Antimicrobial stewardship US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimicrobial stewardship. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimicrobial stewardship US Medical PG Question 1: A previously healthy 35-year-old woman is brought into the emergency department after being found unresponsive by her husband. Her husband finds an empty bottle of diazepam tablets in her pocket. She is stuporous. At the hospital, her blood pressure is 90/40 mm Hg, the pulse is 58/min, and the respirations are 6/min. The examination of the pupils shows normal size and reactivity to light. Deep tendon reflexes are 1+ bilaterally. Babinski sign is absent. All 4 extremities are hypotonic. The patient is intubated and taken to the critical care unit for mechanical ventilation and treatment. Regarding the prevention of pneumonia in this patient, which of the following strategies is most likely to achieve this goal?
- A. Nasogastric tube insertion
- B. Daily evaluation for ventilator weaning
- C. Subglottic drainage of secretions (Correct Answer)
- D. Oropharynx and gut antibacterial decontamination
- E. Prone positioning during mechanical ventilation
Antimicrobial stewardship Explanation: ***Subglottic drainage of secretions***
- This is a highly effective strategy to prevent **ventilator-associated pneumonia (VAP)** by continuously removing secretions that pool above the endotracheal tube cuff before they can be aspirated.
- Endotracheal tubes with a **subglottic secretion drainage port** reduce VAP incidence by preventing microaspiration of contaminated oropharyngeal secretions into the lower respiratory tract.
- This is a **specific mechanical intervention** that directly addresses one of the key pathogenic mechanisms of VAP.
*Nasogastric tube insertion*
- While an NG tube may be needed for feeding or gastric decompression, it does not directly prevent VAP and may **increase aspiration risk** by compromising the lower esophageal sphincter.
- NG tubes can promote gastroesophageal reflux and provide a conduit for bacterial migration.
*Daily evaluation for ventilator weaning*
- This is also a **critical component of VAP prevention** as part of the ventilator bundle, since reducing duration of mechanical ventilation is the most effective overall strategy to prevent VAP.
- However, in this question asking for a strategy to prevent pneumonia in an intubated patient, subglottic drainage is the more specific technical intervention, whereas daily weaning assessment is a broader protocol that reduces exposure time.
- Both strategies are important; subglottic drainage addresses the "how" of prevention during intubation, while weaning protocols address the "duration" of risk exposure.
*Oropharynx and gut antibacterial decontamination*
- Selective digestive decontamination (SDD) aims to reduce bacterial colonization, but evidence for routine use is mixed and raises concerns about **antimicrobial resistance**.
- Not universally recommended as a primary VAP prevention strategy in most guidelines.
*Prone positioning during mechanical ventilation*
- **Prone positioning** is primarily indicated for improving oxygenation in **Acute Respiratory Distress Syndrome (ARDS)**, not for VAP prevention.
- While it may improve secretion drainage, it is not a standard VAP prevention measure and carries its own risks and logistical challenges.
Antimicrobial stewardship US Medical PG Question 2: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
Antimicrobial stewardship Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
Antimicrobial stewardship US Medical PG Question 3: A 37-year-old man with a history of IV drug use presents to the ED with complaints of fevers, chills, and malaise for one week. He admits to recently using IV and intramuscular heroin. Vital signs are as follows: T 40.0 C, HR 120 bpm, BP 110/68 mmHg, RR 14, O2Sat 98%. Examination reveals a new systolic murmur that is loudest at the lower left sternal border. Initial management includes administration of which of the following regimens?
- A. IV Vancomycin, IV ceftriaxone, IV fluconazole
- B. IV Vancomycin, IV ceftriaxone (Correct Answer)
- C. IV Vancomycin, IV levofloxacin
- D. IV Vancomycin
- E. IV Vancomycin, IV gentamicin, PO rifampin
Antimicrobial stewardship Explanation: ***IV Vancomycin, IV ceftriaxone***
- The patient's history of **IV drug use**, fevers, chills, new systolic murmur, and likely **tricuspid valve involvement** (murmur loudest at the lower left sternal border) strongly suggest **infective endocarditis**.
