Ulcerative colitis pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ulcerative colitis pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ulcerative colitis pathophysiology US Medical PG Question 1: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***NF-κB***
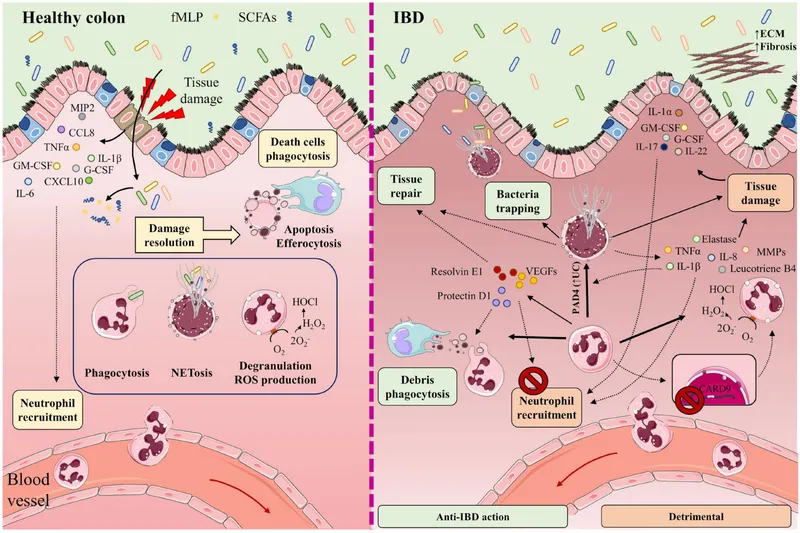
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
Ulcerative colitis pathophysiology US Medical PG Question 2: A 24-year-old woman presents to the clinic with chronic abdominal discomfort and cramping. She seeks medical attention now as she is concerned about the diarrhea that she has developed that is occasionally mixed with tiny streaks of blood. Her medical history is significant for lactose intolerance and asthma. She has a family history of wheat allergy and reports that she has tried to make herself vomit on several occasions to lose weight. After counseling the patient about the dangers of bulimia, physical examination reveals the rectum is red, inflamed, tender, and a perirectal abscess is seen draining purulent material. Colonoscopy demonstrates scattered mucosal lesions involving the colon and terminal ileum. A complete blood count is given below:
Hb%: 10 gm/dL
Total count (WBC): 12,500/mm3
Differential count:
Neutrophils: 50%
Lymphocytes: 40%
Monocytes: 5%
ESR: 22 mm/hr
What is the most likely diagnosis?
- A. Ulcerative colitis
- B. Celiac disease
- C. Irritable bowel syndrome
- D. Crohn’s disease (Correct Answer)
- E. Laxative abuse
Ulcerative colitis pathophysiology Explanation: ***Crohn’s disease***
- The presence of **abdominal discomfort, cramping, bloody diarrhea, perirectal abscess**, and **scattered mucosal lesions involving the colon and terminal ileum** are classic findings consistent with Crohn's disease. The involvement of the terminal ileum is a hallmark of Crohn's.
- Anemia (Hb% 10 gm/dL), leukocytosis (WBC 12,500/mm3), and elevated ESR (22 mm/hr) indicate **chronic inflammation** and are common in Crohn's disease.
*Ulcerative colitis*
- While ulcerative colitis presents with bloody diarrhea and abdominal discomfort, it typically involves **continuous inflammation confined to the colon** and rectum, without skip lesions or involvement of the terminal ileum.
- Perirectal abscesses are also less common in ulcerative colitis compared to Crohn's disease.
*Celiac disease*
- Celiac disease is an autoimmune disorder triggered by **gluten**, primarily affecting the **small intestine** and presenting with malabsorption, diarrhea, and abdominal pain. However, it does not typically cause bloody diarrhea, perirectal abscesses, or colon inflammation visible on colonoscopy.
- While there is a family history of wheat allergy, the clinical picture is more indicative of inflammatory bowel disease.
*Irritable bowel syndrome*
- IBS is characterized by chronic abdominal pain, discomfort, and altered bowel habits (diarrhea, constipation, or both), but it is a **functional gastrointestinal disorder** without evidence of inflammation, structural abnormalities, or bloody stools.
- The presence of bloody diarrhea, perirectal abscess, and inflammatory markers rules out IBS.
