Medical management of ulcerative colitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Medical management of ulcerative colitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Medical management of ulcerative colitis US Medical PG Question 1: A 22-year-old woman comes to the physician because of abdominal pain and diarrhea for 2 months. The pain is intermittent, colicky and localized to her right lower quadrant. She has anorexia and fears eating due to the pain. She has lost 4 kg (8.8 lb) during this time. She has no history of a serious illness and takes no medications. Her temperature is 37.8°C (100.0°F), blood pressure 125/65 mm Hg, pulse 75/min, and respirations 14/min. An abdominal examination shows mild tenderness of the right lower quadrant on deep palpation without guarding. Colonoscopy shows small aphthous-like ulcers in the right colon and terminal ileum. Biopsy from the terminal ileum shows noncaseating granulomas in all layers of the bowel wall. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Budesonide (Correct Answer)
- B. Azathioprine
- C. Ciprofloxacin
- D. Metronidazole
- E. Rectal mesalamine
Medical management of ulcerative colitis Explanation: ***Budesonide***
- This patient presents with symptoms and findings (RLQ pain, aphthous ulcers, noncaseating granulomas in the terminal ileum) consistent with **Crohn's disease** isolated to the **ileum and right colon**.
- **Budesonide** is a glucocorticoid with high first-pass metabolism, making it effective for localized ileal and right colonic Crohn's disease with fewer systemic side effects than prednisone.
*Azathioprine*
- **Azathioprine** is an immunomodulator used for maintaining remission in moderate to severe Crohn's disease, not typically for acute exacerbations as first-line monotherapy.
- Its onset of action is slow (several weeks to months), making it unsuitable for immediate symptom control.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic mainly used when there is concern for bacterial overgrowth, abscess, or perianal disease in Crohn's, none of which are explicitly indicated here.
- There is no evidence suggesting a primary bacterial infection as the cause of her current symptoms.
*Metronidazole*
- **Metronidazole** is an antibiotic often used for Crohn's disease with perianal involvement or fistulas, and sometimes for active colonic disease, but less effective for ileal involvement.
- Like ciprofloxacin, it's not the primary treatment for uncomplicated flare of ileocolonic Crohn's.
*Rectal mesalamine*
- **Rectal mesalamine** is an aminosalicylate primarily used for mild to moderate **ulcerative colitis**, particularly proctitis or left-sided colitis due to its topical action.
- It is ineffective for Crohn's disease involving the terminal ileum and right colon, as it would not reach this location in sufficient concentration.
Medical management of ulcerative colitis US Medical PG Question 2: A 55-year-old woman presents with diarrhea and a rash. She reports having some painful reddish nodules on her legs that she noticed a week ago. She also has been having loose stools associated with cramping lower abdominal pain for the past month. This is associated with an urgency to defecate, and defecation helps relieve the abdominal pain. The stool is occasionally blood-tinged and has some mucus. She feels fatigued but denies fever, weight loss, exposure to any sick people, or history of travel recently. No significant past medical history. Her family history is significant for osteoporosis in her mother, aunt, and older sister. On physical examination, the patient has generalized pallor. There are multiple erythematous tender nodules over the extensor surface of the legs bilaterally below the level of the knee. Abdominal examination reveals mild tenderness to palpation in the left lower quadrant. A DEXA scan is performed and reveals a T-score of -1.5 at the hips and spine. Laboratory findings are significant for microcytic anemia and an elevated ESR. A colonoscopy is performed and reveals patchy inflammation of the colon with rectal sparing. The lesions are present in patches with intermittent normal colonic mucosa. The patient is started on sulfasalazine and shows a good response. However, 6 months later, she returns with a recurrence of her symptoms. A repeat colonoscopy reveals more extensive involvement of the colon and the small bowel. A second drug is added to her treatment regimen. Which of the following is the most common adverse effect associated with the use of this second drug?
