Pneumonia (community-acquired, hospital-acquired) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pneumonia (community-acquired, hospital-acquired). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 1: A 65-year-old woman is brought to the emergency department by her daughter for fever and cough. She just returned from a cruise trip to the Bahamas with her family 5 days ago and reports that she has been feeling ill since then. She endorses fever, productive cough, and general malaise. Her daughter also mentions that the patient has been having some diarrhea but reports that the rest of her family has been experiencing similar symptoms. Physical examination was significant for localized crackles at the right lower lobe. Laboratory findings are as follows:
Serum
Na+: 130 mEq/L
K+: 3.9 mEq/L
Cl-: 98 mEq/L
HCO3-: 27 mEq/L
Mg2+: 1.8 mEq/L
What findings would you expect in this patient?
- A. High titers of cold agglutinins
- B. Gram-negative rod on chocolate agar with factors V and X
- C. Gram-negative on silver stain (Correct Answer)
- D. Gram-positive diplococci on Gram stain
- E. Broad-based budding on fungal sputum culture
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Gram-negative on silver stain***
- The patient's symptoms (fever, productive cough, malaise, diarrhea), recent cruise travel, and hyponatremia are classic presentations of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a **Gram-negative rod** that stains poorly with Gram stain and is best visualized using **silver stain**.
*High titers of cold agglutinins*
- **Cold agglutinins** are typically associated with **atypical pneumonia** caused by *Mycoplasma pneumoniae*.
- While *Mycoplasma* can cause similar respiratory symptoms, the presence of diarrhea and hyponatremia points away from it.
*Gram-negative rod on chocolate agar with factors V and X*
- This describes the growth requirements for *Haemophilus influenzae*, which needs **hematin (factor X)** and **NAD (factor V)** to grow on chocolate agar.
- While *H. influenzae* can cause pneumonia, the patient's specific presentation (cruise travel, diarrhea, hyponatremia) is more indicative of *Legionella*.
*Gram-positive diplococci on Gram stain*
- This microscopic finding is characteristic of **Streptococcus pneumoniae**, the most common cause of **community-acquired pneumonia**.
- Although *S. pneumoniae* can cause pneumonia, the detailed clinical picture, including hyponatremia and diarrhea, is not typical for uncomplicated pneumococcal pneumonia.
*Broad-based budding on fungal sputum culture*
- **Broad-based budding** is a characteristic feature of **Blastomyces dermatitidis**, a cause of fungal pneumonia.
- While fungal infections can cause pneumonia, the rapid onset, cruise exposure, and systemic symptoms (diarrhea, hyponatremia) are not classic for blastomycosis.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 2: A patient is hospitalized for pneumonia. Gram-positive cocci in clusters are seen on sputum gram stain. Which of the following clinical scenarios is most commonly associated with this form of pneumonia?
- A. Elderly patient who has trouble swallowing and poor dentition
- B. An alcoholic with evidence of empyema and "currant jelly sputum"
- C. An otherwise healthy young adult with a week of mild fatigue, chills, and cough
- D. Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness (Correct Answer)
- E. HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness***
- Gram-positive cocci in clusters suggests **Staphylococcus aureus**, which is a common cause of secondary bacterial pneumonia, often following **viral illnesses** (e.g., influenza).
- This scenario represents a classic presentation of **secondary bacterial pneumonia**, where the initial viral infection compromises the respiratory defenses, allowing bacterial superinfection.
*Elderly patient who has trouble swallowing and poor dentition*
- This scenario points towards **aspiration pneumonia**, often caused by a **polymicrobial infection** that includes oral anaerobes, not typically dominated by Gram-positive cocci in clusters.
- While *S. aureus* can cause aspiration pneumonia, the primary concern in this context would be **anaerobic bacteria**, given the aspiration risk factors.
*An alcoholic with evidence of empyema and \"currant jelly sputum\"*
- This description is highly suggestive of **Klebsiella pneumoniae** infection, which typically presents with thick, gelatinous, and often **blood-tinged sputum**.
