Portal hypertension complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Portal hypertension complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Portal hypertension complications US Medical PG Question 1: A 57-year-old man is brought to the emergency department by his family because of several episodes of vomiting of blood in the past 24 hours. He has a history of alcoholic cirrhosis and is being treated for ascites with diuretics and for encephalopathy with lactulose. His vital signs include a temperature of 36.9°C (98.4°F), pulse of 85/min, and blood pressure of 80/52 mm Hg. On examination, he is confused and unable to give a complete history. He is noted to have jaundice, splenomegaly, and multiple spider angiomas over his chest. Which of the following is the best initial management of this patient?
- A. Endoscopic surveillance
- B. Non-selective beta-blockers
- C. Combined vasoactive and endoscopic therapy (Correct Answer)
- D. Balloon tamponade
- E. Transjugular intrahepatic portosystemic shunt (TIPS)
Portal hypertension complications Explanation: ***Combined vasoactive and endoscopic therapy***
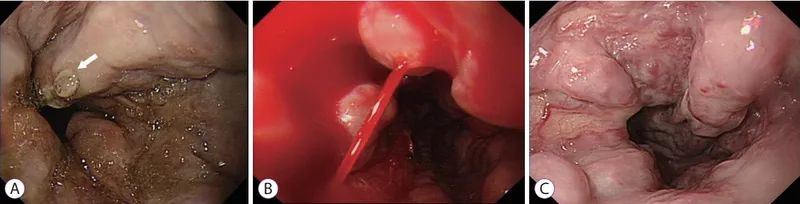
- The patient presents with **hematemesis**, **hypotension**, and signs of decompensated **alcoholic cirrhosis** (jaundice, splenomegaly, spider angiomas). This clinical picture is highly suggestive of **esophageal variceal bleeding**, a life-threatening emergency.
- **Combined vasoactive drug therapy** (e.g., octreotide to reduce splanchnic blood flow) and **endoscopic therapy** (e.g., variceal ligation or sclerotherapy) are the recommended initial management for **active variceal bleeding** to control hemorrhage and prevent rebleeding.
*Endoscopic surveillance*
- **Endoscopic surveillance** is performed for patients with known varices who are **not actively bleeding** to identify varices at high risk of rupture and to initiate primary prophylaxis.
- This patient is actively bleeding, making surveillance an inappropriate initial step.
*Non-selective beta-blockers*
- **Non-selective beta-blockers** (e.g., propranolol, carvedilol) are used for **primary and secondary prophylaxis** of variceal bleeding by reducing portal pressure.
- They are **not appropriate for acute bleeding management**, as their onset of action is too slow to control active hemorrhage.
*Balloon tamponade*
- **Balloon tamponade** (e.g., with a Sengstaken-Blakemore tube) is a **temporary measure** used to control massive, refractory variceal bleeding when endoscopic therapy is unsuccessful or immediately unavailable.
- It is a **bridge to definitive management** and carries significant risks, such as **esophageal rupture** or **aspiration**, so it is not the first-line initial treatment.
*Transjugular intrahepatic portosystemic shunt (TIPS)*
- **TIPS** is typically reserved for patients with **refractory variceal bleeding** that cannot be controlled by endoscopic and pharmacologic therapy, or for those with **recurrent bleeding despite optimal secondary prophylaxis**.
- It is an **invasive procedure** and not the immediate initial intervention for acute variceal hemorrhage.
Portal hypertension complications US Medical PG Question 2: A 49-year-old woman with a history of hepatitis C cirrhosis complicated by esophageal varices, ascites, and hepatic encephalopathy presents with 1 week of increasing abdominal discomfort. Currently, she takes lactulose, rifaximin, furosemide, and spironolactone. On physical examination, she has mild asterixis, generalized jaundice, and a distended abdomen with positive fluid wave. Diagnostic paracentesis yields a WBC count of 1196/uL with 85% neutrophils. Which of the following is the most appropriate treatment?
- A. Cefotaxime (Correct Answer)
- B. Transjugular intrahepatic portosystemic shunt placement
- C. Large volume paracentesis with albumin
- D. Increased furosemide and spironolactone
- E. Metronidazole
Portal hypertension complications Explanation: ***Cefotaxime***
- The patient presents with classic signs of **spontaneous bacterial peritonitis (SBP)**: increasing abdominal discomfort in a cirrhotic patient with ascites, and a diagnostic paracentesis showing **ascitic fluid neutrophil count >250 cells/mm³** (1196 × 0.85 = 1016 neutrophils/μL).
