Non-alcoholic fatty liver disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Non-alcoholic fatty liver disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Non-alcoholic fatty liver disease US Medical PG Question 1: A 20-year-old man presents to the doctor's office for advice on improving his health. He admits to eating mostly junk food, and he knows that he should lose some weight. His daily physical activity is limited to walking around the college campus between classes. Except for an occasional headache for which he takes acetaminophen, he has no health concerns and takes no other medications. He denies smoking and illicit drug use, but admits to occasional beer binge drinking on weekends. He is sexually active with his current girlfriend and regularly uses condoms. His mother has type 2 diabetes mellitus and obesity, while his father has hypertension and hypercholesterolemia. The pulse is 74/min, the respiratory rate is 16/min, and the blood pressure is 130/76 mm Hg. The body mass index (BMI) is 29 kg/m2. Physical examination reveals an overweight young male, and the rest is otherwise unremarkable. The routine lab test results are as follows:
Serum Glucose (fasting) 100 mg/dL
Serum Electrolytes:
Sodium 141 mEq/L
Potassium 4.0 mEq/L
Chloride 100 mEq/L
Cholesterol, total 190 mg/dL
HDL-cholesterol 42 mg/dL
LDL-cholesterol 70 mg/dL
Triglycerides 184 mg/dL
Urinalysis:
Glucose Negative
Ketones Negative
Leukocytes Negative
Nitrites Negative
RBCs Negative
Casts Negative
Which of the following lifestyle changes would most likely benefit this patient the most?
- A. A low sodium diet
- B. Starting a multivitamin
- C. Increasing daily water intake
- D. Weight reduction (Correct Answer)
- E. Increasing dietary fiber
Non-alcoholic fatty liver disease Explanation: ***Weight reduction***
- The patient has a **BMI of 29 kg/m2**, which classifies him as **overweight**, and his diet consists mostly of junk food, making weight reduction a primary and impactful lifestyle change.
- Weight loss significantly improves multiple health markers, including **blood pressure**, **lipid profile**, and **insulin sensitivity**, reducing his risk for conditions like **type 2 diabetes** and **hypertension** that run in his family.
- The patient shows early signs of **metabolic syndrome** (elevated BP, low HDL 42 mg/dL, triglycerides 184 mg/dL, impaired fasting glucose 100 mg/dL), which weight reduction directly addresses.
*A low sodium diet*
- While his father has hypertension, this patient's blood pressure is **130/76 mm Hg**, which is in the **elevated range** (120-129/<80 mm Hg), not yet meeting criteria for hypertension (≥130/80 mm Hg).
- While a low sodium diet is generally healthy and can help prevent hypertension, addressing his **overweight status** and **poor dietary habits** would yield more comprehensive benefits first.
*Starting a multivitamin*
- The patient has no symptoms or signs of **nutrient deficiencies**, and his routine lab tests are normal.
- There is generally **no strong evidence** to support routine multivitamin supplementation in otherwise healthy individuals with no specific deficiencies.
*Increasing daily water intake*
- There is no indication that the patient is **dehydrated** or has any conditions that would specifically benefit from a significant increase in water intake.
- While adequate hydration is important, it is **not the most impactful intervention** for his current health profile compared to addressing his diet and weight.
*Increasing dietary fiber*
- Increasing dietary fiber is beneficial for **digestive health** and can help with **satiety** and **cholesterol management**.
- However, his primary issue is his overall "junk food" diet and overweight status; tackling these directly through **comprehensive dietary changes** (which would include more fiber) and **weight reduction** would be more beneficial than focusing solely on fiber intake initially.
Non-alcoholic fatty liver disease US Medical PG Question 2: A 46-year-old woman presents to her primary care provider for itching. She reports that she has always had dry skin but that the itching has gotten significantly worse over the last few years. The patient also endorses fatigue and dull abdominal pain. Her past medical history includes Hashimoto’s thyroiditis, mitral valve prolapse, and osteoarthritis. She takes levothyroxine and ibuprofen for pain in her knees. The patient drinks 2-3 beers per week. She has a 10 pack-year smoking history but quit 15 years ago. She denies any family history of cancer. On physical exam, her sclera are anicteric. Her abdomen is soft and tender to palpation in the right upper quadrant. Her bowel sounds are normal and hepatomegaly is present. A right upper quadrant ultrasound shows no evidence of extrahepatic biliary dilation. Laboratory studies are performed which reveal the following:
Aspartate aminotransferase (AST): 76 U/L
Alanine aminotransferase (ALT): 57 U/L
Alkaline phosphatase: 574 U/L
Total bilirubin: 1.6 mg/dL
This patient is most likely to have which of the following additional findings?
