Central nervous system infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Central nervous system infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Central nervous system infections US Medical PG Question 1: A 10-year-old boy is brought to the emergency department by his parents because of a dull persistent headache beginning that morning. He has nausea and has vomited twice. During the past four days, the patient has had left-sided ear pain and fever, but his parents did not seek medical attention. He is from Thailand and is visiting his relatives in the United States for the summer. There is no personal or family history of serious illness. He is at the 45th percentile for height and 40th percentile for weight. He appears irritable. His temperature is 38.5°C (101.3°F), pulse is 110/min, and blood pressure is 98/58 mm Hg. The pupils are equal and reactive to light. Lateral gaze of the left eye is limited. The left tympanic membrane is erythematous with purulent discharge. There is no nuchal rigidity. Which of the following is the most appropriate next step in management?
- A. Intravenous ceftriaxone and clindamycin therapy
- B. Lumbar puncture
- C. MRI of the brain (Correct Answer)
- D. Intravenous cefazolin and metronidazole therapy
- E. Cranial burr hole evacuation
Central nervous system infections Explanation: ***MRI of the brain***
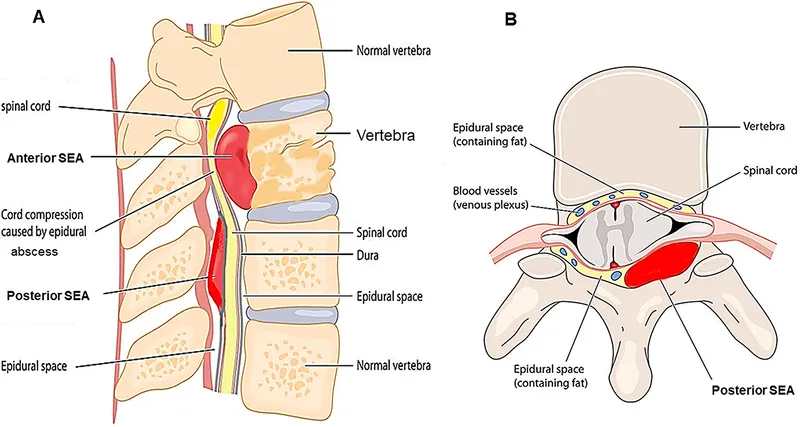
- The patient's presentation with **headache**, **nausea**, **vomiting**, recent **ear infection** (otitis media), **fever**, and **abducens nerve palsy** (limited lateral gaze of the left eye) is highly suggestive of an intracranial complication, such as a **brain abscess** or **epidural abscess**, secondary to the uncontrolled otitis media.
- An MRI of the brain is the **most sensitive and specific imaging modality** for detecting intracranial abscesses, which are critical to diagnose promptly due to their potential for surgical drainage and targeted antibiotic therapy.
*Intravenous ceftriaxone and clindamycin therapy*
- While broad-spectrum antibiotics are necessary, they should be initiated **after establishing a definitive diagnosis and ruling out conditions requiring immediate surgical intervention**.
- Without imaging, there's a risk of delaying crucial surgical management for a contained abscess or empyema.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the presence of focal neurological deficits (like **abducens nerve palsy**) and symptoms of **increased intracranial pressure** (headache, nausea, vomiting), as it carries a significant risk of **herniation** if there's a mass lesion.
- Imaging should always precede LP in such cases.
*Intravenous cefazolin and metronidazole therapy*
- Cefazolin has **poor penetration into the CNS**, making it an inadequate choice for suspected intracranial infection.
- While metronidazole targets anaerobes common in brain abscesses, the overall regimen is not optimal, and imaging is still the priority.
*Cranial burr hole evacuation*
- This is a definitive surgical treatment for a brain abscess but should only be performed **after the abscess has been localized and characterized by imaging**.
- Performing a burr hole without prior imaging would be a blind procedure and is not the appropriate next step in diagnosis and management.
Central nervous system infections US Medical PG Question 2: A 15-year-old boy is brought to the Emergency department by ambulance from school. He started the day with some body aches and joint pain but then had several episodes of vomiting and started complaining of a terrible headache. The school nurse called for emergency services. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Past medical history is noncontributory. He is a good student and enjoys sports. At the hospital, his blood pressure is 120/80 mm Hg, heart rate is 105/min, respiratory rate is 21/min, and his temperature is 38.9°C (102.0°F). On physical exam, he appears drowsy with neck stiffness and sensitivity to light. Kernig’s sign is positive. An ophthalmic exam is performed followed by a lumbar puncture. An aliquot of cerebrospinal fluid is sent to microbiology. A gram stain shows gram-negative diplococci. A smear is prepared on blood agar and grows round, smooth, convex colonies with clearly defined edges. Which of the following would identify the described pathogen?
