Tuberculosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tuberculosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
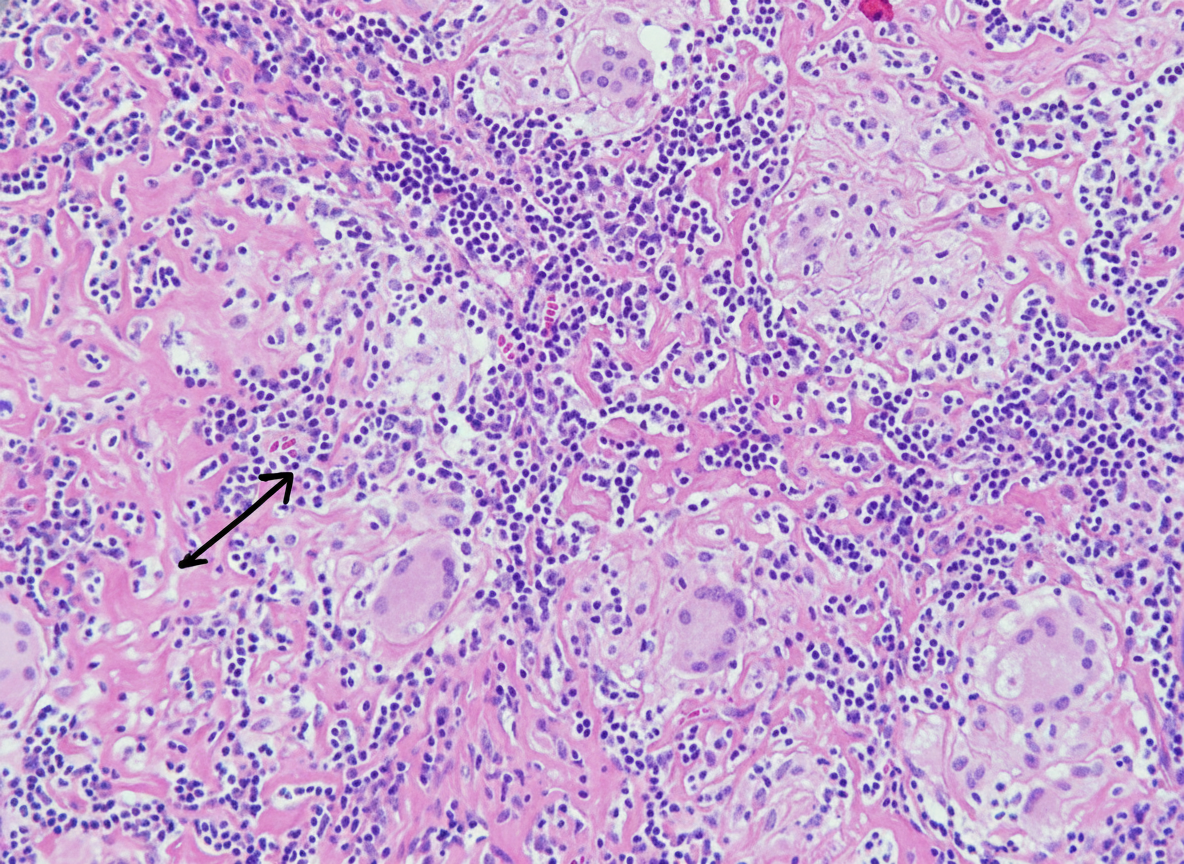
Tuberculosis US Medical PG Question 1: A 32-year-old man who recently emigrated from Somalia comes to the physician because of a 4-week history of fever, cough, and chest pain. He has had a 5-kg (11-lb) weight loss over the last 3 months despite no changes in appetite. His temperature is 38.1°C (100.6°F). Physical examination shows enlarged cervical lymph nodes. The lungs are clear to auscultation. The results of an interferon-γ release assay are positive. An x-ray of the chest shows bilateral mediastinal lymphadenopathy. A transbronchial needle aspiration biopsy of a mediastinal lymph node is performed; a photomicrograph of the specimen is shown. The structure indicated by the arrow is most likely comprised of which of the following types of cells?