- A. Hepatotoxicity
- B. Infection (Correct Answer)
- C. Megaloblastic anemia
- D. Worsening of osteoporosis
- E. Rash
Medical management of ulcerative colitis Explanation: ***Infection***
- The patient's presentation with **patchy inflammation** of the colon, rectal sparing, and later small bowel involvement, along with **erythema nodosum** and **microcytic anemia**, is highly suggestive of **Crohn's disease**.
- Given the recurrence and more extensive involvement, it's likely a **biologic agent** (e.g., TNF-alpha inhibitor) or an **immunomodulator** (e.g., methotrexate, azathioprine) was added. These drugs **suppress the immune system**, making **infection** the most common and serious adverse effect.
*Hepatotoxicity*
- While some drugs used in Crohn's disease, such as **methotrexate** or **azathioprine**, can cause hepatotoxicity, it is generally monitored and is less common than infection.
- **Biologics**, which are frequently used for refractory Crohn's, pose a lower risk of hepatotoxicity compared to their immunomodulatory effects.
*Megaloblastic anemia*
- **Megaloblastic anemia** is typically associated with **folate deficiency** (which can be caused by sulfasalazine or methotrexate) or **B12 deficiency** (which can occur in Crohn's affecting the terminal ileum).
- While possible, it is not the most common adverse effect of the second-line agents used to treat Crohn's disease.
*Worsening of osteoporosis*
- **Osteoporosis** is a common comorbidity in Crohn's disease due to chronic inflammation, malabsorption, and corticosteroid use, but it is not a direct adverse effect of most second-line medications.
- While **corticosteroids** can worsen osteoporosis, they are typically used for acute flares, and the newer biologic or immunomodulatory agents do not directly cause bone loss.
*Rash*
- **Rash** can be an adverse effect of many medications, including some used for Crohn's disease like **sulfasalazine** or **biologics**.
- However, **infection** due to immunosuppression is a far more pervasive and common risk across a broader range of the second-line therapies used in Crohn's disease management.
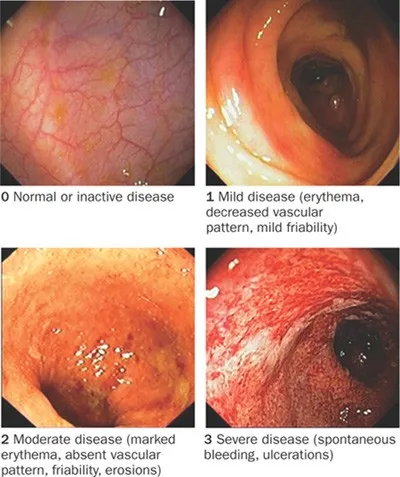
Medical management of ulcerative colitis US Medical PG Question 3: A 31-year-old man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. His vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 87/min, and respiratory rate is 15/min. Rectal examination reveals a small amount of bright red blood. Lower endoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate initial treatment for this patient's underlying disease?
- A. Azathioprine
- B. Mesalamine (Correct Answer)
- C. Systemic corticosteroids
- D. Total proctocolectomy
- E. Sulfasalazine
Medical management of ulcerative colitis Explanation: ***Mesalamine***
- The patient's symptoms (bloody diarrhea, abdominal pain, erythema, pseudopolyps, and inflammation extending from the rectum to the splenic flexure) are highly suggestive of **ulcerative colitis (UC) affecting the left colon (distal colitis)**.
- **Mesalamine** (a 5-aminosalicylic acid or 5-ASA derivative) is the first-line treatment for mild to moderate UC, especially for proctitis and left-sided colitis. Its anti-inflammatory action is exerted topically on the colonic mucosa.
*Azathioprine*
- Azathioprine is an **immunomodulator** used for maintaining remission in UC or in cases where patients are steroid-dependent or refractory to 5-ASAs.
- It is not typically used as a first-line agent for acute, mild to moderate disease.
