Nutritional considerations in IBD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nutritional considerations in IBD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nutritional considerations in IBD US Medical PG Question 1: A 37-year-old man with Crohn disease is admitted to the hospital because of acute small bowel obstruction. Endoscopy shows a stricture in the terminal ileum. The ileum is surgically resected after endoscopic balloon dilatation fails to relieve the obstruction. Three years later, he returns for a follow-up examination. He takes no medications. This patient is most likely to have which of the following physical exam findings?
- A. Dry skin and keratomalacia
- B. Weakness and ataxia (Correct Answer)
- C. Hyperreflexia with tetany
- D. Gingival swelling and bleeding
- E. Pallor with koilonychia
Nutritional considerations in IBD Explanation: ***Weakness and ataxia***
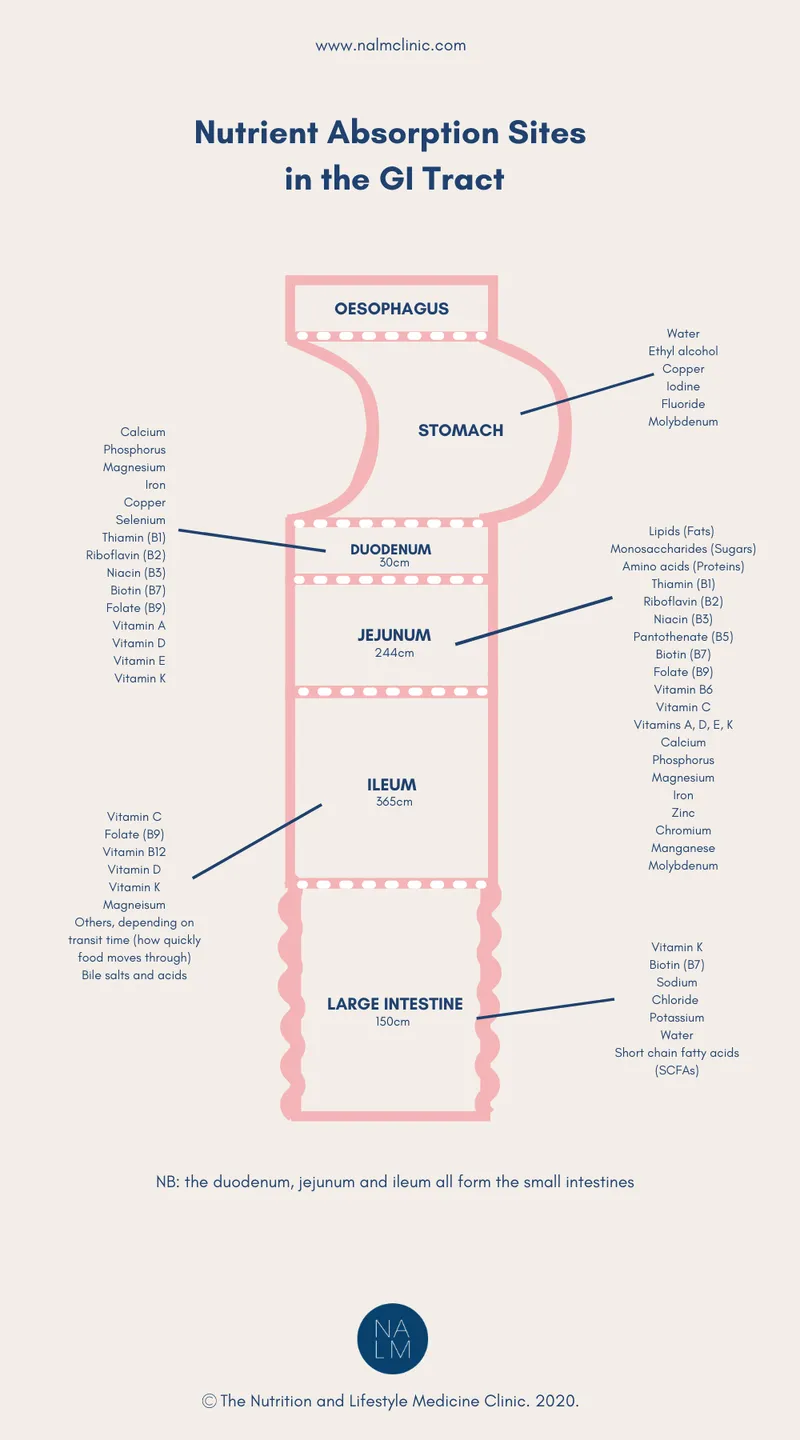
- This patient with a history of **Crohn disease** and significant **ileal resection** is at high risk for **vitamin B12 deficiency** due to the removal of the primary site of absorption in the terminal ileum.
