Infectious diseases (sepsis, endocarditis)

On this page
🦠 The Sepsis Cascade: When Immunity Becomes the Enemy
When infection triggers a systemic inflammatory response, the body's defense mechanisms can spiral into life-threatening organ dysfunction-this is sepsis, where immunity becomes the threat. You'll master the cascade from pathogen invasion through multi-organ failure, learn the diagnostic frameworks that distinguish sepsis from infection, and build the pattern recognition skills to deploy time-critical interventions like antibiotics and source control. By integrating hemodynamic support, immune modulation, and endocarditis-specific strategies, you'll develop the clinical judgment to navigate these high-stakes scenarios where every hour shapes survival.
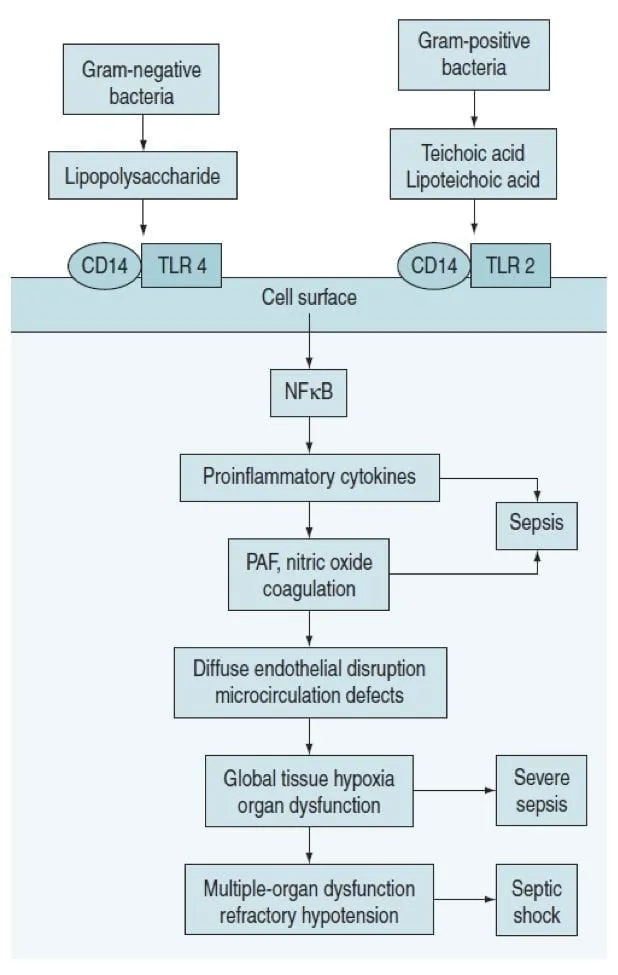
The pathophysiological foundation centers on dysregulated host response rather than simple microbial invasion. In sepsis, cytokine storm triggers widespread endothelial dysfunction, while endocarditis creates septic emboli that seed distant organs with infected material. Both conditions demonstrate how infectious agents exploit normal physiological processes to create life-threatening complications.
📌 Remember: SIRS-SOFA-SHOCK - Systemic Inflammatory Response Syndrome progresses through Sequential Organ Failure Assessment to Septic Shock, with lactate >4 mmol/L and MAP <65 mmHg defining shock parameters
Modern sepsis definitions emphasize organ dysfunction over inflammatory markers. The qSOFA score (altered mental status, systolic BP ≤100 mmHg, respiratory rate ≥22/min) identifies high-risk patients with 2-fold increased mortality when ≥2 criteria are present. This represents a paradigm shift from the previous SIRS-based criteria that captured 90% of ICU patients but lacked specificity.