*Laxative abuse*
- Laxative abuse can cause chronic diarrhea, abdominal cramping, and electrolyte disturbances, but it does **not cause inflammatory changes** such as mucosal lesions, bloody diarrhea, or perirectal abscesses seen on colonoscopy.
- While a history of bulimia is mentioned, the specific findings point towards an inflammatory process.
Ulcerative colitis pathophysiology US Medical PG Question 3: A 22-year-old woman presents to the emergency department with a 3-day history of fever and abdominal pain. She says that the pain is located in the left lower quadrant of the abdomen and feels crampy in nature. The pain has been associated with bloody diarrhea and joint tenderness. She has no past medical history but says that she returned 2 weeks ago from vacation in Asia where she tried many new foods. Her family history is significant for multiple cancers in close relatives. Physical exam reveals swollen ulcers on her legs, and colonoscopy reveals contiguous ulcerations from the rectum through the descending colon. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Noncaseating granulomas
- B. Severe aortic stenosis
- C. Gram-negative rod
- D. HLA-DQ2 positivity
- E. Perinuclear anti-neutrophil cytoplasmic antibodies (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Perinuclear anti-neutrophil cytoplasmic antibodies***
- The patient's presentation with **bloody diarrhea**, low-grade fever, **crampy abdominal pain**, joint tenderness, and contiguous ulcerations in the colon is highly suggestive of **ulcerative colitis**.
- **Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA)** are found in 50-70% of patients with ulcerative colitis and are associated with a more extensive disease.
*Noncaseating granulomas*
- **Noncaseating granulomas** are a characteristic histological finding in **Crohn's disease**, not ulcerative colitis.
- Crohn's disease typically presents with **skip lesions**, **transmural inflammation**, and affects any part of the GI tract, often with perianal disease.
*Severe aortic stenosis*
- **Severe aortic stenosis** is a condition of the heart valves that can lead to symptoms like chest pain, syncope, and heart failure, and is not directly associated with the patient's gastrointestinal and systemic symptoms.
- While inflammatory conditions can rarely have cardiac manifestations, there's no direct link between aortic stenosis and inflammatory bowel disease in this context.
*Gram-negative rod*
- While infections, especially from **Gram-negative rods** like *Shigella* or *Salmonella*, can cause acute bloody diarrhea, the 3-day history with joint tenderness and contiguous ulcers on colonoscopy points more towards an inflammatory bowel disease.
- The chronicity and systemic involvement are less typical for an acute bacterial enteritis, although such infections might trigger IBD.
*HLA-DQ2 positivity*
- **HLA-DQ2 positivity** is strongly associated with **celiac disease**, an immune-mediated enteropathy triggered by gluten.
- Celiac disease typically presents with malabsorption symptoms like fatty stools, weight loss, and iron deficiency, rather than bloody diarrhea and contiguous colonic ulcerations.
Ulcerative colitis pathophysiology US Medical PG Question 4: A 28-year-old man comes to the physician because of a 6-month history of progressive fatigue and intermittent diarrhea. During this time, he has had a 6-kg (13-lb) weight loss. Physical examination shows pale conjunctivae. Abdominal examination shows tenderness to palpation in the lower quadrants. An image from a colonoscopy of the descending colon is shown. Further evaluation is most likely to show which of the following findings?
- A. PAS-positive cytoplasmic granules
- B. Anti-Saccharomyces cerevisiae antibodies
- C. Positive lactose hydrogen breath test
- D. Perinuclear antineutrophil cytoplasmic antibodies (Correct Answer)
- E. Anti-tissue transglutaminase antibodies
Ulcerative colitis pathophysiology Explanation: ***Perinuclear antineutrophil cytoplasmic antibodies***
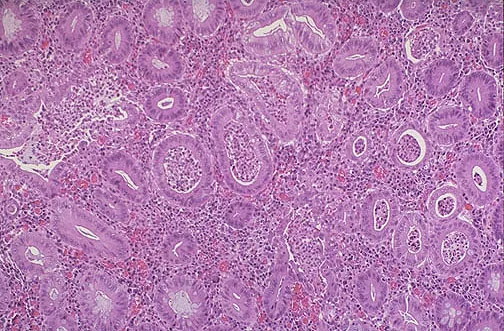
- The image provided, combined with symptoms of **fatigue**, **intermittent diarrhea**, **weight loss**, and **abdominal tenderness**, is highly suggestive of **ulcerative colitis**.
