Liver transplantation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Liver transplantation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Liver transplantation US Medical PG Question 1: A 40-year-old male with a history of chronic alcoholism recently received a liver transplant. Two weeks following the transplant, the patient presents with a skin rash and frequent episodes of bloody diarrhea. A colonoscopy is performed and biopsy reveals apoptosis of colonic epithelial cells. What is most likely mediating these symptoms?
- A. Donor T-cells (Correct Answer)
- B. Recipient T-cells
- C. Recipient B-cells
- D. Recipient antibodies
- E. Donor B-cells
Liver transplantation Explanation: ***Donor T-cells***
- This clinical presentation of **skin rash**, **bloody diarrhea**, and **colonic epithelial apoptosis** following an allogeneic transplant (like a liver transplant) is classic for **Graft-versus-Host Disease (GVHD)**.
- In GVHD, **immunocompetent T-cells from the donor** recognize the recipient's tissues as foreign and mount an immune attack, causing damage to organs like the skin, gastrointestinal tract, and liver.
*Recipient T-cells*
- **Recipient T-cells** are typically immunosuppressed following an organ transplant to prevent organ rejection.
- Furthermore, if activated, recipient T-cells would target the donor organ (the liver in this case), leading to **rejection**, rather than the systemic symptoms observed (skin rash, bloody diarrhea) which suggest an attack by donor cells on recipient tissues.
*Recipient B-cells*
- While recipient B-cells can be involved in **antibody-mediated rejection** of the transplanted organ, they are not the primary mediators of **cellular GVHD**.
- **Antibody-mediated rejection** would typically involve antibodies targeting the donor liver, leading to liver dysfunction, not the widespread GVHD symptoms described.
*Recipient antibodies*
- **Recipient antibodies** are primarily involved in **antibody-mediated rejection** of the transplanted organ, which would manifest as dysfunction of the transplanted liver.
- They do not mediate the symptoms of **Graft-versus-Host Disease (GVHD)**, which is a cell-mediated immune response.
*Donor B-cells*
- **Donor B-cells** are generally not the primary mediators of GVHD.
- While donor immune cells are crucial for GVHD, the major players are **donor T-cells**, which directly recognize and attack host tissues.
Liver transplantation US Medical PG Question 2: A 50-year-old man presents to a clinic with oliguria. Four weeks ago, he had a kidney transplant. Postoperative follow-up was normal. He is currently on cyclosporine and admits that sometimes he forgets to take his medication. On physical examination, the vital signs include: temperature 37.1°C (98.8°F), blood pressure 165/110 mm Hg, heart rate 80/min, and respiratory rate 16/min. There is mild tenderness on renal palpation. His serum creatinine level is 4 mg/dL, well above his baseline level after the transplant. Which of the following best describes the histological finding if a biopsy is taken from the transplanted kidney?
- A. Lymphocytic infiltration of graft vessels and endothelial damage (Correct Answer)
- B. Thrombosis and occlusion of vessels
- C. Atherosclerosis on angiography
- D. Necrosis with granulation tissue
- E. Thickening of blood vessels, fibrosis of graft vessels, and parenchymal atrophy
Liver transplantation Explanation: ***Lymphocytic infiltration of graft vessels and endothelial damage***
- The patient's presentation with **oliguria**, elevated **creatinine**, and **hypertension** following a recent kidney transplant, especially with a history of non-adherence to **cyclosporine** (an immunosuppressant), strongly indicates **acute rejection**.
- Histologically, acute rejection is characterized by **lymphocytic infiltration** of the graft vessels (often referred to as **vasculitis** or **endotheliitis**) and associated **endothelial damage**.
*Thrombosis and occlusion of vessels*
- This finding is more characteristic of **hyperacute rejection**, which typically occurs within minutes to hours of transplantation, not weeks later.
- Hyperacute rejection is mediated by **pre-formed antibodies** and leads to severe, rapid graft failure due to widespread intravascular thrombosis.
*Atherosclerosis on angiography*
- While post-transplant patients can develop accelerated atherosclerosis (a form of **chronic rejection**), it is typically a long-term complication developing months to years after transplantation.
- The acute presentation with rapid creatinine elevation is not typical for primary atherosclerosis.
*Necrosis with granulation tissue*
- **Necrosis** with **granulation tissue** is a general healing response to significant tissue injury or inflammation.