- A. Oxidase-positive and ferments glucose and maltose (Correct Answer)
- B. Oxidase-positive test and ferments glucose only
- C. Catalase-negative and oxidase-positive
- D. No growth on Thayer-Martin medium
- E. Growth in anaerobic conditions
Central nervous system infections Explanation: ***Oxidase-positive and ferments glucose and maltose***
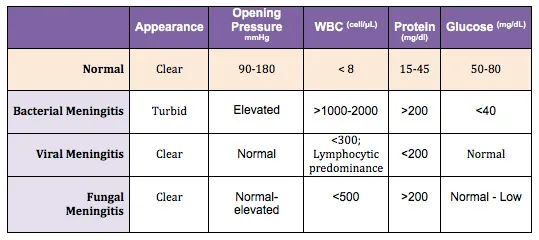
- The patient's symptoms (fever, headache, neck stiffness, sensitivity to light, positive Kernig's sign) are classic for **meningitis**, and the CSF showing **gram-negative diplococci** points to *Neisseria meningitidis*.
- *Neisseria meningitidis* is identified by its positive **oxidase test** and its ability to ferment both **glucose and maltose**.
*Oxidase-positive test and ferments glucose only*
- This description corresponds to *Neisseria gonorrhoeae*, which primarily causes **gonorrhea** and occasionally meningitis due to disseminated infection but is less common in this age group and presentation.
- While *Neisseria gonorrhoeae* is also an **oxidase-positive gram-negative diplococcus**, it specifically ferments only *glucose*, not maltose.
*Catalase-negative and oxidase-positive*
- While *Neisseria meningitidis* is **oxidase-positive**, stating it is "catalase-negative" is incorrect; *Neisseria* species are actually **catalase-positive**.
- This option incorrectly describes a general metabolic property that would rule out *Neisseria meningitidis*.
*No growth on Thayer-Martin medium*
- Thayer-Martin medium is a **selective medium** specifically designed to isolate pathogenic *Neisseria species* by inhibiting the growth of commensal bacteria and fungi.
- Therefore, *Neisseria meningitidis* would **grow well** on Thayer-Martin medium, making "no growth" an incorrect identifier.
*Growth in anaerobic conditions*
- *Neisseria meningitidis* is an **obligate aerobe**, meaning it requires oxygen for growth.
- It would **not grow** in anaerobic conditions, making this statement false for identifying the described pathogen.
Central nervous system infections US Medical PG Question 3: A 27-year-old man is brought to the emergency department by his friends in a confused state. He was doing fine 5 days ago when he started to complain of fever and flu-like symptoms. His fever was low-grade and associated with a headache. For the past 2 days, he has become increasingly irritable, confused, and was getting angry at trivial things. Past medical history is unremarkable. He is a college student and is physically active. He smokes cigarettes occasionally. He drinks alcohol socially. He is sexually active with his girlfriend and they use condoms inconsistently. Physical examination reveals: blood pressure 120/80 mm Hg, heart rate 108/min, respiratory rate 10/min, and temperature 37.4°C (99.4°F). He is confused and disoriented. Pupils are 3 mm in diameter and respond to light sluggishly. He is moving all his limbs spontaneously. His neck is supple. MRI of the brain is shown in the picture. Cerebrospinal fluid (CSF) reveals an opening pressure of 16 cm of H20, a total leukocyte count of 112/mm3 with 85% lymphocytes, the protein of 42 mg/dL, and glucose of 58 mg/dL. What is the best treatment for this condition?
