Hepatocellular carcinoma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hepatocellular carcinoma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hepatocellular carcinoma US Medical PG Question 1: A 52-year-old man comes to the emergency department because of a 3-week history of abdominal distention, yellow coloring of the skin, and dark urine. He also reports malaise and progressive shortness of breath, associated with slight exertion, for several weeks. The patient is a chronic drinker, and he was diagnosed with cirrhosis 2 years ago. He was warned to stop drinking alcohol, but he continues to drink. He hasn't accepted any more testing and has refused to visit the doctor until now. His vital signs are heart rate 62/min, respiratory rate 26/min, temperature 37.4°C (99.3°F), and blood pressure 117/95 mm Hg. On physical examination, there is dyspnea and polypnea. Skin and sclera are jaundiced. The abdomen has visible collateral circulation and looks distended. There is diffuse abdominal pain upon palpation in the right hemiabdomen, and the liver is palpated 10 cm below the right costal border. The legs show significant edema. CT scan shows cirrhosis with portal hypertension and collateral circulation. During the fifth day of his hospital stay, the patient presents with oliguria and altered mental status. Laboratory studies show:
Day 1
Day 5
Hemoglobin
12.1 g/dL
11.2 g/dL
Hematocrit
33.3%
31.4%
Leukocyte count
7,000/mm3
6,880/mm3
Platelet count
220,000/mm3
134,000/mm3
Total bilirubin
20.4 mg/dL
28.0 mg/dL
Direct bilirubin
12.6 mg/dL
21.7 mg/dL
Creatinine
2.2 mg/dL
2.9 mg/dL
Albumin
3.4 g/dL
2.6 g/dL
PT
15 s
16.9 s
aPTT
19 s
35 s
Urinalysis
Negative for nitrite
Negative for leukocyte esterase
0–2 RBCs per high power field
0–1 WBC per high power field
No evidence of casts or proteinuria
What is the most likely cause of this patient's increased creatinine?
- A. Hepatorenal syndrome (Correct Answer)
- B. Chronic kidney disease
- C. Pyelonephritis
- D. Acute tubular necrosis
- E. Glomerulonephritis
Hepatocellular carcinoma Explanation: ***Hepatorenal syndrome***
- This patient with **decompensated cirrhosis** and **oliguria** exhibits a rapid increase in **creatinine** (2.2 to 2.9 mg/dL over 4 days) without evidence of intrinsic kidney disease (negative urinalysis with no casts, minimal proteinuria). This points toward **Hepatorenal Syndrome (HRS)**, a severe complication of advanced liver disease.
- The **bland urinalysis** is the key diagnostic feature of HRS, distinguishing it from acute tubular necrosis. HRS results from severe vasoconstriction of renal arteries in the setting of splanchnic vasodilation from portal hypertension.
- The development of **altered mental status** along with worsening renal function further supports HRS, as it reflects progressive hepatic decompensation and hepatic encephalopathy.
*Chronic kidney disease*
- While patients with cirrhosis can develop CKD, the **rapid onset** of renal failure and oliguria over just 4 days, coupled with normal urinalysis, is less typical for primary chronic kidney disease exacerbation.
- CKD usually presents with more gradual changes in creatinine and may show signs of kidney damage (like proteinuria or casts) on urinalysis, which are absent here.
*Pyelonephritis*
- **Pyelonephritis**, a kidney infection, would typically present with fever, flank pain, and significant abnormalities on urinalysis such as **leukocyte esterase**, **nitrites**, and **white blood cell casts**, none of which are present.
- The absence of infectious markers in the urine makes pyelonephritis an unlikely cause of the acute renal deterioration.
*Acute tubular necrosis*
- **Acute tubular necrosis (ATN)**, often caused by ischemia or nephrotoxins, would typically show signs of tubular damage on urinalysis, such as **muddy brown casts** and renal tubular epithelial cells.
- The urinalysis in this case is bland, with no evidence of casts or significant cellular debris, ruling out ATN as the primary diagnosis.
*Glomerulonephritis*
- **Glomerulonephritis** would typically present with **hematuria**, **proteinuria**, and potentially **red blood cell casts** on urinalysis, indicating glomerular inflammation.
- The patient's urinalysis is benign, showing no red blood cell casts or significant proteinuria, making glomerulonephritis an unlikely diagnosis.