- While some cellular necrosis can occur in severe rejection, it's not the defining feature, and granulation tissue indicates a more prolonged, subacute process rather than the primary histological hallmark of acute rejection.
*Thickening of blood vessels, fibrosis of graft vessels, and parenchymal atrophy*
- These are classic features of **chronic rejection**, which manifests months to years after transplantation as a gradual decline in graft function.
- **Chronic rejection** involves progressive damage leading to vasculopathy, interstitial fibrosis, and tubular atrophy, rather than the acute inflammatory cellular infiltrate seen here.
Liver transplantation US Medical PG Question 3: A 61-year-old-male underwent deceased donor liver transplantation 3 weeks ago. During his follow up visit he complains of nausea and abdominal pain. He has been taking all of his medications as prescribed. He has a history of alcohol abuse and his last drink was one year ago. He does not smoke cigarettes and lives at home with his wife. On physical examination temperature is 98.6°F (37°C), blood pressure is 115/80 mmHg, pulse is 90/min, respirations are 18/min, and pulse oximetry is 99% on room air. He has scleral icterus and a positive fluid wave. Liver function tests are as follows:
Alkaline phosphatase: 110 U/L
Aspartate aminotransferase (AST, GOT): 100 U/L
Alanine aminotransferase (ALT, GPT): 120 U/L
Bilirubin total: 2.2 mg/dL
Liver biopsy shows mixed dense interstitial lymphocytic infiltrates in the portal triad. What is the mechanism of this reaction?
- A. Grafted T lymphocytes reacting against host
- B. CD4+ T lymphocytes reacting against recipient APCs
- C. CD8+ T lymphocytes reacting against donor MHCs (Correct Answer)
- D. Acute viral infection
- E. Pre-existing recipient antibodies
Liver transplantation Explanation: ***CD8+ T lymphocytes reacting against donor MHCs***
- This scenario describes **acute cellular rejection** following liver transplantation, mediated primarily by **recipient CD8+ T lymphocytes** recognizing donor major histocompatibility complex (MHC) class I molecules on donor hepatocytes.
- The **lymphocytic infiltrates** in the portal triad are characteristic of acute rejection, where activated cytotoxic T cells attack the transplanted organ.
*Grafted T lymphocytes reacting against host*
- This mechanism describes **graft-versus-host disease (GVHD)**, which is much more common after hematopoietic stem cell transplantation.
- While liver allografts contain donor lymphocytes, **GVHD from liver transplant is rare** and typically only seen in highly immunosuppressed patients or specific transplant settings.
*CD4+ T lymphocytes reacting against recipient APCs*
- This describes a reaction of donor CD4+ T cells against recipient antigen-presenting cells (APCs), which is part of the mechanism for **graft-versus-host disease (GVHD)**.
- The primary pathology in this patient, with liver damage and lymphocytic infiltration of the portal triad, points to a rejection of the transplanted liver, not GVHD.
*Acute viral infection*
- While possible in transplant recipients, an acute viral infection would typically present with different patterns of liver injury and biopsy findings, such as **viral cytopathic effects** or more widespread inflammation distinct from the dense portal triad infiltrates typical of rejection.
- The clinical presentation and biopsy findings are classic for organ rejection rather than a viral infection.
*Pre-existing recipient antibodies*
- **Pre-existing recipient antibodies** are primarily responsible for **hyperacute rejection**, which occurs minutes to hours after transplant and leads to rapid graft failure.
- This patient is presenting 3 weeks post-transplant, which is too late for hyperacute rejection; this mechanism generally leads to thrombosis and necrosis, not the interstitial lymphocytic infiltrates seen here.
Liver transplantation US Medical PG Question 4: A 28-year-old woman comes to the physician for a follow-up examination. Two months ago, she underwent left renal transplantation for recurrent glomerulonephritis. At the time of discharge, her creatinine was 0.9 mg/dL. She feels well. Current medications include tacrolimus and azathioprine. Her pulse is 85/min and blood pressure is 135/75 mmHg. Physical examination shows a well-healed surgical scar on her left lower abdomen. The remainder of the examination shows no abnormalities. The patient should be monitored for which of the following adverse effects of her medications?