- **Vitamin B12 deficiency** can lead to subacute combined degeneration of the spinal cord, manifesting as **weakness**, **ataxia**, and **paresthesias**.
*Dry skin and keratomalacia*
- This presentation is indicative of **vitamin A deficiency**, which can occur in malabsorption but is less specific to ileal resection than B12 deficiency.
- While fat-soluble vitamins (A, D, E, K) are absorbed in the small intestine, severe isolated vitamin A deficiency causing keratomalacia is not the most likely primary finding after ileal resection.
*Hyperreflexia with tetany*
- These symptoms typically suggest **hypocalcemia** or **hypomagnesemia**, often due to vitamin D deficiency or malabsorption of minerals.
- Although possible with generalized malabsorption, it is not the most characteristic neurological complication following isolated ileal resection compared to vitamin B12 deficiency.
*Gingival swelling and bleeding*
- This is a hallmark of **scurvy**, caused by **vitamin C deficiency**, which is typically absorbed in the small intestine and does not correlate specifically with ileal resection.
- This would be a less likely complication given the specific history compared to micronutrient deficiencies related to terminal ileum function.
*Pallor with koilonychia*
- **Pallor** and **koilonychia (spoon nails)** are characteristic signs of **iron deficiency anemia**.
- While iron is absorbed in the duodenum and proximal jejunum, and anemia is common in Crohn disease, the specific neurological symptoms from B12 deficiency are generally more prominent after ileal resection.
Nutritional considerations in IBD US Medical PG Question 2: A 4-month-old boy is brought to the physician by his parents for a well-child examination. He has cystic fibrosis diagnosed by newborn screening. His parents report frequent feedings and large-volume and greasy stools. His 4-year-old brother has autism. Current medications include bronchodilators, pancreatic enzyme supplements, and fat-soluble vitamins. He is at the 18th percentile for height and 15th percentile for weight. Scattered wheezes are heard throughout both lung fields. Examination shows a distended and tympanic abdomen with no tenderness or guarding. Which of the following is a contraindication for administering one or more routine vaccinations?
- A. Allergy to egg protein
- B. History of cystic fibrosis
- C. History of febrile seizures
- D. Fever of 38.2°C (100.7°F) following previous vaccinations
- E. History of intussusception (Correct Answer)
Nutritional considerations in IBD Explanation: ***History of intussusception***
- A history of **intussusception** is a **contraindication for rotavirus vaccine** administration, as the vaccine itself has a small risk of intussusception, particularly with the first dose.
- The rotavirus vaccine is part of routine childhood immunizations, so this would be a contraindication for one of the routine vaccines.
*Allergy to egg protein*
- Egg allergy is a contraindication primarily for yellow fever vaccine and some influenza vaccines, which are typically not routine vaccinations for a 4-month-old. Many flu vaccines are egg-free or can be safely administered to those with egg allergy under supervision.
- The MMR vaccine is generally safe for those with egg allergy since the amount of egg protein is negligible.
*History of cystic fibrosis*
- **Cystic fibrosis** itself is **not a contraindication** to routine vaccinations; in fact, patients with chronic conditions like CF are often *more* encouraged to receive vaccinations to prevent severe infections.
- The patient's symptoms (poor growth, greasy stools, wheezing) are manifestations of CF, not reasons to defer vaccination.
*History of febrile seizures*
- A history of **febrile seizures** is generally **not a contraindication** to routine vaccinations.
- Parents should be counseled on fever management after vaccination, but the risk of recurrent febrile seizures is not increased by vaccination to a level that warrants deferral.
*Fever of 38.2°C (100.7°F) following previous vaccinations*
- A **low-grade fever** after vaccination is a common and **expected immune response**, not a contraindication for future doses.