- A. Intravenous immunoglobulin
- B. High-dose steroids
- C. Rituximab
- D. Acyclovir (Correct Answer)
- E. Ceftriaxone
Central nervous system infections Explanation: ***Acyclovir***
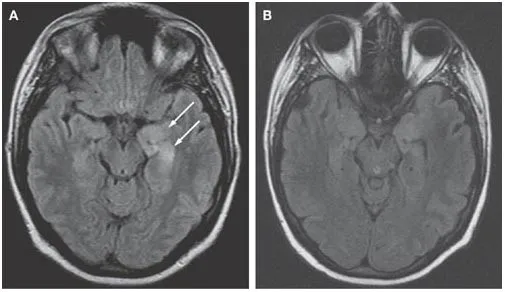
- The patient's presentation with **fever**, **flu-like symptoms** followed by **irritability**, **confusion**, and **MRI findings** suggestive of temporal lobe involvement, along with **lymphocytic pleocytosis** in CSF, is highly indicative of **herpes simplex encephalitis (HSE)**.
- **Acyclovir** is the treatment of choice for HSE, as it is an antiviral drug effective against the **herpes simplex virus (HSV)**. Prompt administration significantly improves outcomes.
*Intravenous immunoglobulin*
- **Intravenous immunoglobulin (IVIG)** is generally used for certain **immunodeficiencies** or **autoimmune conditions**, not for acute viral encephalitis like HSE.
- There is no evidence to support the use of IVIG as a primary treatment for HSV encephalitis.
*High-dose steroids*
- While steroids can reduce cerebral edema and inflammation, their routine use in **viral encephalitis** like HSE is **controversial** and not a first-line treatment.
- Steroids might be considered in specific cases of severe cerebral edema, but not as the primary antiviral therapy.
*Rituximab*
- **Rituximab** is a **monoclonal antibody** targeting **CD20-positive B cells**, primarily used in certain **lymphomas** and **autoimmune diseases** like **rheumatoid arthritis** or **multiple sclerosis**.
- It has no role in the treatment of acute viral encephalitis.
*Ceftriaxone*
- **Ceftriaxone** is a broad-spectrum **antibiotic** used to treat **bacterial meningitis** or other bacterial infections.
- It is ineffective against viral infections such as HSV encephalitis.
Central nervous system infections US Medical PG Question 4: A 26-year-old female with AIDS (CD4 count: 47) presents to the emergency department in severe pain. She states that over the past week she has been fatigued and has had a progressively worse headache and fever. These symptoms have failed to remit leading her to seek care in the ED. A lumbar puncture is performed which demonstrates an opening pressure of 285 mm H2O, increased lymphocytes, elevated protein, and decreased glucose. The emergency physician subsequently initiates treatment with IV amphotericin B and PO flucytosine. What additional treatment in the acute setting may be warranted in this patient?
- A. Serial lumbar punctures (Correct Answer)
- B. Fluconazole
- C. Mannitol
- D. Chloramphenicol
- E. Acetazolamide
Central nervous system infections Explanation: **Serial lumbar punctures**
- The elevated opening pressure (285 mm H2O) indicates **increased intracranial pressure (ICP)**, which is common in cryptococcal meningitis and can be life-threatening.
- Serial lumbar punctures can help to **reduce ICP** and relieve symptoms, improving outcomes in patients with cryptococcal meningitis.
*Fluconazole*
- Fluconazole is used for **maintenance therapy** to prevent relapse after the acute phase of cryptococcal meningitis has been controlled.
- It is generally **not recommended for initial acute treatment** in severe cases due to its fungistatic nature, making it less effective than the combination of amphotericin B and flucytosine.
*Mannitol*
- Mannitol is an **osmotic diuretic** sometimes used to acutely *reduce* ICP in cases of cerebral edema.
- While effective in some situations, it is **not the primary treatment for increased ICP** in cryptococcal meningitis, where repeated LPs are preferred to remove infected CSF and directly reduce pressure.
*Chloramphenicol*
- Chloramphenicol is an **antibiotic** primarily used to treat bacterial infections, not fungal infections.
- It has **no role in the treatment of fungal meningitis** caused by *Cryptococcus neoformans*.
*Acetazolamide*
- Acetazolamide is a **carbonic anhydrase inhibitor** that can reduce CSF production, thereby *reducing* ICP.
- While it can be used in some cases of elevated ICP, routine use in cryptococcal meningitis is **not standard practice**, and serial LPs are generally the preferred method for managing dangerously high ICP in this context due to their immediate efficacy.
