Infective endocarditis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Infective endocarditis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
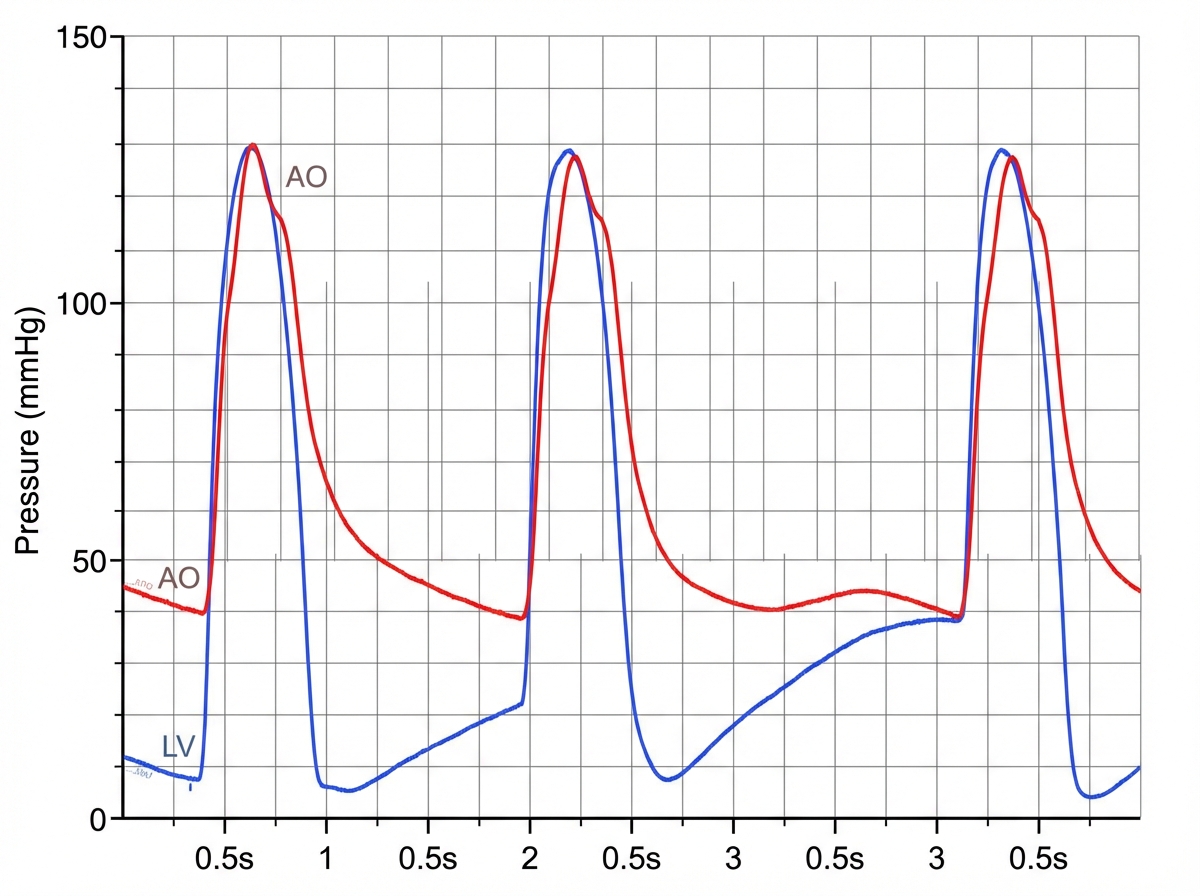
Infective endocarditis US Medical PG Question 1: A 31-year-old man comes to the physician because of a 5-day history of fever, chills, and dyspnea. His temperature is 38.9°C (102°F) and pulse is 90/min. Cardiac examination shows a murmur. In addition to other measures, cardiac catheterization is performed. A graph showing the results of the catheterization is shown. This patient most likely has which of the following valvular heart defects?