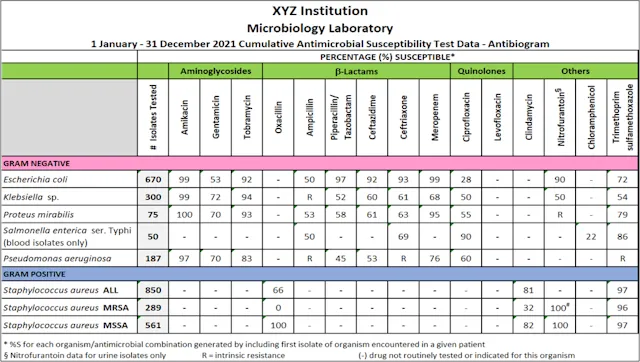
- The empiric regimen for suspected endocarditis in an IV drug user should cover **methicillin-resistant _Staphylococcus aureus_ (MRSA)** with **vancomycin** and gram-negative organisms with a **third-generation cephalosporin** like **ceftriaxone**.
- This combination provides broad coverage for the most common pathogens in native valve endocarditis among IV drug users, including MRSA, streptococci, and many gram-negative organisms.
*IV Vancomycin, IV ceftriaxone, IV fluconazole*
- While vancomycin and ceftriaxone are appropriate, **fluconazole** is an antifungal and is generally not indicated for empiric treatment of bacterial endocarditis unless there's a strong suspicion of **fungal infection**.
- Fungal endocarditis is less common and usually requires prolonged treatment with specific antifungals, often alongside surgical intervention.
*IV Vancomycin, IV levofloxacin*
- **Levofloxacin** is a fluoroquinolone that covers a broad spectrum of bacteria but is not the preferred empiric agent for gram-negative coverage in suspected endocarditis in IV drug users due to concerns about resistance and lack of superior coverage compared to third-generation cephalosporins.
- **Ceftriaxone** provides better coverage for common gram-negative pathogens associated with endocarditis among IV drug users in this context.
*IV Vancomycin, IV gentamicin, PO rifampin*
- **Gentamicin** is an aminoglycoside that provides effective gram-negative coverage and is often used in combination therapy for endocarditis, but **rifampin** is typically reserved for prosthetic valve endocarditis or refractory cases due to its risk of drug interactions and resistance development.
- **Oral rifampin** may not be appropriate for initial aggressive treatment in an acutely ill patient with suspected acute endocarditis, where IV therapy is preferred.
*IV Vancomycin*
- While **vancomycin** is crucial for covering **MRSA** which is common in IV drug users, it alone does not provide adequate coverage for potential **gram-negative pathogens** that can also cause endocarditis in this population.
- **Multidrug empiric therapy** is essential to cover a broad range of likely pathogens causing endocarditis in IV drug users, especially with severe symptoms.
Antimicrobial stewardship US Medical PG Question 4: A 42-year-old woman with a history of multiple sclerosis and recurrent urinary tract infections comes to the emergency department because of flank pain and fever. Her temperature is 38.8°C (101.8°F). Examination shows left-sided costovertebral angle tenderness. She is admitted to the hospital and started on intravenous vancomycin. Three days later, her symptoms have not improved. Urine culture shows growth of Enterococcus faecalis. Which of the following best describes the most likely mechanism of antibiotic resistance in this patient?
- A. Increased efflux across bacterial cell membranes
- B. Production of beta-lactamase
- C. Alteration of penicillin-binding proteins
- D. Alteration of peptidoglycan synthesis (Correct Answer)
- E. Alteration of ribosomal targets
Antimicrobial stewardship Explanation: ***Alteration of peptidoglycan synthesis***
- **Vancomycin** targets the **D-Ala-D-Ala terminus** on the peptidoglycan precursor, preventing cross-linking during bacterial cell wall synthesis.
- **Vancomycin resistance in Enterococcus faecalis** occurs through acquisition of resistance genes (vanA, vanB) that encode enzymes modifying the peptidoglycan precursor from **D-Ala-D-Ala to D-Ala-D-Lac**.
- This structural change reduces vancomycin's binding affinity by approximately 1000-fold, rendering the antibiotic ineffective.
- The mechanism directly involves **alteration of the peptidoglycan synthesis pathway**, specifically the terminal amino acid residues of the pentapeptide precursor.
*Increased efflux across bacterial cell membranes*
- This mechanism involves **efflux pumps that actively transport antibiotics out of the bacterial cell**, reducing intracellular concentration.
- While efflux pumps contribute to resistance for antibiotics like **tetracyclines, fluoroquinolones, and macrolides**, this is not the primary mechanism of vancomycin resistance in Enterococcus.