- **p-ANCA** are found in 60-70% of patients with **ulcerative colitis** and are a valuable diagnostic marker.
- The colonoscopy showing involvement of the descending colon with continuous inflammation is characteristic of UC.
*PAS-positive cytoplasmic granules*
- **PAS-positive macrophages** are characteristic of **Whipple's disease**, which typically presents with malabsorption and arthralgia.
- While Whipple's can cause GI symptoms, the endoscopic findings here are more consistent with **inflammatory bowel disease (IBD)** than with the diffuse mucosal changes of Whipple's disease.
*Anti-Saccharomyces cerevisiae antibodies*
- **Anti-Saccharomyces cerevisiae antibodies (ASCA)** are more commonly associated with **Crohn's disease**, where they are found in up to 60-70% of patients.
- The colonoscopy image, showing diffuse inflammation primarily in the descending colon without skip lesions, is more indicative of **ulcerative colitis** rather than Crohn's disease.
*Positive lactose hydrogen breath test*
- A positive lactose hydrogen breath test indicates **lactose intolerance**, which can cause diarrhea and abdominal discomfort.
- This does not explain the extensive inflammatory changes seen on colonoscopy or the progressive weight loss and anemia characteristic of IBD.
*Anti-tissue transglutaminase antibodies*
- **Anti-tissue transglutaminase antibodies** are highly specific for **celiac disease**, which presents with malabsorption, diarrhea, and weight loss.
- While celiac disease shares some symptoms, the colonoscopy findings are typical of **inflammatory bowel disease**, not celiac disease, which primarily affects the **small intestine** (duodenum and jejunum) rather than the colon.
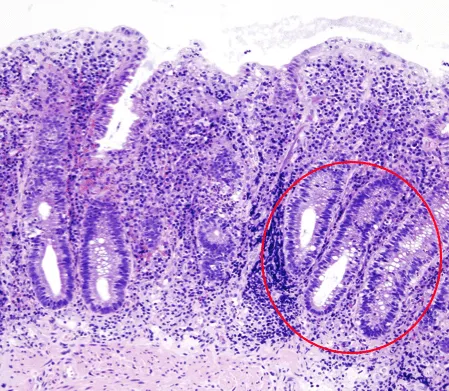
Ulcerative colitis pathophysiology US Medical PG Question 5: A 23-year-old female presents with a seven-day history of abdominal pain, and now bloody diarrhea that brings her to her primary care physician. Review of systems is notable for a 12-pound unintentional weight loss and intermittent loose stools. She has a family history notable for a father with CAD and a mother with primary sclerosing cholangitis. Upon further workup, she is found to have the following on colonoscopy and biopsy, Figures A and B respectively. Serum perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) is positive. This patient's disease is likely to also include which of the following features?
- A. Worse disease severity near the ileocecal valve
- B. Cobblestoning and skip lesions
- C. Fistulae and stricture formation
- D. Perianal disease
- E. Continuous progression beginning in the rectum (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Continuous progression beginning in the rectum***
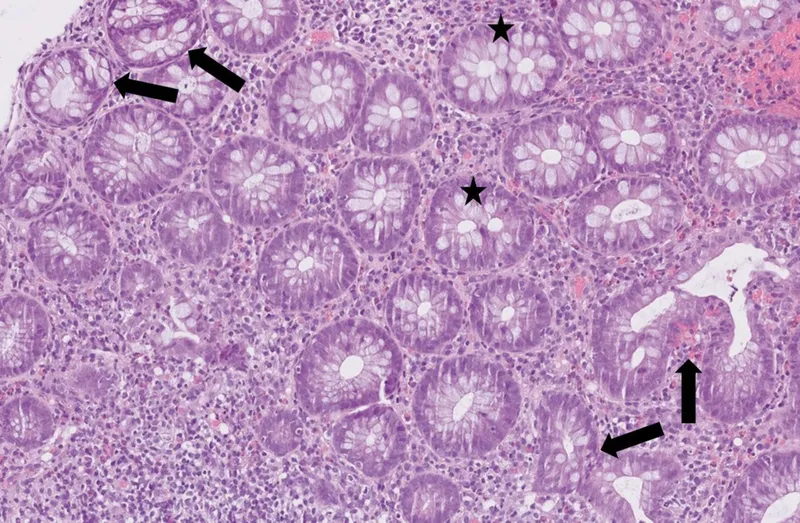
- The patient's presentation with abdominal pain, bloody diarrhea, weight loss, and **positive P-ANCA** is highly suggestive of **ulcerative colitis**.