| Parameter | SIRS Criteria | qSOFA Criteria | Septic Shock Criteria | Mortality Risk | Clinical Significance |
|---|---|---|---|---|---|
| Temperature | >38°C or <36°C | Not included | Variable | Low specificity | Historical marker |
| Heart Rate | >90 bpm | Not included | Often elevated | Low specificity | Compensatory response |
| Respiratory | >20/min or PaCO2 <32 | ≥22/min | Often elevated | Moderate | Metabolic compensation |
| Mental Status | Not included | Altered (GCS <15) | Often altered | High | Cerebral hypoperfusion |
| Blood Pressure | Not included | SBP ≤100 mmHg | MAP <65 mmHg | Very High | Circulatory failure |
The microbiology of severe infections reveals distinct patterns that guide empirical therapy. Gram-positive cocci (Staphylococcus, Streptococcus) dominate endocarditis cases, accounting for 65% of native valve infections, while gram-negative rods cause 40% of sepsis cases in hospitalized patients. Methicillin-resistant Staphylococcus aureus (MRSA) represents 15-20% of endocarditis isolates and requires vancomycin or daptomycin therapy.
- Endocarditis Microbiology Patterns
- Native valve acute: S. aureus (50% of cases)
- Native valve subacute: Viridans streptococci (30% of cases)
- S. sanguinis: dental procedures, MIC ≤0.12 mg/L penicillin sensitive
- S. mutans: poor dental hygiene, biofilm formation
- Prosthetic valve early (<60 days): Coagulase-negative staphylococci (40%)
- Prosthetic valve late (>60 days): S. aureus and streptococci (60%)
- IVDU-associated: S. aureus (75%), tricuspid valve preference
💡 Master This: Sepsis-3 criteria define sepsis as life-threatening organ dysfunction caused by dysregulated host response to infection, with SOFA score increase ≥2 points from baseline indicating organ dysfunction and in-hospital mortality >10%
Connect these foundational concepts through diagnostic frameworks to understand how clinical presentation guides therapeutic decisions.
🦠 The Sepsis Cascade: When Immunity Becomes the Enemy
🎯 Diagnostic Precision: The Clinical Detective Framework
📌 Remember: SOFA-CLOT - Sequential Organ Failure Assessment evaluates Cardiovascular (MAP, vasopressors), Liver (bilirubin), Oxygenation (PaO2/FiO2), Filtration/Renal (creatinine, urine), Coagulation (platelets), and Thinking/CNS (Glasgow Coma Scale)
Duke Criteria remain the gold standard for endocarditis diagnosis, with major criteria including positive blood cultures for typical organisms and echocardiographic evidence of vegetation. Sensitivity reaches 80% for definite endocarditis when both major criteria are present, while minor criteria (predisposing factors, fever >38°C, vascular phenomena) support the diagnosis.
| Duke Criteria Component | Major Criteria | Minor Criteria | Diagnostic Weight | Sensitivity | Clinical Application |
|---|---|---|---|---|---|
| Blood Cultures | Typical organisms in 2+ cultures | Single positive or atypical | High | 85-95% | Guides antimicrobial therapy |
| Echocardiography | Vegetation, abscess, dehiscence | Not applicable | High | 65-85% | TEE superior to TTE |
| Predisposing Factors | Not applicable | Heart condition, IVDU | Low | Variable | Risk stratification |
| Fever | Not applicable | >38°C (100.4°F) | Low | 85-90% | Non-specific finding |
| Vascular Phenomena | Not applicable | Emboli, mycotic aneurysm | Moderate | 15-35% | Suggests complications |
Laboratory biomarkers provide quantitative assessment of disease severity and treatment response. Procalcitonin levels >2 ng/mL suggest bacterial sepsis with 85% sensitivity and 77% specificity, while lactate >4 mmol/L indicates tissue hypoperfusion requiring immediate resuscitation. C-reactive protein lacks specificity but trends correlate with treatment response.