*Systemic corticosteroids*
- **Systemic corticosteroids** are used for moderate to severe UC or for severe flares, not for initial mild to moderate disease, due to their significant side effect profile.
- While effective in inducing remission, their long-term use is limited, and they are not considered a maintenance therapy.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical option reserved for severe, refractory UC that does not respond to medical therapy, or in cases of dysplasia/cancer.
- It is an invasive procedure and not an appropriate initial treatment for a patient presenting with symptoms of mild to moderate disease.
*Sulfasalazine*
- **Sulfasalazine** is an older 5-ASA compound that is also effective for mild to moderate UC.
- However, it has a **higher incidence of side effects** (e.g., GI upset, headaches, hypersensitivity) compared to mesalamine, making mesalamine generally preferred for better tolerability.
Medical management of ulcerative colitis US Medical PG Question 4: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Medical management of ulcerative colitis Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Medical management of ulcerative colitis US Medical PG Question 5: A 34-year-old woman with no significant prior medical history presents to the clinic with several days of bloody stool. She also complains of constipation and straining, but she has no other symptoms. She has no family history of colorectal cancer or inflammatory bowel disease. She does not smoke or drink alcohol. Her vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 77/min, and respiratory rate is 15/min. There is no abdominal discomfort on physical exam, and a digital rectal exam reveals bright red blood. Of the following, which is the most likely diagnosis?
- A. Colorectal cancer
- B. Ulcerative colitis
- C. Anal fissure
- D. External hemorrhoids
- E. Internal hemorrhoids (Correct Answer)
Medical management of ulcerative colitis Explanation: ***Internal hemorrhoids***
- **Painless bright red blood** per rectum, especially with **constipation and straining**, is highly characteristic of internal hemorrhoids.
- Internal hemorrhoids are located **above the dentate line**, making them typically painless, and they often prolapse during defecation, causing bleeding.
*Colorectal cancer*
- While colorectal cancer can cause bloody stool, it is less likely in a **34-year-old woman with no family history** and no other systemic symptoms like weight loss or abdominal pain.
- The bright red blood associated with straining points away from an upper GI bleed, which is more typical of many colorectal cancers.
*Ulcerative colitis*
- Ulcerative colitis typically presents with bloody diarrhea, abdominal pain, and tenesmus, which are **not mentioned** in this patient's history.
- It is a chronic inflammatory condition, and the isolated symptom of bright red blood with constipation is not classic for UC.
*Anal fissure*
- An anal fissure would cause **severe pain during defecation** due to a tear in the anal canal, which is absent in this patient.
- While an anal fissure can cause bright red blood, the lack of pain makes it less likely than hemorrhoids.
*External hemorrhoids*
- **External hemorrhoids are usually painful or itchy** and located below the dentate line.
- They also can cause bleeding, but the absence of pain and bright red blood suggests internal hemorrhoids which are more likely to bleed painlessly.
Medical management of ulcerative colitis US Medical PG Question 6: A 22-year-old man presents to the emergency department with abdominal pain. The patient states that he has had right lower quadrant abdominal pain for "a while now". The pain comes and goes, and today it is particularly painful. The patient is a college student studying philosophy. He drinks alcohol occasionally and is currently sexually active. He states that sometimes he feels anxious about school. The patient's father died of colon cancer at the age of 55, and his mother died of breast cancer when she was 57. The patient has a past medical history of anxiety and depression which is not currently treated. Review of systems is positive for bloody diarrhea. His temperature is 99.5°F (37.5°C), blood pressure is 100/58 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is within normal limits. Abdominal exam reveals diffuse tenderness. A fecal occult blood test is positive. Which of the following is the most likely diagnosis?