- A. Anti-smooth muscle antibodies
- B. Skin hyperpigmentation
- C. Anti-neutrophil cytoplasmic antibodies
- D. Personality changes
- E. Hyperlipidemia (Correct Answer)
Non-alcoholic fatty liver disease Explanation: ***Hyperlipidemia***
- This patient presents with symptoms and lab findings highly suggestive of **primary biliary cholangitis (PBC)**, including pruritus, fatigue, dull abdominal pain with RUQ tenderness, hepatomegaly, elevated AST/ALT, significantly elevated alkaline phosphatase, and mild hyperbilirubinemia.
- **Hyperlipidemia** is one of the most common metabolic complications of PBC, occurring in up to 75-85% of patients, often presenting early in the disease course due to impaired bile acid secretion and altered cholesterol metabolism.
- Total cholesterol can be markedly elevated (often >300 mg/dL), and this finding is more consistent and universal than other potential manifestations.
*Anti-smooth muscle antibodies*
- **Anti-smooth muscle antibodies (ASMA)** are primarily associated with **autoimmune hepatitis**, a condition characterized by significant elevations in transaminases (typically ALT > AST) rather than alkaline phosphatase predominance.
- PBC is characterized by **anti-mitochondrial antibodies (AMA)**, which are present in 90-95% of cases, not ASMA.
- The marked elevation in **alkaline phosphatase** and prominent pruritus point to a cholestatic process (PBC) rather than hepatocellular injury (autoimmune hepatitis).
*Skin hyperpigmentation*
- **Skin hyperpigmentation** does occur in PBC (in approximately 25-50% of patients) due to melanin deposition, particularly in sun-exposed areas and areas of prior scratching.
- However, **hyperlipidemia** is both more prevalent (affecting 75-85% vs 25-50%) and occurs earlier in the disease course, making it the most likely additional finding in this patient.
- Hyperpigmentation typically develops later as the disease progresses.
*Anti-neutrophil cytoplasmic antibodies*
- **Anti-neutrophil cytoplasmic antibodies (ANCA)** are primarily associated with **vasculitis**, such as granulomatosis with polyangiitis (Wegener's) or microscopic polyangiitis.
- This patient's clinical picture, with prominent pruritus and cholestatic liver enzyme pattern, does not suggest an underlying vasculitic process.
*Personality changes*
- **Personality changes** can be a feature of **hepatic encephalopathy**, which occurs in advanced liver failure due to the accumulation of neurotoxins like ammonia.
- While PBC can progress to cirrhosis and liver failure, the current presentation with only mild hyperbilirubinemia (1.6 mg/dL) and absence of neurological signs does not suggest significant encephalopathy at this stage.
- This would be expected only in advanced/decompensated disease.
Non-alcoholic fatty liver disease US Medical PG Question 3: A 62-year-old woman with a history of hypertension, hyperlipidemia, and rheumatoid arthritis presents for evaluation of elevated serum liver chemistries. She has had three months of intense, unremitting itching. Current medications include chlorthalidone, atorvastatin, and ibuprofen. Physical exam is unremarkable. Laboratory studies show aspartate aminotransferase (AST) 42 units/L, alanine aminotransferase (ALT) 39 units/L, alkaline phosphatase 790 units/L, total bilirubin 0.8 mg/dL, and antimitochondrial antibody titer 1:80. What do you expect to see on liver biopsy?
- A. Intrahepatic bile duct destruction (Correct Answer)
- B. Bile plugging of hepatocytes and bile ducts
- C. Granulomas in portal tracts
- D. Intrahepatic and extra hepatic bile duct destruction
- E. Lymphoplasmacytic and eosinophilic infiltration of portal tracts
Non-alcoholic fatty liver disease Explanation: ***Intrahepatic bile duct destruction***
- The patient's presentation with **pruritus**, significantly **elevated alkaline phosphatase**, relatively normal AST/ALT, and a **positive antimitochondrial antibody (AMA)** strongly suggests **primary biliary cholangitis (PBC)**.
- The hallmark histopathological finding in PBC is the **destruction of small and medium-sized intrahepatic bile ducts** by chronic inflammation.
*Bile plugging of hepatocytes and bile ducts*
- This finding is characteristic of significant **biliary obstruction** (cholestasis), where bile flow is severely impaired, leading to the accumulation of bile within hepatocytes and bile ducts.
- While there is cholestasis in PBC (evidenced by high alkaline phosphatase), the primary injury is immune-mediated destruction of ducts, not simply plugging, and bilirubin is not significantly elevated, indicating less severe obstruction.