- Only a **severe allergic reaction** (e.g., anaphylaxis) to a previous dose of a vaccine or one of its components is a contraindication to subsequent doses of that specific vaccine.
Nutritional considerations in IBD US Medical PG Question 3: A 42-year-old man with a history of tuberculosis presents to your office complaining of fatigue for two months. Serum laboratory studies reveal the following: WBC 7,000 cells/mm^3, Hb 9.0 g/dL, Hct 25%, MCV 88 fL, Platelet 450,000 cells/mm^3, Vitamin B12 500 pg/mL (200-800), and Folic acid 17 ng/mL (2.5-20). Which of the following is the most appropriate next step in the management of anemia in this patient?
- A. Iron studies (Correct Answer)
- B. Bone marrow biopsy
- C. Observation
- D. Colonoscopy
- E. Erythropoietin administration
Nutritional considerations in IBD Explanation: ***Iron studies***
- The patient has **normocytic anemia** (MCV 88 fL) and a history of **tuberculosis**, which is a chronic inflammatory condition often associated with **anemia of chronic disease (ACD)**.
- **Iron studies** are critical to differentiate between **ACD** (typically high ferritin, low transferrin saturation) and iron deficiency anemia, which can coexist.
*Bone marrow biopsy*
- A **bone marrow biopsy** is an invasive procedure and is typically reserved for cases of unexplained severe anemia, pancytopenia, or suspicion of primary bone marrow disorders that are not suggested by the current findings.
- The current blood counts do not indicate an urgent need for bone marrow evaluation, as the **anemia is mild to moderate**, and other cell lines are normal (WBC) or elevated (platelets).
*Erythropoietin administration*
- **Erythropoietin administration** is used in specific anemias, such as **anemia of chronic kidney disease** or certain types of myelodysplastic syndromes.
- It is not the initial step for diagnosing and managing anemia in a patient with a chronic inflammatory condition like tuberculosis without first assessing iron status or ruling out other treatable causes.
*Observation*
- **Observation** is inappropriate given the patient's symptomatic anemia (fatigue) and the identified abnormalities (Hb 9.0 g/dL).
- Anemia warrants investigation to identify its cause and provide appropriate treatment, especially in the context of a chronic illness like tuberculosis.
*Colonoscopy*
- A **colonoscopy** is indicated if there is suspicion of **gastrointestinal blood loss**, which typically presents with **microcytic anemia** (low MCV) due to chronic iron deficiency.
- This patient has **normocytic anemia**, and there are no symptoms suggestive of GI bleeding, making colonoscopy not the most appropriate first step.
Nutritional considerations in IBD US Medical PG Question 4: A 65-year-old gentleman presents to his primary care physician for difficulties with his gait and recent fatigue. The patient works in a health food store, follows a strict vegan diet, and takes an array of supplements. He noticed that his symptoms have progressed over the past year and decided to see a physician when he found himself feeling abnormally weak on a daily basis in conjunction with his trouble walking. The patient has a past medical history of Crohn's disease, diagnosed in his early 20's, as well as Celiac disease. He states that he has infrequent exacerbations of his Crohn's disease. Recently, the patient has been having worsening bouts of diarrhea that the patient claims is non-bloody. The patient is not currently taking any medications and is currently taking traditional Chinese medicine supplements. Physical exam is notable for 3/5 strength in the upper and lower extremities, absent upper and lower extremity reflexes, and a staggering, unbalanced gait. Laboratory values reveal the following:
Serum:
Na+: 135 mEq/L
Cl-: 100 mEq/L
K+: 5.6 mEq/L
HCO3-: 22 mEq/L
BUN: 27 mg/dL
Glucose: 79 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 8.4 mg/dL
Mg2+: 1.5 mEq/L
Leukocyte count and differential:
Leukocyte count: 4,522/mm^3
Hemoglobin: 9.2 g/dL
Hematocrit: 29%
Platelet count: 169,000/mm^3
Reticulocyte count: 2.5%
Lactate dehydrogenase: 340 U/L
Mean corpuscular volume: 97 fL
Which of the following is most likely deficient in this patient?
- A. Vitamin D
- B. Iron
- C. Vitamin B9
- D. Vitamin E
- E. Vitamin B12 (Correct Answer)
Nutritional considerations in IBD Explanation: ***Vitamin B12***
- The patient's **vegan diet**, history of **Crohn's disease**, **Celiac disease**, and **diarrhea** all increase the risk of **vitamin B12 malabsorption**.