- A. Irritable bowel syndrome
- B. Colon cancer
- C. Appendicitis
- D. Infectious colitis
- E. Inflammatory bowel disease (IBD) (Correct Answer)
Medical management of ulcerative colitis Explanation: ***Inflammatory bowel disease (IBD)***
- The patient's presentation with **recurrent right lower quadrant pain**, **bloody diarrhea**, a **positive fecal occult blood test**, and a family history concerning for GI issues (colon cancer in father) in a young adult is highly suggestive of IBD, specifically **Crohn's disease** due to the RLQ pain location.
- His history of anxiety and depression is common in IBD patients, and the elevated pulse with mild hypotension suggests **volume depletion** from bloody diarrhea, a common complication.
*Irritable bowel syndrome*
- While IBS can cause recurrent abdominal pain, it is characterized by **functional bowel changes** and typically does not present with **bloody diarrhea** or a positive fecal occult blood test.
- IBS symptoms are often relieved by defecation and are not usually associated with significant systemic inflammation or blood loss.
*Colon cancer*
- Colon cancer is less likely in a **22-year-old** presenting with these acute symptoms, despite the family history, as it typically affects older individuals.
- While it can cause bloody stools and abdominal pain, the **recurrent nature** and acute presentation with bloody diarrhea are more classic for IBD in this age group.
*Appendicitis*
- Appendicitis presents with acute, **migratory right lower quadrant pain** that typically progresses and worsens over hours to a day, often with fever and leukocytosis.
- The given history of pain for "**a while now**" and bloody diarrhea makes appendicitis an unlikely primary diagnosis.
*Infectious colitis*
- Infectious colitis can cause abdominal pain and bloody diarrhea, but it's usually **acute in onset** without a long history of recurrent symptoms.
- While possible, the **recurrent nature** of the pain and bloody diarrhea for "**a while now**" makes a chronic condition like IBD more probable.
Medical management of ulcerative colitis US Medical PG Question 7: A 32-year-old man comes to the physician for a follow-up examination. He has a 2-month history of increasing generalized fatigue and severe pruritus. He has hypertension and ulcerative colitis which was diagnosed via colonoscopy 5 years ago. Current medications include lisinopril and rectal mesalamine. He is sexually active with 2 female partners and uses condoms inconsistently. His temperature is 37.3°C (99.1°F), pulse is 86/min, and blood pressure is 130/84 mm Hg. Examination shows scleral icterus and multiple scratch marks on the trunk and extremities. The lungs are clear to auscultation. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.5 g/dL
Leukocyte count 7500/mm3
Platelet count 280,000/mm3
Serum
Na+ 138 mEq/L
Cl- 101 mEq/L
K+ 4.7 mEq/L
Urea nitrogen 18 mg/dL
Glucose 91 mg/dL
Creatinine 0.8 mg/dL
Bilirubin
Total 1.5 mg/dL
Direct 0.9 mg/dL
Alkaline phosphatase 460 U/L
AST 75 U/L
ALT 78 U/L
Anti-nuclear antibody negative
Antimitochondrial antibodies negative
Abdominal ultrasound shows thickening of the bile ducts and focal bile duct dilatation. Which of the following is the most likely diagnosis?
- A. Primary biliary cholangitis
- B. Hepatitis B infection
- C. Autoimmune hepatitis
- D. IgG4-associated cholangitis
- E. Primary sclerosing cholangitis (Correct Answer)
Medical management of ulcerative colitis Explanation: ***Primary sclerosing cholangitis***
- This patient's history of **ulcerative colitis** combined with cholestatic liver injury (elevated alkaline phosphatase >> transaminases), **scleral icterus**, and **severe pruritus** strongly suggests primary sclerosing cholangitis (PSC).
- The imaging findings of **bile duct thickening and focal dilatation** are characteristic of PSC, which causes chronic inflammation and fibrosis of intra- and extrahepatic bile ducts.
- PSC is strongly associated with inflammatory bowel disease, particularly **ulcerative colitis** (present in 60-80% of PSC patients), and typically affects men in their 30s-40s.
- Negative antimitochondrial antibodies help distinguish this from primary biliary cholangitis.