Central nervous system infections US Medical PG Question 5: A 34-year-old woman presents with confusion, drowsiness, and headache. The patient’s husband says her symptoms began 2 days ago and have progressively worsened with an acute deterioration of her mental status 2 hours ago. The patient describes the headaches as severe, localized to the frontal and periorbital regions, and worse in the morning. Review of symptoms is significant for a mild, low-grade fever, fatigue, and nausea for the past week. Past medical history is significant for HIV infection for which she is not currently receiving therapy. Her CD4+ T cell count last month was 250/mm3. The blood pressure is 140/85 mm Hg, the pulse rate is 90/min, and the temperature is 37.7°C (100.0°F). On physical examination, the patient is conscious but drowsy. Papilledema is present. No pain is elicited with extension of the leg at the knee joint. The remainder of the physical examination is negative. Laboratory findings, including panculture, are ordered. A noncontrast CT scan of the head is negative and is followed by a lumbar puncture. CSF analysis is significant for:
Opening pressure 250 mm H2O (70-180 mm H2O)
Glucose 30 mg/dL (40-70 mg/dL)
Protein 100 mg/dL (<40 mg/dL)
Cell count 20/mm3 (0-5/mm3)
Which of the following additional findings would most likely be found in this patient?
- A. Gram-positive diplococci are present on microscopy
- B. CSF shows a positive acid-fast bacillus stain
- C. Multiple ring-enhancing lesions are seen on a CT scan
- D. CSF shows gram negative diplococci
- E. CSF India ink stain shows encapsulated yeast cells (Correct Answer)
Central nervous system infections Explanation: ***CSF India ink stain shows encapsulated yeast cells***
- The patient's presentation with **subacute meningitis symptoms** (headache, confusion, low-grade fever) in the setting of **untreated HIV infection** with a low CD4+ count (250/mm3) strongly suggests an opportunistic infection.
- The CSF findings of **elevated opening pressure**, **low glucose**, **high protein**, and **moderate pleocytosis** are classic for **cryptococcal meningitis**, for which the India ink stain is diagnostic for encapsulated yeast cells.
*Gram-positive diplococci are present on microscopy*
- This finding suggests **bacterial meningitis**, specifically caused by organisms like *Streptococcus pneumoniae*.
- While bacterial meningitis presents acutely with severe symptoms, the **subacute course** and moderate pleocytosis are less typical, and the patient's immune status points towards an opportunistic infection.
*CSF shows a positive acid-fast bacillus stain*
- A positive **acid-fast bacillus (AFB) stain** in CSF would indicate **tuberculous meningitis**.
- While tuberculous meningitis can present subacutely with similar CSF findings in HIV patients, it typically involves a more significant lymphocytic pleocytosis and a more pronounced chronic course than suggested by the acute worsening.
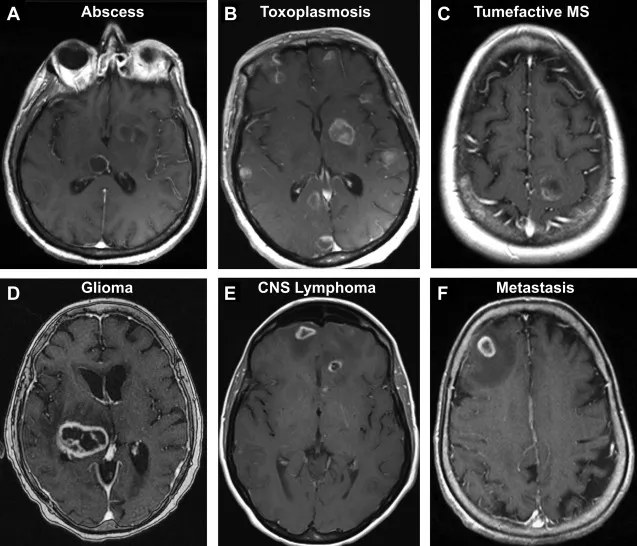
*Multiple ring-enhancing lesions are seen on a CT scan*
- **Multiple ring-enhancing lesions** on CT or MRI are characteristic of **Toxoplasma encephalopathy** or **CNS lymphoma** in HIV-positive patients.
- While these are common HIV-related CNS complications, the patient's primary presentation points to **meningitis** (inflammation of meninges with CSF abnormalities) rather than focal brain lesions without meningeal involvement.
*CSF shows gram negative diplococci*
- **Gram-negative diplococci** in CSF suggest **meningococcal meningitis** (*Neisseria meningitidis*).