- **Ulcerative colitis** characteristically presents with **continuous inflammation** that begins in the **rectum** and extends proximally through the colon.
*Worse disease severity near the ileocecal valve*
- This feature is more characteristic of **Crohn's disease**, where the **ileocecal region** is a common site of severe involvement.
- In **ulcerative colitis**, inflammation is typically confined to the colon and does not disproportionately affect the ileocecal valve unless there is backwash ileitis.
*Cobblestoning and skip lesions*
- **Cobblestoning** and **skip lesions** are classic endoscopic findings in **Crohn's disease**, reflecting the patchy, transmural inflammation.
- **Ulcerative colitis** is characterized by diffuse, superficial inflammation without skip lesions.
*Fistulae and stricture formation*
- The formation of **fistulae** (abnormal connections between organs) and **strictures** (narrowing of the bowel lumen) are hallmarks of **Crohn's disease** due to its transmural inflammation.
- These complications are rare in **ulcerative colitis**, which primarily affects the mucosal layer.
*Perianal disease*
- **Perianal disease**, including **fissures**, **abscesses**, and **fistulae**, is a common extraintestinal manifestation and complication of **Crohn's disease**.
- While other extraintestinal manifestations like **primary sclerosing cholangitis** can occur in both, perianal disease itself is less typical for uncomplicated **ulcerative colitis**.
Ulcerative colitis pathophysiology US Medical PG Question 6: A 42-year-old man comes to the physician because of a 6-week history of intermittent fever, abdominal pain, bloody diarrhea, and sensation of incomplete rectal emptying. He also has had a 4.5-kg (10-lb) weight loss over the past 3 months. Abdominal examination shows diffuse tenderness. Colonoscopy shows circumferential erythematous lesions that extend without interruption from the anal verge to the cecum. A biopsy specimen taken from the rectum shows mucosal and submucosal inflammation with crypt abscesses. This patient is most likely at risk of developing colon cancer with which of the following characteristics?
- A. Low-grade lesion
- B. Unifocal lesion
- C. Non-polypoid dysplasia (Correct Answer)
- D. Late p53 mutation
- E. Early APC mutation
Ulcerative colitis pathophysiology Explanation: ***Non-polypoid dysplasia***
- The patient's symptoms (bloody diarrhea, abdominal pain, crypt abscesses, continuous inflammation extending to the cecum) are highly suggestive of **ulcerative colitis (UC)**.
- In UC, the chronic inflammation causes a field defect across the colonic mucosa, leading to a higher risk of **non-polypoid (flat) dysplasia** and subsequent colon cancer (colitis-associated cancer).
*Low-grade lesion*
- While dysplasia can be low-grade, the primary characteristic of colon cancer development in UC is the **type of growth** (flat/non-polypoid) rather than simply its grade.
- The presence and progression of **dysplasia** (regardless of initial grade) are critical for risk stratification in UC.
*Unifocal lesion*
- Colitis-associated cancer in UC often arises from widespread field changes due to chronic inflammation, making **multifocal or diffuse dysplasia** more common than a single, isolated lesion.
- The diffuse nature of UC inflammation across the colon makes a unifocal cancerous change less typical compared to sporadic colon cancer.
*Late p53 mutation*
- **p53 mutations** are commonly found in colitis-associated colon cancer and are generally considered an **early event** in the progression from dysplasia to invasive carcinoma, rather than a late one.
- Mutations in tumor suppressor genes like **p53** contribute to genomic instability early in the neoplastic process.
*Early APC mutation*
- **APC mutations** are a hallmark of **sporadic colorectal cancer** and familial adenomatous polyposis (FAP), where they typically initiate the adenoma-carcinoma sequence.
- In **colitis-associated cancer**, APC mutations are less frequently the initiating event and often occur later, with other pathways (e.g., p53, microsatellite instability) being more prominent in early carcinogenesis.