- **Klebsiella** is a Gram-negative rod, not Gram-positive cocci in clusters.
*An otherwise healthy young adult with a week of mild fatigue, chills, and cough*
- This presentation is more consistent with **atypical pneumonia** caused by organisms like **Mycoplasma pneumoniae** or **Chlamydophila pneumoniae**, which would not show Gram-positive cocci in clusters on sputum stain.
- **Streptococcus pneumoniae** (Gram-positive cocci in chains) can also cause community-acquired pneumonia in otherwise healthy individuals, but the "clusters" indicate **Staphylococcus aureus**.
*HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity*
- This clinical picture strongly suggests **Pneumocystis jirovecii pneumonia (PJP)**, which is common in severely immunocompromised HIV patients.
- *P. jirovecii* is a fungus and would not be seen as Gram-positive cocci in clusters on a routine Gram stain.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 3: A 59-year-old man comes to the clinic for an annual well-exam. He was lost to follow-up for the past 3 years due to marital issues but reports that he feels fine. The patient reports, “I feel tired but it is probably because I am getting old. I do feel a little feverish today - I think I got a cold.” His past medical history is significant for hypertension that is controlled with hydrochlorothiazide. He reports fatigue, congestion, cough, and night sweats. He denies any sick contacts, recent travel, weight changes, chest pain, or dizziness. His temperature is 101°F (38.3°C), blood pressure is 151/98 mmHg, pulse is 97/min, and respirations are 15/min. His laboratory values are shown below:
Hemoglobin: 13.5 g/dL
Hematocrit: 41%
Leukocyte count: 25,000/mm^3
Segmented neutrophils: 73%
Bands: 8%
Eosinophils: 1%
Basophils: 2%
Lymphocytes: 15%
Monocytes: 2%
Platelet count: 200,000/mm^3
What diagnostic test would be helpful in distinguishing this patient’s condition from pneumonia?
- A. Erythrocyte sedimentation rate
- B. Magnetic resonance imaging of the chest
- C. Leukocyte alkaline phosphatase (Correct Answer)
- D. Presence of smudge cells
- E. C-reactive protein
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Leukocyte alkaline phosphatase***
- This patient's symptoms (fatigue, fever, night sweats, **elevated leukocyte count** with a left shift) suggest a **myeloproliferative disorder** like **Chronic Myeloid Leukemia (CML)**, which can mimic infection.
- A **low Leukocyte Alkaline Phosphatase (LAP) score** is characteristic of CML, while an **elevated LAP score** is seen in bacterial infections (like pneumonia) and leukemoid reactions.
*Erythrocyte sedimentation rate*
- **ESR** is a general marker of **inflammation** and can be elevated in both pneumonia and various hematologic malignancies.
- It does not specifically differentiate between inflammatory processes due to infection versus a myeloproliferative disorder.
*Magnetic resonance imaging of the chest*
- While MRI can detect pulmonary infiltrates suggestive of pneumonia, it is **not typically the first-line imaging** for pneumonia and would not specifically differentiate it from a hematologic malignancy.
- **Chest X-ray or CT scan** would be more appropriate for initial pulmonary evaluation, but neither directly helps distinguish between infection and leukemia without other clinical data.
*Presence of smudge cells*
- **Smudge cells** (fragile lymphocytes) are characteristic of **Chronic Lymphocytic Leukemia (CLL)**.
- This patient's **leukocyte differential** shows a predominance of neutrophils and bands, not lymphocytes, making CLL less likely.
*C-reactive protein*
- **CRP** is another **acute phase reactant** that is elevated in response to inflammation, including infections like pneumonia.