- A. Natural killer cells
- B. B cells
- C. Fibroblasts
- D. Neutrophils
- E. Macrophages (Correct Answer)
Tuberculosis Explanation: ***Macrophages***
- The photomicrograph shows a **granuloma**, characterized by collections of **epithelioid histiocytes** (modified macrophages) and **multinucleated giant cells**, which are essentially fused macrophages.
- This morphology, coupled with the clinical picture of fever, cough, weight loss, positive interferon-γ release assay, and mediastinal lymphadenopathy in a patient from an endemic area, is highly suggestive of **tuberculosis**, a classic granulomatous disease.
*Natural killer cells*
- Natural killer cells are part of the innate immune system and are primarily involved in **killing virally infected cells** and **tumor cells**.
- They are not the primary cellular component forming the characteristic structure of a granuloma.
*B cells*
- B cells are responsible for **antibody production** and antigen presentation.
- While B cells may be present in the periphery of a granuloma, they do not form the core epithelioid and giant cell components.
*Fibroblasts*
- Fibroblasts produce **collagen** and the extracellular matrix, playing a role in **scar formation** and the fibrotic wall that can surround chronic granulomas.
- They do not constitute the primary cellular components of the inflammatory core of a granuloma.
*Neutrophils*
- Neutrophils are typically associated with **acute inflammation** and bacterial infections, characterized by pus formation.
- They are not the predominant cell type in the organized structure of a **granuloma** found in tuberculosis.
Tuberculosis US Medical PG Question 2: A 24-year-old man comes to the physician for a routine health maintenance examination. He feels well. He has type 1 diabetes mellitus. His only medication is insulin. He immigrated from Nepal 2 weeks ago . He lives in a shelter. He has smoked one pack of cigarettes daily for the past 5 years. He has not received any routine childhood vaccinations. The patient appears healthy and well nourished. He is 172 cm (5 ft 8 in) tall and weighs 68 kg (150 lb); BMI is 23 kg/m2. His temperature is 36.8°C (98.2°F), pulse is 72/min, and blood pressure is 123/82 mm Hg. Examination shows a healed scar over his right femur. The remainder of the examination shows no abnormalities. A purified protein derivative (PPD) skin test is performed. Three days later, an induration of 13 mm is noted. Which of the following is the most appropriate initial step in the management of this patient?
- A. Administer isoniazid for 9 months
- B. Collect sputum sample for culture
- C. Perform interferon-γ release assay
- D. Obtain a chest x-ray (Correct Answer)
- E. Perform PCR of the sputum
Tuberculosis Explanation: ***Obtain a chest x-ray***
- A **positive PPD test** (13 mm induration in a patient with risk factors) indicates possible **latent tuberculosis infection (LTBI)**, but before initiating treatment, it's crucial to rule out **active tuberculosis (TB)**.
- A chest x-ray is the initial step to screen for signs of active disease, such as **infiltrates, cavitations**, or **lymphadenopathy**, which would necessitate a different treatment regimen than LTBI.
*Administer isoniazid for 9 months*
- This is a standard treatment for **LTBI**, but it should only be initiated after **active TB has been ruled out**.
- Treating active TB with LTBI monotherapy would be inadequate and could lead to **drug resistance**.
*Collect sputum sample for culture*
- **Sputum culture** is essential for diagnosing active pulmonary TB and for **drug susceptibility testing**, but it's typically performed *after* a chest x-ray suggests active disease.
- In a patient with a positive PPD and no symptoms, starting with sputum cultures without imaging is not the most appropriate first step.
*Perform interferon-γ release assay*
- **Interferon-γ release assays (IGRAs)**, such as QuantiFERON-TB Gold or T-Spot.TB, are alternative tests for detecting **M. tuberculosis infection**.