*Granulomas in portal tracts*
- While **epithelioid granulomas** can be seen in PBC (in up to 30% of cases), they are not the **defining histologic feature**—the bile duct destruction is.
- Granulomas are also more commonly associated with **sarcoidosis** and certain **drug-induced liver injuries**.
- The constellation of symptoms and labs points directly to classic PBC with its characteristic bile duct destruction.
*Intrahepatic and extra hepatic bile duct destruction*
- **Extrahepatic bile duct destruction** is typical of conditions like **primary sclerosing cholangitis (PSC)**, which primarily affects larger intrahepatic and extrahepatic bile ducts and is often associated with inflammatory bowel disease.
- The positive AMA and specific pattern of liver enzyme elevation are highly suggestive of PBC, which is confined to the small and medium intrahepatic ducts, rather than PSC.
*Lymphoplasmacytic and eosinophilic infiltration of portal tracts*
- **Eosinophilic infiltration** can be prominent in allergic reactions, parasitic infections, or some forms of drug-induced liver injury, but it's not the defining feature of PBC.
- While **lymphoplasmacytic infiltration** is present in PBC, it is specifically directed at and causes destruction of the bile ducts, rather than being a generalized, non-specific infiltration of the portal tracts.
Non-alcoholic fatty liver disease US Medical PG Question 4: A 57-year-old woman comes to the physician for a routine health maintenance examination. She has well-controlled type 2 diabetes mellitus, for which she takes metformin. She is 163 cm (5 ft 4 in) tall and weighs 84 kg (185 lb); BMI is 31.6 kg/m2. Her blood pressure is 140/92 mm Hg. Physical examination shows central obesity, with a waist circumference of 90 cm. Laboratory studies show:
Fasting glucose 94 mg/dl
Total cholesterol 200 mg/dL
High-density lipoprotein cholesterol 36 mg/dL
Triglycerides 170 mg/dL
Without treatment, this patient is at greatest risk for which of the following conditions?
- A. Osteoporosis
- B. Rheumatoid arthritis
- C. Subarachnoid hemorrhage
- D. Central sleep apnea
- E. Liver cirrhosis (Correct Answer)
Non-alcoholic fatty liver disease Explanation: ***Liver cirrhosis***
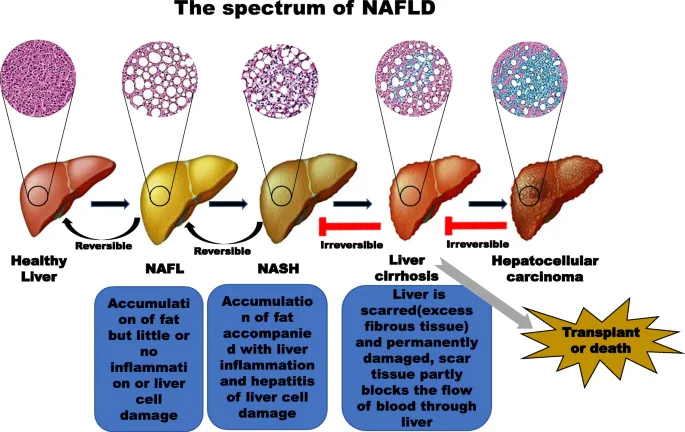
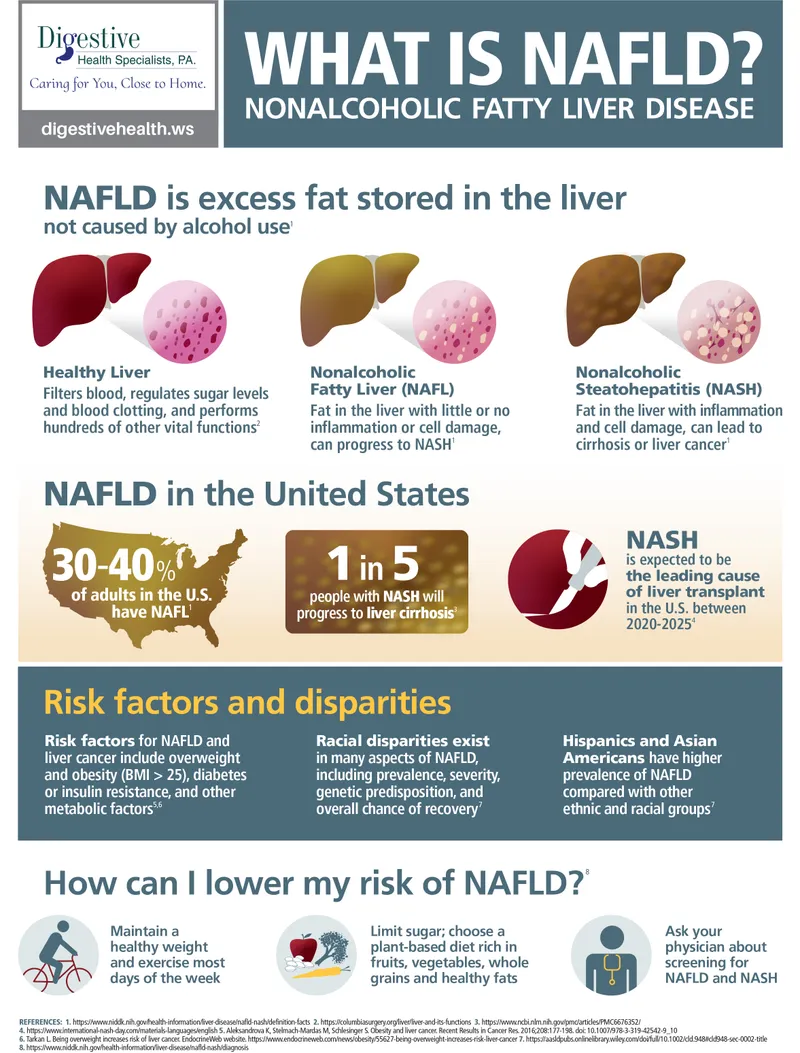
* This patient has **metabolic syndrome**, characterized by **central obesity** (waist >88 cm in women), **hypertension** (≥130/85 mm Hg), **low HDL cholesterol** (<50 mg/dL in women), **elevated triglycerides** (≥150 mg/dL), and **type 2 diabetes mellitus**.
* Metabolic syndrome is strongly associated with **non-alcoholic fatty liver disease (NAFLD)**, which affects **70-90% of patients** with this condition.
* NAFLD can progress to **non-alcoholic steatohepatitis (NASH)**, then to **hepatic fibrosis**, and ultimately **cirrhosis**—making this patient's greatest long-term risk without intervention.