*Primary biliary cholangitis*
- Primary biliary cholangitis (PBC) typically affects **middle-aged women** and is characterized by positive **antimitochondrial antibodies (AMAs)**, which are negative in this patient.
- While PBC also causes cholestatic liver injury with pruritus, the male gender, younger age, strong association with ulcerative colitis, and bile duct changes on imaging point to PSC rather than PBC.
*Hepatitis B infection*
- Viral hepatitis B typically presents with a **hepatocellular pattern** of injury with AST and ALT elevated much higher than alkaline phosphatase (often >1000 U/L).
- This patient shows a **cholestatic pattern** (alkaline phosphatase 460 U/L with transaminases only mildly elevated at 75-78 U/L).
- Diagnosis would require positive hepatitis B serologies (HBsAg, anti-HBc), which are not present.
*Autoimmune hepatitis*
- Autoimmune hepatitis causes a **hepatocellular injury pattern** with very high transaminases (often >500-1000 U/L) and is associated with positive autoantibodies such as **ANA** or **anti-smooth muscle antibodies**, which are negative in this case.
- This patient's predominant cholestatic pattern and bile duct abnormalities are not consistent with autoimmune hepatitis.
*IgG4-associated cholangitis*
- IgG4-associated cholangitis can mimic PSC with bile duct stricturing and obstructive jaundice, but typically presents with **elevated serum IgG4 levels** and characteristic histopathology.
- It is **not associated with ulcerative colitis** and is much less common than PSC.
- This diagnosis would require tissue biopsy showing dense lymphoplasmacytic infiltrate with IgG4-positive plasma cells.
Medical management of ulcerative colitis US Medical PG Question 8: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Medical management of ulcerative colitis Explanation: ***Start annual colonoscopy starting in 8 years***
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Medical management of ulcerative colitis US Medical PG Question 9: A 72-year-old female presents to the emergency department complaining of severe abdominal pain and several days of bloody diarrhea. Her symptoms began with intermittent bloody diarrhea five days ago and have worsened steadily. For the last 24 hours, she has complained of fevers, chills, and abdominal pain. She has a history of ulcerative colitis, idiopathic hypertension, and hypothyroidism. Her medications include hydrochlorothiazide, levothyroxine, and sulfasalazine.
In the ED, her temperature is 39.1°C (102.4°F), pulse is 120/min, blood pressure is 90/60 mmHg, and respirations are 20/min. On exam, the patient is alert and oriented to person and place, but does not know the day. Her mucus membranes are dry. Heart and lung exam are not revealing. Her abdomen is distended with marked rebound tenderness. Bowel sounds are hyperactive.
Serum:
Na+: 142 mEq/L
Cl-: 107 mEq/L
K+: 3.3 mEq/L
HCO3-: 20 mEq/L
BUN: 15 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.2 mg/dL
Calcium: 10.1 mg/dL
Hemoglobin: 11.2 g/dL
Hematocrit: 30%
Leukocyte count: 14,600/mm^3 with normal differential
Platelet count: 405,000/mm^3
What is the next best step in management?
- A. Emergent colonoscopy
- B. Contrast enema
- C. Colectomy
- D. Plain abdominal radiograph
- E. Abdominal CT with IV contrast (Correct Answer)
Medical management of ulcerative colitis Explanation: ***Abdominal CT with IV contrast***
- The patient presents with **severe abdominal pain, bloody diarrhea, fever, hypotension, tachycardia, abdominal distension, rebound tenderness, and leukocytosis**, all suggestive of **toxic megacolon** complicating her ulcerative colitis.
- An **abdominal CT with IV contrast** is the most appropriate next step to confirm the diagnosis, assess the extent of colonic dilation and inflammation, and rule out complications like perforation.
*Emergent colonoscopy*
- **Colonoscopy** is generally **contraindicated** in suspected toxic megacolon due to the high risk of **perforation** of the severely inflamed and dilated colon.