- While IGRAs can be used in place of or in conjunction with PPD, they also do not differentiate between latent and active infection, so a chest x-ray would still be required.
*Perform PCR of the sputum*
- **PCR (nucleic acid amplification test)** of sputum rapidly detects *M. tuberculosis* DNA and is a valuable tool for diagnosing **active TB**, especially in cases where rapid results are needed.
- However, like sputum culture, it is usually reserved for situations where there is a strong suspicion of active disease based on clinical symptoms or imaging findings.
Tuberculosis US Medical PG Question 3: A 68-year-old man presents to the physician with fever, cough, weakness, night sweats, and poor appetite for the past 6 months. Medical records suggest that he has lost 7.5 kg (16.5 lb) of weight during this period. There is no history of breathlessness, nasal discharge, nasal obstruction, palpitations, chest pain, or symptoms related to digestion. He was released from prison 9 months ago after serving a 2-year sentence. His temperature is 38.1°C (100.6°F), pulse is 84/min, respirations are 16/min, and blood pressure is 122/80 mm Hg. Physical examination shows hepatomegaly and generalized lymphadenopathy, and auscultation of the chest reveals diffuse crackles throughout the lung fields bilaterally. On direct ophthalmoscopy, three discrete, yellow-colored, 0.5 mm to 1.0 mm lesions with indistinct borders are seen in the posterior pole. A chest X-ray is shown in the image. Tuberculin skin test with purified protein derivative is negative. What is the most likely diagnosis?
- A. Bronchoalveolar carcinoma
- B. Tuberculosis (Correct Answer)
- C. Chronic histoplasmosis
- D. Langerhans cell histiocytosis
- E. Sarcoidosis
Tuberculosis Explanation: ***Tuberculosis***
- The patient's history of **fever**, **cough**, **weakness**, **night sweats**, **weight loss**, and recent incarceration are highly suggestive of **tuberculosis (TB)**. His chest X-ray shows **miliary infiltrates**, indicative of **miliary tuberculosis**, and the presence of **choroidal tubercles** on ophthalmoscopy is pathognomonic for disseminated TB.
- While the **tuberculin skin test (TST)** is negative, this can occur in disseminated TB due to anergy, where the immune system is severely compromised and unable to mount a response. The **hepatomegaly** and **generalized lymphadenopathy** further support disseminated disease.
*Bronchoalveolar carcinoma*
- Although it can present with **cough** and **weight loss**, **bronchoalveolar carcinoma** typically does not cause generalized lymphadenopathy or hepatomegaly unless it is widely metastatic, which would likely present with more severe respiratory compromise or other focal symptoms.
- The miliary pattern on chest X-ray and choroidal tubercles are not typical features of bronchoalveolar carcinoma, making it a less likely diagnosis.
*Chronic histoplasmosis*
- **Chronic histoplasmosis** can cause fever, cough, weight loss, and widespread pulmonary infiltrates, particularly in immunocompromised individuals or those with significant exposure (e.g., caves, bird/bat excrement).
- However, choroidal tubercles are rare in histoplasmosis, and the patient's history of incarceration (a risk factor for TB) makes histoplasmosis less probable in this context.
*Langerhans cell histiocytosis*
- **Langerhans cell histiocytosis** primarily affects young adults and often presents with respiratory symptoms, bone lesions, and sometimes skin involvement.
- The diffuse miliary pattern on chest X-ray and choroidal tubercles are not characteristic features of Langerhans cell histiocytosis, nor is generalized lymphadenopathy and hepatomegaly as initial presentation.
*Sarcoidosis*
- **Sarcoidosis** is characterized by non-caseating granulomas and can present with cough, fever, weight loss, and lymphadenopathy, especially hilar and mediastinal.
- While pulmonary infiltrates can occur, the miliary pattern characteristic of disseminated infection (as seen in TB) and choroidal tubercles, though sometimes seen in ocular sarcoidosis, are not the hallmark presentation for disseminated sarcoidosis in this manner.