- Similar to ESR, a high CRP level would not specifically distinguish between an infectious process and a myeloproliferative disorder.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 4: A 43-year-old woman comes to the physician because of a fever, nausea, and a nonproductive cough for 7 days. During this period, she has had headaches, generalized fatigue, and muscle and joint pain. She has also had increasing shortness of breath for 2 days. She has type 2 diabetes mellitus and osteoarthritis of her left knee. Current medications include insulin and ibuprofen. She had smoked two packs of cigarettes daily for 20 years but stopped 10 years ago. Her temperature is 38.1°C (100.6°F), pulse is 94/min, respirations are 18/min, and blood pressure is 132/86 mm Hg. The lungs are clear to auscultation. There are multiple skin lesions with a blue livid center, pale intermediate zone, and a dark red peripheral rim on the upper and lower extremities. Laboratory studies show:
Hemoglobin 14.6 g/dL
Leukocyte count 11,100/mm3
Serum
Na+ 137 mEq/L
K+ 4.1 mEq/L
Cl- 99 mEq/L
Urea nitrogen 17 mg/dL
Glucose 123 mg/dL
Creatinine 0.9 mg/dL
Which of the following is the most likely causal organism?
- A. Legionella pneumophila
- B. Mycoplasma pneumoniae (Correct Answer)
- C. Haemophilus influenzae
- D. Klebsiella pneumoniae
- E. Staphylococcus aureus
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Mycoplasma pneumoniae***
- The patient presents with a **nonproductive cough**, **headache**, **fatigue**, **myalgia**, and **arthralgia**, which are classic symptoms of **atypical pneumonia**. The presence of **erythema multiforme** (skin lesions with a blue livid center, pale intermediate zone, and dark red peripheral rim) is also strongly associated with *Mycoplasma pneumoniae* infection.
- While the chest X-ray specifically mentioned is not provided, atypical pneumonias often show **patchy infiltrates** that are out of proportion to the patient's symptoms (walking pneumonia), and the constellation of symptoms strongly points towards *Mycoplasma pneumoniae*.
*Legionella pneumophila*
- While *Legionella* can cause **atypical pneumonia** with gastrointestinal symptoms (**nausea** in this case) and hyponatremia, the prominent skin rash (erythema multiforme) is not a typical feature.
- **Hyponatremia** and **confusion** are more commonly associated with *Legionella*, neither of which are prominent findings here.
*Haemophilus influenzae*
- This typically causes **bacterial pneumonia** with more pronounced purulent sputum and lung consolidation, which is not suggested by the nonproductive cough and clear auscultation.
- While *Haemophilus influenzae* can cause respiratory infections, it is less likely to present with the systemic symptoms and characteristic rash seen in this patient.
*Klebsiella pneumoniae*
- Characteristically causes severe, **lobar pneumonia**, often seen in alcoholics and individuals with chronic lung disease, and is associated with **"currant jelly" sputum**.
- The patient's symptoms (nonproductive cough, systemic symptoms, rash) and the description of the lung auscultation (clear) do not align with a typical *Klebsiella pneumoniae* infection.
*Staphylococcus aureus*
- Can cause severe **necrotizing pneumonia**, often following a viral illness (e.g., influenza), and is associated with multiple cavitations and abscesses on chest imaging.
- While there is a history of smoking, the presentation with diffuse systemic symptoms and erythema multiforme is not typical for **staphylococcal pneumonia**.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 5: A 57-year-old man comes to the physician for a follow-up examination. During the last 6 months, he has had recurring pneumonia after undergoing a surgical operation. He reports that, when food has gone down his windpipe, he has not automatically coughed. Examination shows normal voluntary coughing, but an impaired cough reflex. The nerve responsible for this patient's symptoms is most likely damaged at which of the following anatomical sites?
- A. Foramen magnum
- B. Aortic arch
- C. Piriform recess (Correct Answer)
- D. Parotid gland
- E. Infratemporal fossa
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Piriform recess***
- Damage to the sensory fibers of the **internal laryngeal nerve (a branch of the superior laryngeal nerve, which comes from the vagus nerve)** in the piriform recess impairs the afferent limb of the cough reflex, specifically from the larynx above the vocal folds.
