it can cause cirrhosis, **autoimmune hepatitis** typically presents with elevated **liver enzymes** (AST, ALT) and specific **autoantibodies** (e.g., ANA, anti-smooth muscle antibodies), which are not mentioned here.
- There is no specific risk factor for autoimmune disease in this patient's history.
*Congestive hepatopathy*
- This condition results from **right-sided heart failure**, causing engorgement of the liver and potentially cirrhosis. The absence of **hepatojugular reflux** makes this diagnosis less likely.
- Symptoms like **jugular venous distention** and **cardiac murmurs** associated with heart failure would typically be present.
*Primary biliary cirrhosis*
- This is a **cholestatic liver disease** primarily affecting **middle-aged women** and is characterized by **pruritus**, **fatigue**, and elevated **alkaline phosphatase**.
- The patient's gender and lack of specific cholestatic symptoms make this less probable.
*Non-alcoholic steatohepatitis*
- While **NASH** can progress to cirrhosis, the patient's **normal BMI**, lack of significant **alcohol intake**, and no history of **diabetes** or **dyslipidemia** make this diagnosis less likely.
- NASH is strongly associated with **metabolic syndrome**.
Spontaneous bacterial peritonitis US Medical PG Question 9: A 55-year-old patient who immigrated from the Middle East to the United States 10 years ago presents to the emergency department because of excessive weakness, abdominal discomfort, and weight loss for the past 10 months. He has had type 2 diabetes mellitus for 10 years for which he takes metformin. He had an appendectomy 12 years ago in his home country, and his postoperative course was not complicated. He denies smoking and drinks alcohol socially. His blood pressure is 110/70 mm Hg, pulse is 75/min, and temperature is 37.1°C (98.7°F). On physical examination, the patient appears exhausted, and his sclerae are yellowish. A firm mass is palpated in the right upper abdominal quadrant. Abdominal ultrasonography shows liver surface nodularity, splenomegaly, and increased diameter of the portal vein. Which of the following is the most common complication of this patient condition?
- A. Hepatopulmonary syndrome
- B. Ascites (Correct Answer)
- C. Hepatic encephalopathy
- D. Hepatorenal syndrome
- E. Hepatic osteodystrophy
Spontaneous bacterial peritonitis Explanation: ***Ascites***
- The patient presents with classic signs of **portal hypertension** (splenomegaly, increased portal vein diameter, liver surface nodularity suggesting cirrhosis), and **ascites** is the most common and often the earliest major complication.
- The presence of **abdominal discomfort** and an **RUQ mass** could be related to severe liver disease and its complications, including fluid accumulation or an underlying liver malignancy often associated with cirrhosis.
*Hepatopulmonary syndrome*
- This involves **intrapulmonary vascular dilatations** in the setting of liver disease leading to oxygenation defects, typically marked by platypnea and orthodeoxia, which are not described here.
- While a complication of **cirrhosis**, it is less common than ascites and typically presents with respiratory symptoms not highlighted in this case.
*Hepatic encephalopathy*
- Characterized by **neuropsychiatric symptoms** due to the accumulation of toxins (e.g., ammonia) that the liver cannot detoxify.
- The patient's presentation mainly focuses on physical weakness, abdominal issues, and jaundice, without mention of confusion, asterixis, or altered mental status.
*Hepatorenal syndrome*
- This is a form of **functional renal failure** that occurs in patients with advanced liver disease, presenting with rapidly progressive azotemia due to severe splanchnic vasodilation.
- It is a **later and more severe complication** of liver failure, and while possible, ascites is typically seen much earlier and more frequently.
*Hepatic osteodystrophy*
- This refers to a group of **metabolic bone disorders** (osteoporosis, osteomalacia) that can occur in chronic liver disease.
- While it can manifest as bone pain, it is not a direct or immediate complication of portal hypertension and would not explain the acute abdominal findings.
Spontaneous bacterial peritonitis US Medical PG Question 10: A 49-year-old man presents to the emergency department with abdominal discomfort, fever, and decreased urination. He has a history of liver cirrhosis due to chronic hepatitis C infection. His blood pressure is 90/70 mm Hg, pulse is 75/min, and temperature 38°C (100.4°F). On physical examination he is jaundiced, and he has tense ascites with generalized abdominal tenderness. There is pitting edema to the level of his upper thighs. Which of the following excludes the diagnosis of hepatorenal syndrome in this patient?
- A. Low albumin levels
- B. Normal renal ultrasound
- C. Presence of 30 red cells/high powered field in the urine (Correct Answer)
- D. Low urea levels
- E. Prolonged prothrombin time
Spontaneous bacterial peritonitis Explanation: ***Presence of 30 red cells/high powered field in the urine***
- **Hepatorenal syndrome (HRS)** is a diagnosis of exclusion characterized by **functional renal failure** in the setting of severe liver disease without intrinsic renal pathology. The presence of significant red blood cells in the urine (e.g., >50 RBCs/HPF is a more definitive cutoff often used, but 30 RBCs/HPF is highly suspicious) indicates an **intrinsic renal problem**, such as glomerulonephritis or acute tubular necrosis, which would exclude HRS.
- HRS typically presents with **benign urinary sediment**, meaning few or no red blood cells, white blood cells, or casts, as the kidneys themselves are structurally intact.
*Low albumin levels*
- **Hypoalbuminemia** is a common finding in patients with **cirrhosis** due to impaired hepatic synthesis and is often associated with ascites and edema.
- It is a predisposing factor for HRS development, but its presence does not exclude or confirm the diagnosis.
*Normal renal ultrasound*
- A **normal renal ultrasound** indicates the absence of **structural kidney disease** (e.g., obstruction, polycystic kidneys, or severe chronic kidney disease) that could otherwise explain the renal failure.
- This finding is **consistent with HRS**, as HRS is a functional renal failure without gross renal structural abnormalities, thus it does not exclude the diagnosis.
*Low urea levels*
- **Urea synthesis occurs in the liver**, and in patients with severe **cirrhosis**, the liver's ability to produce urea from ammonia may be impaired.
- Therefore, **low urea levels (or disproportionately low BUN relative to creatinine)** can be seen in advanced liver disease, even with renal impairment, and do not exclude HRS.
*Prolonged prothrombin time*
- A **prolonged prothrombin time (PT)** is a hallmark of severe **liver dysfunction** due to reduced synthesis of coagulation factors.
- It indicates the severity of the underlying liver disease and is a common finding in patients who develop HRS, therefore, it does not exclude the diagnosis.
More Spontaneous bacterial peritonitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.