- A. Mitral regurgitation
- B. Aortic regurgitation (Correct Answer)
- C. Mitral stenosis
- D. Pulmonary regurgitation
- E. Aortic stenosis
Infective endocarditis Explanation: ***Aortic regurgitation***
- Aortic regurgitation is characterized by a high-pitched **diastolic decrescendo murmur**, best heard at the left sternal border.
- The catheterization graph shows a **rapid decline in aortic pressure during diastole**, signifying blood flowing back into the left ventricle, which is characteristic of aortic regurgitation.
*Mitral regurgitation*
- Mitral regurgitation would cause a **pansystolic murmur** and a large **V wave in the pulmonary capillary wedge pressure tracing**, neither of which is implied by the provided information.
- Its primary hemodynamic feature is blood flowing back into the **left atrium during systole**, not diastolic aortic pressure changes.
*Mitral stenosis*
- Mitral stenosis typically presents with a **diastolic rumble** and an **opening snap**, which are different from the findings described.
- Hemodynamically, it would show an **elevated left atrial pressure** and a pressure gradient across the mitral valve during diastole.
*Pulmonary regurgitation*
- Pulmonary regurgitation involves the flow of blood from the pulmonary artery back into the **right ventricle during diastole**.
- This condition would lead to characteristic changes in **right ventricular and pulmonary artery pressures**, not the left-sided heart pressures shown in the graph.
*Aortic stenosis*
- Aortic stenosis causes a **systolic crescendo-decrescendo murmur**, often with radiation to the carotids.
- Hemodynamically, it would show a **significant pressure gradient across the aortic valve during systole** and a delayed carotid upstroke.
Infective endocarditis US Medical PG Question 2: A 37-year-old man with a history of IV drug use presents to the ED with complaints of fevers, chills, and malaise for one week. He admits to recently using IV and intramuscular heroin. Vital signs are as follows: T 40.0 C, HR 120 bpm, BP 110/68 mmHg, RR 14, O2Sat 98%. Examination reveals a new systolic murmur that is loudest at the lower left sternal border. Initial management includes administration of which of the following regimens?
- A. IV Vancomycin, IV ceftriaxone, IV fluconazole
- B. IV Vancomycin, IV ceftriaxone (Correct Answer)
- C. IV Vancomycin, IV levofloxacin
- D. IV Vancomycin
- E. IV Vancomycin, IV gentamicin, PO rifampin
Infective endocarditis Explanation: ***IV Vancomycin, IV ceftriaxone***
- The patient's history of **IV drug use**, fevers, chills, new systolic murmur, and likely **tricuspid valve involvement** (murmur loudest at the lower left sternal border) strongly suggest **infective endocarditis**.
- The empiric regimen for suspected endocarditis in an IV drug user should cover **methicillin-resistant _Staphylococcus aureus_ (MRSA)** with **vancomycin** and gram-negative organisms with a **third-generation cephalosporin** like **ceftriaxone**.
- This combination provides broad coverage for the most common pathogens in native valve endocarditis among IV drug users, including MRSA, streptococci, and many gram-negative organisms.
*IV Vancomycin, IV ceftriaxone, IV fluconazole*
- While vancomycin and ceftriaxone are appropriate, **fluconazole** is an antifungal and is generally not indicated for empiric treatment of bacterial endocarditis unless there's a strong suspicion of **fungal infection**.
- Fungal endocarditis is less common and usually requires prolonged treatment with specific antifungals, often alongside surgical intervention.
*IV Vancomycin, IV levofloxacin*
- **Levofloxacin** is a fluoroquinolone that covers a broad spectrum of bacteria but is not the preferred empiric agent for gram-negative coverage in suspected endocarditis in IV drug users due to concerns about resistance and lack of superior coverage compared to third-generation cephalosporins.
- **Ceftriaxone** provides better coverage for common gram-negative pathogens associated with endocarditis among IV drug users in this context.
