Surgical management in IBD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical management in IBD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical management in IBD US Medical PG Question 1: A 22-year-old woman comes to the physician because of abdominal pain and diarrhea for 2 months. The pain is intermittent, colicky and localized to her right lower quadrant. She has anorexia and fears eating due to the pain. She has lost 4 kg (8.8 lb) during this time. She has no history of a serious illness and takes no medications. Her temperature is 37.8°C (100.0°F), blood pressure 125/65 mm Hg, pulse 75/min, and respirations 14/min. An abdominal examination shows mild tenderness of the right lower quadrant on deep palpation without guarding. Colonoscopy shows small aphthous-like ulcers in the right colon and terminal ileum. Biopsy from the terminal ileum shows noncaseating granulomas in all layers of the bowel wall. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Budesonide (Correct Answer)
- B. Azathioprine
- C. Ciprofloxacin
- D. Metronidazole
- E. Rectal mesalamine
Surgical management in IBD Explanation: ***Budesonide***
- This patient presents with symptoms and findings (RLQ pain, aphthous ulcers, noncaseating granulomas in the terminal ileum) consistent with **Crohn's disease** isolated to the **ileum and right colon**.
- **Budesonide** is a glucocorticoid with high first-pass metabolism, making it effective for localized ileal and right colonic Crohn's disease with fewer systemic side effects than prednisone.
*Azathioprine*
- **Azathioprine** is an immunomodulator used for maintaining remission in moderate to severe Crohn's disease, not typically for acute exacerbations as first-line monotherapy.
- Its onset of action is slow (several weeks to months), making it unsuitable for immediate symptom control.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic mainly used when there is concern for bacterial overgrowth, abscess, or perianal disease in Crohn's, none of which are explicitly indicated here.
- There is no evidence suggesting a primary bacterial infection as the cause of her current symptoms.
*Metronidazole*
- **Metronidazole** is an antibiotic often used for Crohn's disease with perianal involvement or fistulas, and sometimes for active colonic disease, but less effective for ileal involvement.
- Like ciprofloxacin, it's not the primary treatment for uncomplicated flare of ileocolonic Crohn's.
*Rectal mesalamine*
- **Rectal mesalamine** is an aminosalicylate primarily used for mild to moderate **ulcerative colitis**, particularly proctitis or left-sided colitis due to its topical action.
- It is ineffective for Crohn's disease involving the terminal ileum and right colon, as it would not reach this location in sufficient concentration.
Surgical management in IBD US Medical PG Question 2: A 69-year-old male presents to the Emergency Department with bilious vomiting that started within the past 24 hours. His medical history is significant for hypertension, hyperlipidemia, and a myocardial infarction six months ago. His past surgical history is significant for a laparotomy 20 years ago for a perforated diverticulum. Most recently he had some dental work done and has been on narcotic pain medicine for the past week. He reports constipation and obstipation. He is afebrile with a blood pressure of 146/92 mm Hg and a heart rate of 116/min. His abdominal exam reveals multiple well-healed scars with distension but no tenderness. An abdominal/pelvic CT scan reveals dilated small bowel with a transition point to normal caliber bowel distally. When did the cause of his pathology commence?
- A. One week ago
- B. Six months ago
- C. 20 years ago (Correct Answer)
- D. At birth
- E. 24 hours ago
Surgical management in IBD Explanation: ***20 years ago***
- The patient's history of a **laparotomy 20 years ago** for a perforated diverticulum is the most likely cause of his current small bowel obstruction. **Adhesions** from prior abdominal surgery are the leading cause of small bowel obstruction.
- The CT scan finding of **dilated small bowel** with a **transition point** confirms a mechanical obstruction, and the operative scarring supports adhesions as the etiology.
*One week ago*
- While **narcotic pain medicine** can cause constipation and ileus, it typically leads to a more diffuse distention without a clear transition point characteristic of a mechanical obstruction.
- The development of a clear transition point on CT after only one week of narcotic use makes a mechanical obstruction from adhesions more likely than a pure narcotic-induced ileus.
*Six months ago*
- A **myocardial infarction** six months ago is not directly related to the development of a small bowel obstruction.
- While cardiac events can sometimes lead to mesenteric ischemia, the CT findings of a transition point are more indicative of a mechanical obstruction rather than ischemia.