Tuberculosis US Medical PG Question 4: A 55-year-old homeless man is presented to the emergency department by a group of volunteers after they found him coughing up blood during 1 of the beneficiary dinners they offer every week. His medical history is unknown as he recently immigrated from Bangladesh. He says that he has been coughing constantly for the past 3 months with occasional blood in his sputum. He also sweats a lot at nights and for the past 2 days, he has been thirsty with increased frequency of urination and feeling hungrier than usual. The respiratory rate is 30/min and the temperature is 38.6°C (101.5°F). He looks emaciated and has a fruity smell to his breath. The breath sounds are reduced over the apex of the right lung. The remainder of the physical exam is unremarkable. Biochemical tests are ordered, including a hemoglobin A1c (HbA1c) (8.5%) and chest radiography reveals cavitations in the apical region of the right lung. Which of the following immune cells is most critical in orchestrating the formation and maintenance of the granulomatous structure that led to these cavitations?
- A. B lymphocytes
- B. Treg lymphocytes
- C. Epithelioid cells
- D. Th1 lymphocytes (Correct Answer)
- E. Th2 lymphocytes
Tuberculosis Explanation: ***Th1 lymphocytes***
- The clinical picture strongly suggests **reactivation of tuberculosis** due to the cavitary lung lesions, constitutional symptoms, and likely immunocompromise from undiagnosed diabetes (HbA1c 8.5%).
- **Th1 lymphocytes** are crucial for the cell-mediated immune response against **intracellular pathogens** like *Mycobacterium tuberculosis*, producing **interferon-gamma** which activates macrophages to form granulomas and contain the infection, thus preventing dissemination and contributing to cavitation.
*B lymphocytes*
- **B lymphocytes** primarily mediate **humoral immunity** by producing antibodies, which are less critical for controlling intracellular bacterial infections like tuberculosis.
- While antibodies can play a role in modulating inflammation, they are not the primary cells involved in the **granuloma formation** and containment of *M. tuberculosis* within the lungs.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) primarily function to **suppress immune responses** to prevent autoimmunity and limit tissue damage.
- While they can modulate the immune response in tuberculosis, their main role is not in the initial formation of **cavities** or primary defense against the pathogen, but rather in regulating the overall inflammatory process.
*Epithelioid cells*
- **Epithelioid cells** are **activated macrophages** that form the core of granulomas, but they are not lymphocytes; they are derived from monocytes.
- They are a crucial component of the **granulomatous structure** itself, but their differentiation and activation are largely driven by cytokines produced by **Th1 lymphocytes**.
*Th2 lymphocytes*
- **Th2 lymphocytes** are primarily involved in immunity against **extracellular parasites** and in allergic reactions, mediating humoral responses through cytokines like **IL-4, IL-5, and IL-13**.
- An effective immune response against *Mycobacterium tuberculosis* is dominated by a **Th1 cellular response**, and a prominent Th2 response is generally considered detrimental or insufficient in controlling the infection.
Tuberculosis US Medical PG Question 5: A 21-year-old U.S. born first year medical student with no prior hospital or healthcare work presents to the physician for a routine physical exam. The patient is HIV negative, denies drug use, and denies sick contacts. The physician places a purified protein tuberculin test in the patient's right forearm intradermally. What is the proper time to read the test and induration diameter that would indicate a positive test result?
- A. 36 hours and 7mm diameter
- B. 48 hours and 11mm diameter
- C. 72 hours and 16mm diameter (Correct Answer)
- D. 96 hours and 14mm diameter
- E. 24 hours and 18mm diameter
Tuberculosis Explanation: ***72 hours and 16mm diameter***
- The **purified protein derivative (PPD) test** should ideally be read between 48 and 72 hours after administration to allow for the **Type IV hypersensitivity reaction** to fully develop.
- For individuals with no known risk factors for tuberculosis and no prior exposure, an induration of **≥15 mm** is considered a positive result. A 16mm diameter falls within this range.