*Production of beta-lactamase*
- **Beta-lactamase enzymes** hydrolyze the **beta-lactam ring** of antibiotics like **penicillins and cephalosporins**, rendering them inactive.
- **Vancomycin is a glycopeptide antibiotic, not a beta-lactam**, so its efficacy is not affected by beta-lactamase production.
*Alteration of ribosomal targets*
- This mechanism confers resistance to antibiotics that target **bacterial ribosomes** to inhibit protein synthesis, such as **macrolides, aminoglycosides, and tetracyclines**.
- **Vancomycin acts on cell wall synthesis**, not protein synthesis, so alteration of ribosomal targets is not relevant to vancomycin resistance.
*Alteration of penicillin-binding proteins*
- **Penicillin-binding proteins (PBPs)** are the targets of **beta-lactam antibiotics** (penicillins, cephalosporins, carbapenems).
- Alterations in PBPs cause resistance to beta-lactams, not to vancomycin.
- **Vancomycin does not interact with PBPs**; it binds directly to the D-Ala-D-Ala terminus of peptidoglycan precursors in the cell wall.
Antimicrobial stewardship US Medical PG Question 5: A 27-year-old man presents to the emergency department for altered mental status. The patient was found napping in a local market and brought to the hospital. The patient has a past medical history of polysubstance abuse and is homeless. His temperature is 104°F (40.0°C), blood pressure is 100/52 mmHg, pulse is 133/min, respirations are 25/min, and oxygen saturation is 99% on room air. Physical exam is notable for an altered man. Cardiopulmonary exam reveals a murmur over the left lower sternal border. A bedside ultrasound reveals a vegetation on the tricuspid valve. The patient is ultimately started on IV fluids, norepinephrine, vasopressin, vancomycin, and piperacillin-tazobactam. A central line is immediately placed in the internal jugular vein and the femoral vein secondary to poor IV access. Cardiothoracic surgery subsequently intervenes to remove the vegetation. While recovering in the ICU, days 3-5 are notable for an improvement in the patient’s symptoms. Two additional peripheral IVs are placed while in the ICU on day 5, and the femoral line is removed. On day 6, the patient's fever and hemodynamic status worsen. Though he is currently responding and not complaining of any symptoms including headache, photophobia, neck stiffness, or pain, he states he is feeling weak. Jolt accentuation of headache is negative and his abdominal exam is benign. A chest radiograph, urinalysis, and echocardiogram are unremarkable though the patient’s blood cultures are positive when drawn. Which of the following is the best next step in management?
- A. Add micafungin to the patient’s antibiotics
- B. Perform a lumbar puncture
- C. Remove all peripheral IV’s and send for cultures
- D. Add cefepime to the patient’s antibiotics
- E. Remove the central line and send for cultures (Correct Answer)
Antimicrobial stewardship Explanation: **Correct: Remove the central line and send for cultures**
- The patient's worsening fever and hemodynamic instability on day 6, despite initial improvement, raise suspicion for a **catheter-related bloodstream infection (CRBSI)**, especially given the history of central line placement.
- **Prompt removal of the catheter** and sending the tip for culture is crucial for diagnosis and treatment of potential CRBSI, as the source of infection often resides within the biofilm on the catheter.
*Incorrect: Remove all peripheral IV's and send for cultures*
- While **peripheral IVs** can be a source of infection, the central line was placed earlier and is associated with a much higher risk of serious infection, especially in a critically ill patient.
- The patient's initial improvement followed by deterioration points more towards a **central line-associated infection** rather than new peripheral IVs placed only on day 5.
*Incorrect: Perform a lumbar puncture*
- Although the patient has altered mental status, the absence of focal neurological deficits, headache, photophobia, and neck stiffness, along with a negative **Jolt accentuation of headache**, makes **meningitis** less likely as the primary cause of deterioration.
- The more immediate and likely cause of worsening sepsis in this context is a **catheter-related infection**.
*Incorrect: Add micafungin to the patient's antibiotics*
- Adding an antifungal agent such as **micafungin** would be considered if there was a strong suspicion of a fungal infection, which is not indicated by the current blood cultures or clinical picture.
- Empiric antifungal therapy is typically reserved for patients with persistent fever refractory to broad-spectrum antibiotics, known fungal exposure, or specific risk factors.