- **Third-generation cephalosporins** like cefotaxime or ceftriaxone are the **first-line treatment** for SBP due to their broad-spectrum coverage against common enteric gram-negative bacteria (especially E. coli and Klebsiella).
- Treatment should be initiated promptly once SBP is diagnosed to reduce mortality.
*Transjugular intrahepatic portosystemic shunt placement*
- TIPS is primarily used for **refractory ascites** or **recurrent variceal bleeding** that is not responsive to medical management.
- It is **not indicated** for the acute treatment of SBP and would be inappropriate in the setting of active infection.
*Large volume paracentesis with albumin*
- Large volume paracentesis is used to relieve symptoms of **tense ascites** causing respiratory compromise or severe discomfort, not as a primary treatment for SBP.
- While albumin is often given with large volume paracentesis (>5L removed) to prevent post-paracentesis circulatory dysfunction, it does not treat the underlying bacterial infection.
*Increased furosemide and spironolactone*
- Diuretics like furosemide and spironolactone are used to manage **chronic ascites** by promoting fluid excretion.
- Increasing their dose will not address the active bacterial infection causing SBP and may worsen renal function in an acutely ill patient.
*Metronidazole*
- Metronidazole is primarily effective against **anaerobic bacteria** and some protozoa.
- While it might be considered in specific polymicrobial intra-abdominal infections, it is **not sufficient as monotherapy** for SBP, which commonly involves gram-negative aerobic bacteria like E. coli and Klebsiella species.
Portal hypertension complications US Medical PG Question 3: A 56-year-old woman with a history of alcoholic cirrhosis and recurrent esophageal varices who recently underwent transjugular intrahepatic portosystemic shunt (TIPS) placement is brought to the emergency room by her daughter due to confusion and agitation. Starting this morning, the patient has appeared sleepy, difficult to arouse, and slow to respond to questions. Her temperature is 97.6°F (36.4°C), blood pressure is 122/81 mmHg, pulse is 130/min, respirations are 22/min, and oxygen saturation is 98% on room air. She repeatedly falls asleep and is combative during the exam. Laboratory values are notable for a potassium of 3.0 mEq/L. The patient is given normal saline with potassium. Which of the following is the most appropriate treatment for this patient?
- A. Rifaximin
- B. Lactulose (Correct Answer)
- C. Nadolol
- D. Ciprofloxacin
- E. Protein-restricted diet
Portal hypertension complications Explanation: ***Lactulose***
- The patient's symptoms (confusion, agitation, somnolence) following **TIPS placement** and with a history of **cirrhosis** are highly suggestive of **hepatic encephalopathy**. Lactulose is a first-line treatment as it acidifies the colon, converting ammonia (a neurotoxin) to ammonium, which is then trapped and excreted.
- Additionally, this patient has **hypokalemia**, which can exacerbate hepatic encephalopathy by increasing renal ammonia production due to intracellular potassium shifts. Correcting hypokalemia is crucial alongside lactulose therapy.
*Rifaximin*
- Rifaximin is a non-absorbable antibiotic that can be used as an **adjunctive therapy** in hepatic encephalopathy, particularly in patients who do not respond adequately to lactulose or in whom lactulose is contraindicated.
- It works by reducing the number of **ammonia-producing bacteria** in the gut, but it is not the primary or initial treatment of choice for acute hepatic encephalopathy and is typically used after lactulose.
*Nadolol*
- Nadolol is a **non-selective beta-blocker** primarily used to prevent rebleeding from esophageal varices by reducing portal pressure.
- It does not directly treat or improve the symptoms of **hepatic encephalopathy** and is not indicated for the acute management of this condition.
*Ciprofloxacin*
- Ciprofloxacin is an antibiotic sometimes used to prevent **spontaneous bacterial peritonitis (SBP)** in patients with cirrhosis and ascites, or for the treatment of **bacterial infections**.
- While infections can precipitate hepatic encephalopathy, ciprofloxacin is not a direct treatment for encephalopathy itself, nor is there evidence of active infection here (e.g., fever, leukocytosis) that would necessitate its use over lactulose.