*36 hours and 7mm diameter*
- **36 hours** is too early to accurately read a PPD test, as the delayed-type hypersensitivity reaction may not have fully manifested.
- A **7mm induration** would generally be considered negative in a low-risk individual, as the threshold for positivity in this group is higher.
*48 hours and 11mm diameter*
- While **48 hours** is within the acceptable window for reading a PPD test, an **11mm induration** is not considered positive for a young, low-risk individual without any predisposing conditions like HIV or organ transplant.
- The threshold for a positive result in this demographic is typically **≥15 mm**.
*96 hours and 14mm diameter*
- **96 hours** (4 days) is generally too late to accurately read a PPD test, as the reaction may begin to fade, leading to a potentially false negative.
- A **14mm induration** is still below the positive threshold of ≥15mm for a low-risk individual.
*24 hours and 18mm diameter*
- **24 hours** is significantly too early to read a PPD test, as the immune response will not have fully developed, leading to unreliable results.
- While **18mm induration** would be a positive result, the timing makes the reading invalid.
Tuberculosis US Medical PG Question 6: A 25-year-old woman presented to an urgent care center with a complaint of a cough for more than 3 weeks that was accompanied by night sweats, weight loss, and malaise. On physical examination, the patient had slightly pale palpebral conjunctivae, bilateral posterior cervical lymphadenopathy, but with no adventitious breath sounds in the lung fields bilaterally. The remainder of the physical examination was routine. The patient was started on a drug regimen that was to be taken for 6 months. On follow-up after 2 months, the ALT and AST levels were elevated. Which of the following anti-tubercular drugs could have contributed to this laboratory result?
- A. Streptomycin
- B. Rifampicin
- C. Ethambutol
- D. Isoniazid (Correct Answer)
- E. Pyrazinamide
Tuberculosis Explanation: ***Isoniazid***
- **Isoniazid** is the **most commonly implicated** anti-tubercular drug in hepatotoxicity, particularly in the first 2 months of therapy, which matches this patient's timeline.
- While **Pyrazinamide** and **Rifampicin** can also cause hepatotoxicity, **Isoniazid** causes hepatotoxicity in **10-20% of patients** with elevated transaminases and is the **most frequent single agent** responsible for drug-induced liver injury in TB treatment.
- The hepatotoxicity manifests as elevated **ALT and AST levels** and can range from mild, asymptomatic enzyme elevations to severe, fatal hepatitis.
- Risk factors include **fast acetylator status**, alcohol use, and concurrent use of other hepatotoxic drugs.
*Rifampicin*
- **Rifampicin** can cause **hepatotoxicity**, but when it occurs alone (without Isoniazid), it typically presents as a **cholestatic pattern** with elevated alkaline phosphatase and bilirubin rather than predominantly elevated transaminases.
- Its primary adverse effects include **red-orange discoloration** of bodily fluids and significant drug interactions due to potent **cytochrome P450 enzyme induction**.
- Hepatotoxicity from Rifampicin is **less common** than from Isoniazid when used as monotherapy.
*Pyrazinamide*
- **Pyrazinamide** can cause **hepatotoxicity** and is associated with elevated liver enzymes, making it a possible contributor.
- However, **hepatotoxicity from Pyrazinamide** is **dose-dependent** and typically seen more with higher doses (>30 mg/kg/day) or in patients with pre-existing liver disease.
- It is also associated with **hyperuricemia** and can precipitate gouty arthritis, which is not indicated in this clinical scenario.
- In standard first-line therapy, **Isoniazid remains statistically more likely** to cause isolated transaminase elevation.
*Streptomycin*
- **Streptomycin** is an aminoglycoside antibiotic primarily known for its **ototoxicity** (vestibular and cochlear damage) and **nephrotoxicity**, rather than hepatotoxicity.
- Liver enzyme elevation is **not a characteristic adverse effect** of streptomycin and is rarely reported.
*Ethambutol*
- **Ethambutol** is primarily associated with **optic neuritis**, leading to decreased visual acuity and red-green color blindness, which requires monitoring with regular visual acuity and color vision testing.