* NAFLD is now the **leading cause of chronic liver disease** in developed countries, and the combination of obesity, insulin resistance, and dyslipidemia directly promotes hepatic lipid accumulation and inflammation.
*Incorrect: Osteoporosis*
* While common in post-menopausal women, **obesity is generally protective against osteoporosis** due to increased weight-bearing stress on bones and higher estrogen levels from adipose tissue aromatization.
* No specific risk factors for osteoporosis (e.g., corticosteroid use, smoking, low calcium intake) are present.
*Incorrect: Rheumatoid arthritis*
* This is an **autoimmune condition** not associated with metabolic syndrome.
* The patient has no symptoms of joint pain, morning stiffness, or synovitis that would suggest rheumatoid arthritis.
* Metabolic factors do not increase the risk of developing rheumatoid arthritis.
*Incorrect: Subarachnoid hemorrhage*
* While **hypertension** is a risk factor for hemorrhagic stroke, subarachnoid hemorrhage is more specifically associated with **ruptured aneurysms** or **arteriovenous malformations**.
* The patient's moderately elevated blood pressure poses some cardiovascular risk, but this is not the greatest risk compared to the progressive liver disease associated with metabolic syndrome.
*Incorrect: Central sleep apnea*
* **Central sleep apnea** (cessation of respiratory effort) is primarily associated with **heart failure**, **stroke**, or **opioid use**—not metabolic syndrome.
* **Obstructive sleep apnea** (OSA) is what's associated with obesity and metabolic syndrome, but that is not an option here.
* While this patient may be at risk for OSA, central sleep apnea is not the primary concern in metabolic syndrome.
Non-alcoholic fatty liver disease US Medical PG Question 5: A 48-year-old man presents to the emergency department with shortness of breath. He reports that 6 months ago he was able to walk several miles without stopping. Yesterday, he became short of breath walking from his bed to the bathroom. He also endorses worsening abdominal distension and leg swelling, which he reports is new from several months ago. The patient has a past medical history of hypertension and hyperlipidemia. He admits to drinking 6-8 beers daily for the past 10 years. On physical exam, the patient has moderate abdominal distension and pitting edema to the knee. Crackles are present at the bilateral bases. Laboratory testing reveals the following:
Hemoglobin: 13.4 g/dL
Mean corpuscular volume (MCV): 102 μm³
Leukocyte count: 11,200/mm³ with normal differential
Platelet count: 256,000/mm³
Serum:
Na+: 137 mEq/L
Cl-: 100 mEq/L
K+: 4.2 mEq/L
HCO3-: 25 mEq/L
BUN: 18 mg/dL
Glucose: 126 mg/dL
Creatinine: 0.9 mg/dL
Alkaline phosphatase: 88 U/L
Aspartate aminotransferase (AST): 212 U/L
Alanine aminotransferase (ALT): 104 U/L
Which of the following is the best next step in management?