Hepatocellular carcinoma US Medical PG Question 2: The patient undergoes a mammogram, which shows a 6.5mm sized mass with an irregular border and spiculated margins. A subsequent core needle biopsy of the mass shows infiltrating ductal carcinoma with HER2-positive, estrogen-negative, and progesterone-negative immunohistochemistry staining. Blood counts and liver function tests are normal. Laboratory studies show:
Hemoglobin 12.5 g/dL
Serum
Na+ 140 mEq/L
Cl- 103 mEq/L
K+ 4.2 mEq/L
HCO3- 26 mEq/L
Ca2+ 8.9 mg/dL
Urea Nitrogen 12 mg/dL
Glucose 110 mg/dL
Alkaline Phosphatase 25 U/L
Alanine aminotransferase (ALT) 15 U/L
Aspartate aminotransferase (AST) 13 U/L
Which of the following is the most appropriate next step in management?
- A. Breast-conserving therapy and sentinel lymph node biopsy (Correct Answer)
- B. Bilateral mastectomy with lymph node dissection
- C. Trastuzumab therapy
- D. Bone scan
- E. Whole-body PET/CT
Hepatocellular carcinoma Explanation: ***Breast-conserving therapy and sentinel lymph node biopsy***
- The patient has **early-stage (T1) breast cancer** (6.5mm mass), which is amenable to **breast-conserving therapy (lumpectomy)** as the primary surgical approach.
- A **sentinel lymph node biopsy** is essential to determine nodal status and guide further staging and adjuvant therapy, as the tumor size does not preclude nodal involvement.
*Bilateral mastectomy with lymph node dissection*
- This is an **overly aggressive surgical approach** for a small, unifocal tumor without evidence of multifocality or significant risk factors for recurrence in the contralateral breast.
- While **axillary lymph node dissection** may be indicated if the sentinel node is positive, it is not the initial preferred approach for all patients, especially with no current evidence of nodal metastasis.
*Trastuzumab therapy*
- **Trastuzumab** is a targeted therapy for **HER2-positive breast cancer**, but it is typically administered as **adjuvant therapy** (after surgery) or neoadjuvant therapy (before surgery).
- It is not the most appropriate *initial* next step before surgical management and comprehensive staging have been completed.
*Bone scan*
- A **bone scan** is used to detect **bone metastases**, but it is generally reserved for patients with **advanced-stage cancer** (e.g., T3/T4 tumor, N2/N3 nodes), symptoms suggestive of bony involvement, or significantly elevated alkaline phosphatase.
- Given the patient's small tumor size (6.5mm), normal labs, and lack of symptoms, a bone scan is not indicated as the *next* immediate step.
*Whole-body PET/CT*
- **Whole-body PET/CT** is primarily used for **staging advanced cancer** or investigating suspicious findings in symptomatic patients.
- For this small, early-stage breast cancer with no signs of distant metastasis indicated by normal blood tests, a PET/CT is **not recommended** as routine staging and carries unnecessary radiation exposure and cost.
Hepatocellular carcinoma US Medical PG Question 3: A 56-year-old African American presents to the emergency department due to abdominal pain, fatigue, and weight loss over the past 3 months. He has a long-standing history of chronic hepatitis B virus infection complicated by cirrhosis. On examination, he has jaundice, leg edema, and a palpable mass in the right upper abdominal quadrant. Abdominal ultrasound shows a 3-cm liver mass with poorly defined margins and coarse, irregular internal echoes. Blood investigations are shown:
Aspartate aminotransferase (AST) 90 U/L
Alanine aminotransferase (ALT) 50 U/L
Total bilirubin 2 mg/dL
Albumin 3 g/dL
Alkaline phosphatase 100 U/L
Alpha fetoprotein 600 micrograms/L
Which of the following targeted agents is approved for advanced-stage hepatoma?
- A. Ustekinumab
- B. Daclizumab
- C. Sorafenib (Correct Answer)
- D. Abciximab
- E. Palivizumab
Hepatocellular carcinoma Explanation: ***Sorafenib***
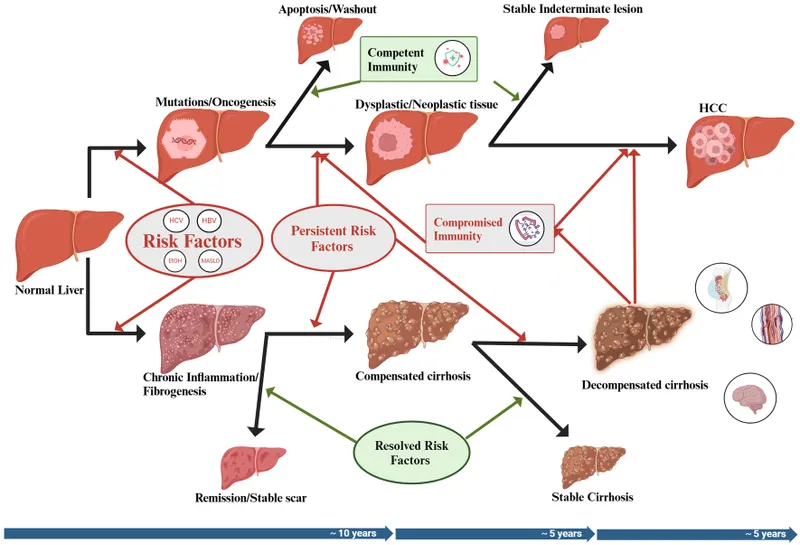
- This patient's presentation with chronic hepatitis B, cirrhosis, a liver mass, and an **elevated alpha-fetoprotein** is highly suggestive of **hepatocellular carcinoma (HCC)**, also known as hepatoma.