- A. Gingival hyperplasia
- B. Kidney injury (Correct Answer)
- C. Polycythemia
- D. Hepatic necrosis
- E. Bone marrow suppression
Liver transplantation Explanation: ***Kidney injury***
- **Tacrolimus** is a potent calcineurin inhibitor that can cause **nephrotoxicity** (kidney injury) by inducing afferent arteriolar vasoconstriction and direct tubular toxicity.
- Close monitoring of **creatinine** and **tacrolimus trough levels** is essential to prevent and detect this adverse effect, especially in renal transplant patients where baseline function must be preserved.
- This is the **most critical monitoring parameter** for tacrolimus therapy.
*Gingival hyperplasia*
- This adverse effect is more commonly associated with **cyclosporine**, another calcineurin inhibitor, rather than tacrolimus.
- While both are immunosuppressants used in transplant, tacrolimus has a lower incidence of this cosmetic side effect.
*Polycythemia*
- Polycythemia is not a typical adverse effect of **tacrolimus** or **azathioprine**.
- Renal transplant patients may sometimes experience erythrocytosis due to increased erythropoietin production from the native kidneys or the transplanted kidney, but it's not directly related to these immunosuppressive medications.
*Hepatic necrosis*
- While **azathioprine** can cause **hepatotoxicity**, it typically manifests as cholestatic injury or dose-dependent hepatitis, rather than acute hepatic necrosis.
- Tacrolimus is not primarily associated with hepatic necrosis.
*Bone marrow suppression*
- **Azathioprine** is an antimetabolite that can cause **myelosuppression** (leukopenia, thrombocytopenia, anemia) by interfering with DNA synthesis.
- While this requires regular **CBC monitoring**, in this clinical scenario, **nephrotoxicity from tacrolimus** is the more immediate concern given the recent renal transplant and the need to preserve graft function.
- The question emphasizes creatinine monitoring (baseline 0.9 mg/dL mentioned), directing focus toward tacrolimus nephrotoxicity as the primary monitoring concern.
Liver transplantation US Medical PG Question 5: A 57-year-old man presents to the emergency department with fatigue. He states that his symptoms started yesterday and have been worsening steadily. The patient endorses a recent weight loss of 7 pounds this past week and states that he feels diffusely itchy. The patient has a past medical history of alcohol abuse, obesity, asthma, and IV drug use. His current medications include metformin, atorvastatin, albuterol, and fluticasone. In addition, the patient admits to smoking and drinking more than usual lately due to the stress he has experienced. His temperature is 98.7°F (37.1°C), blood pressure is 130/75 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam is notable for an ill-appearing man. The patient's skin appears yellow. Abdominal exam is notable for right upper quadrant tenderness. Cardiac and pulmonary exams are within normal limits. Laboratory values are ordered as seen below:
Hemoglobin: 14 g/dL
Hematocrit: 42%
Leukocyte count: 5,500 cells/mm^3 with normal differential
Platelet count: 70,000/mm^3
Partial thromboplastin time: 92 seconds
Prothrombin time: 42 seconds
AST: 1110 U/L
ALT: 990 U/L
Which of the following is most likely to be found in this patient's history?
- A. Recent antibiotic treatment with gentamicin
- B. Appropriate acute management of a deep vein thrombosis
- C. Decreased UDP-glucuronosyltransferase activity at birth
- D. Prosthetic valve with appropriate post-operative care
- E. Severe migraine headaches treated with acetaminophen (Correct Answer)
Liver transplantation Explanation: ***Severe migraine headaches treated with acetaminophen***
- The patient's presentation with **acute liver failure** (elevated AST/ALT, coagulopathy, jaundice) in the context of increased stress and likely increased medication use, strongly suggests **acetaminophen overdose** as the cause. Given his past medical history of alcohol abuse further increases his risk of liver injury with acetaminophen.
- While other etiologies such as acute viral hepatitis or ischemic hepatitis should be considered, acetaminophen overdose is the most common cause of acute liver failure.
*Recent antibiotic treatment with gentamicin*
- **Gentamicin** is an **aminoglycoside antibiotic** primarily associated with **nephrotoxicity** and **ototoxicity**, not acute liver failure.
- Liver dysfunction is not a typical adverse effect of gentamicin, making it an unlikely cause of the patient's symptoms.