- While it can diagnose ulcerative colitis, the current acute, severe presentation makes it too risky.
*Contrast enema*
- A **contrast enema** is also **contraindicated** in setting of potential **toxic megacolon** or suspected colonic perforation.
- The pressure from the contrast agent could worsen dilation or cause perforation in an already compromised colon.
*Colectomy*
- **Colectomy** is a surgical intervention reserved for cases of **toxic megacolon** that **fail medical management** or when there is evidence of **perforation** or **ischemia**.
- It is not the *immediate* next step in management without further imaging and attempts at medical stabilization.
*Plain abdominal radiograph*
- A plain abdominal radiograph can show colonic dilation and air-fluid levels, which are indicative of toxic megacolon; however, it has **limited ability to assess the extent of inflammation**, detect complications like **perforation**, or rule out other intra-abdominal pathologies.
- It might be a useful initial screen but is not as comprehensive as a CT scan, especially when a definitive diagnosis and management plan is needed.
Medical management of ulcerative colitis US Medical PG Question 10: A 34-year-old man with a 2-year history of rheumatoid arthritis is being evaluated on a follow-up visit. He is currently on methotrexate and celecoxib for pain management and has shown a good response until now. However, on this visit, he mentions that the morning stiffness has been getting progressively worse. On physical examination, both his wrists are erythematous and swollen, nodules on his elbows are also noted. Rheumatoid factor is 30 (normal reference values: < 15 IU/mL), ESR is 50 mm/h, anti-citrullinated protein antibodies is 55 (normal reference values: < 20). What is the next best step in the management of this patient?
- A. Sulfasalazine
- B. Adalimumab monotherapy
- C. Methotrexate and Corticosteroids
- D. Methotrexate and Infliximab (Correct Answer)
- E. Infliximab monotherapy
Medical management of ulcerative colitis Explanation: **Methotrexate and Infliximab**
- The patient is experiencing a **flare-up of rheumatoid arthritis** despite being on methotrexate, indicated by worsening morning stiffness, active synovitis (erythematous and swollen wrists), elevated ESR, and positive rheumatoid factor and anti-CCP. This suggests a need for more aggressive therapy, and adding a **biologic agent like infliximab (an anti-TNF agent)** to methotrexate is a standard approach for moderate to severe RA that is not adequately controlled by methotrexate monotherapy.
- Combination therapy with **methotrexate and a biologic DMARD** (e.g., TNF inhibitors like infliximab) has been shown to be more effective than monotherapy for controlling disease activity and preventing joint damage in refractory RA.
*Sulfasalazine*
- **Sulfasalazine** is a conventional synthetic DMARD that is generally used as a **first-line agent or in combination therapy** for mild to moderate RA.
- Given the patient's ongoing active disease despite methotrexate and the severity of his symptoms, sulfasalazine is unlikely to be sufficient to achieve disease control.
*Adalimumab monotherapy*
- While adalimumab (another anti-TNF biologic) is an effective treatment for RA, **biologic monotherapy is generally less effective** than combination therapy with methotrexate.
- Current guidelines and clinical practice favor combining biologic DMARDs with methotrexate for optimal outcomes in RA management, especially in patients with active disease.
*Methotrexate and Corticosteroids*
- **Corticosteroids** are effective in rapidly reducing inflammation and can be used for **short-term management of RA flares**.
- However, corticosteroids are not recommended for long-term use due to significant side effects and do not address the underlying disease progression as comprehensively as biologic DMARDs in patients refractory to methotrexate.
*Infliximab monotherapy*
- Similar to adalimumab monotherapy, **infliximab is typically more effective when combined with methotrexate**.
- Using infliximab alone would be a less optimal choice for this patient whose disease is clearly not controlled by methotrexate, as it may lead to a suboptimal response and potentially increase the risk of developing anti-drug antibodies.
More Medical management of ulcerative colitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.