*IV Vancomycin, IV gentamicin, PO rifampin*
- **Gentamicin** is an aminoglycoside that provides effective gram-negative coverage and is often used in combination therapy for endocarditis, but **rifampin** is typically reserved for prosthetic valve endocarditis or refractory cases due to its risk of drug interactions and resistance development.
- **Oral rifampin** may not be appropriate for initial aggressive treatment in an acutely ill patient with suspected acute endocarditis, where IV therapy is preferred.
*IV Vancomycin*
- While **vancomycin** is crucial for covering **MRSA** which is common in IV drug users, it alone does not provide adequate coverage for potential **gram-negative pathogens** that can also cause endocarditis in this population.
- **Multidrug empiric therapy** is essential to cover a broad range of likely pathogens causing endocarditis in IV drug users, especially with severe symptoms.
Infective endocarditis US Medical PG Question 3: A 75-year-old man presents to his primary care provider with malaise and low-grade fever after he underwent a cystoscopy for recurrent cystitis and pyelonephritis two weeks ago. His past medical history is significant for coronary artery disease and asthma. His current medications include aspirin, metoprolol, atorvastatin, and albuterol inhaler. Temperature is 37.2°C (99.0°F), blood pressure is 110/70 mm Hg, pulse is 92/min and respirations are 14/min. On physical examination, there are painless areas of hemorrhage on his palms and soles. Cardiac auscultation reveals a new pansystolic murmur over the apex. An echocardiogram shows echogenic endocardial vegetation on a leaflet of the mitral valve. Which of the following pathogens is most likely responsible for his condition?
- A. Staphylococcus aureus
- B. Enterococcus (Correct Answer)
- C. Pseudomonas aeruginosa
- D. Staphylococcus epidermidis
- E. Streptococcus gallolyticus
Infective endocarditis Explanation: ***Enterococcus***
- The patient's history of recent **cystoscopy**, recurrent **cystitis**, and **pyelonephritis** suggests a genitourinary source of infection, making *Enterococcus* a likely pathogen for **infective endocarditis**.
- **Enterococci** are common causes of urinary tract infections, especially in elderly males and those undergoing urological procedures, and can subsequently cause endocarditis.
*Staphylococcus aureus*
- While *S. aureus* is a leading cause of infective endocarditis, particularly in intravenous drug users or those with central lines, there is no direct evidence here to suggest a **cutaneous** or **catheter-related** entry point.
- The patient's clinical presentation, specifically the preceding genitourinary procedure, points away from *S. aureus* as the most probable cause.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* typically causes endocarditis in specific contexts such as **intravenous drug use** or in patients with **prosthetic valves** and healthcare-associated infections, none of which are strongly indicated.
- Despite the history of recent instrumentation, *Pseudomonas* is less common as a cause of endocarditis following cystoscopy compared to *Enterococcus*.
*Staphylococcus epidermidis*
- *S. epidermidis* is usually associated with **prosthetic valve endocarditis** or infection of **intravascular devices**, as it is a common skin commensal.
- The patient has no history of prosthetic valves, and the infection appears to be linked to a genitourinary procedure rather than a device-related contamination.
*Streptococcus gallolyticus*
- *Streptococcus gallolyticus* (**formerly *S. bovis***) is classically associated with **colorectal carcinoma** and gastrointestinal sources of bacteremia.
- Although it can cause endocarditis, the patient's presentation with a recent cystoscopy points towards a genitourinary pathogen rather than a gastrointestinal one.
Infective endocarditis US Medical PG Question 4: A 24-year-old male is brought into the emergency department complaining of chills, headaches, and malaise for several days. He also states that he experiences shortness of breath when climbing two flights of stairs in his home. He admits to occasionally using intravenous drugs during the previous year. On exam, his vital signs are temperature 39.2° C, heart rate 108/min, blood pressure 124/82 mm Hg, respiratory rate 20/min, and oxygen saturation 98% on room air. A holosystolic murmur is heard near the lower left sternal border. An echocardiogram confirms vegetations on the tricuspid valve. What is the most likely causative organism of this patient's condition?