*Appropriate acute management of a deep vein thrombosis*
- Treatment for deep vein thrombosis typically involves **anticoagulants** such as heparin or warfarin. While these medications can rarely cause liver injury, the severe and acute elevation in liver enzymes and coagulopathy seen here points away from a standard anticoagulant side effect.
- The clinical picture aligns much more closely with a direct hepatotoxic injury rather than an idiosyncratic reaction to anticoagulation.
*Decreased UDP-glucuronosyltransferase activity at birth*
- **Decreased UDP-glucuronosyltransferase (UGT) activity** at birth is characteristic of **Crigler-Najjar syndrome** or **Gilbert's syndrome**, which cause **unconjugated hyperbilirubinemia**.
- These are typically chronic conditions that present earlier in life and do not cause acute, severe hepatocellular injury with massively elevated AST/ALT and coagulopathy.
*Prosthetic valve with appropriate post-operative care*
- A prosthetic heart valve, even with appropriate post-operative care, is not directly linked to acute liver failure.
- While complications like endocarditis or hemolysis could cause some liver involvement, they would not typically present with this constellation of severe acute symptoms and laboratory findings.
Liver transplantation US Medical PG Question 6: A 47-year-old woman presents to the physician with complaints of fatigue accompanied by symmetric pain, swelling, and stiffness in her wrists, fingers, knees, and other joints. She describes the stiffness as being particularly severe upon awakening, but gradually improves as she moves throughout her day. Her physician initially suggests that she take NSAIDs. However, after a few months of minimal symptomatic improvement, she is prescribed an immunosuppressive drug that has a mechanism of preventing IL-2 transcription. What is the main toxicity that the patient must be aware of with this particular class of drugs?
- A. Pancytopenia
- B. Osteoporosis
- C. Hepatotoxicity
- D. Nephrotoxicity (Correct Answer)
- E. Hyperglycemia
Liver transplantation Explanation: ***Nephrotoxicity***
- The drug described, which prevents **IL-2 transcription**, is likely a **calcineurin inhibitor** like cyclosporine or tacrolimus, often used in autoimmune diseases.
- **Nephrotoxicity** (kidney damage) is a major dose-limiting toxicity of calcineurin inhibitors, causing both acute and chronic kidney injury.
*Pancytopenia*
- While some immunosuppressants can cause **pancytopenia** (e.g., azathioprine, methotrexate), it is not the classic or primary toxicity associated with calcineurin inhibitors.
- Calcineurin inhibitors primarily affect **renal function** and can cause other side effects like hypertension or neurotoxicity.
*Osteoporosis*
- **Osteoporosis** is a known side effect of long-term glucocorticoid use, but not typically a primary toxicity of calcineurin inhibitors.
- Glucocorticoids reduce bone formation and increase bone resorption, leading to bone density loss.
*Hepatotoxicity*
- **Hepatotoxicity** (liver damage) can occur with various immunosuppressants, such as methotrexate, but it is not the most prominent or defining toxicity for calcineurin inhibitors.
- While cyclosporine can cause some liver enzyme elevation, **nephrotoxicity** is far more common and severe.
*Hyperglycemia*
- **Hyperglycemia** can be a side effect of some immunosuppressants, particularly **glucocorticoids** and **tacrolimus** (another calcineurin inhibitor).
- However, for the class of drugs that prevent IL-2 transcription (calcineurin inhibitors), **nephrotoxicity** remains the most significant and common major toxicity to be aware of.
Liver transplantation US Medical PG Question 7: A 14-year-old boy has undergone kidney transplantation due to stage V chronic kidney disease. A pre-transplantation serologic assessment showed that he is negative for past or present HIV infection, viral hepatitis, EBV, and CMV infection. He has a known allergy for macrolides. The patient has no complaints 1 day after transplantation. His vital signs include: blood pressure 120/70 mm Hg, heart rate 89/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical examination, the patient appears to be pale, his lungs are clear on auscultation, heart sounds are normal, and his abdomen is non-tender on palpation. His creatinine is 0.65 mg/dL (57.5 µmol/L), GFR is 71.3 mL/min/1.73 m2, and urine output is 0.9 mL/kg/h. Which of the following drugs should be used in the immunosuppressive regimen in this patient?