- Sepsis Laboratory Patterns
- Procalcitonin: <0.25 ng/mL (low bacterial risk), 0.25-0.5 ng/mL (possible), >2 ng/mL (likely bacterial)
- Sensitivity: 85% for bacterial sepsis
- Specificity: 77% for distinguishing bacterial from viral
- Lactate: <2 mmol/L (normal), 2-4 mmol/L (elevated), >4 mmol/L (severe hypoperfusion)
- Clearance >10% in 6 hours associated with improved survival
- White Blood Cell Count: <4,000 or >12,000 cells/μL (SIRS criteria)
- Bandemia >10% suggests bacterial infection
- Leukopenia indicates poor prognosis in sepsis
- Procalcitonin: <0.25 ng/mL (low bacterial risk), 0.25-0.5 ng/mL (possible), >2 ng/mL (likely bacterial)
⭐ Clinical Pearl: Transesophageal echocardiography (TEE) detects vegetations in 90-95% of endocarditis cases compared to 65% with transthoracic echo, making TEE essential when clinical suspicion is high despite negative TTE
Blood culture optimization requires proper technique and timing to maximize diagnostic yield. Two sets from different sites before antibiotics yield positive cultures in 85-95% of endocarditis cases, while three sets within 24 hours capture 99% of bacteremic episodes. Volume matters: 20-30 mL per culture increases sensitivity by 30% compared to smaller volumes.
💡 Master This: Modified Duke Criteria require 2 major, 1 major + 3 minor, or 5 minor criteria for definite endocarditis diagnosis, with negative predictive value >95% when criteria are not met and alternative diagnosis is established
Connect diagnostic precision through pattern recognition frameworks to understand how clinical presentations guide immediate therapeutic interventions.
🎯 Diagnostic Precision: The Clinical Detective Framework
🚨 Pattern Recognition: The Emergency Response Matrix
Sepsis phenotypes present distinct clinical patterns that guide therapeutic intensity and monitoring requirements. Warm shock (early sepsis) shows hyperdynamic circulation with cardiac output >8 L/min, warm extremities, and wide pulse pressure, while cold shock (late sepsis) demonstrates myocardial depression with cardiac output <4 L/min, cool extremities, and narrow pulse pressure.
- Sepsis Phenotype Recognition Patterns
- Hyperdynamic Phase ("Warm Shock")
- Cardiac output: ↑ (>8 L/min), SVR: ↓ (<800 dynes·sec/cm⁵)
- Skin: Warm, flushed, capillary refill <2 seconds
- Mental status: Alert to mildly confused
- Urine output: Initially preserved (>0.5 mL/kg/hr)
- Hypodynamic Phase ("Cold Shock")
- Cardiac output: ↓ (<4 L/min), SVR: Variable
- Skin: Cool, mottled, capillary refill >3 seconds
- Mental status: Altered, obtunded
- Urine output: Oliguria (<0.5 mL/kg/hr)
- Hyperdynamic Phase ("Warm Shock")
📌 Remember: WARM-COLD - Warm shock shows Wide pulse pressure, Alert mentality, Robust output, Maintained perfusion; Cold shock shows Constricted pulse pressure, Obtunded state, Low output, Diminished perfusion
Endocarditis presentation patterns correlate with organism virulence and valve involvement. Acute endocarditis (typically S. aureus) presents with high fever >39°C, rapid valve destruction within days, and systemic toxicity, while subacute endocarditis (typically viridans streptococci) shows low-grade fever, gradual onset over weeks, and constitutional symptoms.