- This results in the inability to automatically cough when food enters the windpipe (aspiration), explaining the recurrent pneumonia.
*Foramen magnum*
- Damage at the foramen magnum would typically affect structures like the **medulla oblongata** or proximal cervical spinal cord, leading to more widespread neurological deficits such as respiratory failure, severe motor and sensory deficits, or cranial nerve palsies.
- Such extensive involvement is not indicated by isolated impairment of the cough reflex with normal voluntary coughing.
*Aortic arch*
- The **left recurrent laryngeal nerve** loops around the aortic arch, but damage here would primarily cause **hoarseness** due to vocal cord paralysis, which is not described.
- While the recurrent laryngeal nerves innervate the intrinsic muscles of the larynx and provide some sensation below the vocal folds, impairment here is less likely to cause the specific symptom of absent cough reflex upon aspiration without hoarseness.
*Parotid gland*
- The parotid gland houses the **facial nerve (CN VII)**, which innervates muscles of facial expression, and the **auriculotemporal nerve** (a branch of CN V3) provides sensation.
- Damage here would cause **facial paralysis** or sensory deficits, neither of which are consistent with an impaired cough reflex.
*Infratemporal fossa*
- The infratemporal fossa contains structures like the **mandibular nerve (CN V3)**, **otic ganglion**, and the **chorda tympani** (a branch of CN VII).
- Damage here would typically affect mastication, sensation to the lower face, or taste, none of which explain the patient's specific symptoms related to coughing and aspiration.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 6: A 59-year-old woman comes to the emergency department because of a 2-day history of worsening fever, chills, malaise, productive cough, and difficulty breathing. Three days ago, she returned from a trip to South Africa. She has type 2 diabetes mellitus, hypertension, and varicose veins. Her current medications include metformin, lisinopril, and atorvastatin. Her temperature is 39.4°C (102.9°F), pulse is 102/minute, blood pressure is 94/68 mm Hg, and respirations are 31/minute. Pulse oximetry on 2 L of oxygen via nasal cannula shows an oxygen saturation of 91%. Examination reveals decreased breath sounds and dull percussion over the left lung base. The skin is very warm and well-perfused. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.6 g/dL
Leukocyte count 15,400/mm3
platelet count 282,000/mm3
Serum
Na+ 144 mEq/L
Cl- 104 mEq/L
K+ 4.9 mEq/L
Creatinine 1.5 mg/dL
Blood and urine for cultures are obtained. Intravenous fluid resuscitation is begun. Which of the following is the next best step in management?
- A. Erythromycin
- B. Intravenous ceftriaxone and azithromycin (Correct Answer)
- C. External cooling and intravenous acetaminophen
- D. Intravenous vancomycin and ceftriaxone
- E. CT of the chest with contrast
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Intravenous ceftriaxone and azithromycin***
* This patient presents with **severe community-acquired pneumonia (CAP)** meeting criteria for ICU-level care, including hypotension (94/68 mm Hg), hypoxemia requiring supplemental oxygen, tachypnea (31/min), and altered mental status indicators. The presentation meets multiple **severe CAP criteria** (CURB-65 score ≥3 or IDSA/ATS major criteria).
* **Intravenous ceftriaxone** (a third-generation cephalosporin) provides broad-spectrum coverage against common bacterial causes of CAP, including *Streptococcus pneumoniae* and *Haemophilus influenzae*. **Azithromycin** (a macrolide) is crucial to cover atypical pathogens like *Mycoplasma pneumoniae*, *Chlamydophila pneumoniae*, and *Legionella pneumoniae*.
* This combination represents the **standard empiric therapy for severe CAP** per IDSA/ATS guidelines. The patient's recent travel to South Africa and severe symptoms increase the likelihood of atypical pathogens or resistant strains, making dual therapy essential.