- A. Antiviral therapy
- B. Alcohol cessation (Correct Answer)
- C. Immunosuppressive therapy
- D. Hormone replacement
- E. Vitamin repletion
Non-alcoholic fatty liver disease Explanation: ***Alcohol cessation***
- The patient exhibits clear signs of **decompensated cirrhosis** due to chronic alcohol use, including **abdominal distension** (ascites), **leg swelling** (peripheral edema), and **shortness of breath** (likely due to fluid overload or hepatopulmonary syndrome). The elevated AST/ALT with an AST:ALT ratio > 2:1 is also suggestive of **alcoholic liver disease**.
- **Alcohol cessation** is the most critical intervention to halt the progression of liver damage and improve outcomes in alcoholic liver disease.
*Antiviral therapy*
- Antiviral therapy is indicated for **viral hepatitis (e.g., hepatitis B or C)**, but the patient's history of heavy alcohol consumption and the AST:ALT ratio > 2:1 specifically point towards **alcoholic liver disease**, not viral hepatitis.
- There is no lab or clinical evidence (e.g., positive hepatitis serologies) presented that would suggest a viral etiology requiring antiviral treatment.
*Immunosuppressive therapy*
- Immunosuppressive therapy is used for **autoimmune liver diseases** (e.g., autoimmune hepatitis) or conditions requiring immune modulation.
- The patient's history and lab findings are not consistent with an autoimmune liver disease, and there is no indication for immunosuppression in uncomplicated alcoholic liver disease.
*Hormone replacement*
- Hormone replacement is typically considered for **endocrine disorders** or **menopause**.
- There is no clinical or laboratory evidence to suggest any hormonal imbalance or deficiency in this male patient.
*Vitamin repletion*
- While patients with chronic alcoholism often have **vitamin deficiencies** (e.g., thiamine, folate), **vitamin repletion** alone will not address the underlying liver damage and decompensation this patient is experiencing.
- While it may be a supportive measure, it is not the most crucial next step for immediate management and preventing further progression of severe liver disease.
Non-alcoholic fatty liver disease US Medical PG Question 6: A 15-year-old girl comes to the physician for a well-child examination. She feels well. Her father has coronary artery disease and hypertension. Her mother has type 2 diabetes mellitus, hypercholesterolemia, and had a myocardial infarction at the age of 52 years. She is at the 25th percentile for height and above the 95th percentile for weight. Her BMI is 32 kg/m2. Her temperature is 37°C (98.6°F), pulse is 99/min, and blood pressure is 140/88 mm Hg. Physical examination shows no abnormalities. Random serum studies show:
Glucose 160 mg/dL
Creatinine 0.8 mg/dL
Total cholesterol 212 mg/dL
HDL-cholesterol 32 mg/dL
LDL-cholesterol 134 mg/dL
Triglycerides 230 mg/dL
In addition to regular aerobic physical activity, which of the following is the most appropriate next step in management?
- A. Atorvastatin therapy
- B. Reduced-calorie diet (Correct Answer)
- C. Fenofibrate therapy
- D. Metformin therapy
- E. Niacin therapy
Non-alcoholic fatty liver disease Explanation: ***Reduced-calorie diet***
- Given the patient's **obesity (BMI 32 kg/m2)**, **elevated blood pressure (140/88 mmHg)**, **impaired fasting glucose (160 mg/dL)**, and **dyslipidemia (high triglycerides, low HDL)**, lifestyle modifications, particularly a **reduced-calorie diet**, are the cornerstone of initial management. This approach aims to address the underlying metabolic cluster contributing to her risk.
- A **reduced-calorie diet** combined with regular aerobic physical activity can lead to weight loss, which in turn can improve blood pressure, glucose levels, and lipid profiles, thereby mitigating her significant risk factors for cardiovascular disease and type 2 diabetes.
*Atorvastatin therapy*
- **Atorvastatin (a statin)** is typically indicated for severe dyslipidemia, particularly elevated LDL-cholesterol, or in patients with established cardiovascular disease in adults. For adolescents, statin use is reserved for those with **severe primary hypercholesterolemia** unresponsive to lifestyle changes.
- While her **LDL is elevated (134 mg/dL)**, given her age and the multifactorial nature of her metabolic abnormalities, initial management should focus on lifestyle modifications before considering pharmacotherapy like statins.
*Fenofibrate therapy*
- **Fenofibrate** is primarily used to treat **severe hypertriglyceridemia** and to improve low HDL-cholesterol. While her **triglycerides are elevated (230 mg/dL)**, similar to statins, pharmacologic interventions for dyslipidemia in adolescents usually follow a trial of intensive lifestyle modifications.