| Endocarditis Type | Typical Organism | Onset Timeline | Fever Pattern | Valve Destruction | Embolic Risk | Mortality |
|---|---|---|---|---|---|---|
| Acute Native | S. aureus (70%) | Days to 2 weeks | High (>39°C) | Rapid, severe | High (35%) | 15-25% |
| Subacute Native | Viridans strep (60%) | Weeks to months | Low-grade | Gradual | Moderate (20%) | 5-10% |
| Prosthetic Early | CoNS (40%) | <60 days post-op | Variable | Dehiscence risk | High (30%) | 20-40% |
| Prosthetic Late | S. aureus (30%) | >60 days post-op | High | Rapid | High (35%) | 15-30% |
| IVDU-Associated | S. aureus (75%) | Days to weeks | High | Tricuspid common | Pulmonary (60%) | 5-15% |
Embolic phenomena provide crucial diagnostic clues and indicate disease severity. Septic emboli occur in 15-35% of endocarditis cases, with left-sided disease causing systemic emboli (stroke, splenic infarct, renal infarct) and right-sided disease causing pulmonary emboli. Mycotic aneurysms develop in 2-15% of cases and require urgent vascular surgery consultation.
⭐ Clinical Pearl: Osler nodes (painful finger/toe nodules) and Janeway lesions (painless palmar/plantar macules) occur in 10-25% of endocarditis cases, with Osler nodes suggesting immune complex deposition and Janeway lesions indicating septic emboli
Shock recognition patterns guide resuscitation priorities and vasopressor selection. Distributive shock (sepsis) shows low SVR <800 dynes·sec/cm⁵ requiring norepinephrine as first-line vasopressor, while cardiogenic shock (septic cardiomyopathy) shows low cardiac output <2.2 L/min/m² requiring dobutamine or milrinone support.
- Hemodynamic Pattern Recognition
- Distributive Shock (Classic Sepsis)
- CVP: Normal to low (6-12 mmHg)
- PCWP: Normal to low (<18 mmHg)
- Cardiac output: High early, low late
- SVR: Low (<800 dynes·sec/cm⁵)
- Mixed Shock (Sepsis + Cardiogenic)
- CVP: Elevated (>12 mmHg)
- PCWP: Elevated (>18 mmHg)
- Cardiac output: Low (<2.2 L/min/m²)
- SVR: Variable
- Distributive Shock (Classic Sepsis)
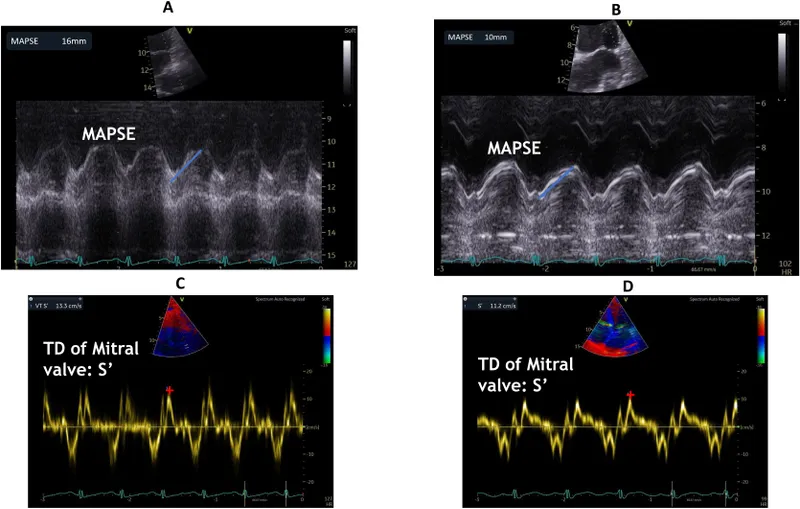
💡 Master This: Sepsis-induced cardiomyopathy occurs in 40-50% of septic shock patients, with reversible myocardial depression showing ejection fraction <45% that typically recovers within 7-10 days with appropriate treatment
Connect pattern recognition through systematic discrimination frameworks to understand how clinical presentations guide targeted therapeutic approaches.
🚨 Pattern Recognition: The Emergency Response Matrix
⚖️ Therapeutic Precision: The Treatment Algorithm Matrix
Hour-1 bundle implementation represents the cornerstone of sepsis management, with each hour delay in appropriate antibiotics increasing mortality by 7.6%. The bundle includes blood cultures before antibiotics, broad-spectrum antimicrobials within 60 minutes, 30 mL/kg crystalloid for hypotension or lactate ≥4 mmol/L, and vasopressors for persistent hypotension after fluid resuscitation.