*Erythromycin*
* While erythromycin is a macrolide that covers atypical pathogens, its use is generally limited due to higher rates of gastrointestinal side effects and a less favorable dosing profile compared to newer macrolides like azithromycin. It does not provide adequate coverage for typical bacterial causes of CAP.
* In severe CAP with signs of sepsis, monotherapy with erythromycin would be insufficient and would not address the need for broad-spectrum coverage against both typical and atypical bacteria. Dual antibiotic therapy is required for severe cases.
*External cooling and intravenous acetaminophen*
* These interventions are appropriate for **fever reduction** but do not address the underlying severe infection (pneumonia with sepsis). While important for symptomatic relief, they are not the "next best step in management" for a life-threatening condition.
* Treating the infection with appropriate antibiotics is paramount to prevent further deterioration and organ damage. In severe sepsis from pneumonia, **source control through antimicrobial therapy takes precedence** over symptomatic fever management.
*Intravenous vancomycin and ceftriaxone*
* **Vancomycin** is primarily used to cover **methicillin-resistant *Staphylococcus aureus* (MRSA)**. While MRSA can cause severe pneumonia, there are no specific risk factors for MRSA in this patient (e.g., recent hospitalization, IV drug use, prior MRSA infection, severe influenza, cavitary lesions, hemoptysis).
* Adding vancomycin without specific indications for MRSA coverage would represent unnecessary broad-spectrum antibiotic use and could contribute to antibiotic resistance. The combination of **ceftriaxone and azithromycin is the standard empiric therapy** for severe CAP without MRSA risk factors.
*CT of the chest with contrast*
* A CT scan of the chest might be useful for further characterizing the pneumonia, identifying complications (e.g., empyema, abscess), or differentiating from other conditions **after initial stabilization**. However, in a patient with severe pneumonia, hypoxemia, and hypotension, the immediate priority is stabilization and initiation of empiric antibiotic therapy.
* Delaying life-saving antibiotic treatment to obtain a CT scan could worsen the patient's prognosis and violate the principle of **early appropriate antibiotics in sepsis** (ideally within 1 hour). Clinical diagnosis with chest X-ray is sufficient to initiate treatment, and further imaging can be obtained after stabilization if needed.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 7: A 55-year-old man is brought to the emergency department by ambulance after being found disoriented. He has limited ability to communicate in English but indicates that he has left flank pain and a fever. Chart review reveals that he has diabetes and sleep apnea but both are well controlled. He also has a 30-pack-year smoking history and has lost about 20 pounds since his last presentation. Physical exam reveals a bulge in his left scrotum and ultrasound reveals bilateral kidney stones. Which of the following findings is also associated with the most likely cause of this patient's symptoms?
- A. Gynecomastia
- B. Cavitary lung lesion
- C. Jaundice
- D. Increased hematocrit (Correct Answer)
- E. Aniridia
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Increased hematocrit***
- This patient's symptoms (disorientation, left flank pain, fever, weight loss, smoking history, and **left scrotal bulge suggesting varicocele**) are highly suggestive of **renal cell carcinoma (RCC)**.
- The **left-sided varicocele** in an adult male is particularly significant, as it may indicate **left renal vein obstruction** by the tumor (the left testicular vein drains into the left renal vein).
- Approximately 3-10% of patients with RCC develop **erythrocytosis** due to **ectopic erythropoietin (EPO) production** by the tumor, leading to **increased hematocrit** as a paraneoplastic syndrome.
- Other paraneoplastic manifestations of RCC include hypercalcemia (PTHrP production), hypertension (renin production), and Stauffer syndrome (hepatic dysfunction).
*Gynecomastia*
- While paraneoplastic syndromes can occur with RCC, **gynecomastia** is not a common associated finding.
- Gynecomastia is more often associated with **testicular tumors** (hCG-secreting), liver disease, or certain medications.