*At birth*
- Congenital conditions causing small bowel obstruction, such as **atresia** or **malrotation**, typically present in infancy or early childhood.
- Given the patient's age and history of prior abdominal surgery, a congenital cause is highly unlikely.
*24 hours ago*
- The onset of symptoms within the past 24 hours describes the **acute presentation** of the obstruction, not its underlying cause.
- The obstruction itself developed over time due to a predisposing factor from his past medical history.
Surgical management in IBD US Medical PG Question 3: A 17-year-old girl comes to the physician for a scheduled colonoscopy. She was diagnosed with familial adenomatous polyposis at the age of 13 years. Last year, her flexible sigmoidoscopy showed 12 adenomatous polyps (< 6 mm) that were removed endoscopically. Her father and her paternal grandmother were diagnosed with colon cancer at the age of 37 and 39 years, respectively. The patient appears nervous but otherwise well. Her vital signs are within normal limits. Examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. A colonoscopy shows hundreds of diffuse 4–9 mm adenomatous polyps covering the colon and > 30 rectal adenomas. Which of the following is the most appropriate next step in management?
- A. Endoscopic biopsy of polyps
- B. Proctocolectomy with ileoanal anastomosis (Correct Answer)
- C. CT scan of the abdomen with contrast
- D. Folinic acid (leucovorin) + 5-Fluorouracil + oxaliplatin therapy
- E. Repeat colonoscopy in 6 months
Surgical management in IBD Explanation: ***Proctocolectomy with ileoanal anastomosis***
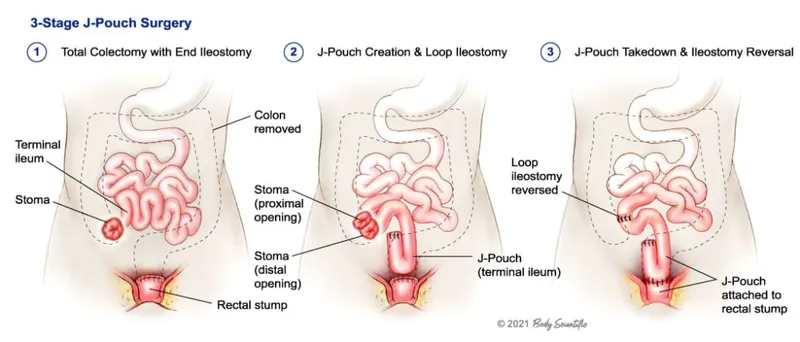
- This patient has **familial adenomatous polyposis (FAP)** with an advanced stage characterized by hundreds of diffuse polyps, indicating a high risk of **colorectal cancer**. A proctocolectomy with ileoanal anastomosis is the definitive surgical management to prevent cancer.
- The procedure removes the entire colon and most of the rectum, eliminating the source of future polyps and cancer while preserving an acceptable quality of life through the ileoanal pouch.
*Endoscopic biopsy of polyps*
- While biopsies are important for initial diagnosis, the diagnosis of FAP is already established, and the presence of **hundreds of diffuse polyps** means individual biopsies are not appropriate as a primary management strategy for cancer prevention.
- Doing multiple biopsies would be time-consuming and not prevent the inevitable progression to cancer given the extent of polyposis.
*CT scan of the abdomen with contrast*
- A CT scan is primarily used for **staging if cancer is suspected** or for evaluating metastases, not as a primary management step for polyps in FAP.
- The immediate concern is the incredibly high risk of developing cancer due to the polyps themselves, which surgical removal directly addresses.
*Folinic acid (leucovorin) + 5-Fluorouracil + oxaliplatin therapy*
- This is a chemotherapy regimen (**FOLFOX**) typically used for **established colorectal cancer**, particularly in advanced or metastatic stages.
- The patient has extensive polyposis but not yet confirmed colorectal cancer requiring chemotherapy, making this treatment premature and inappropriate.
*Repeat colonoscopy in 6 months*
- Repeating a colonoscopy in 6 months is insufficient for managing FAP with **hundreds of diffuse polyps**, as the risk of malignant transformation is imminent and widespread.
- The sheer volume of polyps makes endoscopic removal impractical and ineffective in preventing cancer; definitive surgery is required.