📌 Remember: MAPS-30 - Measure lactate, Antibiotics <60 minutes, Pressure support with 30 mL/kg crystalloid, then Support with vasopressors for MAP ≥65 mmHg
Antimicrobial selection requires balancing broad coverage with resistance patterns and toxicity profiles. Piperacillin-tazobactam plus vancomycin provides excellent empirical coverage for 85% of sepsis pathogens, while meropenem plus vancomycin covers multidrug-resistant organisms in high-risk patients. De-escalation within 48-72 hours based on culture results reduces C. difficile risk by 40%.
| Clinical Scenario | First-line Empirical | Alternative Options | Coverage Spectrum | Duration | De-escalation Target |
|---|---|---|---|---|---|
| Community Sepsis | Pip-tazo + vancomycin | Ceftriaxone + azithromycin | Gram+/-, anaerobes | 7-10 days | Narrow based on cultures |
| Hospital-acquired | Meropenem + vancomycin | Cefepime + linezolid | MDR gram-, MRSA | 7-14 days | Targeted therapy |
| Immunocompromised | Meropenem + voriconazole | Cefepime + micafungin | Bacteria + fungi | 14-21 days | Organism-specific |
| Post-surgical | Pip-tazo + metronidazole | Ertapenem | Gram+/-, anaerobes | 5-7 days | Surgical source control |
| Neutropenic Fever | Cefepime monotherapy | Meropenem | Gram+/- coverage | Until ANC >500 | Risk-stratified |
- Endocarditis Treatment Protocols
- MSSA Native Valve
- Nafcillin: 12g/day divided q4h × 6 weeks
- Alternative: Cefazolin 6g/day divided q8h
- Gentamicin: 3 mg/kg/day × 3-5 days (synergy)
- MRSA Native Valve
- Vancomycin: 30-60 mg/kg/day (target trough 15-20 mg/L)
- Alternative: Daptomycin 8-10 mg/kg/day
- Duration: 6 weeks minimum
- Streptococcal Native Valve
- Penicillin G: 18-30 million units/day × 4 weeks
- Alternative: Ceftriaxone 2g daily × 4 weeks
- Gentamicin: 3 mg/kg/day × 2 weeks (if MIC ≤0.12)
- MSSA Native Valve
⭐ Clinical Pearl: Daptomycin at 8-10 mg/kg/day shows superior efficacy to vancomycin for MRSA endocarditis with faster bacterial clearance and reduced treatment failure rates, but requires weekly CPK monitoring for myopathy
Surgical intervention in endocarditis follows specific indications with timing critical for optimal outcomes. Heart failure from severe valve regurgitation requires urgent surgery with mortality benefit >50% when performed within 48 hours. Persistent bacteremia >5-7 days despite appropriate antibiotics indicates surgical source control necessity.
Vasopressor management in septic shock follows evidence-based protocols with norepinephrine as first-line therapy targeting MAP ≥65 mmHg. Vasopressin 0.03-0.04 units/min can be added as second-line agent, while epinephrine is reserved for refractory shock. Dobutamine 2.5-10 mcg/kg/min addresses septic cardiomyopathy when cardiac output <2.2 L/min/m².
💡 Master This: Early goal-directed therapy principles focus on MAP ≥65 mmHg, CVP 8-12 mmHg, urine output ≥0.5 mL/kg/hr, and ScvO2 ≥70% within 6 hours, with lactate clearance ≥10% as key resuscitation endpoint
Connect therapeutic precision through multi-system integration frameworks to understand how treatment decisions impact multiple organ systems simultaneously.