- A. Candida albicans
- B. Staphylococcus aureus (Correct Answer)
- C. Streptococcus mutans
- D. Staphylococcus epidermidis
- E. Streptococcus bovis
Infective endocarditis Explanation: ***Staphylococcus aureus***
- This patient's history of **intravenous drug use** and the finding of **tricuspid valve vegetations** are highly characteristic of **infectious endocarditis** caused by *Staphylococcus aureus.*
- *S. aureus* is the most common pathogen in IV drug users due to its prevalence on the skin and ability to adhere to and colonize damaged heart valves.
*Candida albicans*
- While *Candida albicans* can cause endocarditis, especially in immunocompromised individuals or those with central venous catheters, it is **less common** than *S. aureus* in IV drug users and does not typically present with the same high frequency.
- Fungal endocarditis often has a more **subacute course** and can be associated with larger vegetations.
*Streptococcus mutans*
- *Streptococcus mutans* is a common cause of **dental caries** and is associated with infective endocarditis, particularly in patients with pre-existing valvular heart disease and poor dental hygiene, affecting the **mitral or aortic valves**.
- It is **not typically associated** with endocarditis in intravenous drug users.
*Staphylococcus epidermidis*
- *Staphylococcus epidermidis* is a common cause of **prosthetic valve endocarditis** but is less frequently involved in native valve endocarditis, especially in IV drug users, compared to *S. aureus*.
- It is a **coagulase-negative staphylococcus** and a common skin commensal.
*Streptococcus bovis*
- *Streptococcus bovis* (now *Streptococcus gallolyticus*) endocarditis is strongly associated with **colorectal cancer** or other gastrointestinal pathologies.
- This patient has no features suggestive of gastrointestinal disease, making *S. bovis* an **unlikely causative agent**.
Infective endocarditis US Medical PG Question 5: A 37-year-old man presents to the emergency department for a persistent fever. The patient states he has felt unwell for the past week and has felt subjectively febrile. The patient has a past medical history of a suicide attempt and alcohol abuse. He is not currently taking any medications. The patient admits to using heroin and cocaine and drinking 5-8 alcoholic drinks per day. His temperature is 103°F (39.4°C), blood pressure is 92/59 mmHg, pulse is 110/min, respirations are 20/min, and oxygen saturation is 96% on room air. Cardiopulmonary exam is notable for a systolic murmur heard best along the left sternal border. Dermatologic exam reveals scarring in the antecubital fossa. Which of the following is the next best step in management?
- A. CT scan
- B. Ultrasound
- C. Chest radiograph
- D. Blood cultures (Correct Answer)
- E. Vancomycin and gentamicin
Infective endocarditis Explanation: ***Blood cultures***
- The patient's history of **intravenous drug use (IVDU)**, persistent fever, and a **new systolic murmur** strongly suggest **infective endocarditis**.
- **Blood cultures** are crucial for identifying the causative organism and guiding appropriate antibiotic therapy, serving as the cornerstone of diagnosis in suspected endocarditis.
*CT scan*
- While CT scans can be useful for identifying complications of endocarditis (e.g., septic emboli in the brain or lungs), they are **not the initial diagnostic step** for identifying the source of infection.
- CT scans expose the patient to **radiation** and are more expensive, making them less suitable as a first step compared to blood cultures.
*Ultrasound*
- An **echocardiogram** (a type of ultrasound) is essential for visualizing vegetations on heart valves, but it is typically performed *after* blood cultures reveal bacteremia to confirm the diagnosis and assess severity.
- A general ultrasound of other body areas would be non-specific and **unlikely to pinpoint the cause** of persistent fever in this clinical context.
*Chest radiograph*
- A chest radiograph can identify **pulmonary infiltrates** or **septic emboli in the lungs**, which are potential complications of right-sided endocarditis (common in IVDU).