- While mild liver enzyme elevations can rarely occur, significant **hepatotoxicity is uncommon** and not a characteristic primary adverse effect of ethambutol.
Tuberculosis US Medical PG Question 7: A 62-year-old man presents to the emergency department with increased fatigue and changes in his vision. The patient states that for the past month he has felt abnormally tired, and today he noticed his vision was blurry. The patient also endorses increased sweating at night and new onset headaches. He states that he currently feels dizzy. The patient has a past medical history of diabetes and hypertension. His current medications include insulin, metformin, and lisinopril. His temperature is 99.5°F (37.5°C), blood pressure is 157/98 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is within normal limits. HEENT exam reveals non-tender posterior and anterior chain lymphadenopathy. Abdominal exam reveals splenomegaly and hepatomegaly. There are large, non-tender palpable lymph nodes in the patient's inguinal region. Neurological exam is notable for decreased sensation in the patient's hands and feet. He also complains of a numb/tingling pain in his extremities that has been persistent during this time. Dermatologic exam is notable for multiple bruises on his upper and lower extremities. Which of the following is most likely to be abnormal in this patient?
- A. Calcium
- B. IgA and IgG
- C. IgM (Correct Answer)
- D. Natural killer cells
- E. T-cells
Tuberculosis Explanation: ***IgM***
- The patient's symptoms, including **fatigue**, **vision changes (blurry vision)**, **night sweats**, **headaches**, **dizziness**, **lymphadenopathy**, **hepatosplenomegaly**, **peripheral neuropathy** (decreased sensation, numb/tingling pain), and **easy bruising**, are highly suggestive of **Waldenström macroglobulinemia (WM)**.
- WM is a **B-cell lymphoma** characterized by the overproduction of **monoclonal IgM paraprotein**, which can lead to **hyperviscosity syndrome** (causing vision changes, headaches, dizziness) and other systemic symptoms.
*Calcium*
- While hypercalcemia can be seen in some hematologic malignancies, it is **not a typical feature of Waldenström macroglobulinemia**.
- **Multiple myeloma**, another plasma cell dyscrasia, is more commonly associated with hypercalcemia due to increased osteoclastic activity.
*IgA and IgG*
- **IgA and IgG myelomas** involve the overproduction of IgA and IgG antibodies, respectively, and present with different clinical features than described.
- The constellation of symptoms in this patient, particularly the signs of hyperviscosity and a B-cell lymphoma affecting IgM production, does not align with these types of immunoglobulin abnormalities.
*Natural killer cells*
- Abnormalities in **natural killer (NK) cells** are typically associated with certain viral infections, autoimmune diseases, or specific NK cell lymphomas, which do not match the clinical picture.
- While NK cells are part of the immune system, their primary role or dysfunction is not directly implicated in the presenting symptoms of Waldenström macroglobulinemia.
*T-cells*
- **T-cell lymphomas** involve the abnormal proliferation of T-lymphocytes and generally present with different clinical manifestations, such as skin lesions, lymphadenopathy, and organ infiltration.
- The systemic symptoms, hyperviscosity, and specific organ involvement noted in this patient are more characteristic of a B-cell malignancy like Waldenström macroglobulinemia, not a primary T-cell disorder.
Tuberculosis US Medical PG Question 8: A 67-year-old man presents to his primary care provider for routine follow-up. He complains of mild fatigue and occasional tingling in both feet. He reports that this numbness and tingling has led to him having 3 falls over the last month. He has had type 2 diabetes mellitus for 23 years and hypertension for 15 years, for which he takes metformin and enalapril. He denies tobacco or alcohol use. His blood pressure is 126/82 mm Hg, the heart rate is 78/min, and the respiratory rate is 15/min. Significant laboratory results are shown:
Hemoglobin 10 g/dL
Hematocrit 30%
Mean corpuscular volume (MCV) 110 fL
Serum B12 level 210 picograms/mL
Which of the following is the best next step in the management of this patient’s condition?