*Incorrect: Add cefepime to the patient's antibiotics*
- The patient is already on **vancomycin and piperacillin-tazobactam**, which provides broad-spectrum coverage for both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*.
- Adding **cefepime** would broaden gram-negative coverage further but is usually unnecessary unless the current regimen is failing due to specific resistant organisms, and the more likely source of infection should be addressed first.
Antimicrobial stewardship US Medical PG Question 6: A 59-year-old woman comes to the emergency department because of a 2-day history of worsening fever, chills, malaise, productive cough, and difficulty breathing. Three days ago, she returned from a trip to South Africa. She has type 2 diabetes mellitus, hypertension, and varicose veins. Her current medications include metformin, lisinopril, and atorvastatin. Her temperature is 39.4°C (102.9°F), pulse is 102/minute, blood pressure is 94/68 mm Hg, and respirations are 31/minute. Pulse oximetry on 2 L of oxygen via nasal cannula shows an oxygen saturation of 91%. Examination reveals decreased breath sounds and dull percussion over the left lung base. The skin is very warm and well-perfused. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.6 g/dL
Leukocyte count 15,400/mm3
platelet count 282,000/mm3
Serum
Na+ 144 mEq/L
Cl- 104 mEq/L
K+ 4.9 mEq/L
Creatinine 1.5 mg/dL
Blood and urine for cultures are obtained. Intravenous fluid resuscitation is begun. Which of the following is the next best step in management?
- A. Erythromycin
- B. Intravenous ceftriaxone and azithromycin (Correct Answer)
- C. External cooling and intravenous acetaminophen
- D. Intravenous vancomycin and ceftriaxone
- E. CT of the chest with contrast
Antimicrobial stewardship Explanation: ***Intravenous ceftriaxone and azithromycin***
* This patient presents with **severe community-acquired pneumonia (CAP)** meeting criteria for ICU-level care, including hypotension (94/68 mm Hg), hypoxemia requiring supplemental oxygen, tachypnea (31/min), and altered mental status indicators. The presentation meets multiple **severe CAP criteria** (CURB-65 score ≥3 or IDSA/ATS major criteria).
* **Intravenous ceftriaxone** (a third-generation cephalosporin) provides broad-spectrum coverage against common bacterial causes of CAP, including *Streptococcus pneumoniae* and *Haemophilus influenzae*. **Azithromycin** (a macrolide) is crucial to cover atypical pathogens like *Mycoplasma pneumoniae*, *Chlamydophila pneumoniae*, and *Legionella pneumoniae*.
* This combination represents the **standard empiric therapy for severe CAP** per IDSA/ATS guidelines. The patient's recent travel to South Africa and severe symptoms increase the likelihood of atypical pathogens or resistant strains, making dual therapy essential.
*Erythromycin*
* While erythromycin is a macrolide that covers atypical pathogens, its use is generally limited due to higher rates of gastrointestinal side effects and a less favorable dosing profile compared to newer macrolides like azithromycin. It does not provide adequate coverage for typical bacterial causes of CAP.
* In severe CAP with signs of sepsis, monotherapy with erythromycin would be insufficient and would not address the need for broad-spectrum coverage against both typical and atypical bacteria. Dual antibiotic therapy is required for severe cases.
*External cooling and intravenous acetaminophen*
* These interventions are appropriate for **fever reduction** but do not address the underlying severe infection (pneumonia with sepsis). While important for symptomatic relief, they are not the "next best step in management" for a life-threatening condition.
* Treating the infection with appropriate antibiotics is paramount to prevent further deterioration and organ damage. In severe sepsis from pneumonia, **source control through antimicrobial therapy takes precedence** over symptomatic fever management.
*Intravenous vancomycin and ceftriaxone*
* **Vancomycin** is primarily used to cover **methicillin-resistant *Staphylococcus aureus* (MRSA)**. While MRSA can cause severe pneumonia, there are no specific risk factors for MRSA in this patient (e.g., recent hospitalization, IV drug use, prior MRSA infection, severe influenza, cavitary lesions, hemoptysis).
* Adding vancomycin without specific indications for MRSA coverage would represent unnecessary broad-spectrum antibiotic use and could contribute to antibiotic resistance. The combination of **ceftriaxone and azithromycin is the standard empiric therapy** for severe CAP without MRSA risk factors.