- However, a chest radiograph **does not identify the causative organism** or confirm the primary diagnosis of endocarditis, making it a secondary investigation.
*Vancomycin and gentamicin*
- This combination represents a broad-spectrum antibiotic regimen often used for **empiric treatment of infective endocarditis**, particularly in IVDU patients due to concerns for MRSA or resistant streptococcal species.
- While ultimately necessary, administering antibiotics *before* obtaining **blood cultures** can significantly reduce the yield of cultures and hinder definitive diagnosis and tailored treatment.
Infective endocarditis US Medical PG Question 6: A 65-year-old man presents with low-grade fever and malaise for the last 4 months. He also says he has lost 9 kg (20 lb) during this period and suffers from extreme fatigue. Past medical history is significant for a mitral valve replacement 5 years ago. His temperature is 38.1°C (100.6°F), respirations are 22/min, pulse is 102/min, and blood pressure is 138/78 mm Hg. On physical examination, there is a new onset 2/6 holosystolic murmur loudest in the apical area of the precordium. Which of the following organisms is the most likely cause of this patient’s condition?
- A. Enterococcus (Correct Answer)
- B. Candida albicans
- C. Coagulase-negative Staphylococcus spp.
- D. Escherichia coli
- E. Pseudomonas aeruginosa
Infective endocarditis Explanation: ***Enterococcus***
- This patient has **late prosthetic valve endocarditis (PVE)**, occurring **5 years after mitral valve replacement**.
- Late PVE (>1 year post-surgery) is most commonly caused by **viridans streptococci** and ***Staphylococcus aureus***, followed by **Enterococcus species**.
- Among the given options, ***Enterococcus*** is the most common cause, particularly in **elderly patients**.
- The **subacute presentation** with **4 months of low-grade fever, malaise, weight loss**, and **new-onset murmur** is consistent with enterococcal endocarditis.
- Enterococcus is a common cause of healthcare-associated endocarditis and has increased prevalence in patients with prosthetic valves.
*Coagulase-negative Staphylococcus spp.*
- Coagulase-negative staphylococci (e.g., *S. epidermidis*) are the **most common cause of early PVE** (within the first year after surgery).
- At **5 years post-surgery**, this represents **late PVE**, where coagulase-negative staph is much less common than streptococci, *S. aureus*, and enterococci.
- While it can occur in late PVE, it is not the most likely organism in this timeframe.
*Escherichia coli*
- *E. coli* is an uncommon cause of endocarditis, typically associated with underlying gastrointestinal or urinary tract sources.
- It generally presents **acutely** rather than with the subacute 4-month course seen here.
- Not a typical cause of prosthetic valve endocarditis.
*Candida albicans*
- Fungal endocarditis is rare and typically seen in **immunocompromised patients, IV drug users**, or those with **prolonged ICU stays** with indwelling catheters.
- While *Candida* can cause PVE, it is much less common than bacterial causes in this clinical context.
*Pseudomonas aeruginosa*
- *Pseudomonas* endocarditis typically occurs in **IV drug users** and commonly affects the **tricuspid valve** (right-sided).
- Usually presents as an **acute infection** rather than the subacute presentation here.
- Not a common cause of late prosthetic valve endocarditis in non-IVDU patients.
Infective endocarditis US Medical PG Question 7: A 27-year-old man presents to the emergency department with weakness and a fever for the past week. The patient is homeless and has a past medical history of alcohol and IV drug abuse. His temperature is 102°F (38.9°C), blood pressure is 107/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a tremulous patient with antecubital scars and a murmur over the left lower sternal border. Blood cultures are drawn and the patient is started on vancomycin and ceftriaxone and is admitted to the ICU. The patient's fever and symptoms do not improve despite antibiotic therapy for which the initial identified organism is susceptible. Cultures currently reveal MRSA as one of the infective organisms. Which of the following is the best next step in management?