Surgical management in IBD US Medical PG Question 4: An 18-year-old man presents with bloody diarrhea and weight loss. He undergoes endoscopic biopsy which shows pseudopolyps. Biopsies taken during the endoscopy show inflammation only involving the mucosa and submucosa. He is diagnosed with an inflammatory bowel disease. Which of the following characteristics was most likely present?
- A. Cobblestone mucosa
- B. Skip lesions
- C. Fistulas and strictures
- D. Noncaseating granuloma
- E. Rectal involvement (Correct Answer)
Surgical management in IBD Explanation: **_Rectal involvement_**
- The description of **bloody diarrhea** and **pseudopolyps** on endoscopy, along with inflammation limited to the **mucosa and submucosa**, is highly characteristic of **ulcerative colitis (UC)**. UC invariably involves the rectum and extends proximally in a continuous fashion.
- The presence of **pseudopolyps** is common in UC due to cycles of mucosal ulceration and regeneration.
*Cobblestone mucosa*
- **Cobblestone mucosa** is a classic endoscopic finding in **Crohn's disease**, resulting from deep ulcerations interspersed with islands of edematous, non-ulcerated mucosa.
- This feature points to a transmural pattern of inflammation, which is inconsistent with the superficial inflammation confined to the **mucosa and submucosa** described.
*Skip lesions*
- **Skip lesions** refer to discontinuous areas of inflammation separated by healthy tissue, a hallmark feature of **Crohn's disease**.
- **Ulcerative colitis** (implied by the superficial inflammation) is characterized by continuous inflammation extending proximally from the rectum without skipped areas.
*Fistulas and strictures*
- **Fistulas** (abnormal connections between organs or to the skin) and **strictures** (narrowing of the intestinal lumen) are complications typically associated with **Crohn's disease**, due to its **transmural inflammation**.
- These are rare in **ulcerative colitis**, which primarily affects the superficial layers of the colon.
*Noncaseating granuloma*
- The presence of **noncaseating granulomas** on biopsy is a key histological feature distinguishing **Crohn's disease** from ulcerative colitis.
- The inflammation described as restricted to the **mucosa and submucosa** makes granulomas less likely, as they often imply a transmural process.
Surgical management in IBD US Medical PG Question 5: A 32-year-old man comes to the emergency department because of recurrent episodes of vomiting for 1 day. He has had over 15 episodes of bilious vomiting. During this period he has had cramping abdominal pain but has not had a bowel movement or passed flatus. He does not have fever or diarrhea. He was diagnosed with Crohn disease at the age of 28 years which has been well controlled with oral mesalamine. He underwent a partial small bowel resection for midgut volvulus at birth. His other medications include vitamin B12, folic acid, loperamide, ferrous sulfate, and vitamin D3. He appears uncomfortable and his lips are parched. His temperature is 37.1°C (99.3°F), pulse is 103/min, and blood pressure is 104/70 mm Hg. The abdomen is distended, tympanitic, and tender to palpation over the periumbilical area and the right lower quadrant. Rectal examination is unremarkable. A CT scan of the abdomen shows multiple dilated loops of small bowel with a transition zone in the mid to distal ileum. After 24 hours of conservative management with IV fluid resuscitation, nasogastric bowel decompression, promethazine, and analgesia, his condition does not improve and a laparotomy is scheduled. During the laparotomy, two discrete strictures are noted in the mid-ileum, around 20 cm apart. Which of the following is the most appropriate next step in management?
- A. Small bowel resection with ileostomy
- B. Abdominal closure and start palliative care
- C. Small bowel resection and primary anastomosis
- D. Strictureplasty of individual strictures (Correct Answer)
- E. Ileocolectomy
Surgical management in IBD Explanation: ***Strictureplasty of individual strictures***
- This patient presents with **multiple strictures** in the mid-ileum causing a small bowel obstruction in the setting of **Crohn's disease**. Strictureplasty is the preferred surgical approach for *short, multiple (up to four), or recurrent Crohn's disease strictures* as it preserves bowel length.
- While small bowel resection is an option, **strictureplasty** is favored in Crohn's disease to *avoid short bowel syndrome*, especially if multiple strictures are present, as seen here.
*Small bowel resection with ileostomy*
- An ileostomy is typically created when a primary anastomosis is not safe due to high risk of leak (e.g., severe inflammation, peritonitis, patient instability) or when there is extensive disease not amenable to strictureplasty with primary anastomosis.