*Protein-restricted diet*
- In the past, protein restriction was a common recommendation for hepatic encephalopathy to reduce ammonia production from protein catabolism. However, severe protein restriction can lead to **malnutrition and sarcopenia**, which are detrimental in cirrhotic patients.
- Current guidelines recommend maintaining adequate protein intake and only briefly restricting protein (if at all) in severe, refractory cases, as it is generally not helpful for acute management and can worsen patient outcomes in the long term.
Portal hypertension complications US Medical PG Question 4: A 55-year-old patient who immigrated from the Middle East to the United States 10 years ago presents to the emergency department because of excessive weakness, abdominal discomfort, and weight loss for the past 10 months. He has had type 2 diabetes mellitus for 10 years for which he takes metformin. He had an appendectomy 12 years ago in his home country, and his postoperative course was not complicated. He denies smoking and drinks alcohol socially. His blood pressure is 110/70 mm Hg, pulse is 75/min, and temperature is 37.1°C (98.7°F). On physical examination, the patient appears exhausted, and his sclerae are yellowish. A firm mass is palpated in the right upper abdominal quadrant. Abdominal ultrasonography shows liver surface nodularity, splenomegaly, and increased diameter of the portal vein. Which of the following is the most common complication of this patient condition?
- A. Hepatopulmonary syndrome
- B. Ascites (Correct Answer)
- C. Hepatic encephalopathy
- D. Hepatorenal syndrome
- E. Hepatic osteodystrophy
Portal hypertension complications Explanation: ***Ascites***
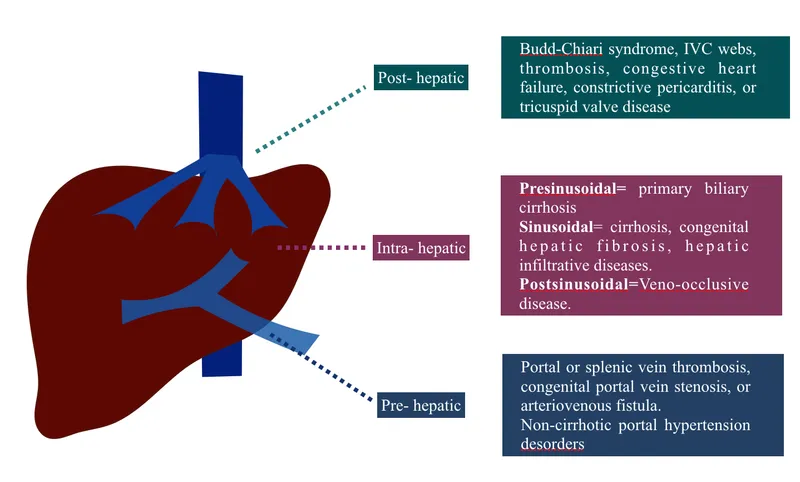
- The patient presents with classic signs of **portal hypertension** (splenomegaly, increased portal vein diameter, liver surface nodularity suggesting cirrhosis), and **ascites** is the most common and often the earliest major complication.
- The presence of **abdominal discomfort** and an **RUQ mass** could be related to severe liver disease and its complications, including fluid accumulation or an underlying liver malignancy often associated with cirrhosis.
*Hepatopulmonary syndrome*
- This involves **intrapulmonary vascular dilatations** in the setting of liver disease leading to oxygenation defects, typically marked by platypnea and orthodeoxia, which are not described here.
- While a complication of **cirrhosis**, it is less common than ascites and typically presents with respiratory symptoms not highlighted in this case.
*Hepatic encephalopathy*
- Characterized by **neuropsychiatric symptoms** due to the accumulation of toxins (e.g., ammonia) that the liver cannot detoxify.
- The patient's presentation mainly focuses on physical weakness, abdominal issues, and jaundice, without mention of confusion, asterixis, or altered mental status.
*Hepatorenal syndrome*
- This is a form of **functional renal failure** that occurs in patients with advanced liver disease, presenting with rapidly progressive azotemia due to severe splanchnic vasodilation.
- It is a **later and more severe complication** of liver failure, and while possible, ascites is typically seen much earlier and more frequently.