- This typically presents as an **acute, severe bacterial meningitis** with rapid deterioration, usually in immunocompetent individuals or specific outbreaks, which doesn't align with the subacute onset and specific CSF profile for cryptococcus.
Central nervous system infections US Medical PG Question 6: A 42-year-old man is brought to the physician 25 minutes after an episode of violent jerky movements of his hands and legs that lasted for 5 minutes. After the episode, he had difficulty conversing. For the past 10 days, he has had a left-sided headache and nausea. Apart from a history of recurrent ear infections treated with antibiotics, he reports no other personal or family history of serious illness. He works as an assistant at a veterinarian clinic. He appears ill and is oriented to place and person only. His temperature is 37.8°C (100°F), pulse is 102/min, and blood pressure 112/78 mm Hg. Examination shows bilateral optic disc swelling. There is no lymphadenopathy. Muscle strength and tone is normal in all extremities. Deep tendon reflexes are 2+ bilaterally. Plantar reflex shows a flexor response bilaterally. Laboratory studies show a CD4 count within the reference range. An MRI of the brain is shown. Intravenous mannitol and levetiracetam are administered. Which of the following is the most appropriate next step in management?
- A. Aspiration and surgical drainage (Correct Answer)
- B. Pyrimethamine and sulfadiazine therapy
- C. Ciprofloxacin and metronidazole therapy
- D. Albendazole therapy
- E. Metronidazole and cefotaxime therapy
Central nervous system infections Explanation: ***Aspiration and surgical drainage***
- The MRI shows a **ring-enhancing lesion** with surrounding edema, consistent with a **brain abscess**, indicated by the patient's symptoms (headache, nausea, seizures, fever, optic disc swelling from increased intracranial pressure) and history of ear infections.
- Due to the size of the lesion and the associated mass effect (seizures, altered mental status, papilledema), **surgical drainage** is crucial to relieve pressure, obtain a pathogen sample for targeted antibiotic therapy, and achieve rapid improvement, especially in cases where empiric antibiotics alone may not be sufficient or the abscess is large.
*Pyrimethamine and sulfadiazine therapy*
- This regimen is the primary treatment for **Toxoplasma gondii encephalitis**, which typically occurs in immunocompromised individuals (e.g., HIV with low CD4 count).
- The patient's **CD4 count is within the reference range**, making toxoplasmosis less likely, and the MRI appearance of a single, large ring-enhancing lesion is not as typical for multifocal toxoplasmosis.
*Ciprofloxacin and metronidazole therapy*
- While metronidazole is often used for anaerobic coverage in brain abscesses, ciprofloxacin is a broad-spectrum antibiotic but not the first-line choice for typical brain abscess pathogens originating from otitis media (e.g., Strep species, anaerobes).
- **Empiric antibiotic therapy** is typically initiated, but given the significant mass effect and neurological compromise, **surgical intervention is generally prioritized alongside antibiotics** for symptomatic abscesses.
*Albendazole therapy*
- **Albendazole** is an **anti-parasitic medication** used to treat infections like neurocysticercosis, which can present with ring-enhancing lesions.
- However, the patient's history (ear infections, no travel to endemic areas for neurocysticercosis) and the imaging characteristics (single, thick-walled cavity) make a bacterial abscess more probable.
*Metronidazole and cefotaxime therapy*
- This is a common **empiric antibiotic regimen for brain abscesses**, covering both anaerobic bacteria (metronidazole) and common streptococcal species (cefotaxime, a third-generation cephalosporin).
- While appropriate as medical therapy, given the patient's **acute neurological symptoms** (seizures, altered mental status from high intracranial pressure) and the size of the abscess on MRI, **surgical aspiration and drainage** are equally, if not more, important as an initial step to reduce mass effect and obtain cultures, rather than relying solely on antibiotics.
Central nervous system infections US Medical PG Question 7: A 21-year-old G3P2 woman presents to her obstetrician at 6 weeks gestation for routine prenatal care. Her past medical history includes obesity and gestational diabetes. She has had two spontaneous vaginal deliveries at term. One infant was macrosomic with hypoglycemia, but otherwise, she has had no complications. Her physician informs her that she must start taking a multivitamin with folic acid daily. The defect that folic acid supplementation protects against arises in tissue that is derived from which germ cell layer?