- Addressing the patient's overall metabolic syndrome through weight loss and dietary changes is a more comprehensive initial approach, as it can simultaneously improve her dyslipidemia, hyperglycemia, and hypertension.
*Metformin therapy*
- **Metformin** is used to manage **type 2 diabetes mellitus** and often for **insulin resistance**, particularly in obese individuals. While her **random glucose is elevated (160 mg/dL)**, indicating impaired glucose regulation, a definitive diagnosis of type 2 diabetes or prediabetes requiring metformin typically involves fasting glucose levels, oral glucose tolerance tests, or HbA1c.
- For a 15-year-old with these findings, intensive lifestyle intervention to achieve weight loss is the **first-line therapy** to improve glucose metabolism and prevent the progression to type 2 diabetes.
*Niacin therapy*
- **Niacin** is used to reduce LDL-cholesterol and triglycerides, and to increase HDL-cholesterol. However, it can have significant side effects like flushing and hepatotoxicity.
- Its role in the management of dyslipidemia, especially in adolescents, is generally limited and considered after other agents or in specific conditions, as lifestyle modification remains the initial and most appropriate step.
Non-alcoholic fatty liver disease US Medical PG Question 7: A 31-year-old man presents to his primary care physician with shortness of breath. He states that he had a “cold” 2 weeks ago and since then has had a persistent cough and worsening shortness of breath. He denies fever, chills, chest pain, sore throat, or rhinorrhea. His medical history is significant for seasonal allergies. He uses fluticasone nasal spray. He had his tonsils removed when he was 8 years of age. His mother and maternal grandfather have cirrhosis, and his father has depression and hypertension. The patient endorses that he smokes tobacco socially on the weekends and uses marijuana daily. He drinks 1-2 beers after work with his co-workers most evenings. A chest radiograph shows hyperinflation of the lungs and hyperlucency. Routine labs are drawn, as shown below.
Serum:
Na+: 139 mEq/L
Cl-: 105 mEq/L
K+: 4.0 mEq/L
HCO3-: 26 mEq/L
Urea nitrogen: 15 mg/dL
Glucose: 100 mg/dL
Creatinine: 0.8 mg/dL
Alkaline phosphatase: 98 U/L
Aspartate aminotransferase (AST, GOT): 46 U/L
Alanine aminotransferase (ALT, GPT): 49 U/L
Pulmonary function tests are pending. Which of the following is most likely to confirm the patient’s diagnosis?
- A. Enzyme-linked immunosorbent assay (Correct Answer)
- B. Bronchoalveolar lavage
- C. Abdominal ultrasound
- D. Viral hepatitis serologies
- E. Pulmonary function tests
Non-alcoholic fatty liver disease Explanation: ***Enzyme-linked immunosorbent assay (ELISA)***
- This patient's presentation with **early-onset emphysema at age 31**, **hyperinflation and hyperlucency** on chest X-ray, and **strong family history of cirrhosis** (mother and maternal grandfather) strongly suggests **alpha-1 antitrypsin deficiency**.
- **ELISA is used to measure serum alpha-1 antitrypsin levels**, which is the key confirmatory test for this diagnosis. Low levels (<50-80 mg/dL) confirm the deficiency.
- Alpha-1 antitrypsin deficiency causes **panacinar emphysema** (especially in lower lobes) and can also cause **liver cirrhosis**, explaining the family history and mildly elevated transaminases.
- Once low levels are detected, **phenotyping or genotyping** can further characterize the specific mutation (most commonly PiZZ).
*Pulmonary function tests*
- PFTs would demonstrate **obstructive lung disease** with reduced FEV1/FVC ratio and confirm the presence of airflow limitation.
- However, PFTs are **non-specific** and would not distinguish alpha-1 antitrypsin deficiency from other causes of COPD/emphysema (smoking-related, chronic bronchitis, etc.).
- While diagnostically useful for characterizing severity, PFTs do not confirm the underlying etiology.
*Bronchoalveolar lavage*
- **Bronchoalveolar lavage (BAL)** is useful for diagnosing **infections**, **interstitial lung diseases**, **malignancies**, or **alveolar hemorrhage**.
- It is not indicated for confirming emphysema or alpha-1 antitrypsin deficiency, as these are diagnosed through clinical presentation, imaging, and serologic testing.
*Abdominal ultrasound*
- An **abdominal ultrasound** could evaluate for **liver disease** (cirrhosis, hepatomegaly) associated with alpha-1 antitrypsin deficiency.