*Hepatic osteodystrophy*
- This refers to a group of **metabolic bone disorders** (osteoporosis, osteomalacia) that can occur in chronic liver disease.
- While it can manifest as bone pain, it is not a direct or immediate complication of portal hypertension and would not explain the acute abdominal findings.
Portal hypertension complications US Medical PG Question 5: A 36-year-old man is brought to the emergency department by his girlfriend because of increasing confusion for the past 6 hours. He drinks large amounts of alcohol daily and occasionally uses illicit drugs. He is lethargic and oriented only to person. Physical examination shows jaundice, hepatomegaly, and scattered petechiae over the trunk and back. Neurologic examination shows normal, reactive pupils and a flapping tremor when the wrists are extended. A drug with which of the following mechanism of action would be most appropriate for this patient's condition?
- A. Production of NH3
- B. Activation of GABA receptors
- C. Excretion of free iron
- D. Inhibition of D2 receptors
- E. Excretion of NH4 (Correct Answer)
Portal hypertension complications Explanation: ***Excretion of NH4***
- The patient presents with **hepatic encephalopathy**, characterized by **confusion**, **jaundice**, **hepatomegaly**, **petechiae**, and a **flapping tremor (asterixis)**, stemming from chronic alcohol abuse and liver damage. The main pathophysiology in hepatic encephalopathy is the accumulation of **ammonia (NH3)**, which is neurotoxic.
- Excretion of **NH4** (ammonium) through drug mechanisms such as **lactulose** (which acidifies the colon, trapping ammonia as ammonium for excretion) is the primary therapeutic target to reduce ammonia levels and improve neurological symptoms.
*Production of NH3*
- This mechanism would exacerbate the patient's condition by increasing the toxic load of **ammonia (NH3)**, which is already elevated in hepatic encephalopathy.
- Therapeutic interventions aim to decrease, not increase, ammonia production or absorption.
*Activation of GABA receptors*
- While **GABA receptor activation** is involved in the neurological effects of some substances that contribute to confusion, it is not the primary target for treating the underlying pathophysiology of **hepatic encephalopathy**.
- Medications that activate GABA receptors (e.g., benzodiazepines) can worsen encephalopathy by further depressing CNS function.
*Excretion of free iron*
- **Iron overload** can cause liver damage, but the acute confusion and flapping tremor are more indicative of **hepatic encephalopathy** due to ammonia toxicity, not primarily iron accumulation.
- Excreting free iron (e.g., with chelation therapy) is for conditions like hemochromatosis and would not address the immediate, life-threatening neurological symptoms in this patient.
*Inhibition of D2 receptors*
- This mechanism is characteristic of some **antipsychotic medications**. While dopamine imbalances can play a role in some neurological disorders, inhibiting D2 receptors is not a primary therapeutic target for **hepatic encephalopathy**.
- Such medications could have side effects that might complicate the clinical picture in a patient with acute liver failure.
Portal hypertension complications US Medical PG Question 6: A 54-year-old man with alcoholism comes to the emergency department because of vomiting blood for 6 hours. He has had 3–4 episodes in which he has vomited dark red blood during this period. He has had no epigastric pain or tarry stools. On arrival, his temperature is 37.3°C (99.1°F), pulse is 134/min, and blood pressure is 80/50 mm Hg. He is resuscitated with 0.9% saline and undergoes an emergency upper endoscopy, which shows actively bleeding varices. Band ligation of the varices is done and hemostasis is achieved. He is diagnosed with Child class B cirrhosis. He is concerned about the possibility of recurrence of such an episode. He is asked to abstain from alcohol, to which he readily agrees. In addition to non-selective beta-blocker therapy, which of the following is the most appropriate recommendation to prevent future morbidity and mortality from this condition?
- A. Terlipressin
- B. Transjugular intrahepatic portosystemic shunt
- C. Variceal sclerotherapy
- D. Variceal ligation (Correct Answer)
- E. Octreotide therapy
Portal hypertension complications Explanation: ***Variceal ligation***
- **Endoscopic variceal ligation (EVL) is the gold standard for secondary prophylaxis** (preventing re-bleeding) in patients who have already experienced a variceal hemorrhage.
- It involves placing elastic bands on varices to occlude them, leading to fibrosis and eradication of the varices.