*Cavitary lung lesion*
- While RCC can metastasize to the lungs, presenting as **nodules or masses** (cannonball metastases), a **cavitary lesion** is more characteristic of infections (e.g., tuberculosis, fungal infections) or **squamous cell carcinoma** of the lung.
- The primary presentation here points to renal pathology with paraneoplastic manifestations.
*Jaundice*
- **Jaundice** indicates **hyperbilirubinemia** and is not a direct paraneoplastic syndrome of RCC.
- It may occur with extensive metastatic disease to the liver causing biliary obstruction or in Stauffer syndrome (non-metastatic hepatic dysfunction), but this is less common than erythrocytosis.
*Aniridia*
- **Aniridia** (absence of the iris) is a rare congenital condition strongly associated with **Wilms' tumor** (nephroblastoma), a pediatric kidney cancer, as part of the **WAGR syndrome** (Wilms tumor, Aniridia, Genitourinary abnormalities, intellectual disability/Range of developmental delays).
- It is not associated with adult renal cell carcinoma.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 8: A 34-year-old woman comes to the emergency department because of right flank pain and vomiting for 5 hours. She has had fever and chills for the past 2 days. She attended a barbecue 3 days ago, where she ate egg salad. She underwent surgery for left ovarian torsion a year ago. Menses occur at regular 28-day intervals and last 5 days. She is sexually active with 2 male partners and uses condoms inconsistently. Her only medication is an oral contraceptive pill. She is 163 cm (5 ft 4 in) tall and weighs 72.5 kg (160 lb); BMI is 27.5 kg/m2. She appears uncomfortable. Her temperature is 38.9°C (102°F), pulse is 101/min, and blood pressure is 118/76 mm Hg. The lungs are clear to auscultation. The right lower quadrant and right flank show severe tenderness to palpation. Pelvic examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12.8 g/dL
Leukocyte count 14,200/mm3
Platelet count 230,000/mm3
Serum
Na+ 136 mEq/L
K+ 3.8 mEq/L
Cl- 103 mEq/L
Urea nitrogen 23 mg/dL
Creatinine 1.2 mg/dL
Urine
Blood 1+
Protein 1+
Glucose negative
Leukocyte esterase positive
Nitrites negative
RBC 6–8/hpf
WBC 80–85/hpf
Which of the following is the most likely diagnosis?
- A. Ovarian torsion
- B. Pelvic inflammatory disease
- C. Urethritis
- D. Pyelonephritis (Correct Answer)
- E. Gastroenteritis
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Pyelonephritis***
- The patient presents with **fever, chills, right flank pain**, and **vomiting**, with **costovertebral angle tenderness** on examination, all characteristic of pyelonephritis.
- Urinalysis shows significant **leukocyturia (WBC 80-85/hpf)**, **leukocyte esterase positivity**, and low-grade **hematuria**, further supporting a urinary tract infection that has ascended to the kidneys.
*Ovarian torsion*
- While ovarian torsion can cause acute, severe unilateral abdominal pain and vomiting, the patient's **fever and chills**, severe **flank tenderness**, and **urinalysis findings (leukocyturia)** are inconsistent with ovarian torsion.
- A pelvic exam showing **no abnormalities** also makes ovarian pathology less likely.
*Pelvic inflammatory disease*
- PID typically presents with **lower abdominal pain**, fever, and vaginal discharge, often associated with a **positive cervical motion tenderness** or adnexal tenderness on pelvic exam.
- The patient's primary complaint of **flank pain** and the absence of pelvic exam findings or discharge make PID less likely.
*Urethritis*
- Urethritis primarily causes **dysuria, urinary frequency, and urgency** with little to no fever or flank pain unless it progresses to cystitis or pyelonephritis.
- The patient's systemic symptoms (fever, chills) and significant flank pain indicate a more severe, upper urinary tract infection.
*Gastroenteritis*
- Gastroenteritis typically presents with **nausea, vomiting, diarrhea**, and abdominal cramping, often preceded by exposure to contaminated food.