- While it might reveal liver involvement, it does not confirm the pulmonary diagnosis or the underlying enzymatic deficiency itself.
- It would be considered as part of a comprehensive evaluation but is not the confirmatory test.
*Viral hepatitis serologies*
- These would test for **hepatitis A, B, C** infection, which are common causes of cirrhosis and elevated transaminases.
- However, the patient's respiratory symptoms, imaging findings of emphysema, young age, and family history point toward alpha-1 antitrypsin deficiency rather than viral hepatitis.
- While worth checking given the liver enzyme elevation, this would not confirm the primary diagnosis.
Non-alcoholic fatty liver disease US Medical PG Question 8: A 48-year-old man comes to the physician because of increasing generalized fatigue for 1 month. He has been unable to do normal household duties or go for his evening walks during this period. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. His father died of liver cancer at the age of 60 years. He does not smoke. He drinks one alcoholic beverage daily. Current medications include atorvastatin, enalapril, metformin, and insulin glargine. He is 170 cm (5 ft 7 in) tall and weighs 100 kg (220 lb); BMI is 34.6 kg/m2. His temperature is 36.6°C (97.9°F), pulse is 116/min, and blood pressure is 140/90 mm Hg. Examination shows hyperpigmented skin over the nape of the neck and extremities. The liver is palpated 4 cm below the right costal margin. Laboratory studies show:
Hemoglobin 10.6 g/dL
Mean corpuscular volume 87 μm3
Leukocyte count 9,700/mm3
Platelet count 182,000/mm3
Serum
Glucose 213 mg/dL
Creatinine 1.4 mg/dL
Albumin 4.1 g/dL
Total bilirubin 1.1 mg/dL
Alkaline phosphatase 66 U/L
AST 100 U/L
ALT 69 U/L
γ-glutamyl transferase 28 U/L (N=5–50)
Hepatitis B surface antigen negative
Hepatitis C antibody negative
Iron studies
Iron 261 μg/dL
Ferritin 558 ng/dL
Transferrin saturation 83%
Anti-nuclear antibody negative
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Abdominal ultrasonography
- B. CT of the abdomen
- C. Bone marrow biopsy
- D. Liver biopsy
- E. Genetic testing (Correct Answer)
Non-alcoholic fatty liver disease Explanation: ***Genetic testing***
- The patient's **elevated iron (261 μg/dL), ferritin (558 ng/dL), and transferrin saturation (83%)**, along with **hyperpigmented skin**, **hepatomegaly**, and a family history of liver cancer, are highly suggestive of **hereditary hemochromatosis**.
- **Genetic testing for HFE gene mutations (C282Y and H63D)** is the **current first-line confirmatory test** per AASLD guidelines when hereditary hemochromatosis is suspected with elevated iron studies.
- **C282Y homozygosity** accounts for ~85-90% of hereditary hemochromatosis cases in Caucasian populations.
*Abdominal ultrasonography*
- While ultrasound can show **hepatomegaly** and assess for liver masses (important given family history of liver cancer), it is **not specific for hemochromatosis**.
- It cannot differentiate hemochromatosis from other causes of liver enlargement or provide information about the underlying cause of iron overload.
*CT of the abdomen*
- CT can show increased liver density due to **iron deposition** in hemochromatosis, but this finding is **neither sensitive nor specific** enough for diagnosis.
- It involves radiation exposure and is less definitive than **genetic testing** for confirming hereditary hemochromatosis.
*Bone marrow biopsy*
- Bone marrow biopsy evaluates **hematologic disorders** and can assess reticuloendothelial iron stores, but this is **not the site of pathologic iron accumulation** in hemochromatosis.
- In hemochromatosis, iron accumulates in **parenchymal cells** (liver, pancreas, heart, pituitary), not primarily in bone marrow macrophages.
- This invasive procedure is not indicated for diagnosing hemochromatosis.
*Liver biopsy*
- Liver biopsy with **Prussian blue staining** and hepatic iron concentration measurement was historically the gold standard for diagnosis.
- Today, liver biopsy is **reserved for staging** (assessing degree of fibrosis/cirrhosis) or when **non-HFE hemochromatosis** is suspected after negative genetic testing.
- Given strong biochemical evidence and availability of non-invasive genetic testing, biopsy is not the initial confirmatory test.
Non-alcoholic fatty liver disease US Medical PG Question 9: A 45-year-old man presents for follow-up to monitor his chronic hepatitis C treatment. The patient was infected with hepatitis C genotype 1, one year ago. He has been managed on a combination of pegylated interferon-alpha and ribavirin, but a sustained viral response has not been achieved. Past medical history is significant for non-alcoholic fatty liver disease for the last 5 years. Which of the following, if added to the patient’s current treatment regimen, would most likely benefit this patient?