- A. Belatacept
- B. Sirolimus
- C. Omalizumab
- D. Daclizumab
- E. Basiliximab (Correct Answer)
Liver transplantation Explanation: **Basiliximab**
- **Basiliximab** is a **monoclonal antibody** that targets the **IL-2 receptor (CD25)** on activated T cells, preventing their proliferation and inducing immunosuppression.
- It is commonly used as **induction therapy** in kidney transplant recipients due to its good safety profile, especially in pediatric patients, without the nephrotoxicity associated with calcineurin inhibitors, minimizing acute rejection risks immediately post-transplant.
*Belatacept*
- **Belatacept** works by co-stimulation blockade, binding to **CD80 and CD86** on antigen-presenting cells to prevent T-cell activation.
- It is typically reserved for patients who cannot tolerate calcineurin inhibitors due to **nephrotoxicity** or require a steroid-sparing regimen, which is not indicated as an immediate need in this patient.
*Sirolimus*
- **Sirolimus** is an **mTOR inhibitor** that works by blocking T-cell proliferation and B-cell differentiation.
- It is associated with several side effects, including **delayed wound healing**, **thrombocytopenia**, and **hyperlipidemia**, which are undesirable in the immediate post-transplant period, especially in a growing adolescent.
*Omalizumab*
- **Omalizumab** is an **anti-IgE monoclonal antibody** primarily used for allergic asthma and chronic spontaneous urticaria.
- It has no role in **immunosuppression for organ transplantation** as its mechanism of action is unrelated to preventing graft rejection.
*Daclizumab*
- **Daclizumab** is another **monoclonal antibody** that also targets the **IL-2 receptor (CD25)**, similar to basiliximab.
- However, daclizumab has been **withdrawn from the market** due to serious adverse effects including severe liver injury and autoimmune encephalitis, making it unavailable for clinical use in transplantation.
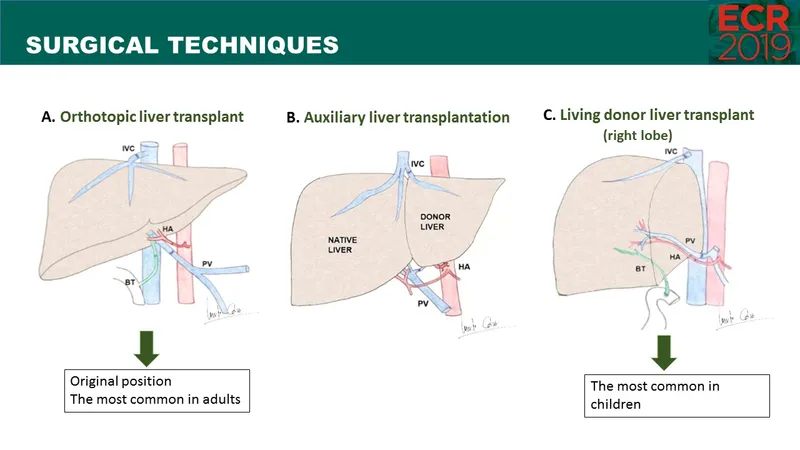
Liver transplantation US Medical PG Question 8: A 45-year-old man is brought to the emergency department because of a 1-day history of malaise and abdominal pain. Six weeks ago, he had vomiting and watery diarrhea for 2 days that resolved without treatment. Twelve weeks ago, he underwent orthotopic liver transplantation for alcoholic cirrhosis. At the time of discharge, his total serum bilirubin concentration was 1.0 mg/dL. He stopped drinking alcohol one year ago. His current medications include daily tacrolimus, prednisone, valganciclovir, and trimethoprim-sulfamethoxazole. His temperature is 37.7°C (99.9°F), pulse is 95/min, and blood pressure is 150/80 mm Hg. He appears uncomfortable and has mild jaundice. Examination shows scleral icterus. The abdomen is soft and tender to deep palpation over the right upper quadrant, where there is a well-healed surgical scar. His leukocyte count is 2500/mm3, serum bilirubin concentration is 2.6 mg/dL, and serum tacrolimus concentration is within therapeutic range. Which of the following is the next appropriate step in diagnosis?