- A. Mesoderm
- B. Notochord
- C. Endoderm
- D. Mesenchyme
- E. Ectoderm (Correct Answer)
Central nervous system infections Explanation: ***Ectoderm***
- Folic acid supplementation primarily prevents **neural tube defects**, such as **spina bifida** and **anencephaly**.
- The **neural tube**, which forms the brain and spinal cord, is derived from the **ectoderm**.
*Mesoderm*
- The **mesoderm** gives rise to structures like muscle, bone, connective tissue, and the cardiovascular system.
- Defects in mesodermal development are not primarily prevented by folic acid supplementation.
*Notochord*
- The **notochord** is a transient embryonic structure that induces the formation of the neural plate from the ectoderm.
- While critical for nervous system development, it is not a germ cell layer itself, and defects in its development are not directly prevented by folic acid.
*Endoderm*
- The **endoderm** forms the lining of the gastrointestinal and respiratory tracts, as well as glands like the thyroid and pancreas.
- Anomalies of these internal organs are not the primary target of folic acid supplementation.
*Mesenchyme*
- **Mesenchyme** is embryonic connective tissue, largely derived from the mesoderm, but can also come from neural crest (ectoderm).
- It differentiates into connective tissues, blood, and lymphatic vessels; neural tube defects are not considered mesenchymal in origin.
Central nervous system infections US Medical PG Question 8: A 32-year-old woman presents with a 3-month history of intermittent blurred vision and problems walking. The patient states that she often feels “pins and needles” in her legs that cause her problems when she’s walking. The patient is afebrile, and her vital signs are within normal limits. An autoimmune disorder is suspected. Which of the following findings would most likely be present in this patient?
- A. Damaged myelin sheath and myelin-producing cells (Correct Answer)
- B. Absence of interneurons
- C. Destruction of blood-brain barrier
- D. Degeneration of anterior horn cells
- E. Decreased cerebrospinal fluid due to destruction of cells
Central nervous system infections Explanation: ***Damaged myelin sheath and myelin-producing cells***
- The patient's symptoms of intermittent **blurred vision** (optic neuritis), **problems walking** (ataxia, spasticity), and **paresthesias** ("pins and needles") are classical presentations of Multiple Sclerosis (MS).
- MS is characterized by multifocal areas of inflammation and **demyelination** in the central nervous system, where the **myelin sheath** surrounding axons is damaged, and the **oligodendrocytes** (myelin-producing cells) are attacked.
- This demyelination disrupts saltatory conduction, leading to the varied and intermittent neurological symptoms.
*Absence of interneurons*
- The absence of **interneurons** is typically associated with conditions like **spinal muscular atrophy** or certain **neuropathies**, which present with different clinical features (e.g., muscle weakness, atrophy) than those described.
- While interneurons are crucial for neuronal communication, their absence doesn't explain the *intermittent* and multifocal symptoms seen in this case.
*Destruction of blood-brain barrier*
- While **blood-brain barrier (BBB) breakdown** does occur in MS, it is a *consequence* of the inflammatory process rather than the primary *pathological finding* that directly explains the neurological symptoms.
- BBB destruction allows inflammatory cells to enter the CNS, contributing to demyelination, but the core issue remains the myelin damage itself.
*Degeneration of anterior horn cells*
- **Anterior horn cell degeneration** is the hallmark of **amyotrophic lateral sclerosis (ALS)** and **spinal muscular atrophy**, presenting with progressive muscle weakness, atrophy, and fasciculations.
- These conditions lack the sensory symptoms (paresthesias) and visual disturbances seen in this patient, and typically show a progressive rather than intermittent course.
*Decreased cerebrospinal fluid due to destruction of cells*
- **Decreased CSF volume** is not a characteristic feature of MS; in fact, CSF analysis often shows increased protein and **oligoclonal bands**.
- The destruction of cells in MS primarily affects myelin and oligodendrocytes, not cells responsible for CSF production or volume regulation.
Central nervous system infections US Medical PG Question 9: A 3-year-old boy is brought to the physician for the evaluation of recurrent skin lesions. The episodes of lesions started at the age of 3 months. He has also had several episodes of respiratory tract infections, enlarged lymph nodes, and recurrent fevers since birth. The boy attends daycare. The patient's immunizations are up-to-date. He is at the 5th percentile for length and 10th percentile for weight. He appears ill. Temperature is 38°C (100.4°F). Examination shows several raised, erythematous lesions of different sizes over the face, neck, groin, and extremities; some are purulent. Bilateral cervical and axillary lymphadenopathy are present. What is the most likely underlying mechanism of this patient's symptoms?