- **Sorafenib** is a **multi-targeted tyrosine kinase inhibitor** that inhibits tumor cell proliferation and angiogenesis by targeting VEGFR, PDGFR, Raf kinases, and other kinases involved in tumor progression.
- It was the **first systemic therapy approved for advanced-stage HCC** and remains an important first-line treatment option for patients with advanced disease who are not candidates for surgical or locoregional therapies.
*Ustekinumab*
- **Ustekinumab** is a monoclonal antibody that targets the **p40 subunit of IL-12 and IL-23**, primarily used in the treatment of **psoriasis** and psoriatic arthritis, not HCC.
- It works by blocking inflammatory pathways involved in autoimmune conditions.
*Daclizumab*
- **Daclizumab** is a humanized monoclonal antibody that targets the **CD25 subunit of the IL-2 receptor**; it was previously used for treating **multiple sclerosis** but has been largely discontinued due to safety concerns.
- It is not indicated for the treatment of any form of cancer.
*Abciximab*
- **Abciximab** is a monoclonal antibody that targets the **glycoprotein IIb/IIIa receptor** on platelets, used as an **antiplatelet agent** in patients undergoing percutaneous coronary intervention.
- Its mechanism of action is related to inhibition of platelet aggregation and thrombosis, not cancer therapy.
*Palivizumab*
- **Palivizumab** is a monoclonal antibody used for the **prevention of serious lower respiratory tract disease** caused by **respiratory syncytial virus (RSV)** in high-risk infants.
- It provides passive immunity against RSV and has no role in cancer treatment.
Hepatocellular carcinoma US Medical PG Question 4: A scientist is researching the long term effects of the hepatitis viruses on hepatic tissue. She finds that certain strains are oncogenic and increase the risk of hepatocellular carcinoma. However, they appear to do so via different mechanisms. Which of the following answer choices correctly pairs the hepatitis virus with the correct oncogenic process?
- A. Hepatitis A virus - chronic inflammation
- B. Hepatitis C virus - chronic inflammation
- C. Hepatitis E virus - integration of viral DNA into host hepatocyte genome
- D. Hepatitis B virus - integration of viral DNA into host hepatocyte genome (Correct Answer)
- E. Hepatitis A virus - integration of viral DNA into host hepatocyte genome
Hepatocellular carcinoma Explanation: ***Hepatitis B virus - integration of viral DNA into host hepatocyte genome***
- **Hepatitis B virus (HBV)** is a **DNA virus** that can integrate its genetic material into the host hepatocyte genome, leading to genomic instability and promoting oncogenesis.
- This integration, along with chronic inflammation and the production of viral regulatory proteins, contributes significantly to the development of **hepatocellular carcinoma (HCC)**.
*Hepatitis A virus - chronic inflammation*
- **Hepatitis A virus (HAV)** is an **RNA virus** that causes **acute hepatitis** but does not lead to chronic infection or chronic inflammation.
- Due to its acute and self-limiting nature, HAV is **not associated with hepatocellular carcinoma**.
*Hepatitis C virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis C virus (HCV)** is an **RNA virus** and therefore does not integrate its DNA into the host genome (as it has no DNA phase).
- HCV causes HCC primarily through **chronic inflammation**, **fibrosis**, and **cirrhosis**, not DNA integration.
*Hepatitis E virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis E virus (HEV)** is an **RNA virus** that typically causes acute, self-limiting hepatitis and does not integrate its genetic material into the host genome.
- While HEV can cause chronic infection in immunocompromised individuals, it is **not generally recognized as an oncogenic virus** leading to HCC.