- Performing an ileostomy when primary anastomosis is possible unnecessarily creates a stoma, which can lead to complications and impact quality of life.
*Abdominal closure and start palliative care*
- This patient, while acutely unwell, has a surgically correctable cause for his obstruction and is not described as having an incurable or end-stage condition necessitating only palliative care.
- Palliative care would be considered for patients with widespread untreatable disease or severe comorbidities, which is not indicated here given the localized, treatable strictures.
*Small bowel resection and primary anastomosis*
- While small bowel resection is a valid treatment for isolated, non-recurrent strictures, strictureplasty is generally preferred in Crohn's disease when multiple strictures are present.
- **Resection of multiple segments** can lead to significant **short bowel syndrome**, especially in a patient with a history of prior small bowel resection, making strictureplasty a more bowel-sparing and appropriate choice.
*Ileocolectomy*
- **Ileocolectomy** involves resection of the terminal ileum and a portion of the colon. This would be indicated if the disease involves the *ileocecal valve region* or the *colon*, which is not the case in this patient, whose strictures are in the mid-ileum.
- This procedure is excessive for mid-ileal strictures and would result in unnecessary removal of healthy bowel given the location of the strictures.
Surgical management in IBD US Medical PG Question 6: A 56-year-old woman is one week status post abdominal hysterectomy when she develops a fever of 101.4°F (38.6°C). Her past medical history is significant for type II diabetes mellitus and a prior history of alcohol abuse. The operative report and intraoperative cystoscopy indicate that the surgery was uncomplicated. The nurse reports that since the surgery, the patient has also complained of worsening lower abdominal pain. She has given the patient the appropriate pain medications with little improvement. The patient has tolerated an oral diet well and denies nausea, vomiting, or abdominal distension. Her blood pressure is 110/62 mmHg, pulse is 122/min, and respirations are 14/min. Since being given 1000 mL of intravenous fluids yesterday, the patient has excreted 800 mL of urine. On physical exam, she is uncomfortable, shivering, and sweating. The surgical site is intact, but the surrounding skin appears red. No drainage is appreciated. The abdominal examination reveals tenderness to palpation and hypoactive bowel sounds. Labs and a clean catch urine specimen are obtained as shown below:
Leukocyte count and differential:
Leukocyte count: 18,000/mm^3
Segmented neutrophils: 80%
Bands: 10%
Eosinophils: 1%
Basophils: < 1%
Lymphocytes: 5%
Monocytes: 4%
Platelet count: 300,000/mm^3
Hemoglobin: 12.5 g/dL
Hematocrit: 42%
Urine:
Epithelial cells: 15/hpf
Glucose: positive
RBC: 1/hpf
WBC: 2/hpf
Bacteria: 50 cfu/mL
Ketones: none
Nitrites: negative
Leukocyte esterase: negative
Which of the following is most likely the cause of this patient’s symptoms?
- A. Surgical error
- B. Post-operative ileus
- C. Wound infection (Correct Answer)
- D. Alcohol withdrawal
- E. Urinary tract infection
Surgical management in IBD Explanation: ***Wound infection***
- The patient presents with **fever**, worsening **lower abdominal pain**, **tachycardia**, and **local signs of inflammation** (redness around the surgical site, tenderness) one week post-hysterectomy, with a **leukocytosis and left shift** (elevated neutrophils and bands). These findings are highly characteristic of a common **post-surgical wound infection**.
- The lack of significant drainage initially does not rule out infection, and the symptoms are localized to the surgical area.
*Surgical error*
- The operative report and intraoperative cystoscopy indicated the surgery was **uncomplicated**, making an immediate post-operative surgical error less likely to be the primary cause of these symptoms.
- While complications can arise later, the current presentation points more directly to an infectious process rather than an unnoted immediate surgical complication.
*Post-operative ileus*
- Although bowel sounds are hypoactive, the patient is **tolerating an oral diet well** and denies nausea, vomiting, or abdominal distension, which are key symptoms of a clinically significant ileus.
- Her primary complaint is localized pain and systemic signs of infection, rather than generalized abdominal distension and inability to pass flatus or stool.
*Alcohol withdrawal*
- While the patient has a history of alcohol abuse, the primary symptoms (fever, localized abdominal pain, redness around the incision, leukocytosis) are more indicative of an **infectious process** than alcohol withdrawal.