- A. Transesophageal echocardiography (Correct Answer)
- B. Obtain new blood cultures
- C. CT scan of the chest
- D. Nafcillin and piperacillin-tazobactam
- E. Vancomycin and gentamicin
Infective endocarditis Explanation: ***Transesophageal echocardiography***
- The patient's history of **IV drug abuse**, **fever**, **new murmur**, and identification of **MRSA** strongly suggest **infective endocarditis**.
- A Transesophageal echocardiography (TEE) is the **most sensitive and specific imaging modality** to detect vegetations, abscesses, or valvular damage, which is crucial for guiding further management.
*Obtain new blood cultures*
- While repeating blood cultures can be useful to confirm eradication or identify new pathogens, the initial blood cultures already revealed MRSA, which is a common cause of **endocarditis in IV drug users**.
- The immediate priority given the lack of improvement and high suspicion of endocarditis is to visualize the heart valves for vegetations.
*CT scan of the chest*
- A CT scan of the chest would be useful to look for complications such as **septic emboli in the lungs** or other pulmonary pathologies.
- However, it would not provide the detailed visualization of heart valves necessary to diagnose or rule out valvular vegetations characteristic of endocarditis.
*Nafcillin and piperacillin-tazobactam*
- **Nafcillin** is active against **methicillin-susceptible Staphylococcus aureus (MSSA)**, but the patient's cultures already identified **MRSA**.
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic but not a first-line treatment for MRSA infections and would not be appropriate given the identified pathogen.
*Vancomycin and gentamicin*
- The patient is already on **Vancomycin**, which is appropriate for MRSA, but adding **gentamicin** without clear indication would not be the best next step.
- While gentamicin is sometimes used as an adjunct in specific endocarditis regimens (e.g., enterococcal), the primary concern here is the lack of clinical improvement despite appropriate MRSA coverage, pointing towards a structural cardiac issue.
Infective endocarditis US Medical PG Question 8: A 42-year-old woman presents to a medical office with complaints of fatigue, weight loss, and low-grade fever for 1 week. She noticed bleeding spots on her feet this morning. The past medical history is significant for a recent dental appointment. She is a non-smoker and does not drink alcohol. She does not currently take any medications. On examination, the vital signs include temperature 37.8°C (100.0°F), blood pressure 138/90 mm Hg, respirations 21/min, and pulse 87/min. Cardiac auscultation reveals a pansystolic murmur in the mitral area with radiation to the left axilla. Laboratory studies show hemoglobin levels of 17.2 g/dL, erythrocyte sedimentation rate (ESR) of 25 mm/h, and a white blood cell (WBC) count of 12,000 cells/mm3. An echocardiogram reveals valvular vegetations on the mitral valve with mild regurgitation. Blood samples are sent for bacterial culture. Empiric antibiotic therapy is initiated with ceftriaxone and vancomycin. The blood cultures most likely will yield the growth of which of the following organisms?
- A. Actinomyces israelii
- B. Coxiella burnetii
- C. Group B Streptococcus
- D. Staphylococcus aureus
- E. Streptococcus viridans (Correct Answer)
Infective endocarditis Explanation: ***Streptococcus viridans***
- The patient's recent **dental appointment**, the presence of an **oral organism**, and symptoms consistent with **subacute bacterial endocarditis** (fatigue, fever, weight loss, petechiae) strongly suggest *S. viridans* as the causative agent.
- *Streptococcus viridans* species are common inhabitants of the **oral flora** and are a leading cause of endocarditis following dental procedures, especially in individuals with pre-existing valvular abnormalities.
*Actinomyces israelii*
- While *Actinomyces israelii* is an oral commensal, it typically causes **actinomycosis**, a chronic, suppurative infection characterized by abscess formation and sinus tracts, often following dental procedures.
- It less commonly presents as acute or subacute endocarditis and would not typically cause the rapid progression of symptoms described.
*Coxiella burnetii*
- *Coxiella burnetii* causes **Q fever**, which can manifest as endocarditis, often associated with exposure to **farm animals** or their products.