*Hepatitis A virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis A virus (HAV)** is an **RNA virus**, meaning it does not have a DNA stage and therefore cannot integrate DNA into the host genome.
- HAV causes **acute, self-limiting infections** and is definitively **not associated with hepatocellular carcinoma**.
Hepatocellular carcinoma US Medical PG Question 5: A 56-year-old African American presents to the emergency department due to abdominal pain, fatigue, and weight loss over the past 3 months. He has a long-standing history of chronic hepatitis B virus infection complicated by cirrhosis. On examination, he has jaundice, leg edema, and a palpable mass in the right upper abdominal quadrant. Abdominal ultrasound shows a 3-cm liver mass with poorly defined margins and coarse, irregular internal echoes. Lab results are shown:
Aspartate aminotransferase (AST) 90 U/L
Alanine aminotransferase (ALT) 50 U/L
Total bilirubin 2 mg/dL
Albumin 3 g/dL
Alkaline phosphatase 100 U/L
Alpha-fetoprotein 600 ng/mL
Which of the following is a feature of this patient's condition?
- A. It arises from the bile duct epithelium
- B. Daughter cysts are usually present on abdominal ultrasound
- C. Liver biopsy is required for diagnosis in a majority of patients
- D. It arises from hepatocytes (Correct Answer)
- E. Doppler blood flow shows venous pattern
Hepatocellular carcinoma Explanation: ***It arises from hepatocytes***
- This patient's clinical presentation, including chronic **hepatitis B** with **cirrhosis**, an abdominal mass, and significantly elevated **alpha-fetoprotein (AFP)**, strongly indicates **hepatocellular carcinoma (HCC)**.
- HCC is a primary liver cancer that originates from the **hepatocytes**, the main functional cells of the liver.
*It arises from the bile duct epithelium*
- This describes **cholangiocarcinoma**, which arises from the **bile duct cells**.
- While cholangiocarcinoma is a primary liver cancer, its risk factors, imaging features, and tumor markers (e.g., **CA 19-9**) typically differ from those seen in this patient, and **AFP** elevation is not characteristic.
*Daughter cysts are usually present on abdominal ultrasound*
- **Daughter cysts** on ultrasound are characteristic of **hydatid cysts**, typically caused by **Echinococcus granulosus** infection.
- This parasitic condition presents differently, and the patient's elevated **AFP** and history of **cirrhosis** are not associated with hydatid disease.
*Liver biopsy is required for diagnosis in a majority of patients*
- In patients with **cirrhosis** and a lesion larger than 1 cm with characteristic imaging findings **(e.g., contrast enhancement on MRI/CT)**, along with a high **alpha-fetoprotein (AFP)** level, a biopsy is often **not required** for the diagnosis of HCC, as per standard guidelines.
- The combination of risk factors (cirrhosis, chronic HBV), elevated AFP, and imaging findings is sufficient for diagnosis in many cases, especially to avoid biopsy-related risks like bleeding or tumor seeding.
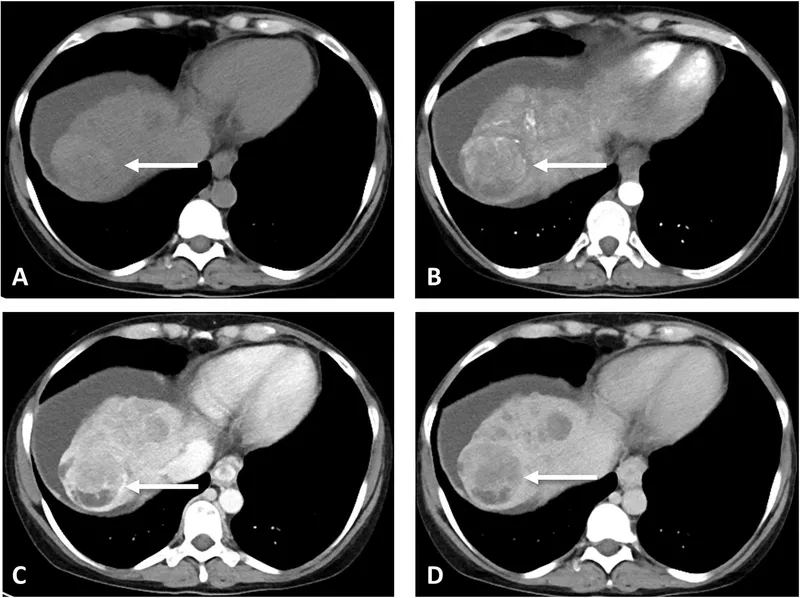
*Doppler blood flow shows venous pattern*
- **Hepatocellular carcinoma** typically exhibits a **hypervascular arterial enhancement pattern** on imaging with **early washout** in the venous phase.