Ulcerative colitis pathophysiology US Medical PG Question 7: A 34-year-old woman with no significant prior medical history presents to the clinic with several days of bloody stool. She also complains of constipation and straining, but she has no other symptoms. She has no family history of colorectal cancer or inflammatory bowel disease. She does not smoke or drink alcohol. Her vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 77/min, and respiratory rate is 15/min. There is no abdominal discomfort on physical exam, and a digital rectal exam reveals bright red blood. Of the following, which is the most likely diagnosis?
- A. Colorectal cancer
- B. Ulcerative colitis
- C. Anal fissure
- D. External hemorrhoids
- E. Internal hemorrhoids (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Internal hemorrhoids***
- **Painless bright red blood** per rectum, especially with **constipation and straining**, is highly characteristic of internal hemorrhoids.
- Internal hemorrhoids are located **above the dentate line**, making them typically painless, and they often prolapse during defecation, causing bleeding.
*Colorectal cancer*
- While colorectal cancer can cause bloody stool, it is less likely in a **34-year-old woman with no family history** and no other systemic symptoms like weight loss or abdominal pain.
- The bright red blood associated with straining points away from an upper GI bleed, which is more typical of many colorectal cancers.
*Ulcerative colitis*
- Ulcerative colitis typically presents with bloody diarrhea, abdominal pain, and tenesmus, which are **not mentioned** in this patient's history.
- It is a chronic inflammatory condition, and the isolated symptom of bright red blood with constipation is not classic for UC.
*Anal fissure*
- An anal fissure would cause **severe pain during defecation** due to a tear in the anal canal, which is absent in this patient.
- While an anal fissure can cause bright red blood, the lack of pain makes it less likely than hemorrhoids.
*External hemorrhoids*
- **External hemorrhoids are usually painful or itchy** and located below the dentate line.
- They also can cause bleeding, but the absence of pain and bright red blood suggests internal hemorrhoids which are more likely to bleed painlessly.
Ulcerative colitis pathophysiology US Medical PG Question 8: A 32-year-old man comes to the physician for a follow-up examination. He has a 2-month history of increasing generalized fatigue and severe pruritus. He has hypertension and ulcerative colitis which was diagnosed via colonoscopy 5 years ago. Current medications include lisinopril and rectal mesalamine. He is sexually active with 2 female partners and uses condoms inconsistently. His temperature is 37.3°C (99.1°F), pulse is 86/min, and blood pressure is 130/84 mm Hg. Examination shows scleral icterus and multiple scratch marks on the trunk and extremities. The lungs are clear to auscultation. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.5 g/dL
Leukocyte count 7500/mm3
Platelet count 280,000/mm3
Serum
Na+ 138 mEq/L
Cl- 101 mEq/L
K+ 4.7 mEq/L
Urea nitrogen 18 mg/dL
Glucose 91 mg/dL
Creatinine 0.8 mg/dL
Bilirubin
Total 1.5 mg/dL
Direct 0.9 mg/dL
Alkaline phosphatase 460 U/L
AST 75 U/L
ALT 78 U/L
Anti-nuclear antibody negative
Antimitochondrial antibodies negative
Abdominal ultrasound shows thickening of the bile ducts and focal bile duct dilatation. Which of the following is the most likely diagnosis?
- A. Primary biliary cholangitis
- B. Hepatitis B infection
- C. Autoimmune hepatitis
- D. IgG4-associated cholangitis
- E. Primary sclerosing cholangitis (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Primary sclerosing cholangitis***
- This patient's history of **ulcerative colitis** combined with cholestatic liver injury (elevated alkaline phosphatase >> transaminases), **scleral icterus**, and **severe pruritus** strongly suggests primary sclerosing cholangitis (PSC).
- The imaging findings of **bile duct thickening and focal dilatation** are characteristic of PSC, which causes chronic inflammation and fibrosis of intra- and extrahepatic bile ducts.
- PSC is strongly associated with inflammatory bowel disease, particularly **ulcerative colitis** (present in 60-80% of PSC patients), and typically affects men in their 30s-40s.
- Negative antimitochondrial antibodies help distinguish this from primary biliary cholangitis.
*Primary biliary cholangitis*
- Primary biliary cholangitis (PBC) typically affects **middle-aged women** and is characterized by positive **antimitochondrial antibodies (AMAs)**, which are negative in this patient.