*CT of the chest with contrast*
* A CT scan of the chest might be useful for further characterizing the pneumonia, identifying complications (e.g., empyema, abscess), or differentiating from other conditions **after initial stabilization**. However, in a patient with severe pneumonia, hypoxemia, and hypotension, the immediate priority is stabilization and initiation of empiric antibiotic therapy.
* Delaying life-saving antibiotic treatment to obtain a CT scan could worsen the patient's prognosis and violate the principle of **early appropriate antibiotics in sepsis** (ideally within 1 hour). Clinical diagnosis with chest X-ray is sufficient to initiate treatment, and further imaging can be obtained after stabilization if needed.
Antimicrobial stewardship US Medical PG Question 7: A 37-year-old man presents to the emergency department for a persistent fever. The patient states he has felt unwell for the past week and has felt subjectively febrile. The patient has a past medical history of a suicide attempt and alcohol abuse. He is not currently taking any medications. The patient admits to using heroin and cocaine and drinking 5-8 alcoholic drinks per day. His temperature is 103°F (39.4°C), blood pressure is 92/59 mmHg, pulse is 110/min, respirations are 20/min, and oxygen saturation is 96% on room air. Cardiopulmonary exam is notable for a systolic murmur heard best along the left sternal border. Dermatologic exam reveals scarring in the antecubital fossa. Which of the following is the next best step in management?
- A. CT scan
- B. Ultrasound
- C. Chest radiograph
- D. Blood cultures (Correct Answer)
- E. Vancomycin and gentamicin
Antimicrobial stewardship Explanation: ***Blood cultures***
- The patient's history of **intravenous drug use (IVDU)**, persistent fever, and a **new systolic murmur** strongly suggest **infective endocarditis**.
- **Blood cultures** are crucial for identifying the causative organism and guiding appropriate antibiotic therapy, serving as the cornerstone of diagnosis in suspected endocarditis.
*CT scan*
- While CT scans can be useful for identifying complications of endocarditis (e.g., septic emboli in the brain or lungs), they are **not the initial diagnostic step** for identifying the source of infection.
- CT scans expose the patient to **radiation** and are more expensive, making them less suitable as a first step compared to blood cultures.
*Ultrasound*
- An **echocardiogram** (a type of ultrasound) is essential for visualizing vegetations on heart valves, but it is typically performed *after* blood cultures reveal bacteremia to confirm the diagnosis and assess severity.
- A general ultrasound of other body areas would be non-specific and **unlikely to pinpoint the cause** of persistent fever in this clinical context.
*Chest radiograph*
- A chest radiograph can identify **pulmonary infiltrates** or **septic emboli in the lungs**, which are potential complications of right-sided endocarditis (common in IVDU).
- However, a chest radiograph **does not identify the causative organism** or confirm the primary diagnosis of endocarditis, making it a secondary investigation.
*Vancomycin and gentamicin*
- This combination represents a broad-spectrum antibiotic regimen often used for **empiric treatment of infective endocarditis**, particularly in IVDU patients due to concerns for MRSA or resistant streptococcal species.
- While ultimately necessary, administering antibiotics *before* obtaining **blood cultures** can significantly reduce the yield of cultures and hinder definitive diagnosis and tailored treatment.
Antimicrobial stewardship US Medical PG Question 8: In a randomized controlled trial studying a new treatment, the primary endpoint (mortality) occurred in 14.4% of the treatment group and 16.7% of the control group. Which of the following represents the number of patients needed to treat to save one life, based on the primary endpoint?
- A. 1/(0.144 - 0.167)
- B. 1/(0.167 - 0.144) (Correct Answer)
- C. 1/(0.300 - 0.267)
- D. 1/(0.267 - 0.300)
- E. 1/(0.136 - 0.118)
Antimicrobial stewardship Explanation: ***1/(0.167 - 0.144)***
- The **Number Needed to Treat (NNT)** is calculated as **1 / Absolute Risk Reduction (ARR)**.
- The **Absolute Risk Reduction (ARR)** is the difference between the event rate in the control group (16.7%) and the event rate in the treatment group (14.4%), which is **0.167 - 0.144**.
*1/(0.144 - 0.167)*
- This calculation represents 1 divided by the **Absolute Risk Increase**, which would be relevant if the treatment increased mortality.
- The **NNT should always be a positive value**, indicating the number of patients to treat to prevent one adverse event.