- A. Defective cytoplasmic tyrosine kinase
- B. NADPH oxidase deficiency (Correct Answer)
- C. Impaired signaling to actin cytoskeleton reorganization
- D. Defective neutrophil chemotaxis
- E. Impaired repair of double-strand DNA breaks
Central nervous system infections Explanation: ***NADPH oxidase deficiency***
- The recurrent skin abscesses (purulent lesions), respiratory tract infections, lymphadenopathy, and fevers point to chronic granulomatous disease (CGD), which is caused by a deficiency in **NADPH oxidase**.
- **NADPH oxidase** is essential for the production of reactive oxygen species (ROS) in phagocytes, which are critical for killing catalase-positive bacteria and fungi.
*Defective cytoplasmic tyrosine kinase*
- This mechanism is associated with **X-linked agammaglobulinemia (Bruton's agammaglobulinemia)**, which primarily causes recurrent bacterial infections due to a lack of B cells and antibodies.
- While recurrent infections occur, the typical presentation involves encapsulated bacteria and lacks the widespread purulent skin lesions and lymphadenopathy seen in CGD.
*Impaired signaling to actin cytoskeleton reorganization*
- This defect is characteristic of **Wiskott-Aldrich syndrome**, leading to thrombocytopenia, eczema, and recurrent infections, particularly by encapsulated bacteria.
- The clinical picture of recurrent widespread skin abscesses and granuloma formation is not typical for Wiskott-Aldrich syndrome.
*Defective neutrophil chemotaxis*
- This can be seen in conditions like **leukocyte adhesion deficiency (LAD)** or **Chédiak-Higashi syndrome**.
- LAD presents with recurrent bacterial infections, impaired wound healing, and delayed umbilical cord separation, while Chédiak-Higashi involves partial oculocutaneous albinism and recurrent pyogenic infections, distinct from this patient's symptoms.
*Impaired repair of double-strand DNA breaks*
- This defect is associated with conditions like **ataxia-telangiectasia**, which involves cerebellar ataxia, telangiectasias, and immunodeficiency (T-cell and IgA deficiency).
- The patient's symptoms of recurrent purulent skin lesions and infections are not characteristic of the DNA repair defects seen in ataxia-telangiectasia.
Central nervous system infections US Medical PG Question 10: A 33-year-old man is brought to the emergency department 20 minutes after he fell from the roof of his house. On arrival, he is unresponsive to verbal and painful stimuli. His pulse is 72/min and blood pressure is 132/86 mm Hg. A CT scan of the head shows a fracture in the anterior cranial fossa and a 1-cm laceration in the left anterior orbital gyrus. If the patient survives, which of the following would ultimately be the most common cell type at the injured region of the frontal lobe?
- A. Microglia
- B. Oligodendrocytes
- C. Neurons
- D. Schwann cells
- E. Astrocytes (Correct Answer)
Central nervous system infections Explanation: ***Astrocytes***
- Following **neuronal injury**, astrocytes proliferate rapidly and form a **glial scar** around the damaged area to isolate it and prevent further spread of damage.
- This process, known as **astrogliosis**, leads to astrocytes becoming the most abundant cell type in the chronically injured region of the central nervous system.
*Microglia*
- **Microglia** are the brain's resident immune cells and are primarily involved in **phagocytosis** of cellular debris and pathogens after injury.
- While they are activated and proliferate early after injury, they typically do not become the most common cell type in the *chronically injured* region.
*Oligodendrocytes*
- **Oligodendrocytes** are responsible for forming the **myelin sheath** around axons in the central nervous system.
- They are often damaged during acute brain injury and do not typically proliferate to become the most common cell type in the scar tissue.
*Neurons*
- **Neurons** are the primary cells affected by acute brain injury, and many are irrecoverably lost at the site of trauma.
- The adult central nervous system has very limited capacity for neurogenesis, so neurons do not regenerate or become the most common cell type after injury.
*Schwann cells*
- **Schwann cells** are responsible for myelinating axons in the **peripheral nervous system (PNS)**.
- They are not found in the central nervous system (CNS) region of brain injury and therefore would not be involved in the repair or scarring process there.
More Central nervous system infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.