- While PBC also causes cholestatic liver injury with pruritus, the male gender, younger age, strong association with ulcerative colitis, and bile duct changes on imaging point to PSC rather than PBC.
*Hepatitis B infection*
- Viral hepatitis B typically presents with a **hepatocellular pattern** of injury with AST and ALT elevated much higher than alkaline phosphatase (often >1000 U/L).
- This patient shows a **cholestatic pattern** (alkaline phosphatase 460 U/L with transaminases only mildly elevated at 75-78 U/L).
- Diagnosis would require positive hepatitis B serologies (HBsAg, anti-HBc), which are not present.
*Autoimmune hepatitis*
- Autoimmune hepatitis causes a **hepatocellular injury pattern** with very high transaminases (often >500-1000 U/L) and is associated with positive autoantibodies such as **ANA** or **anti-smooth muscle antibodies**, which are negative in this case.
- This patient's predominant cholestatic pattern and bile duct abnormalities are not consistent with autoimmune hepatitis.
*IgG4-associated cholangitis*
- IgG4-associated cholangitis can mimic PSC with bile duct stricturing and obstructive jaundice, but typically presents with **elevated serum IgG4 levels** and characteristic histopathology.
- It is **not associated with ulcerative colitis** and is much less common than PSC.
- This diagnosis would require tissue biopsy showing dense lymphoplasmacytic infiltrate with IgG4-positive plasma cells.
Ulcerative colitis pathophysiology US Medical PG Question 9: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Start annual colonoscopy starting in 8 years***
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Ulcerative colitis pathophysiology US Medical PG Question 10: A 22-year-old man presents to the emergency department with abdominal pain. The patient states that he has had right lower quadrant abdominal pain for "a while now". The pain comes and goes, and today it is particularly painful. The patient is a college student studying philosophy. He drinks alcohol occasionally and is currently sexually active. He states that sometimes he feels anxious about school. The patient's father died of colon cancer at the age of 55, and his mother died of breast cancer when she was 57. The patient has a past medical history of anxiety and depression which is not currently treated. Review of systems is positive for bloody diarrhea. His temperature is 99.5°F (37.5°C), blood pressure is 100/58 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is within normal limits. Abdominal exam reveals diffuse tenderness. A fecal occult blood test is positive. Which of the following is the most likely diagnosis?
- A. Irritable bowel syndrome
- B. Colon cancer
- C. Appendicitis
- D. Infectious colitis
- E. Inflammatory bowel disease (IBD) (Correct Answer)
Ulcerative colitis pathophysiology Explanation: ***Inflammatory bowel disease (IBD)***
- The patient's presentation with **recurrent right lower quadrant pain**, **bloody diarrhea**, a **positive fecal occult blood test**, and a family history concerning for GI issues (colon cancer in father) in a young adult is highly suggestive of IBD, specifically **Crohn's disease** due to the RLQ pain location.
- His history of anxiety and depression is common in IBD patients, and the elevated pulse with mild hypotension suggests **volume depletion** from bloody diarrhea, a common complication.
*Irritable bowel syndrome*
- While IBS can cause recurrent abdominal pain, it is characterized by **functional bowel changes** and typically does not present with **bloody diarrhea** or a positive fecal occult blood test.
- IBS symptoms are often relieved by defecation and are not usually associated with significant systemic inflammation or blood loss.
*Colon cancer*
- Colon cancer is less likely in a **22-year-old** presenting with these acute symptoms, despite the family history, as it typically affects older individuals.
- While it can cause bloody stools and abdominal pain, the **recurrent nature** and acute presentation with bloody diarrhea are more classic for IBD in this age group.
*Appendicitis*
- Appendicitis presents with acute, **migratory right lower quadrant pain** that typically progresses and worsens over hours to a day, often with fever and leukocytosis.
- The given history of pain for "**a while now**" and bloody diarrhea makes appendicitis an unlikely primary diagnosis.
*Infectious colitis*
- Infectious colitis can cause abdominal pain and bloody diarrhea, but it's usually **acute in onset** without a long history of recurrent symptoms.
- While possible, the **recurrent nature** of the pain and bloody diarrhea for "**a while now**" makes a chronic condition like IBD more probable.
More Ulcerative colitis pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.