- Alcohol withdrawal typically presents with tremors, agitation, hallucinations, and autonomic instability, and while some overlap (tachycardia) exists, the overall clinical picture doesn't fit.
*Urinary tract infection*
- The urine analysis shows **negative nitrites and leukocyte esterase**, with only 2 WBC/hpf, which makes a **urinary tract infection (UTI) highly unlikely** despite the presence of some bacteria (50 cfu/mL, which is often considered contamination in a clean catch).
- The patient's symptoms are also predominantly localized to the surgical wound area rather than dysuria, frequency, or urgency.
Surgical management in IBD US Medical PG Question 7: A 22-year-old man presents to the emergency department with abdominal pain. The patient states that he has had right lower quadrant abdominal pain for "a while now". The pain comes and goes, and today it is particularly painful. The patient is a college student studying philosophy. He drinks alcohol occasionally and is currently sexually active. He states that sometimes he feels anxious about school. The patient's father died of colon cancer at the age of 55, and his mother died of breast cancer when she was 57. The patient has a past medical history of anxiety and depression which is not currently treated. Review of systems is positive for bloody diarrhea. His temperature is 99.5°F (37.5°C), blood pressure is 100/58 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is within normal limits. Abdominal exam reveals diffuse tenderness. A fecal occult blood test is positive. Which of the following is the most likely diagnosis?
- A. Irritable bowel syndrome
- B. Colon cancer
- C. Appendicitis
- D. Infectious colitis
- E. Inflammatory bowel disease (IBD) (Correct Answer)
Surgical management in IBD Explanation: ***Inflammatory bowel disease (IBD)***
- The patient's presentation with **recurrent right lower quadrant pain**, **bloody diarrhea**, a **positive fecal occult blood test**, and a family history concerning for GI issues (colon cancer in father) in a young adult is highly suggestive of IBD, specifically **Crohn's disease** due to the RLQ pain location.
- His history of anxiety and depression is common in IBD patients, and the elevated pulse with mild hypotension suggests **volume depletion** from bloody diarrhea, a common complication.
*Irritable bowel syndrome*
- While IBS can cause recurrent abdominal pain, it is characterized by **functional bowel changes** and typically does not present with **bloody diarrhea** or a positive fecal occult blood test.
- IBS symptoms are often relieved by defecation and are not usually associated with significant systemic inflammation or blood loss.
*Colon cancer*
- Colon cancer is less likely in a **22-year-old** presenting with these acute symptoms, despite the family history, as it typically affects older individuals.
- While it can cause bloody stools and abdominal pain, the **recurrent nature** and acute presentation with bloody diarrhea are more classic for IBD in this age group.
*Appendicitis*
- Appendicitis presents with acute, **migratory right lower quadrant pain** that typically progresses and worsens over hours to a day, often with fever and leukocytosis.
- The given history of pain for "**a while now**" and bloody diarrhea makes appendicitis an unlikely primary diagnosis.
*Infectious colitis*
- Infectious colitis can cause abdominal pain and bloody diarrhea, but it's usually **acute in onset** without a long history of recurrent symptoms.
- While possible, the **recurrent nature** of the pain and bloody diarrhea for "**a while now**" makes a chronic condition like IBD more probable.
Surgical management in IBD US Medical PG Question 8: A 32-year-old man with Crohn disease is brought to the emergency department after he fainted at work. He says that he has been feeling increasingly fatigued and weak over the last several weeks though he has not previously had any episodes of syncope. On presentation he is found to be pale and agitated. A panel of lab tests is performed showing the following:
Hemoglobin: 10.2 g/dL
Hematocrit: 30.1%
Leukocyte count: 9,900 cells/mm^3 with normal differential
Platelet count: 290,000/mm^3
Mean corpuscular volume: 118 µm^3
Elevated homocysteine level
Normal methylmalonic acid level
Which of the following mechanisms explains how Crohn disease may have contributed to this patient's symptoms?
- A. Gastrointestinal blood loss
- B. Inflammation of the ileum
- C. Inflammation of the jejunum (Correct Answer)
- D. Release of acute phase proteins
- E. Inflammation of the duodenum
Surgical management in IBD Explanation: ***Inflammation of the jejunum***
- The patient's **macrocytic anemia** (MCV 118 fL) with **elevated homocysteine** and **normal methylmalonic acid** points to a **folate deficiency**.