⚖️ Therapeutic Precision: The Treatment Algorithm Matrix
🔗 Systems Integration: The Multi-Organ Response Network
Sepsis-induced organ dysfunction follows predictable patterns based on microcirculatory failure and mitochondrial dysfunction. Cardiovascular collapse occurs through vasodilation (↓SVR), capillary leak (↓preload), and myocardial depression (↓contractility), while acute kidney injury develops in 40-50% of septic patients through hypoperfusion and inflammatory nephritis.
- Multi-System Sepsis Pathophysiology
- Cardiovascular System
- Vasodilation: NO-mediated, SVR ↓ 50-70% from baseline
- Capillary leak: Increased permeability, fluid extravasation
- Myocardial depression: EF ↓ 20-30%, reversible in 7-10 days
- Respiratory System
- ARDS development: 15-20% of sepsis patients
- V/Q mismatch: PaO2/FiO2 ratio <300
- Increased work: Respiratory rate >22/min
- Renal System
- AKI incidence: 40-50% of septic patients
- Creatinine rise: ≥0.3 mg/dL or 50% increase
- Oliguria: <0.5 mL/kg/hr for 6+ hours
- Neurological System
- Encephalopathy: 70% of sepsis patients
- Delirium: CAM-ICU positive in 60-80%
- Altered consciousness: GCS <15
- Cardiovascular System
📌 Remember: CARDIOVASCULAR-RESPIRATORY-RENAL-NEURO - Sepsis affects Circulation (vasodilation, leak), Airways (ARDS, V/Q mismatch), Renal function (AKI, oliguria), and Neurological status (encephalopathy, delirium)
Endocarditis complications demonstrate how cardiac infections create systemic manifestations through embolic phenomena, immune complex deposition, and hemodynamic compromise. Cerebral emboli occur in 15-20% of left-sided endocarditis cases, while splenic infarction and mycotic aneurysms represent septic embolic complications requiring multidisciplinary management.
| Complication Type | Incidence Rate | Pathophysiology | Clinical Manifestation | Diagnostic Method | Management Approach |
|---|---|---|---|---|---|
| Cerebral Emboli | 15-20% | Vegetation fragments | Stroke, TIA, seizures | MRI brain, CT | Anticoagulation contraindicated |
| Splenic Infarct | 40-60% | Septic emboli | LUQ pain, splenomegaly | CT abdomen | Conservative vs splenectomy |
| Mycotic Aneurysm | 2-15% | Arterial wall infection | Pulsatile mass, rupture | CT angiography | Urgent vascular surgery |
| Heart Failure | 40-70% | Valve destruction | Dyspnea, pulmonary edema | Echocardiography | Diuretics, valve surgery |
| Renal Infarct | 10-30% | Embolic occlusion | Flank pain, hematuria | CT with contrast | Supportive care |
Coagulation dysfunction in sepsis involves activation of both pro-coagulant and fibrinolytic pathways, leading to disseminated intravascular coagulation (DIC) in 30-50% of severe cases. Platelet consumption, factor depletion, and fibrin deposition create bleeding risk while simultaneously promoting microvascular thrombosis.
Metabolic derangements reflect cellular dysfunction and energy failure at the mitochondrial level. Lactate elevation >4 mmol/L indicates tissue hypoxia and anaerobic metabolism, while hyperglycemia (often >180 mg/dL) results from stress response and insulin resistance. Acidosis develops through lactate accumulation and renal dysfunction.