- A. Methylmalonic acid level (Correct Answer)
- B. Folic acid supplementation
- C. Pregabalin or gabapentin
- D. Intrinsic factor antibody
- E. Schilling test
Tuberculosis Explanation: ***Methylmalonic acid level***
- The patient presents with symptoms of **peripheral neuropathy** (tingling, numbness, falls) and **macrocytic anemia** (MCV 110 fL, Hb 10 g/dL), along with a **borderline low serum vitamin B12 level** (210 pg/mL).
- **Long-term metformin use** (23 years in this patient) is a well-known risk factor for vitamin B12 deficiency due to impaired intestinal absorption.
- **Methylmalonic acid (MMA)** is a more sensitive and specific marker for **functional vitamin B12 deficiency**, as its levels are elevated when B12 is insufficient to convert MMA to succinyl CoA.
- When serum B12 is in the borderline range (200-400 pg/mL) but clinical suspicion is high, MMA and homocysteine levels confirm true deficiency.
*Folic acid supplementation*
- While folic acid deficiency also causes **macrocytic anemia**, the neurological symptoms (neuropathy, falls) are characteristic of **vitamin B12 deficiency**, not folate deficiency.
- Supplementing with folic acid in a B12-deficient patient can mask the hematological signs of B12 deficiency while allowing neurological damage to progress.
*Pregabalin or gabapentin*
- These medications are used to treat **neuropathic pain**, which can be a symptom of vitamin B12 deficiency.
- However, they address symptoms rather than the underlying cause, and the priority is to diagnose and treat the deficiency to prevent further neurological deterioration.
*Intrinsic factor antibody*
- **Intrinsic factor antibodies** are helpful in diagnosing **pernicious anemia**, a common cause of vitamin B12 deficiency.
- However, the initial step after identifying borderline B12 and symptoms of deficiency is to confirm the actual functional deficiency with MMA and homocysteine levels, before determining the cause.
*Schilling test*
- The **Schilling test** is an older diagnostic test used to determine the cause of vitamin B12 malabsorption.
- It is rarely performed due to its complexity and the availability of more modern diagnostic tools like anti-intrinsic factor antibodies and gastric parietal cell antibodies.
Tuberculosis US Medical PG Question 9: A 25-year-old woman presents to the emergency department with fatigue and weakness. She states over the past 24 hours she has not felt like herself and has felt like she has no strength. The patient has no significant past medical history other than a single episode of blood-tinged diarrhea 1 week ago which resolved on its own. Her temperature is 99.4°F (37.4°C), blood pressure is 124/62 mmHg, pulse is 95/min, respirations are 29/min, and oxygen saturation is 95% on room air. Physical exam is notable for 2/5 strength of the lower extremities and decreased sensation in the lower extremities and finger tips. Which of the following is the best initial step in management?
- A. IV immunoglobulin
- B. Dexamethasone
- C. Spirometry (Correct Answer)
- D. Intubation
- E. Pyridostigmine
Tuberculosis Explanation: ***Spirometry***
- The patient's symptoms (fatigue, weakness, decreased strength, and sensation in extremities) following a gastrointestinal infection are highly suggestive of **Guillain-Barré Syndrome (GBS)**.
- **Spirometry** is the most critical initial step to assess respiratory function, as **respiratory muscle weakness** is the primary cause of morbidity and mortality in GBS.
*IV immunoglobulin*
- While **intravenous immunoglobulin (IVIG)** is a treatment for GBS, it is not the *initial* management step.
- The immediate priority in suspected GBS is to assess and stabilize the patient's respiratory status, not to initiate definitive treatment.
*Dexamethasone*
- **Corticosteroids** like dexamethasone have **not been shown to be effective** in treating GBS and may even prolong recovery in some cases.
- Their use is generally avoided in the management of GBS.
*Intubation*
- **Intubation** is indicated if spirometry reveals rapidly declining or severely compromised respiratory function, but it is not the *initial* step.