- A. Emtricitabine
- B. Entecavir
- C. Simeprevir (Correct Answer)
- D. Tenofovir
- E. Telbivudine
Non-alcoholic fatty liver disease Explanation: ***Simeprevir***
- Simeprevir is a **first-generation direct-acting antiviral (DAA)**, specifically a **protease inhibitor (NS3/4A inhibitor)**, highly effective against **HCV genotype 1**.
- Adding simeprevir to a regimen of **pegylated interferon-alpha and ribavirin** significantly increases the likelihood of achieving a **sustained virologic response** for patients who previously failed interferon-based therapy.
- **Note:** While this triple therapy approach was standard practice historically, current guidelines (as of 2024-2025) favor **interferon-free DAA combination regimens** (such as sofosbuvir/ledipasvir or glecaprevir/pibrentasvir) as first-line treatment for HCV genotype 1. However, among the options provided, simeprevir remains the only appropriate HCV-specific antiviral agent.
*Emtricitabine*
- This is a **nucleoside reverse transcriptase inhibitor (NRTI)** primarily used in the treatment of **HIV infection** and sometimes for hepatitis B.
- It has **no significant role** in the treatment of **hepatitis C viral infection**.
*Entecavir*
- Entecavir is an **antiviral agent** specifically used for the treatment of **chronic hepatitis B virus (HBV)** infection.
- It has **no established efficacy** against the **hepatitis C virus (HCV)**.
*Tenofovir*
- Tenofovir is a **nucleotide reverse transcriptase inhibitor** primarily used for treating **HIV infection** and **chronic hepatitis B virus (HBV)** infection.
- It is **not effective** against **hepatitis C virus (HCV)**.
*Telbivudine*
- Telbivudine is an **oral antiviral agent** indicated specifically for the treatment of **chronic hepatitis B virus (HBV)** infection.
- It does **not have antiviral activity** against the **hepatitis C virus (HCV)**.
Non-alcoholic fatty liver disease US Medical PG Question 10: A 38-year-old woman presents to her primary care physician for a new patient appointment. She states that she feels well and has no current complaints. The patient recently started seeing a specialist for treatment for another medical condition but otherwise has had no medical problems. The patient lives alone and drinks 2 alcoholic beverages every night. She has had 3 sexual partners in her lifetime, uses oral contraceptive pills for contraception, and has never been pregnant. Physical exam reveals a pleasant, obese woman with normal S1 and S2 on cardiac exam. Musculoskeletal exam reveals swelling of the MCP and PIP joints of the hands as well as ulnar deviation of the fingers. Laboratory tests are ordered and results are below:
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.2 mg/dL
AST: 95 U/L
ALT: 68 U/L
Which of the following best explains this patient's abnormal laboratory values?
- A. Viral infection
- B. Medication (Correct Answer)
- C. Obesity
- D. Bacterial infection
- E. Alcohol
Non-alcoholic fatty liver disease Explanation: ***Medication***
- The AST and ALT elevations, along with the patient's rheumatological findings (**MCP and PIP joint swelling**, **ulnar deviation**), strongly suggest **rheumatoid arthritis**.
- A common treatment for rheumatoid arthritis is **methotrexate**, which is known to cause **elevated liver enzymes (AST, ALT)**.
*Viral infection*
- While viral infections can cause elevated transaminases, this patient presents with classic signs of **rheumatoid arthritis** without other typical symptoms of acute viral illness.
- The chronic nature of joint changes (ulnar deviation) makes an acute viral etiology for the liver enzyme elevation less likely as the primary cause.
*Obesity*
- Obesity is a risk factor for **non-alcoholic fatty liver disease (NAFLD)**, which can cause elevated AST and ALT.
- However, NAFLD typically causes more modest elevations, often with **ALT > AST**, and obesity alone does not explain the rheumatological findings.
*Bacterial infection*
- Bacterial infections can cause systemic inflammation and potentially affect liver enzymes, but this patient shows no signs of acute infection (e.g., fever, leukocytosis) and presents with chronic joint issues.
- The pattern of joint involvement and liver enzyme elevation is not typical for a bacterial infection.
*Alcohol*
- Chronic alcohol consumption (2 drinks/night) can lead to **alcoholic liver disease** and elevated AST and ALT, typically with an **AST:ALT ratio of 2:1 or greater**.
- While the patient drinks alcohol, the liver enzyme elevations are relatively mild, and her presentation also includes rheumatological symptoms that are not explained by alcohol alone; the AST:ALT ratio here is less than 2:1.
More Non-alcoholic fatty liver disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.