- The patient's history lacks any such exposure, and the clinical presentation is more aligned with standard bacterial endocarditis from oral flora.
*Group B Streptococcus*
- **Group B Streptococcus** (*Streptococcus agalactiae*) is primarily known as a cause of **neonatal sepsis** and meningitis, and infections in immunocompromised adults or those with underlying conditions like diabetes.
- It is not typically associated with endocarditis following a dental procedure in an otherwise healthy adult.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause endocarditis, particularly in **intravenous drug users** or patients with prosthetic valves/indwelling lines, and often presents as a more **acute and aggressive disease**.
- While possible, the association with a recent dental procedure and the subacute course makes *Streptococcus viridans* a more likely culprit in this specific scenario.
Infective endocarditis US Medical PG Question 9: A 54-year-old man is brought to the emergency department 1 hour after an episode of loss of consciousness that lasted 3 minutes. Since awakening, he has had weakness of the left arm and leg, and his speech has been slurred. He has had a fever for 10 days. He has not had vomiting or headache. He was treated for bacterial sinusitis 3 weeks ago with amoxicillin-clavulanate. He has hypertension, hypothyroidism, hyperlipidemia, and type 2 diabetes mellitus. Current medications include amlodipine, hydrochlorothiazide, metformin, simvastatin, aspirin, and levothyroxine. His temperature is 38.6°C (101.4°F), pulse is 106/min, and blood pressure is 160/90 mm Hg. He is alert and oriented to person, place, and time. Examination shows multiple petechiae on his trunk and painless macules over both palms. A new grade 3/6 systolic murmur is heard best at the apex. He follows commands, but he slurs his words and has difficulty naming common objects. There is left facial droop. Muscle strength is 4/5 in the left upper and lower extremities. Deep tendon reflexes are 3+ on the left side and 2+ on the right side. The left big toe shows an extensor response. Fundoscopic examination shows retinal hemorrhages with white centers. Laboratory studies show:
Hemoglobin 15.3 g/dL
Leukocyte count 12,300/mm3
Serum
Na+ 136 mEq/L
Cl- 103 mEq/L
K+ 4.3 mEq/L
Glucose 108 mg/dL
Creatinine 1.1 mg/dL
Urine
Protein 1+
Glucose negative
Blood 1+
WBC 1–2/hpf
RBC 7–10/hpf
Which of the following is the most likely cause of these findings?
- A. Temporal encephalitis
- B. Contiguous spread of infection
- C. Todd's paralysis
- D. Ruptured saccular aneurysm
- E. Septic emboli (Correct Answer)
Infective endocarditis Explanation: ***Septic emboli***
* The constellation of symptoms including **fever**, a **new cardiac murmur**, **petechiae**, **Janeway lesions** (painless macules on palms), **Roth spots** (retinal hemorrhages with white centers), and neurologic deficits (left-sided weakness, slurred speech, aphasia) strongly points towards **infective endocarditis** with subsequent **septic embolization**.
* The neurologic deficits are consistent with an **embolic stroke** originating from vegetations on an infected heart valve, showering emboli to the brain.
*Temporal encephalitis*
* While **fever** and **neurologic deficits** can be seen, **temporal encephalitis** typically presents with **seizures**, **altered mental status**, and *specific abnormalities on MRI*, which are not the primary or most distinguishing features here.
* The presence of **peripheral embolic phenomena** like petechiae, Janeway lesions, and Roth spots is not characteristic of primary encephalitis.
*Contiguous spread of infection*
* Although the patient had **bacterial sinusitis** 3 weeks prior, and intracranial complications can arise from contiguous spread, this mechanism would typically lead to conditions like **brain abscess** or **meningitis**, which usually present with different clinical findings such as headache, focal neurological signs progressing over time, or distinct CSF changes.
* The sudden onset of neurological deficits following a transient loss of consciousness, combined with widespread embolic signs, makes a **septic embolic event** much more likely than direct extension from sinusitis.