- While vomiting is present, the **lack of diarrhea**, prominent **flank pain**, fever, and especially the **pathologic urinalysis findings** (high WBCs) rule out uncomplicated gastroenteritis.
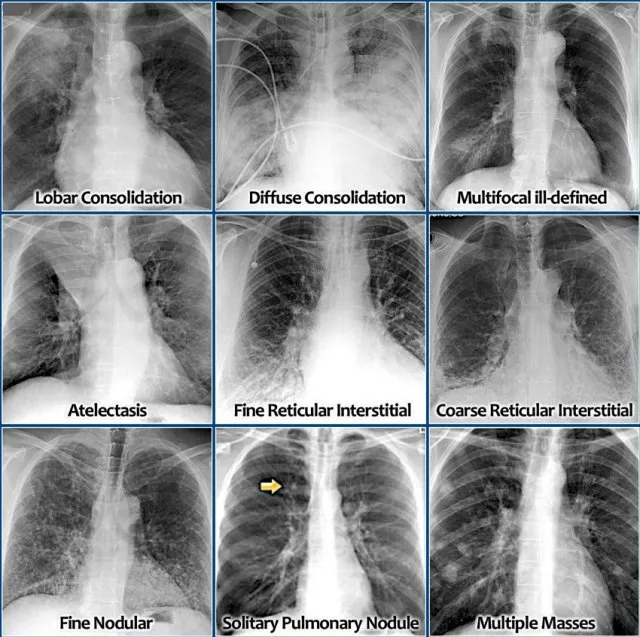
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 9: A 24-year-old woman, otherwise healthy, presents with a non-productive cough, sore throat, and myalgia. The patient reports that her symptoms started gradually 2 weeks ago and have not improved. She has no significant past medical history and no current medications. She is a college student and denies any recent overseas travel. The patient received the flu vaccine this year, and her 2-part PPD required for school was negative. She does not smoke, drink, or use recreational drugs. The patient denies being sexually active. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 110/75 mm Hg, pulse 98/min, respirations 20/min, and oxygen saturation 99% on room air. On physical exam, the patient is alert and cooperative. The cardiac exam is normal. There are rales present bilaterally over both lung fields. The skin and conjunctiva are pale. The laboratory tests are pending. The chest X-ray is shown in the image. Which of the following laboratory findings would also commonly be found in this patient?
- A. Elevated cold agglutinin titers (Correct Answer)
- B. Heinz bodies on peripheral smear
- C. Low serum levels of complement
- D. Low serum ferritin and serum iron
- E. Schistocytes on peripheral smear
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Elevated cold agglutinin titers***
- The clinical presentation (non-productive cough, sore throat, myalgia, bilateral rales, pallor) in a young, otherwise healthy patient, along with the chest X-ray showing bilateral patchy infiltrates, is consistent with **atypical pneumonia**, most likely caused by ***Mycoplasma pneumoniae***.
- ***Mycoplasma pneumoniae*** infection can induce **autoimmune hemolytic anemia** through the production of **cold agglutinins** (IgM antibodies that agglutinate RBCs at cold temperatures). This occurs in approximately 50% of Mycoplasma infections, though clinically significant hemolysis is less common.
- Laboratory findings include **elevated cold agglutinin titers** (typically >1:64), **positive direct Coombs test** (IgM and complement), **spherocytes** on peripheral smear (from extravascular hemolysis), elevated indirect bilirubin, and decreased haptoglobin.
- The pallor noted on exam reflects the hemolytic anemia caused by these cold-reactive autoantibodies.
*Low serum ferritin and serum iron*
- **Iron deficiency anemia** presents with pallor and fatigue, but results from chronic blood loss, inadequate dietary intake, or malabsorption, not from acute atypical pneumonia.
- While anemia is present in this case, it's **hemolytic anemia** (from cold agglutinins), not iron deficiency. Iron studies would typically be normal or show elevated ferritin (acute phase reactant).