- This is a key diagnostic feature, and flow showing a venous pattern would be inconsistent with HCC.
Hepatocellular carcinoma US Medical PG Question 6: A 27-year-old woman presents to the emergency department complaining of a left-sided headache and right-sided blurry vision. She states that 2 weeks ago she developed dark urine and abdominal pain. She thought it was a urinary tract infection so she took trimethoprim-sulfamethoxazole that she had left over. She planned on going to her primary care physician today but then she developed headache and blurry vision so she came to the emergency department. The patient states she is otherwise healthy. Her family history is significant for a brother with sickle cell trait. On physical examination, there is mild abdominal tenderness, and the liver edge is felt 4 cm below the right costal margin. Labs are drawn as below:
Hemoglobin: 7.0 g/dL
Platelets: 149,000/mm^3
Reticulocyte count: 5.4%
Lactate dehydrogenase: 3128 U/L
Total bilirubin: 2.1 mg/dL
Indirect bilirubin: 1.4 mg/dL
Aspartate aminotransferase: 78 U/L
Alanine aminotransferase: 64 U/L
A peripheral smear shows polychromasia. A Doppler ultrasound of the liver shows decreased flow in the right hepatic vein. Magnetic resonance imaging of the brain is pending. Which of the following tests, if performed, would most likely identify the patient’s diagnosis?
- A. Flow cytometry (Correct Answer)
- B. Glucose-6-phosphate-dehydrogenase levels
- C. Anti-histone antibodies
- D. Bone marrow biopsy
- E. Hemoglobin electrophoresis
Hepatocellular carcinoma Explanation: ***Flow cytometry***
- The patient's symptoms (headache, blurry vision, dark urine, abdominal pain, hepatomegaly) along with laboratory findings of **hemolytic anemia** (low hemoglobin, elevated reticulocyte count, high LDH, elevated indirect bilirubin) and signs of **thrombosis** (decreased hepatic vein flow, neurological symptoms) are highly suggestive of **paroxysmal nocturnal hemoglobinuria (PNH)**.
- **Flow cytometry** is the gold standard for diagnosing PNH by detecting the absence of **CD55** and **CD59** on red blood cells, granulocytes, and monocytes, indicating a deficiency in the **GPI anchor protein**.
*Glucose-6-phosphate-dehydrogenase levels*
- **G6PD deficiency** typically presents with hemolytic anemia triggered by **oxidant stressors** (like trimethoprim-sulfamethoxazole) but does not typically cause **thrombosis** or widespread organ involvement (e.g., hepatic vein thrombosis, neurological symptoms) as seen in this patient.
- Measuring G6PD levels would be appropriate if G6PD deficiency was suspected, but the clinical picture points more strongly to PNH due to the thrombotic events.
*Anti-histone antibodies*
- **Anti-histone antibodies** are primarily associated with drug-induced **lupus erythematosus**, which can manifest with various systemic symptoms, but not typically with severe hemolytic anemia and thrombotic microangiopathy in this specific pattern.
- While drug exposure is present (trimethoprim-sulfamethoxazole), the overall clinical and lab findings (especially the severe hemolytic picture and thrombosis) are not characteristic of drug-induced lupus in this context.
*Bone marrow biopsy*
- A **bone marrow biopsy** might show findings consistent with increased erythropoiesis due to hemolysis but is not a primary diagnostic test for PNH or its associated thrombotic complications.
- While it could be part of an evaluation for underlying bone marrow disorders, it would not directly confirm a diagnosis of PNH, which requires specific surface marker detection.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** such as **sickle cell disease** or **thalassemia**. The patient's brother has sickle cell trait, but the patient's symptoms, particularly the prominent hemolytic anemia and thrombotic events, are not typical of a hemoglobinopathy in this acute presentation.
- While it could rule out a hemoglobinopathy, it wouldn't explain the full spectrum of symptoms, especially the thrombosis and the specific pattern of hemolysis (e.g., elevated LDH, indirect bilirubin).