- **Neurological symptoms** like gait difficulties, weakness, and absent reflexes are characteristic of **vitamin B12 deficiency**, which can also cause **anemia** with a **normal MCV** (masked by co-existing iron deficiency or thalassemia trait).
*Vitamin D*
- While common in patients with malabsorption conditions like Crohn's disease and Celiac disease, **vitamin D deficiency** primarily presents with **bone pain**, **muscle weakness**, and **osteoporosis**, not the prominent neurological findings seen here.
- The patient's **calcium level (8.4 mg/dL)** is at the lower end of normal, but not overtly hypocalcemic, which would be expected with severe vitamin D deficiency.
*Iron*
- **Iron deficiency** is common in Crohn's and Celiac disease due to malabsorption and chronic blood loss, leading to **microcytic anemia** and **fatigue**.
- However, the patient's **MCV is normal (97 fL)**, and iron deficiency does not typically explain the **neurological symptoms** (gait difficulties, absent reflexes) described.
*Vitamin B9*
- **Folate deficiency** can cause **megaloblastic anemia** and fatigue, similar to vitamin B12 deficiency, but it is less likely to cause the **severe neurological symptoms** seen here.
- While malabsorption conditions can affect folate, the specific neurological presentation points more strongly towards B12.
*Vitamin E*
- **Vitamin E deficiency** can cause **neurological symptoms** such as ataxia, peripheral neuropathy, and muscle weakness due to its role as an antioxidant.
- However, deficiency is rare in adults and usually severe malabsorption of fats from conditions like abetalipoproteinemia. While Crohn's and Celiac can cause fat malabsorption, the constellation of symptoms, including anemia and masked MCV, aligns more directly with B12.
Nutritional considerations in IBD US Medical PG Question 5: An 11-month-old boy is brought to a pediatrician by his parents for evaluation of vomiting and watery diarrhea over the last day. The mother informs the pediatrician that the boy had consumed an apple bought from a fruit vendor on the previous day, but that otherwise there has been no recent change in his diet. There is no history of blood in the stool, flatulence, irritability, or poor appetite. There is no history of recurrent or chronic diarrhea or any other gastrointestinal symptoms. On physical examination, his temperature is 37.6°C (99.6°F), pulse is 120/min, respirations are 24/min, and blood pressure is 92/60 mm Hg. General examination reveals a playful infant with normal skin turgor and no sunken eyes. The pediatrician explains to the parents that he most likely has acute gastroenteritis and that no specific medication is indicated at present. He also instructs the parents about his diet during the illness and reviews the danger signs of dehydration. He suggests a follow-up evaluation after 48 hours or earlier if any complications arise. Which of the following dietary recommendations did the pediatrician make?
- A. Plenty of juices and carbonated sodas
- B. Age-appropriate diet (Correct Answer)
- C. Diluted formula milk
- D. Lactose-free diet
- E. BRAT diet
Nutritional considerations in IBD Explanation: ***Age-appropriate diet***
- For **mild acute gastroenteritis** without significant dehydration, the latest recommendations advise continuing **age-appropriate feeding** to support nutritional requirements and promote gut recovery.
- This approach helps to prevent malnutrition and does not prolong the course of diarrhea.
*Plenty of juices and carbonated sodas*
- **High sugar content** in juices and sodas can worsen diarrhea due to their **osmotic effect**, drawing more water into the intestine.
- These beverages also lack essential **electrolytes** needed for rehydration.
*Diluted formula milk*
- Diluting formula can lead to **insufficient caloric intake** and nutritional deficiencies, which is generally not recommended for mild gastroenteritis.
- Undiluted formula is usually well-tolerated, as most infants with acute gastroenteritis do not develop significant **lactose intolerance**.
*Lactose-free diet*
- Routine use of **lactose-free diets** is generally not recommended unless there is strong evidence of **secondary lactase deficiency**, which typically presents with increased flatulence, bloating, and worsening diarrhea.
- The majority of children with acute gastroenteritis can tolerate their usual milk intake.