*Heinz bodies on peripheral smear*
- **Heinz bodies** are inclusions of denatured hemoglobin seen in **G6PD deficiency** after oxidative stress or with unstable hemoglobin variants.
- While G6PD deficiency causes hemolytic anemia, it's not associated with *Mycoplasma pneumoniae* infection and doesn't explain the respiratory symptoms or chest X-ray findings.
*Schistocytes on peripheral smear*
- **Schistocytes** are fragmented RBCs indicating **microangiopathic hemolytic anemia** (TTP, HUS, DIC) where RBCs are mechanically sheared in damaged microvasculature.
- *Mycoplasma pneumoniae* causes **immune-mediated extravascular hemolysis** via cold agglutinins, not microangiopathic intravascular hemolysis. Spherocytes, not schistocytes, would be seen.
*Low serum levels of complement*
- Low complement levels indicate complement consumption in **immune complex diseases** (SLE, post-infectious glomerulonephritis) or alternative pathway activation (C3 glomerulonephritis).
- While cold agglutinins can activate complement (causing hemolysis), this is a **local effect on RBC surfaces**, not systemic complement depletion. Serum complement levels typically remain normal in cold agglutinin disease.
Pneumonia (community-acquired, hospital-acquired) US Medical PG Question 10: A 43-year-old woman visits her primary care physician complaining of abdominal pain for the past 6 months. She reports that the pain is localized to her lower abdomen and often resolves with bowel movements. She states that some days she has diarrhea while other times she will go 4-5 days without having a bowel movement. She started a gluten-free diet in hopes that it would help her symptoms, but she has not noticed much improvement. She denies nausea, vomiting, hematochezia, or melena. Her medical history is significant for generalized anxiety disorder and hypothyroidism. Her father has a history of colon cancer. The patient takes citalopram and levothyroxine. Physical examination reveals mild abdominal tenderness with palpation of lower quadrant but no guarding or rebound. A guaiac test is negative. A complete blood count is pending. Which of the following is the next best step in management?
- A. Loperamide
- B. Thyroid ultrasound
- C. High fiber diet
- D. Anti-endomysial antibody titer
- E. Colonoscopy (Correct Answer)
Pneumonia (community-acquired, hospital-acquired) Explanation: ***Colonoscopy***
- Given her age (43 years), **family history of colon cancer** (father), and new-onset, fluctuating bowel habits with abdominal pain, a **colonoscopy** is indicated to rule out organic pathology.
- While her symptoms are suggestive of **irritable bowel syndrome (IBS)**, the **red flag symptom** of a family history of colon cancer necessitates further investigation beyond a clinical diagnosis of IBS.
*Loperamide*
- **Loperamide** is an antidiarrheal generally used for **symptomatic relief** in individuals with diarrhea-predominant IBS (IBS-D).
- Her symptoms fluctuate between diarrhea and constipation, and addressing the underlying cause or ruling out more serious conditions should precede symptomatic treatment.
*Thyroid ultrasound*
- She has a history of **hypothyroidism** and is on **levothyroxine**, but there is no indication of uncontrolled thyroid disease or a new thyroid issue.
- Her abdominal symptoms are unrelated to her thyroid condition, making a thyroid ultrasound an inappropriate next step.
*High fiber diet*
- A **high-fiber diet** can be beneficial for some forms of IBS, particularly **constipation-predominant IBS (IBS-C)**.
- However, it would not address the **red flag symptom** of family history of colon cancer and would not be the priority over ruling out malignancy.
*Anti-endomysial antibody titer*
- An **anti-endomysial antibody titer** is used to screen for **celiac disease**.
- While she tried a gluten-free diet, there are no other symptoms highly suggestive of celiac disease, and more importantly, this test would not address the **red flag concerns** for colorectal cancer.
More Pneumonia (community-acquired, hospital-acquired) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.