*Todd's paralysis*
* **Todd's paralysis** refers to a **post-ictal focal weakness** following a **seizure**. While the patient had a 3-minute loss of consciousness, which could represent a seizure, the **systemic signs of infection** and **embolism** (fever, new murmur, petechiae, Janeway lesions, Roth spots) are not explained by Todd's paralysis alone.
* Furthermore, the continued presence of neurological deficits along with the other findings suggests an underlying process other than a transient post-ictal state.
*Ruptured saccular aneurysm*
* A **ruptured saccular aneurysm** typically causes a **sudden, severe headache** (thunderclap headache), **nuchal rigidity**, and often **rapidly declining consciousness** due to **subarachnoid hemorrhage**.
* Although focal neurological deficits can occur, the absence of severe headache, nuchal rigidity, and the presence of widespread signs of **infective endocarditis** make an aneurysm rupture an unlikely primary diagnosis.
Infective endocarditis US Medical PG Question 10: A 65-year-old man presents to the emergency department with a fever and weakness. He states his symptoms started yesterday and have been gradually worsening. The patient has a past medical history of obesity, diabetes, alcohol abuse, as well as a 30 pack-year smoking history. He lives in a nursing home and has presented multiple times in the past for ulcers and delirium. His temperature is 103°F (39.4°C), blood pressure is 122/88 mmHg, pulse is 129/min, respirations are 24/min, and oxygen saturation is 99% on room air. Physical exam is notable for a murmur. The patient is started on vancomycin and piperacillin-tazobactam and is admitted to the medicine floor. During his hospital stay, blood cultures grow Streptococcus bovis and his antibiotics are appropriately altered. A transesophageal echocardiograph is within normal limits. The patient’s fever decreases and his symptoms improve. Which of the following is also necessary in this patient?
- A. Addiction medicine referral
- B. Colonoscopy (Correct Answer)
- C. Social work consult for elder abuse
- D. Repeat blood cultures for contamination concern
- E. Replace the patient’s central line and repeat echocardiography
Infective endocarditis Explanation: ***Colonoscopy***
- The isolation of **_Streptococcus bovis_** (now often referred to as _Streptococcus gallolyticus_) from blood cultures is highly associated with **colorectal neoplasms** or other gastrointestinal pathologies.
- A comprehensive workup, including a **colonoscopy**, is crucial to identify the underlying source of bacteremia and screen for malignancy.
*Addiction medicine referral*
- While the patient has a history of **alcohol abuse**, there is no indication that his current presentation or the discovery of _Streptococcus bovis_ necessitates an immediate addiction medicine referral as the primary next step from an acute management perspective.
- Addiction management is an important long-term consideration but not the most pressing diagnostic need.
*Social work consult for elder abuse*
- The patient lives in a **nursing home** and has a history of delirium and frequent hospitalizations for ulcers, which can be concerning. However, there are no specific signs or symptoms presented in this vignette that directly suggest elder abuse as the reason for his current _S. bovis_ bacteremia, making it a less immediate priority compared to diagnosing the source of infection.
- While a general social work assessment might be beneficial for a vulnerable patient in a nursing home, it is not the most necessary intervention based on the microbiological finding.
*Repeat blood cultures for contamination concern*
- The question states that **_Streptococcus bovis_** blood cultures "grew" and antibiotics were "appropriately altered," suggesting a confirmed infection rather than contamination.
- Furthermore, _S. bovis_ is a known pathogen with specific associations and is not typically considered a common contaminant in the same vein as coagulase-negative staphylococci.
*Replace the patient’s central line and repeat echocardiography*
- The patient's **transesophageal echocardiogram (TEE) was normal**, ruling out endocarditis as the source of bacteremia in this case.
- There is no mention of a central line, and even if there were, the normal TEE and the specific pathogen (_S. bovis_) point towards a gastrointestinal source.
More Infective endocarditis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.