- Sepsis Metabolic Patterns
- Lactate Metabolism
- Normal: <2 mmol/L
- Elevated: 2-4 mmol/L (compensated shock)
- Severe: >4 mmol/L (tissue hypoperfusion)
- Clearance: >10% reduction in 6 hours predicts survival
- Glucose Dysregulation
- Hyperglycemia: Often >180 mg/dL despite no diabetes
- Insulin resistance: 3-5 fold increase in requirements
- Target range: 140-180 mg/dL in critically ill
- Acid-Base Status
- Metabolic acidosis: pH <7.35, HCO3 <22 mEq/L
- Anion gap: Often >12 mEq/L (lactate, ketoacids)
- Compensation: Respiratory alkalosis (↓PCO2)
- Lactate Metabolism
⭐ Clinical Pearl: Sepsis-associated encephalopathy occurs in 70% of patients through blood-brain barrier disruption, neuroinflammation, and microcirculatory dysfunction, with delirium being the most common manifestation requiring CAM-ICU assessment every 8 hours
Immune dysfunction in sepsis creates paradoxical immunosuppression following initial hyperinflammation, with lymphocyte apoptosis and monocyte deactivation leading to secondary infections in 25-30% of survivors. Immunoparalysis can persist for weeks to months, requiring vigilant monitoring for opportunistic pathogens.
💡 Master This: Sepsis represents a dysregulated host response where initial hyperinflammation (cytokine storm) transitions to compensatory anti-inflammatory response (immunoparalysis), creating biphasic immune dysfunction that requires different therapeutic approaches at different disease stages
Connect multi-system integration through evidence-based evaluation frameworks to understand how treatment decisions must account for complex organ interactions and recovery patterns.
🔗 Systems Integration: The Multi-Organ Response Network
🎯 Clinical Mastery: The Expert Decision Framework
Advanced sepsis management requires personalized medicine approaches based on biomarker profiles, genetic polymorphisms, and comorbidity patterns. Procalcitonin-guided therapy reduces antibiotic duration by 2.4 days without increasing mortality, while lactate clearance protocols improve survival by 11% when clearance >20% is achieved within 6 hours.
- Expert-Level Sepsis Decision Points
- Antibiotic Duration Optimization
- Procalcitonin <0.25 ng/mL: Consider discontinuation
- Clinical improvement + negative cultures: 5-7 days often sufficient
- Immunocompromised patients: Extended courses (10-14 days)
- Fluid Resuscitation Precision
- Initial: 30 mL/kg crystalloid within 3 hours
- Reassessment: Passive leg raise or fluid challenge
- Goal: Stroke volume optimization, not CVP targets
- Vasopressor Weaning Strategy
- MAP target: 65 mmHg minimum, higher if chronic HTN
- Weaning order: Vasopressin first, then norepinephrine
- Monitoring: Lactate clearance and urine output
- Antibiotic Duration Optimization
📌 Remember: PERSONALIZED-SEPSIS - Procalcitonin-guided antibiotics, Evaluate fluid responsiveness, Reassess targets frequently, Stratify by comorbidities, Optimize rather than maximize, Normalize lactate, Assess immune status, Lactate clearance goals, Individual MAP targets, Zero tolerance for delays, Early mobilization, Delirium prevention, Support family, Evaluate for rehabilitation, Prevent complications, Surveillance for secondary infections, Individualized care plans, Stewardship principles
Endocarditis surgical decision-making integrates hemodynamic status, vegetation characteristics, organism factors, and patient comorbidities into risk-benefit calculations. EuroSCORE II predicts operative mortality with good calibration for endocarditis patients, while vegetation size >10 mm with mobile characteristics increases embolic risk by 3-fold.
| Surgical Indication | Urgency Level | Mortality Benefit | Risk Factors | Timing Considerations | Success Rates |
|---|---|---|---|---|---|
| Acute Heart Failure | Emergent | 50% reduction | Cardiogenic shock | <24-48 hours | 85-90% |
| Large Mobile Vegetation | Urgent | 30% reduction | Size >10mm, mobility | <7 days | 80-85% |
| Persistent Bacteremia | Semi-urgent | 25% reduction | >5-7 days therapy | <14 days | 75-80% |
| Recurrent Emboli | Urgent | 40% reduction | Multiple events | <48 hours | 70-75% |
| Prosthetic Valve | Variable | 35% reduction | Early vs late | Case-dependent | 65-75% |
Long-term outcomes and quality metrics guide performance improvement in sepsis and endocarditis care. Sepsis survivors have 2-3 fold increased long-term mortality, cognitive impairment in 25%, and functional disability in 40%. Post-sepsis syndrome requires comprehensive rehabilitation and surveillance for secondary complications.