*1/(0.300 - 0.267)*
- This option uses arbitrary numbers (0.300 and 0.267) that do not correspond to the given **mortality rates** in the problem.
- It does not reflect the correct calculation for **absolute risk reduction** based on the provided data.
*1/(0.267 - 0.300)*
- This option also uses arbitrary numbers not derived from the problem's data, and it would result in a **negative value** for the denominator.
- The difference between event rates of 0.267 and 0.300 is not present in the given information for this study.
*1/(0.136 - 0.118)*
- This calculation uses arbitrary numbers (0.136 and 0.118) that are not consistent with the reported **mortality rates** of 14.4% and 16.7%.
- These values do not represent the **Absolute Risk Reduction** required for calculating NNT in this specific scenario.
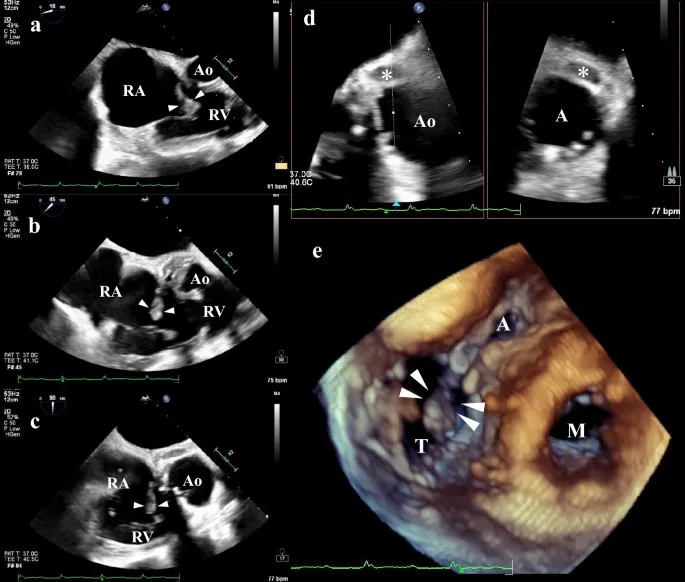
Antimicrobial stewardship US Medical PG Question 9: A 50-year-old man with a history of stage 4 kidney disease was admitted to the hospital for an elective hemicolectomy. His past medical history is significant for severe diverticulitis. After the procedure he becomes septic and was placed on broad spectrum antibiotics. On morning rounds, he appear weak and complains of fatigue and nausea. His words are soft and he has difficulty answering questions. His temperature is 38.9°C (102.1°F), heart rate is 110/min, respiratory rate is 15/min, blood pressure 90/65 mm Hg, and saturation is 89% on room air. On physical exam, his mental status appears altered. He has a bruise on his left arm that spontaneously appeared overnight. His cardiac exam is positive for a weak friction rub. Blood specimens are collected and sent for evaluation. An ECG is performed (see image). What therapy will this patient most likely receive next?
- A. Send the patient for hemodialysis (Correct Answer)
- B. Perform a STAT pericardiocentesis
- C. Prepare the patient for renal transplant
- D. Treat the patient with aspirin
- E. Treat the patient with cyclophosphamide and prednisone
Antimicrobial stewardship Explanation: ***Send the patient for hemodialysis***
- This patient presents with symptoms of **uremic encephalopathy** and **uremic pericarditis** in the context of **stage 4 kidney disease**. The altered mental status, weakness, fatigue, nausea, and the development of a bruise (which could indicate uremic coagulopathy) are suggestive of severe uremia. The ECG shows widespread **ST elevation and PR depression**, particularly noticeable in leads like II, V2-V6, which is a classic finding for pericarditis. The **weak friction rub** confirms this clinical suspicion. Hemodialysis is crucial to rapidly remove uremic toxins and resolve both uremic encephalopathy and pericarditis.
- The ECG findings, including diffuse **ST elevation** with **PR depression**, are characteristic of **pericarditis**. In a patient with end-stage renal disease, **uremia** is a common cause of pericarditis, which can be life-threatening if not promptly treated with dialysis.
*Perform a STAT pericardiocentesis*
- While the patient has pericarditis, there are no immediate signs of **cardiac tamponade**, such as muffled heart sounds, jugular venous distension, or pulsus paradoxus, that would necessitate an emergency pericardiocentesis.