- **Folate** is primarily absorbed in the **proximal small intestine**, particularly the **jejunum**; inflammation in this segment due to Crohn's disease would impair its absorption, leading to deficiency.
- While Crohn's disease classically affects the **terminal ileum**, it can involve any part of the GI tract, and **jejunal involvement** would specifically impair folate absorption.
*Gastrointestinal blood loss*
- Chronic gastrointestinal blood loss typically causes **microcytic anemia** due to iron deficiency, not the macrocytic anemia seen here.
- While Crohn's can cause bleeding, the **elevated homocysteine with normal methylmalonic acid** is specific for **folate deficiency**, not blood loss.
*Inflammation of the ileum*
- **Ileal inflammation** is the most common location in Crohn disease and primarily affects the absorption of **vitamin B12** and **bile salts**.
- **Vitamin B12 deficiency** would cause elevated **both homocysteine and methylmalonic acid** levels, which contradicts the normal methylmalonic acid observed in this patient.
*Release of acute phase proteins*
- **Acute phase proteins** are markers of inflammation and contribute to **anemia of chronic disease**, which is typically **normocytic** or mildly **microcytic**.
- This mechanism does not explain the **macrocytic anemia** with the specific biochemical pattern of elevated homocysteine and normal methylmalonic acid, which indicates **folate deficiency**.
*Inflammation of the duodenum*
- The **duodenum** is the primary site for **iron absorption**, though it also participates in **folate absorption** along with the jejunum.
- However, inflammation here would more likely lead to **iron deficiency anemia** (microcytic), and duodenal involvement is **less common** in Crohn disease compared to terminal ileal or jejunal disease.
- The clinical picture is most consistent with **jejunal inflammation** causing isolated folate malabsorption.
Surgical management in IBD US Medical PG Question 9: A 28-year-old woman comes to the physician because of a 2-month history of multiple right inframammary lumps. They are tender and have a foul-smelling odor. She has had previous episodes of painful swellings in the axillae 12 months ago that resolved with antibiotic therapy, leaving some scarring. She has Crohn disease. Menses occur at irregular 18- to 40-day intervals and last 1–5 days. The patient's only medication is mesalamine. She appears anxious. She is 162 cm (5 ft 4 in) tall and weighs 87 kg (192 lb); BMI is 33 kg/m2. Vital signs are within normal limits. Examination of the right inframammary fold shows multiple tender, erythematous nodules and fistulas with purulent discharge. Hirsutism is present. Her fasting glucose concentration is 136 mg/dL. Which of the following areas is most likely to also be affected by this patient's condition?
- A. Forehead
- B. Back
- C. Shin
- D. Central face
- E. Groin (Correct Answer)
Surgical management in IBD Explanation: ***Groin***
- The patient's presentation with recurrent tender, foul-smelling lumps in the **inframammary fold** and past episodes in the **axillae**, along with scarring, strongly suggests **hidradenitis suppurativa (HS)**. HS commonly affects areas with a high density of apocrine glands, including the **axillae, groin, inframammary folds**, and anogenital region.
- Her history of **Crohn disease**, obesity (BMI 33 kg/m²), and possible insulin resistance (fasting glucose 136 mg/dL) are all associated risk factors for HS. The groin is another typical site for lesions.
*Forehead*
- The forehead is generally considered part of the **T-zone of the face**, where sebaceous glands are abundant, but it is not a primary site for *hidradenitis suppurativa*.
- Lesions in this area are more commonly associated with **acne vulgaris** or other folliculitis, which typically present differently.
*Back*
- While the back can be affected by various follicular conditions like **acne inversa** or folliculitis, it is not a primary or highly characteristic site for the deep, painful, and recurring lesions of *hidradenitis suppurativa* in the way intertriginous areas are.
- The specific pattern of involvement in **skin folds** points away from the broader back area as an equally likely site.
*Shin*
- The shins are not typically affected by *hidradenitis suppurativa* as they lack the high concentration of **apocrine glands** found in the classic affected areas.
- Lesions on the shin are more characteristic of conditions like **erythema nodosum** or other forms of vasculitis, which have different presentations.