- Quality Improvement Metrics
- Process Measures
- Hour-1 bundle compliance: Target >80%
- Appropriate empirical antibiotics: Target >90%
- Blood cultures before antibiotics: Target >95%
- Outcome Measures
- In-hospital mortality: Benchmark <15% for sepsis
- Length of stay: Monitor trends and outliers
- Readmission rates: Target <10% within 30 days
- Long-term Measures
- Functional status: Barthel Index at discharge
- Cognitive assessment: Montreal Cognitive Assessment
- Quality of life: SF-36 at 6 months
- Process Measures
⭐ Clinical Pearl: Post-sepsis syndrome affects 50% of survivors with persistent inflammation, immunosuppression, and catabolism leading to muscle weakness, cognitive dysfunction, and increased infection susceptibility requiring multidisciplinary rehabilitation and long-term monitoring
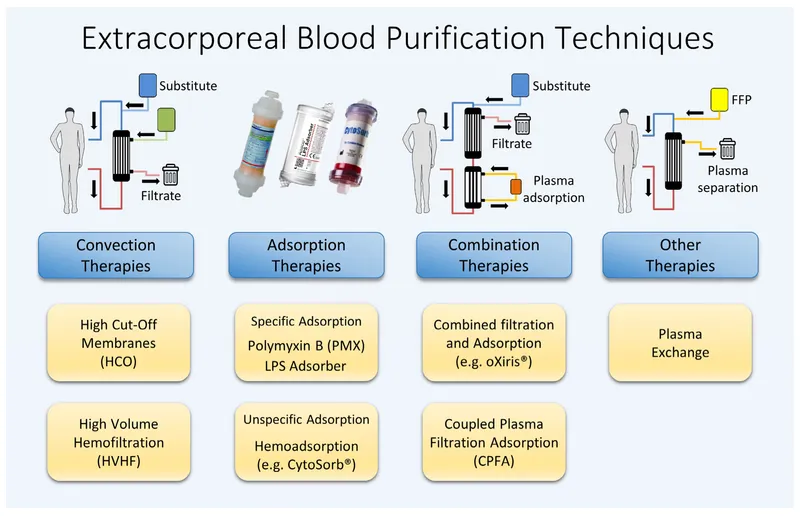
Emerging therapies and precision medicine approaches show promise for refractory cases. Extracorporeal cytokine removal with CytoSorb or Oxiris filters may benefit patients with cytokine storm, while immunomodulatory agents like anakinra (IL-1 antagonist) show mortality reduction in hyperinflammatory sepsis subgroups.
💡 Master This: Expert sepsis management requires dynamic assessment and adaptive strategies based on patient response, biomarker trends, and multi-organ function, with early recognition and aggressive initial treatment followed by personalized de-escalation and comprehensive rehabilitation planning
🎯 Clinical Mastery: The Expert Decision Framework
Practice Questions: Infectious diseases (sepsis, endocarditis)
Test your understanding with these related questions
A 51-year-old woman is brought into the emergency department following a motor vehicle accident. She is unconscious and was intubated in the field. Past medical history is unknown. Upon arrival, she is hypotensive and tachycardic. Her temperature is 37.2°C (99.1°F), the pulse is 110/min, the respiratory rate is 22/min, and the blood pressure is 85/60 mm Hg. There is no evidence of head trauma, she withdraws to pain and her pupils are 2mm and reactive to light. Her heart has a regular rhythm without any murmurs or rubs and her lungs are clear to auscultation. Her abdomen is firm and distended with decreased bowel sounds. Her extremities are cool and clammy with weak, thready pulses. There is no peripheral edema. Of the following, what is the likely cause of her presentation?