- The primary treatment for **uremic pericarditis** is typically **hemodialysis** to resolve the underlying uremic state, not direct fluid removal unless tamponade is present.
*Prepare the patient for renal transplant*
- **Renal transplant** is a long-term solution for end-stage renal disease, but it is not an acute intervention for immediate life-threatening uremic complications like uremic pericarditis and encephalopathy.
- The patient needs urgent stabilization and treatment of his current acute medical issues before transplant consideration.
*Treat the patient with aspirin*
- While aspirin can be used for some forms of pericarditis, it is generally **contraindicated** in patients with **uremic pericarditis** due to the increased risk of **gastric bleeding** and potential exacerbation of uremic coagulopathy.
- The primary treatment for uremic pericarditis is **dialysis**, not anti-inflammatory medications, as the inflammation is driven by uremic toxins.
*Treat the patient with cyclophosphamide and prednisone*
- **Immunosuppressants** like cyclophosphamide and prednisone are used for autoimmune or inflammatory conditions causing pericarditis, such as systemic lupus erythematosus.
- This patient's pericarditis is clearly linked to **uremia** from kidney disease, not an autoimmune condition, making immunosuppressive therapy inappropriate and potentially harmful.
Antimicrobial stewardship US Medical PG Question 10: Five days after admission into the ICU for drug-induced acute kidney injury, a 27-year-old woman develops fever. She is currently on a ventilator and sedatives. Hemodialysis is performed via a catheter placed in the right internal jugular vein. Feeding is via a nasogastric tube. An indwelling urinary catheter shows minimum output. Her blood pressure is 85/45 mm Hg, the pulse is 112/min, the respirations are 32/min, and the temperature is 39.6°C (103.3°F). The examination of the central catheter shows erythema around the insertion site with no discharge. Lung auscultation shows rhonchi. Cardiac examination shows no new findings. A chest CT scan shows bilateral pleural effusions with no lung infiltration. Empirical antibiotic therapy is initiated. Blood cultures obtained from peripheral blood and the catheter tip show S. aureus with a similar antibiogram. Urinary culture obtained from the indwelling catheter shows polymicrobial growth. Which of the following best explains this patient’s recent findings?
- A. Catheter-associated urinary tract infection
- B. Central catheter-related bacteremia (Correct Answer)
- C. Endocarditis
- D. Ventilator-associated pneumonia
- E. Naso-gastric tube sinusitis
Antimicrobial stewardship Explanation: ***Central catheter-related bacteremia***
- The presence of **erythema at the catheter insertion site** and the isolation of **_S. aureus_ with a similar antibiogram from both peripheral blood and the catheter tip** are highly indicative of a catheter-related bloodstream infection.
- This type of infection is common in critically ill patients with central venous catheters due to the direct access provided for bacteria to enter the bloodstream.
*Catheter-associated urinary tract infection*
- While a **polymicrobial growth** in the urinary culture suggests a urinary tract infection, the isolation of **_S. aureus_ in blood cultures** with signs of local catheter infection points away from the urinary tract as the primary source of bacteremia.
- The patient has an **indwelling urinary catheter**, which is a risk factor for UTIs, but the systemic infection with _S. aureus_ is better explained by the central line.
*Endocarditis*
- Although **_S. aureus_ bacteremia** can lead to endocarditis, the case states that the **cardiac examination shows no new findings**, making endocarditis less likely as the primary explanation for the acute deterioration without other supporting evidence like a new murmur or imaging findings.
- Endocarditis is a potential complication of bacteremia, not typically the initial source, especially with a clear source like a central line.
*Ventilator-associated pneumonia*
- Pulmonary symptoms like **rhonchi** and **bilateral pleural effusions** are present, but the **lack of lung infiltration on CT** and the **isolation of _S. aureus_ from blood and catheter tip** (not respiratory samples) make VAP unlikely to be the primary cause of this systemic infection.
- The patient is also on a ventilator, which is a risk factor for VAP, but the microbiologic and imaging evidence does not fully support it as the main diagnosis.
*Naso-gastric tube sinusitis*
- While nasogastric tubes can cause sinusitis, which could manifest with fever, it is less likely to result in **_S. aureus_ bacteremia with a positive catheter tip culture**.
- Sinusitis would explain fever, but not the specific microbiological findings of _S. aureus_ in blood and catheter tip, nor the local erythema at the catheter site.
More Antimicrobial stewardship US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.