*Terlipressin*
- **Terlipressin is a vasoconstrictor primarily used to control acute variceal bleeding**, not for long-term secondary prevention.
- It reduces portal pressure by causing splanchnic vasoconstriction but is not suitable for chronic management.
*Transjugular intrahepatic portosystemic shunt*
- **TIPS is typically reserved for patients who fail endoscopic and pharmacological therapies** or have refractory ascites.
- While effective in reducing portal pressure, it carries risks such as **hepatic encephalopathy** and is not the first-line secondary prevention strategy.
*Variceal sclerotherapy*
- **Variceal sclerotherapy involves injecting a sclerosant solution into or adjacent to varices to induce thrombosis and fibrosis.**
- It is an alternative to band ligation but is generally **less preferred for secondary prophylaxis due to a higher rate of complications** like esophageal ulceration and re-bleeding.
*Octreotide therapy*
- **Octreotide, a somatostatin analog, is used to reduce splanchnic blood flow and portal pressure during acute variceal bleeding episodes.**
- It is **not recommended for long-term secondary prophylaxis** and is typically used in conjunction with endoscopic therapy for acute management.
Portal hypertension complications US Medical PG Question 7: A 64-year-old man comes to the emergency department complaining of fatigue and abdominal distension. He has a remote history of intravenous drug use. Vital signs include a normal temperature, blood pressure of 120/80 mm Hg, and a pulse of 75/min. Physical examination reveals jaundice and a firm liver. Abdominal ultrasonography shows liver surface nodularity, moderate splenomegaly, and increased diameter of the portal vein. Complete blood count of the patient is shown:
Hemoglobin 14 g/dL
Mean corpuscular volume 90/μm3
Mean corpuscular hemoglobin 30 pg/cell
Mean corpuscular hemoglobin concentration 34%
Leukocyte count 7,000/mm3
Platelet count 50,000/mm3
Which of the following best represents the mechanism of low platelet count in this patient?
- A. Platelet sequestration (Correct Answer)
- B. Dilutional effect
- C. Bone marrow-based disorder
- D. Increased platelet clearance
- E. Genetic disorder
Portal hypertension complications Explanation: ***Platelet sequestration***
- The patient's history of IV drug use, jaundice, abdominal distension, firm liver, splenomegaly, and increased portal vein diameter are highly suggestive of **portal hypertension** due to **cirrhosis**, which often leads to **splenomegaly**.
- An enlarged spleen (splenomegaly) sequesters a disproportionately high percentage of the body's platelets, leading to **thrombocytopenia**, even if total platelet production is normal.
- **Splenic sequestration** is the **primary mechanism** of thrombocytopenia in cirrhosis with portal hypertension; up to **90% of platelets** can be sequestered in an enlarged spleen.
- Additionally, the diseased liver produces less **thrombopoietin (TPO)**, which contributes to reduced platelet production, but sequestration remains the dominant mechanism.
*Dilutional effect*
- A dilutional effect on platelet count typically occurs with **massive transfusions** of packed red blood cells and crystalloids, which is not indicated in this patient's presentation.
- While fluid overload can dilute blood components, the patient's symptoms point specifically to a **liver pathology** and related complications, not simply volume expansion.
*Bone marrow-based disorder*
- A primary bone marrow disorder would likely affect other cell lines as well, but the patient's hemoglobin and leukocyte counts are within normal limits, making a general **bone marrow suppression** less likely.
- Furthermore, the strong evidence of **cirrhosis and portal hypertension** provides a more direct and common explanation for isolated thrombocytopenia in this context.
*Increased platelet clearance*
- While increased platelet clearance can cause thrombocytopenia (e.g., in immune thrombocytopenia or thrombotic microangiopathies), there are no signs of increased destruction or consumption in this case.
- Conditions involving increased clearance usually present with other features like petechiae, purpura, or schistocytes, which are not mentioned.
- The clinical picture is most consistent with **sequestration** rather than **destruction**.
*Genetic disorder*
- Genetic disorders causing thrombocytopenia typically present much earlier in life or have a family history, which does not fit this patient's age and clinical presentation.
- The patient's history of **IV drug use** and the findings of advanced liver disease indicate an **acquired condition**, not a congenital one.