*BRAT diet*
- The **B**ananas, **R**ice, **A**pplesauce, **T**oast (BRAT) diet is **nutritionally restrictive**, providing inadequate protein and fat, which can hinder recovery and growth in infants.
- Current guidelines no longer recommend the BRAT diet for acute gastroenteritis.
Nutritional considerations in IBD US Medical PG Question 6: A 24-year-old man presents to the emergency department complaining of a prolonged course of diarrhea. He reports that he has had 3–4 large volume watery stools daily for the last several weeks. He has no pain with bowel movements, no abdominal pain, and no blood in his stools. He is homeless and uses recreational drugs. He also reports that he usually drinks a half-liter of whiskey, or whatever else he can find, every day and he has done this for several years. The physical exam is notable for a hyperpigmented rash across his face, neck, chest, and the backs of his hands and forearms. On mental status exam, he is oriented to person and place but not time; he scores a 23/30 on the Montreal Cognitive Assessment (MOCA). This patient's presentation is most likely related to which of the following micronutrients?
- A. Vitamin B2
- B. Vitamin B12
- C. Vitamin D
- D. Vitamin C
- E. Vitamin B3 (Correct Answer)
Nutritional considerations in IBD Explanation: ***Vitamin B3***
- The patient's symptoms—diarrhea, dermatitis (hyperpigmented rash), and dementia (disorientation to time, MOCA 23/30)—are the classic **3 Ds of pellagra**, which is caused by a **vitamin B3 (niacin) deficiency**.
- His chronic alcohol use and poor nutritional status (homelessness, recreational drug use) put him at high risk for such a deficiency, as alcohol impairs nutrient absorption and niacin is often lacking in the diets of those with limited food access.
*Vitamin B2*
- Deficiency in **vitamin B2 (riboflavin)** typically presents with cheilosis, angular stomatitis, glossitis, seborrheic dermatitis, and ocular symptoms like corneal vascularization, none of which are specifically mentioned here.
- While chronic alcohol use can also cause riboflavin deficiency, the patient's full symptom complex points more strongly to pellagra.
*Vitamin B12*
- **Vitamin B12 deficiency** often leads to **macrocytic anemia**, neurological symptoms including peripheral neuropathy, ataxia, and cognitive impairment, and glossitis, but it does not typically cause the characteristic dermatologic rash or diarrhea seen in this patient.
- While chronic alcohol use is a risk factor, the specific triad of diarrhea, dermatitis, and dementia is not consistent with B12 deficiency.
*Vitamin D*
- **Vitamin D deficiency** is associated with bone health issues (rickets in children, osteomalacia in adults), muscle weakness, and in severe cases, hypocalcemia.
- It does not present with the specific combination of diarrhea, hyperpigmented rash, and cognitive changes described in the patient.
*Vitamin C*
- **Vitamin C deficiency (scurvy)** typically manifests as perifollicular hyperkeratosis, bleeding gums, petechiae, impaired wound healing, and musculoskeletal pain.
- While malnourishment and alcohol abuse increase the risk of scurvy, the patient's symptoms do not align with the classic presentation of vitamin C deficiency.
Nutritional considerations in IBD US Medical PG Question 7: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Nutritional considerations in IBD Explanation: ***Start annual colonoscopy starting in 8 years***
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Nutritional considerations in IBD US Medical PG Question 8: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Nutritional considerations in IBD Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
Nutritional considerations in IBD US Medical PG Question 9: A 19-year-old woman comes to the physician because of a 1-year history of severe abdominal pain, bloating, and episodic diarrhea. She also has a 10-kg (22-lb) weight loss over the past 10 months. Physical examination shows a mildly distended abdomen, diffuse abdominal tenderness, and multiple erythematous, tender nodules on the anterior aspect of both legs. There is a small draining lesion in the perianal region. Further evaluation of this patient's gastrointestinal tract is most likely to show which of the following findings?
- A. Transmural inflammation (Correct Answer)
- B. Melanosis coli
- C. Villous atrophy
- D. Crypt abscesses
- E. No structural abnormalities
Nutritional considerations in IBD Explanation: **Transmural inflammation**
- The patient's symptoms (abdominal pain, bloating, diarrhea, weight loss) and extraintestinal manifestations (erythematous nodules, perianal lesion) are classic for **Crohn's disease**.