- A. Ultrasound of the liver (Correct Answer)
- B. Viral loads
- C. CT scan of the abdomen with contrast
- D. Liver biopsy
- E. Esophagogastroduodenoscopy
Liver transplantation Explanation: ***Ultrasound of the liver***
Given the patient's recent liver transplant (12 weeks ago), presenting with abdominal pain, jaundice, and elevated bilirubin, an ultrasound is the **initial diagnostic step** to assess for post-transplant complications. The most critical early complications include **hepatic artery thrombosis** (can occur within the first 3 months), **biliary complications** (strictures, obstruction, bile leak), and vascular issues. Ultrasound with Doppler is **non-invasive, readily available, and cost-effective**, providing crucial information about hepatic vasculature, bile ducts, liver parenchyma, and fluid collections. This should be the first-line imaging modality in any post-transplant patient with new onset jaundice and RUQ pain.
*Viral loads*
While viral infections (particularly CMV, EBV, hepatitis viruses) are common in immunosuppressed transplant patients, the acute presentation with jaundice and RUQ pain makes a structural/vascular complication more immediately likely. The patient is on valganciclovir (CMV prophylaxis), and the prior GI illness 6 weeks ago could have been viral, but this doesn't explain the current acute hepatic dysfunction. Viral loads would be appropriate if imaging is unrevealing or if there are specific clinical features suggesting viral hepatitis, but it's not the **first diagnostic step** for acute post-transplant jaundice with abdominal pain.
*CT scan of the abdomen with contrast*
CT with contrast provides more detailed anatomical information and better characterizes complex intra-abdominal pathology, but it is typically **reserved for when ultrasound is inconclusive** or inadequate. CT involves ionizing radiation exposure and contrast-related risks (nephrotoxicity, particularly important in transplant patients who may have renal dysfunction from calcineurin inhibitors like tacrolimus). Ultrasound should be attempted first as it can answer the critical initial questions about vascular patency and biliary dilation without these risks.
*Liver biopsy*
Liver biopsy is an invasive procedure with risks (bleeding, infection, bile leak) and is generally performed **after non-invasive imaging** to diagnose conditions such as acute/chronic rejection, recurrent disease, or drug-induced liver injury. Since mechanical complications (vascular thrombosis, biliary obstruction) are potentially reversible emergencies that require urgent intervention, imaging must precede biopsy to rule out these structural causes. The therapeutic tacrolimus level makes acute drug toxicity less likely as an immediate cause.
*Esophagogastroduodenoscopy*
EGD evaluates the upper GI tract for bleeding, varices, ulcers, or mucosal lesions. While post-transplant patients can develop portal hypertensive gastropathy or medication-related gastropathy, the dominant features here are **jaundice and elevated bilirubin**, indicating a hepatobiliary rather than luminal GI problem. There's no mention of hematemesis, melena, or significant anemia that would prioritize upper GI evaluation. The RUQ pain and hyperbilirubinemia point toward hepatic/biliary pathology requiring hepatobiliary imaging first.
Liver transplantation US Medical PG Question 9: A 54-year-old man with known end-stage liver disease from alcoholic cirrhosis presents to the emergency department with decreased urinary output and swelling in his lower extremities. His disease has been complicated by ascites and hepatic encephalopathy in the past. Initial laboratory studies show a creatinine of 1.73 mg/dL up from a previous value of 1.12 one month prior. There have been no new medication changes, and no recent procedures performed. A diagnostic paracentesis is performed that is negative for infection, and he is admitted to the hospital for further management and initiated on albumin. Two days later, his creatinine has risen to 2.34 and he is oliguric. Which of the following is the most definitive treatment for this patient's condition?
- A. Liver transplantation (Correct Answer)
- B. Transjugular intrahepatic portosystemic shunt (TIPS)
- C. Peritoneovenous shunt
- D. Hemodialysis
- E. Cessation of alcohol use
Liver transplantation Explanation: ***Liver transplantation***
- This patient is presenting with **hepatorenal syndrome (HRS)** as indicated by the worsening renal function, presence of cirrhosis, ascites, and lack of response to albumin. **Liver transplantation** is the only definitive treatment as it addresses the underlying liver dysfunction causing HRS.
- While other treatments like vasoconstrictors and albumin can temporarily stabilize the patient, they do not cure the underlying pathophysiology.
*Transjugular intrahepatic portosystemic shunt (TIPS)*
- TIPS can be used to reduce **portal hypertension** and treat complications like refractory ascites or variceal bleeding.