Hepatocellular carcinoma US Medical PG Question 7: A 52-year-old man presents to his physician after his routine screening revealed that he has elevated liver enzymes. He complains of occasional headaches during the past year, but otherwise feels well. The patient reports that he was involved in a serious car accident in the 1980s. He does not smoke or drink alcohol. He has no history of illicit intravenous drug use. He does not currently take any medications and has no known allergies. His father had a history of alcoholism and died of liver cancer. The patient appears thin. His temperature is 37.8°C (100°F), pulse is 100/min, and blood pressure is 110/70 mm Hg. The physical examination reveals no abnormalities. The laboratory test results show the following:
Complete blood count
Hemoglobin 14 g/dL
Leukocyte count 10,000/mm3
Platelet count 146,000/mm3
Comprehensive metabolic profile
Glucose 150 mg/dL
Albumin 3.2 g/dL
Total bilirubin 1.5 mg/dL
Alkaline phosphatase 75 IU/L
AST 95 IU/L
ALT 73 IU/L
Other lab tests
HIV negative
Hepatitis B surface antigen negative
Hepatitis C antibody positive
HCV RNA positive
HCV genotype 1
A liver biopsy is performed and shows mononuclear infiltrates localized to portal tracts that reveal periportal hepatocyte necrosis. Which of the following is the most appropriate next step in management?
- A. Peginterferon alpha therapy
- B. Interferon and ribavirin therapy
- C. Sofosbuvir and ledipasvir therapy (Correct Answer)
- D. Tenofovir and entecavir therapy
- E. Tenofovir and velpatasvir therapy
Hepatocellular carcinoma Explanation: ***Sofosbuvir and ledipasvir therapy***
- This patient has chronic **Hepatitis C (HCV) infection** (HCV antibody positive, HCV RNA positive). **Sofosbuvir/ledipasvir** is an effective **direct-acting antiviral (DAA)** regimen for **genotype 1 HCV**, which is indicated for treatment-naïve patients without cirrhosis.
- The liver biopsy findings of **mononuclear infiltrates** and **periportal necrosis** confirm active hepatitis and the need for antiviral treatment to prevent progression to cirrhosis.
*Peginterferon alpha therapy*
- **Peginterferon alpha** was historically used for HCV, but its use has largely been replaced by **DAAs** due to significant side effects and lower efficacy.
- This therapy is associated with numerous adverse effects, including **flu-like symptoms**, **depression**, and **bone marrow suppression**.
*Interferon and ribavirin therapy*
- This combination was a standard treatment for HCV before the advent of DAAs, but it is associated with a high burden of **side effects** like **hemolytic anemia** (from ribavirin) and **flu-like symptoms** (from interferon).
- Given the availability of highly effective and well-tolerated DAAs, this regimen is no longer considered first-line for chronic HCV.
*Tenofovir and entecavir therapy*
- **Tenofovir** and **entecavir** are antiviral medications primarily used for the treatment of **chronic Hepatitis B (HBV) infection**.
- This patient's **Hepatitis B surface antigen is negative**, ruling out chronic HBV infection as the primary issue requiring these specific drugs.
*Tenofovir and velpatasvir therapy*
- While **velpatasvir** is a DAA used for HCV, its combination with **tenofovir** is not a standard HCV treatment for genotype 1.
- **Tenofovir** is primarily an anti-HBV drug; for HCV, velpatasvir is typically combined with **sofosbuvir** (as in Epclusa) for pan-genotypic coverage.
Hepatocellular carcinoma US Medical PG Question 8: A 36-year-old female presents to the emergency department with right upper quadrant (RUQ) pain. She describes the pain as dull and getting progressively worse over the last several weeks. She denies any relationship to eating. Her past medical history is significant for endometriosis, which she manages with oral contraceptive pills, and follicular thyroid cancer, for which she underwent total thyroidectomy and now takes levothyroxine. The patient drinks a six pack of beer most nights of the week, and she has a 20 pack-year smoking history. She recently returned from visiting cousins in Mexico who have several dogs. Her temperature is 98.2°F (36.8°C), blood pressure is 132/87 mmHg, pulse is 76/min, and respirations are 14/min. On physical exam, her abdomen is soft and non-distended with tenderness in the right upper quadrant and palpable hepatomegaly. Laboratory testing is performed and reveals the following:
Aspartate aminotransferase (AST, GOT): 38 U/L
Alanine aminotransferase (ALT, GPT): 32 U/L
Alkaline phosphatase: 196 U/L
gamma-Glutamyltransferase (GGT): 107 U/L
Total bilirubin: 0.8 mg/dL
RUQ ultrasound demonstrates a solitary, well-demarcated, heterogeneous 6 cm mass in the right lobe of the liver. CT scan with contrast reveals peripheral enhancement during the early phase with centripetal flow during the portal venous phase. Which of the following is a risk factor for this condition?