- A hallmark pathological feature of Crohn's disease is **transmural inflammation**, affecting all layers of the bowel wall, which can lead to complications like strictures, fistulas, and abscesses.
*Melanosis coli*
- This is a harmless condition characterized by **pigmentation of the colonic mucosa** due to chronic laxative use, particularly **anthraquinone laxatives**.
- It is not associated with inflammatory bowel disease or the systemic symptoms described.
*Villous atrophy*
- **Villous atrophy** is the flattening of the villi in the small intestine, most commonly seen in **celiac disease**.
- While celiac disease can cause malabsorption and gastrointestinal symptoms, the extraintestinal manifestations and perianal draining lesion are inconsistent with celiac disease.
*Crypt abscesses*
- **Crypt abscesses** are a characteristic histological finding in **ulcerative colitis**, which primarily affects the colon and rectum.
- While ulcerative colitis, like Crohn's, is an inflammatory bowel disease, the presence of transmural inflammation and perianal disease (fistulas/draining lesions) is more indicative of Crohn's.
*No structural abnormalities*
- The severe symptoms, significant weight loss, and presence of extraintestinal manifestations (erythema nodosum, perianal disease) strongly suggest an underlying structural and inflammatory pathology in the GI tract.
- **Irritable Bowel Syndrome (IBS)** typically presents with similar symptoms but lacks structural abnormalities and the systemic inflammatory signs seen here.
Nutritional considerations in IBD US Medical PG Question 10: A 28-year-old man presents to his primary care provider complaining of intermittent stomach pain, non-bloody diarrhea, and weight loss for the last 3 months. He has occasional abdominal pain and fever. This condition makes studying difficult. He has tried omeprazole and dietary changes with no improvement. Past medical history is significant for occasional pain in the wrists and knees for several years. He takes ibuprofen for pain relief. His temperature is 38°C (100.4°F). On mental status examination, short-term memory is impaired. Attention and concentration are reduced. Examination shows no abnormalities or tenderness of the wrists or knees. There are no abnormalities on heart and lung examinations. Abdominal examination is normal. Upper endoscopy shows normal stomach mucosa but in the duodenum, there is pale yellow mucosa with erythema and ulcerations. Biopsies show infiltration of the lamina propria with periodic acid-Schiff (PAS)-positive macrophages. Which of the following best explains these findings?
- A. Wilson’s disease
- B. Celiac disease
- C. Giardia lamblia infection
- D. Whipple’s disease (Correct Answer)
- E. Crohn’s disease
Nutritional considerations in IBD Explanation: ***Whipple’s disease***
- The combination of **gastrointestinal symptoms** (diarrhea, weight loss, abdominal pain) with **arthralgia**, **fever**, **neurological symptoms** (impaired short-term memory, reduced attention/concentration), and **PAS-positive macrophages** in duodenal biopsies is highly characteristic of Whipple's disease.
- This multisystemic bacterial infection, caused by *Tropheryma whipplei*, often presents with diverse, non-specific symptoms before the classic GI findings, and central nervous system involvement is common.
*Wilson’s disease*
- This is a disorder of **copper metabolism** leading to copper accumulation in organs like the liver, brain, and eyes (Kayser-Fleischer rings).
- While it can cause neurological symptoms and liver disease, the GI and biopsy findings (PAS-positive macrophages) are not consistent with Wilson's disease.
*Celiac disease*
- Characterized by **malabsorption** due to an immune reaction to gluten, presenting with diarrhea, weight loss, and abdominal pain.
- However, jejunal biopsies would show **villous atrophy** and crypt hyperplasia, not PAS-positive macrophages, and neurological findings are less common and typically peripheral in nature.
*Giardia lamblia infection*
- This parasitic infection causes **diarrhea**, abdominal cramps, and malabsorption.
- Diagnosis is usually made by identifying **trophozoites or cysts** in stool samples or duodenal aspirates/biopsies, not PAS-positive macrophages.
*Crohn’s disease*
- An **inflammatory bowel disease** characterized by transmural inflammation, skip lesions, and granulomas, which can affect any part of the GI tract.
- While it can present with abdominal pain, diarrhea, weight loss, and arthralgia, the presence of **PAS-positive macrophages** in the duodenum and neurological involvement are not typical features of Crohn's disease.
More Nutritional considerations in IBD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.