- However, TIPS is generally **contraindicated in HRS** with severe renal impairment due to the risk of worsening liver function and encephalopathy.
*Peritoneovenous shunt*
- A peritoneovenous shunt is a rarely used procedure to drain **ascites** from the peritoneal cavity into the venous system.
- It does not address the underlying **renal dysfunction** or liver failure and carries a high risk of complications like infection and coagulation abnormalities.
*Hemodialysis*
- Hemodialysis can be used as a **bridge therapy** to manage acute renal failure in HRS, but it is not a definitive treatment.
- It provides renal support but does not correct the **hemodynamic derangements** or underlying liver disease.
*Cessation of alcohol use*
- While essential for slowing the progression of liver disease, **cessation of alcohol** can improve liver function in some cases.
- In a patient with end-stage cirrhosis and acute-on-chronic renal failure (HRS), it is **not an immediate or definitive treatment** for the acute crisis.
Liver transplantation US Medical PG Question 10: A 37-year-old man who had undergone liver transplantation 7 years ago, presents to the physician because of yellowish discoloration of the skin, sclera, and urine. He is on regular immunosuppressive therapy and is well-adherent to the treatment. He has no comorbidities and is not taking any other medication. He provides a history of similar episodes of yellowish skin discoloration 6–7 times since he underwent liver transplantation. Physical examination shows clinical jaundice. Laboratory studies show:
While blood cell (WBC) count 4,400/mm3
Hemoglobin 11.1 g/dL
Serum creatinine 0.9 mg/dL
Serum bilirubin (total) 44 mg/dL
Aspartate transaminase (AST) 1,111 U/L
Alanine transaminase (ALT) 671 U/L
Serum gamma-glutamyl transpeptidase 777 U/L
Alkaline phosphatase 888 U/L
Prothrombin time 17 seconds
A Doppler ultrasound shows significantly reduced blood flow into the transplanted liver. A biopsy of the transplanted liver is likely to show which of the following histological features?
- A. Ballooning degeneration of hepatocytes
- B. Normal architecture of bile ducts and hepatocytes
- C. Irregularly shaped nodules of regenerating hepatocytes with peripheral halo
- D. Broad fibrous septations with formation of micronodules
- E. Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis (Correct Answer)
Liver transplantation Explanation: ***Interstitial cellular infiltration with parenchymal fibrosis, obliterative arteritis***
- The patient's history of **repeated jaundice episodes** after liver transplantation, coupled with **elevated liver enzymes** and **significantly reduced transplanted liver blood flow** on Doppler, points to **chronic rejection**.
- **Chronic rejection** is histologically characterized by **interstitial cellular infiltration**, **parenchymal fibrosis**, and hallmark **obliterative arteritis**, which describes the progressive luminal narrowing and obliteration of hepatic arteries due to intimal proliferation.
*Ballooning degeneration of hepatocytes*
- This feature is typically associated with **acute hepatitis**, often viral or alcoholic, and indicates **hepatocyte swelling and necrosis**.
- While reflecting liver injury, it doesn't specifically point to **chronic rejection** in a transplanted liver with repeated episodes and vascular changes.
*Normal architecture of bile ducts and hepatocytes*
- This finding would suggest a **healthy liver** or a successful response to treatment, which contradicts the patient's symptoms of **jaundice**, highly elevated **liver enzymes**, and **reduced blood flow**.
- The presence of clinical symptoms and abnormal lab values rules out a normal liver architecture.
*Irregularly shaped nodules of regenerating hepatocytes with peripheral halo*
- This description is characteristic of **biliary hamartomas** (von Meyenburg complexes) or focal nodular hyperplasia, which are typically benign lesions and not indicative of the **severe liver injury** seen here.
- It does not align with the progressive nature of the patient's recurrent jaundice and vascular compromise identified.
*Broad fibrous septations with formation of micronodules*
- This histological pattern is typical of **cirrhosis**, a condition characterized by diffuse **fibrosis** and the formation of **regenerative nodules**, often resulting from chronic liver diseases like hepatitis or alcohol abuse.
- While fibrosis is part of chronic rejection, the description does not capture the specific **vascular and inflammatory changes** of **obliterative arteritis** that are central to chronic rejection.
More Liver transplantation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.