- A. Recent contact with dogs
- B. Extrahepatic malignancy
- C. Chronic alcohol abuse
- D. Recent travel to Mexico
- E. Oral contraceptive pill use (Correct Answer)
Hepatocellular carcinoma Explanation: ***Oral contraceptive pill use***
- The patient's presentation with a solitary, well-demarcated hepatic mass showing **peripheral enhancement with centripetal filling** on CT scan is pathognomonic for a **hepatic hemangioma**.
- Hepatic hemangiomas are the most common benign liver tumors and are typically asymptomatic, though large lesions (>4 cm) can cause symptoms.
- While hemangiomas have no clearly established risk factors, they are more common in women and may have an association with **oral contraceptive pill (OCP) use**, though this relationship is less definitive than with hepatic adenomas.
- Some studies suggest OCPs may influence hemangioma growth, making this the most relevant risk factor among the options provided.
*Recent contact with dogs*
- Contact with dogs, especially in endemic areas, is a risk factor for **echinococcal cysts** (hydatid disease).
- Echinococcal cysts appear as multiloculated, cystic lesions with daughter cysts or calcifications on imaging, not as a solid mass with the described enhancement pattern.
*Extrahepatic malignancy*
- An extrahepatic malignancy could lead to **metastatic liver disease**, which typically presents as multiple lesions with different enhancement characteristics (e.g., rim enhancement or rapid washout).
- While the patient has a history of follicular thyroid cancer, the characteristic centripetal filling pattern is specific for hemangioma, not metastases.
*Chronic alcohol abuse*
- **Chronic alcohol abuse** is a major risk factor for alcoholic liver disease, cirrhosis, and **hepatocellular carcinoma (HCC)**.
- HCC typically shows arterial hyperenhancement with portal venous washout (not centripetal filling), and is usually associated with cirrhosis.
- The patient's imaging findings and clinical presentation are not consistent with HCC.
*Recent travel to Mexico*
- Travel to Mexico with potential exposure to contaminated food or water could be a risk factor for **parasitic infections** or **amebic liver abscess**.
- However, the imaging findings of a well-demarcated solid mass with classic hemangioma enhancement pattern are inconsistent with infectious or abscess formations, which would show rim enhancement and internal heterogeneity.
Hepatocellular carcinoma US Medical PG Question 9: A 48-year-old homeless male presents to the ED because he hasn’t felt well recently. He states that he has been feeling nauseous and extremely weak over the past few days. He has several previous admissions for alcohol intoxication and uses heroin occasionally. His temperature is 100.9°F (38.3°C), blood pressure is 127/89 mmHg, and pulse is 101/min. His physical examination is notable for palmar erythema, tender hepatomegaly, and gynecomastia. His laboratory findings are notable for:
AST: 170 U/L
ALT: 60 U/L
GGT: 400 (normal range: 0-45 U/L)
Alkaline phosphatase: 150 IU/L
Direct bilirubin: 0.2 mg/dL
Total bilirubin: 0.8 mg/dL
WBC: 10,500
Serum iron: 100 µg/dL
TIBC: 300 µg/dL (normal range: 250–370 µg/dL)
Serum acetaminophen screen: Negative
Serum AFP: 6 ng/mL (normal range: < 10ng/mL)
Which of the following is the most likely cause of this patient’s symptoms?
- A. Acute viral hepatitis
- B. Acute cholangitis
- C. Hereditary hemochromatosis
- D. Hepatocellular carcinoma
- E. Alcoholic hepatitis (Correct Answer)
Hepatocellular carcinoma Explanation: ***Alcoholic hepatitis***
- The patient's history of **heavy alcohol use**, along with symptoms such as **nausea**, **weakness**, **palmar erythema**, **tender hepatomegaly**, and **gynecomastia**, strongly points to alcoholic hepatitis.
- Laboratory findings of **AST:ALT ratio > 2:1** (170:60), **elevated GGT** (400 U/L), and **mildly elevated WBC** are characteristic of alcoholic liver injury.
*Acute viral hepatitis*
- While acute viral hepatitis can cause similar symptoms and elevated transaminases, the **AST:ALT ratio being significantly greater than 1** (specifically >2) is highly suggestive of alcoholic liver disease, whereas viral hepatitis typically shows ALT > AST.
- The elevated GGT is also more indicative of chronic alcohol use rather than acute viral infection.
*Acute cholangitis*
- Acute cholangitis typically presents with **Charcot's triad** (fever, right upper quadrant pain, jaundice) or **Reynolds' pentad** (Charcot's triad plus altered mental status and hypotension), along with **elevated alkaline phosphatase** and **direct bilirubin**.