Portal hypertension complications US Medical PG Question 8: A 60-year-old man is rushed to the emergency room after he was found unconscious in bed that afternoon. The patient’s wife says he has been confused and irritable for the past several days. She says he has a history of chronic daily alcohol abuse and has been hospitalized multiple times with similar symptoms His temperature is 37°C (98.6°F), the blood pressure is 110/80 mm Hg, the pulse is 90/min, and the respiratory rate is 14/min. On physical examination, the patient is minimally responsive to painful stimuli. His abdomen is distended with positive shifting dullness. Laboratory results are as follows:
Complete blood count
Hematocrit 35%
Platelets 100,000/mm3
White blood cells 5000/mm3
Liver function studies
Serum Albumin 2 g/dL
Alkaline phosphatase (ALP) 200 IU/L
Aspartate aminotransferase (AST) 106 IU/L
Alanine aminotransferase (ALT) 56 IU/L
The patient is admitted to the hospital and started on the appropriate treatment to improve his mental status. Which of the following best describes the mechanism of action of the drug that is most likely used to treat this patient’s symptoms?
- A. Prevents the conversion of ammonia into ammonium
- B. Increases ammonia production and absorption
- C. Increases pH in the gastrointestinal lumen
- D. Decreases pH in the gastrointestinal lumen (Correct Answer)
- E. Decreases the colonic concentration of bacteria
Portal hypertension complications Explanation: ***Decreases pH in the gastrointestinal lumen***
- The patient's presentation with altered mental status, chronic alcohol abuse, distended abdomen with shifting dullness (*ascites*), and abnormal liver function tests (low *albumin*, elevated *AST/ALT*) is highly suggestive of **hepatic encephalopathy**.
- **Lactulose** is the mainstay treatment for hepatic encephalopathy, and its mechanism involves lowering the colonic pH, which converts ammonia (NH3) into poorly absorbed ammonium (NH4+), thereby reducing systemic ammonia levels.
*Prevents the conversion of ammonia into ammonium*
- This statement is incorrect; the goal of treatment for hepatic encephalopathy is to **promote** the conversion of ammonia to ammonium to prevent its absorption.
- Ammonia (NH3) is lipophilic and readily crosses the blood-brain barrier, while ammonium (NH4+) is hydrophilic and poorly absorbed from the gut.
*Increases ammonia production and absorption*
- This is incorrect and would exacerbate hepatic encephalopathy by increasing the toxic ammonia load.
- The primary aim of treatment is to **reduce** ammonia production and enhance its excretion or conversion into a non-absorbable form.
*Increases pH in the gastrointestinal lumen*
- Elevating the pH in the colon would favor the production of **ammonia (NH3)** from ammonium (NH4+), leading to increased systemic ammonia absorption and worsening hepatic encephalopathy.
- Therefore, this mechanism would be detrimental to a patient with hepatic encephalopathy.
*Decreases the colonic concentration of bacteria*
- While **rifaximin** (a non-absorbable antibiotic) does decrease ammonia-producing bacteria in the gut and is used in conjunction with lactulose, this option describes the mechanism of an antibiotic, not the primary action of lactulose.
- Lactulose itself does not primarily decrease the overall concentration of gut bacteria, but rather modifies the *metabolic activity* of the existing bacteria.
Portal hypertension complications US Medical PG Question 9: A 38-year-old woman comes to the physician because of a 3-month history of moderate abdominal pain that is unresponsive to medication. She has a history of two spontaneous abortions at 11 and 12 weeks' gestation. Ultrasound examination of the abdomen shows normal liver parenchyma, a dilated portal vein, and splenic enlargement. Upper endoscopy shows dilated submucosal veins in the lower esophagus. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased serum bilirubin levels
- B. Increased prothrombin time
- C. Thrombocytopenia (Correct Answer)
- D. Hepatic venous congestion
- E. Councilman bodies
Portal hypertension complications Explanation: ***Thrombocytopenia***
- The patient's **recurrent spontaneous abortions** suggest **antiphospholipid syndrome (APS)**, a hypercoagulable state that predisposes to both arterial and venous thrombosis.
- APS likely caused **portal vein thrombosis**, leading to **prehepatic portal hypertension** (dilated portal vein, esophageal varices, and splenomegaly) with **normal liver parenchyma**.
- The **splenomegaly** causes **hypersplenism**, resulting in **thrombocytopenia** due to splenic sequestration and increased destruction of platelets.