- An assessment of respiratory capacity via spirometry should precede intubation unless acute respiratory failure is immediately apparent.
*Pyridostigmine*
- **Pyridostigmine** is an anticholinesterase inhibitor used primarily for the symptomatic treatment of **myasthenia gravis**.
- It is not indicated for the management of GBS, which involves a different pathophysiological mechanism.
Tuberculosis US Medical PG Question 10: A 58-year-old man is diagnosed with right lower lobe pneumonia and has been admitted to a tertiary care hospital. His laboratory investigations suggest that he acquired an infection from the hospital where he underwent an elective abdominal surgery 3 weeks ago. His past medical records reveal a history of deep vein thrombosis and pulmonary embolism one year prior. After a steady clinical improvement over 5 days of inpatient treatment, he develops a cough, breathlessness, and hemoptysis on the 6th day. His temperature is 38.6°C (101.5°F), the pulse is 112/min, the blood pressure is 130/84 mm Hg, and the respiratory rate is 28/min. A general examination shows the presence of edema over the right leg and tenderness over the right calf region. Auscultation of the chest reveals localized crackles over the left mammary region and right infrascapular region. However, his heart sounds are normal, except for the presence of tachycardia, and there are no murmurs. Which of the following is the investigation of choice as the immediate next step in this patient’s management?
- A. Ventilation-perfusion scanning
- B. Echocardiography
- C. Contrast-enhanced computed tomography (CECT) of chest (Correct Answer)
- D. Serum brain natriuretic peptide
- E. Plasma D-dimer
Tuberculosis Explanation: ***Contrast-enhanced computed tomography (CECT) of chest***
- This patient presents with an acute onset of **cough, breathlessness, and hemoptysis** along with signs of **deep vein thrombosis (DVT)**, including leg edema and calf tenderness. This clinical picture, especially with a history of DVT and pulmonary embolism, is highly suggestive of a **pulmonary embolism (PE)**.
- **CT pulmonary angiography (CTPA)**, performed as a contrast-enhanced CT of the chest, is the **gold standard** for diagnosing PE, as it directly visualizes thrombi within the pulmonary arteries and provides detailed anatomical information.
- Given the **high pre-test probability** (prior DVT/PE, clinical signs of DVT, recent surgery, hemoptysis, tachycardia), immediate imaging with CTPA is indicated without need for D-dimer testing.
*Ventilation-perfusion scanning*
- **Ventilation-perfusion (V/Q) scanning** is an alternative for diagnosing PE, but it is less sensitive and specific than CTPA, especially in the presence of **pre-existing lung disease** (like the pneumonia this patient has), which can lead to indeterminate results.
- It is usually reserved for patients with **renal insufficiency** or **contrast allergy** who cannot undergo CTPA.
*Echocardiography*
- **Echocardiography** can show signs of **right heart strain** in massive PE, but it is not diagnostic for PE itself, as it cannot directly visualize the emboli in the pulmonary arteries.
- It is more useful in assessing **cardiac function** and ruling out other cardiac causes of breathlessness, or for risk stratification in confirmed PE.
*Serum brain natriuretic peptide*
- **Serum brain natriuretic peptide (BNP)** levels can be elevated in patients with **right heart strain** due to PE, but it is a **non-specific marker** and cannot confirm the diagnosis of PE.
- Elevated BNP can also indicate other cardiac conditions, such as **heart failure**.
*Plasma D-dimer*
- **Plasma D-dimer** is a useful test to **exclude PE** in patients with a **low or intermediate pre-test probability**, but a **positive D-dimer** is non-specific and can be elevated in many conditions, including infection, surgery, and inflammation.
- Given the patient's **high clinical probability** for PE (prior DVT/PE, current DVT signs, recent surgery, hemoptysis) and active pneumonia, D-dimer testing is **not indicated** as it would not change management—imaging with CTPA is already warranted regardless of D-dimer result.
More Tuberculosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.