- This patient's symptoms do not align with a classic presentation of cholangitis, and his direct bilirubin is normal.
*Hereditary hemochromatosis*
- Hereditary hemochromatosis is characterized by **iron overload**, which would manifest as **elevated serum iron** and **transferrin saturation**, along with a **decreased TIBC**.
- This patient's serum iron is normal, and his TIBC is within the normal range, ruling out iron overload as the primary cause.
*Hepatocellular carcinoma*
- HCC is a form of **liver cancer** that often develops in the setting of chronic liver disease (e.g., cirrhosis). While his history of alcohol use puts him at risk for cirrhosis, his **alpha-fetoprotein (AFP)** level is normal.
- The acute presentation with elevated transaminases and inflammatory markers is more consistent with acute hepatitis rather than carcinoma, which typically presents insidiously.
Hepatocellular carcinoma US Medical PG Question 10: A 44-year-old man comes to the physician for a routine health maintenance examination. He had not seen his primary care physician for 7 years. He has no complaints other than feeling easily fatigued. He has no significant medical history. He reports drinking half a pint of liquor a day. His temperature is 98.7°F (37.1°C), pulse is 65/min, respiratory rate is 15/min, and blood pressure is 120/70 mm Hg. Physical examination shows reddish color to both of his palms. His abdomen has no focal tenderness but is difficult to assess due to distention. Laboratory studies show:
Hemoglobin 11.0 g/dL
Hematocrit 33%
Leukocyte count 5,000/mm3
Platelet count 60,000/mm3
Serum
Na+ 135 mEq/L
K+ 4.5 mEq/L
Cl- 100 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 15 mg/dL
Creatinine 1.3 mg/dL
Total bilirubin 3.0 mg/dL
AST 112 U/L
ALT 80 U/L
Alkaline phosphatase 130 U/L
Which of the following is the most likely explanation for this patient's thrombocytopenia?
- A. Uremia
- B. Hypersplenism (Correct Answer)
- C. Autoimmune antibodies
- D. Bone marrow infiltration
- E. Decreased protein synthesis
Hepatocellular carcinoma Explanation: ***Hypersplenism***
- This patient presents with **severe alcohol use**, signs of **liver disease** (fatigue, palmar erythema, abdominal distention suggestive of ascites, elevated bilirubin, AST, ALT), and **thrombocytopenia**. **Cirrhosis** from heavy alcohol use can lead to **portal hypertension**, causing **splenomegaly** and subsequent **hypersplenism**, where the spleen sequesters and destroys platelets at an accelerated rate.
- The combination of **liver dysfunction** and **low platelet count** in the context of chronic alcohol abuse strongly points to hypersplenism as the cause for thrombocytopenia.
*Uremia*
- **Uremia** refers to a buildup of waste products in the blood due to **kidney dysfunction**, which can cause platelet dysfunction but typically does not cause a significant decrease in platelet count (thrombocytopenia) itself.
- While the patient's **creatinine is slightly elevated** (1.3 mg/dL), it is not indicative of severe renal failure that would typically lead to uremia-induced bleeding diathesis, and his platelet count is significantly low rather than merely dysfunctional.
*Autoimmune antibodies*
- **Immune thrombocytopenia (ITP)** is caused by **autoantibodies** against platelets, leading to their premature destruction. While it causes severe thrombocytopenia, it is typically a diagnosis of exclusion and less likely given the clear evidence of advanced **liver disease** and **portal hypertension** in this patient.
- There is no specific evidence or clinical context suggesting an autoimmune process is at play rather than a direct complication of chronic liver disease.
*Bone marrow infiltration*
- **Bone marrow infiltration** (e.g., by malignancy or fibrosis) can lead to **myelophthisic anemia** and thrombocytopenia due to the displacement of megakaryocytes.
- This patient's presentation with prominent signs of **liver disease** and **chronic alcohol abuse** does not suggest bone marrow pathology as the primary cause for his thrombocytopenia. No other cytopenias (beyond mild anemia, which can be multifactorial in liver disease) are profoundly out of proportion to suggest a primary marrow disorder.
*Decreased protein synthesis*
- **Decreased protein synthesis** is a hallmark of severe **liver failure**, affecting the production of many proteins, including clotting factors. However, the liver primarily produces factors involved in coagulation, not platelets themselves.
- While liver failure can impair thrombopoietin production, which stimulates platelet production, **hypersplenism** is a more direct and common cause of significant thrombocytopenia in the context of advanced liver disease with portal hypertension.
More Hepatocellular carcinoma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.