- While APS can also cause immune-mediated thrombocytopenia directly, the primary mechanism here is hypersplenism secondary to portal hypertension.
*Increased serum bilirubin levels*
- Elevated bilirubin indicates **hepatocellular dysfunction** or **biliary obstruction**.
- The ultrasound shows **normal liver parenchyma**, making significant hepatocellular damage unlikely.
- Portal vein thrombosis without liver parenchymal disease does not typically cause hyperbilirubinemia.
*Increased prothrombin time*
- Prolonged PT reflects impaired **hepatic synthesis of coagulation factors** (II, VII, IX, X).
- With **normal liver parenchyma** on imaging, synthetic liver function should be preserved.
- Portal vein thrombosis alone does not impair hepatocyte function or coagulation factor synthesis.
*Hepatic venous congestion*
- This finding is characteristic of **Budd-Chiari syndrome** (hepatic vein thrombosis), which presents with hepatomegaly, ascites, and signs of hepatic outflow obstruction.
- The patient's findings (dilated **portal vein**, normal liver parenchyma) indicate **portal vein thrombosis** causing **prehepatic portal hypertension**, not posthepatic venous congestion.
*Councilman bodies*
- These are **eosinophilic apoptotic hepatocytes** seen in acute liver injury (viral hepatitis, yellow fever, toxic injury).
- **Normal liver parenchyma** on ultrasound excludes significant hepatocellular necrosis.
- This finding is unrelated to thrombotic disorders or portal hypertension.
Portal hypertension complications US Medical PG Question 10: A 59-year-old man presents to the emergency department with a sudden onset of severe pain (10/10 in severity) between the shoulder blades. He describes the pain as tearing in nature. Medical history is positive for essential hypertension for 11 years. The patient has smoked 10–15 cigarettes daily for the past 30 years. His temperature is 36.6°C (97.8°F), the heart rate is 107/min, and the blood pressure is 179/86 mm Hg in the right arm and 157/72 mm Hg in the left arm. CT scan of the chest shows an intimal flap limited to the descending thoracic aorta. Which of the following best describes the most likely predisposing factor for this condition?
- A. Coronary atherosclerosis
- B. Aortic coarctation
- C. Hypertensive urgency
- D. Aortic atherosclerosis
- E. Abnormal elastic properties of the aorta (Correct Answer)
Portal hypertension complications Explanation: ***Abnormal elastic properties of the aorta***
- Chronic **hypertension** (11 years) is the #1 risk factor for aortic dissection, causing **cystic medial degeneration** (breakdown of elastic fibers and smooth muscle in the tunica media).
- This degenerative process results in **abnormal elastic properties** and weakening of the aortic wall, predisposing to dissection.
- The tearing pain, blood pressure differential between arms, and CT findings of intimal flap are classic for **Type B aortic dissection**.
- While often associated with connective tissue disorders in younger patients, cystic medial degeneration is also the pathophysiologic result of chronic hypertension in older patients.
*Aortic atherosclerosis*
- Atherosclerosis primarily affects the **intima** layer, while aortic dissection occurs in the **media** layer.
- Though hypertension and smoking contribute to atherosclerosis, this is not the primary predisposing mechanism for dissection.
- The underlying pathology is medial degeneration with abnormal elastic properties, not atherosclerotic plaque.
*Coronary atherosclerosis*
- This affects the coronary arteries supplying the heart, not the aortic wall structure.
- Does not explain the anatomical location of dissection or the tearing interscapular pain.
- Not a predisposing factor for aortic dissection.
*Hypertensive urgency*
- This refers to elevated blood pressure without acute end-organ damage.
- The patient has **aortic dissection**, which represents acute end-organ damage (hypertensive emergency, not urgency).
- While hypertension can precipitate dissection, the underlying **predisposing factor** is the chronic medial wall changes (abnormal elastic properties), not the acute blood pressure elevation itself.
*Aortic coarctation*
- This is a **congenital** narrowing of the aorta, typically diagnosed in childhood or young adulthood.
- Classic finding is upper extremity hypertension with **lower extremity hypotension** (opposite pattern from arm-to-arm differential seen in dissection).
- The patient's age, presentation, and 11-year history of essential hypertension make this unlikely.
More Portal hypertension complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.