*Central face*
- The central face, like the forehead, is rich in **sebaceous glands** and is a common site for conditions like **acne vulgaris** or rosacea.
- However, it is not a typical anatomical location for the characteristic deep, recurrent abscesses and sinus tracts seen in *hidradenitis suppurativa*.
Surgical management in IBD US Medical PG Question 10: A 25-year-old man presents to the emergency department for severe abdominal pain. The patient states that for the past week he has felt fatigued and had a fever. He states that he has had crampy lower abdominal pain and has experienced several bouts of diarrhea. The patient states that his pain is somewhat relieved by defecation. The patient returned from a camping trip 2 weeks ago in the Rocky Mountains. He is concerned that consuming undercooked meats on his trip may have caused this. He admits to consuming beef and chicken cooked over a fire pit. The patient is started on IV fluids and morphine. His temperature is 99.5°F (37.5°C), blood pressure is 130/77 mmHg, pulse is 90/min, respirations are 12/min, and oxygen saturation is 98% on room air. Laboratory studies are ordered and are seen below.
Hemoglobin: 10 g/dL
Hematocrit: 28%
Leukocyte count: 11,500 cells/mm^3 with normal differential
Platelet count: 445,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 102 mEq/L
K+: 4.1 mEq/L
HCO3-: 24 mEq/L
BUN: 24 mg/dL
Glucose: 145 mg/dL
Creatinine: 1.4 mg/dL
Ca2+: 9.6 mg/dL
Erythrocyte sedimentation rate (ESR): 75 mm/hour
Physical exam is notable for a patient who appears to be uncomfortable. Gastrointestinal (GI) exam is notable for abdominal pain upon palpation. Ear, nose, and throat exam is notable for multiple painful shallow ulcers in the patient's mouth. Inspection of the patient's lower extremities reveals a pruritic ring-like lesion. Cardiac and pulmonary exams are within normal limits. Which of the following best describes this patient's underlying condition?
- A. p-ANCA positive autoimmune bowel disease
- B. Transmural granulomas in the bowel (Correct Answer)
- C. Gram-negative microaerophilic organism
- D. Rectal mucosa outpouching
- E. Bowel wall spasticity
Surgical management in IBD Explanation: ***Transmural granulomas in the bowel***
- This patient's symptoms, including **chronic diarrhea**, **abdominal pain relieved by defecation**, **oral ulcers**, **fatigue**, **fever**, and **elevated ESR**, along with a **pruritic ring-like lesion** (suggestive of erythema nodosum, a common extraintestinal manifestation), are highly indicative of **Crohn's disease**.
- **Crohn's disease** is characterized by **transmural inflammation** of any part of the GI tract, often with the formation of **non-caseating granulomas**.
*p-ANCA positive autoimmune bowel disease*
- This describes **ulcerative colitis**, which is typically associated with **p-ANCA positivity** in a subset of patients.
- Unlike the diffuse and continuous inflammation seen in ulcerative colitis, Crohn's disease features **skip lesions** and **transmural inflammation**, which aligns better with the varied symptoms and extraintestinal manifestations presented.
*Gram-negative microaerophilic organism*
- This refers to bacterial infections such as those caused by **Campylobacter jejuni** or **Helicobacter pylori**, which can cause GI symptoms.
- While the patient's camping trip and consumption of undercooked meat might suggest an infectious etiology, the **chronic nature of symptoms** (week-long fatigue and fever), **oral ulcers**, **elevated ESR**, and **erythema nodosum-like lesion** point more strongly towards an autoimmune/inflammatory bowel disease rather than an acute bacterial infection.
*Rectal mucosa outpouching*
- **Diverticula** are outpouchings of the colon, commonly affecting the sigmoid colon, and are typically associated with **diverticulitis** when inflamed.
- This condition does not explain the widespread systemic symptoms, oral ulcers, or the chronic, crampy abdominal pain and diarrhea pattern seen in this patient.
*Bowel wall spasticity*
- **Bowel spasticity** is a feature of **irritable bowel syndrome (IBS)**.
- While IBS can cause crampy abdominal pain and changes in bowel habits, it is a **functional disorder** and does not cause **fever**, **oral ulcers**, **elevated ESR**, or significant **anemia** and **thrombocytosis** as seen in this patient.
More Surgical management in IBD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.