IBD-related complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for IBD-related complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
IBD-related complications US Medical PG Question 1: A 23-year-old man complains of lower back pain that began approximately 6 months ago. He is unsure why he is experiencing this pain and notices that this pain is worse in the morning after waking up and improves with physical activity. Ibuprofen provides significant relief. He denies bowel and bladder incontinence or erectile dysfunction. Physical exam is notable for decreased chest expansion, decreased spinal range of motion, 5/5 strength in both lower extremities, 2+ patellar reflexes bilaterally, and an absence of saddle anesthesia. Which of the following is the most appropriate next test for this patient?
- A. HLA-B27
- B. Slit-lamp examination
- C. MRI sacroiliac joint
- D. Radiograph sacroiliac joint (Correct Answer)
- E. ESR
IBD-related complications Explanation: **Radiograph sacroiliac joint**
- Plain **radiographs of the sacroiliac (SI) joints** are typically the **initial imaging modality** for suspected **ankylosing spondylitis** due to affordability and diagnostic value.
- They can reveal characteristic changes such as **sacroiliitis (joint erosion, sclerosis, fusion)**, which are common in early-stage disease.
*HLA-B27*
- While a **positive HLA-B27** is associated with ankylosing spondylitis, it is **not diagnostic** on its own, as many HLA-B27 positive individuals never develop the disease.
- Its use is more in **confirming suspicion** or in cases where imaging is equivocal, but it's not the primary diagnostic test.
*Slit-lamp examination*
- A slit-lamp examination is used to detect **uveitis**, which can be an **extra-articular manifestation** of ankylosing spondylitis.
- However, it is not a primary diagnostic test for the condition itself, and its utility arises once the diagnosis is strongly considered or established.
*MRI sacroiliac joint*
- **MRI of the sacroiliac (SI) joints** is more sensitive than radiographs for detecting **early inflammatory changes** (e.g., bone marrow edema) that may not be visible on plain films.
- However, given the duration of symptoms (6 months) and the characteristic inflammatory back pain, **radiographs are typically the first-line imaging** due to cost-effectiveness, reserving MRI for cases with normal radiographs but high clinical suspicion.
*ESR*
- **Erythrocyte sedimentation rate (ESR)** is a **non-specific marker of inflammation** and can be elevated in various inflammatory conditions, including ankylosing spondylitis.
- It is not diagnostic for ankylosing spondylitis and cannot differentiate it from other inflammatory or infectious conditions.
IBD-related complications US Medical PG Question 2: A 32-year-old man comes to the physician for a follow-up examination. He has a 2-month history of increasing generalized fatigue and severe pruritus. He has hypertension and ulcerative colitis which was diagnosed via colonoscopy 5 years ago. Current medications include lisinopril and rectal mesalamine. He is sexually active with 2 female partners and uses condoms inconsistently. His temperature is 37.3°C (99.1°F), pulse is 86/min, and blood pressure is 130/84 mm Hg. Examination shows scleral icterus and multiple scratch marks on the trunk and extremities. The lungs are clear to auscultation. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.5 g/dL
Leukocyte count 7500/mm3
Platelet count 280,000/mm3
Serum
Na+ 138 mEq/L
Cl- 101 mEq/L
K+ 4.7 mEq/L
Urea nitrogen 18 mg/dL
Glucose 91 mg/dL
Creatinine 0.8 mg/dL
Bilirubin
Total 1.5 mg/dL
Direct 0.9 mg/dL
Alkaline phosphatase 460 U/L
AST 75 U/L
ALT 78 U/L
Anti-nuclear antibody negative
Antimitochondrial antibodies negative
Abdominal ultrasound shows thickening of the bile ducts and focal bile duct dilatation. Which of the following is the most likely diagnosis?
- A. Primary biliary cholangitis
- B. Hepatitis B infection
- C. Autoimmune hepatitis
- D. IgG4-associated cholangitis
- E. Primary sclerosing cholangitis (Correct Answer)
IBD-related complications Explanation: ***Primary sclerosing cholangitis***
- This patient's history of **ulcerative colitis** combined with cholestatic liver injury (elevated alkaline phosphatase >> transaminases), **scleral icterus**, and **severe pruritus** strongly suggests primary sclerosing cholangitis (PSC).
- The imaging findings of **bile duct thickening and focal dilatation** are characteristic of PSC, which causes chronic inflammation and fibrosis of intra- and extrahepatic bile ducts.
- PSC is strongly associated with inflammatory bowel disease, particularly **ulcerative colitis** (present in 60-80% of PSC patients), and typically affects men in their 30s-40s.
- Negative antimitochondrial antibodies help distinguish this from primary biliary cholangitis.
*Primary biliary cholangitis*
- Primary biliary cholangitis (PBC) typically affects **middle-aged women** and is characterized by positive **antimitochondrial antibodies (AMAs)**, which are negative in this patient.
- While PBC also causes cholestatic liver injury with pruritus, the male gender, younger age, strong association with ulcerative colitis, and bile duct changes on imaging point to PSC rather than PBC.
*Hepatitis B infection*
- Viral hepatitis B typically presents with a **hepatocellular pattern** of injury with AST and ALT elevated much higher than alkaline phosphatase (often >1000 U/L).
- This patient shows a **cholestatic pattern** (alkaline phosphatase 460 U/L with transaminases only mildly elevated at 75-78 U/L).
- Diagnosis would require positive hepatitis B serologies (HBsAg, anti-HBc), which are not present.
*Autoimmune hepatitis*
- Autoimmune hepatitis causes a **hepatocellular injury pattern** with very high transaminases (often >500-1000 U/L) and is associated with positive autoantibodies such as **ANA** or **anti-smooth muscle antibodies**, which are negative in this case.
- This patient's predominant cholestatic pattern and bile duct abnormalities are not consistent with autoimmune hepatitis.
*IgG4-associated cholangitis*
- IgG4-associated cholangitis can mimic PSC with bile duct stricturing and obstructive jaundice, but typically presents with **elevated serum IgG4 levels** and characteristic histopathology.
- It is **not associated with ulcerative colitis** and is much less common than PSC.
- This diagnosis would require tissue biopsy showing dense lymphoplasmacytic infiltrate with IgG4-positive plasma cells.
IBD-related complications US Medical PG Question 3: A 32-year-old man comes to the emergency department because of recurrent episodes of vomiting for 1 day. He has had over 15 episodes of bilious vomiting. During this period he has had cramping abdominal pain but has not had a bowel movement or passed flatus. He does not have fever or diarrhea. He was diagnosed with Crohn disease at the age of 28 years which has been well controlled with oral mesalamine. He underwent a partial small bowel resection for midgut volvulus at birth. His other medications include vitamin B12, folic acid, loperamide, ferrous sulfate, and vitamin D3. He appears uncomfortable and his lips are parched. His temperature is 37.1°C (99.3°F), pulse is 103/min, and blood pressure is 104/70 mm Hg. The abdomen is distended, tympanitic, and tender to palpation over the periumbilical area and the right lower quadrant. Rectal examination is unremarkable. A CT scan of the abdomen shows multiple dilated loops of small bowel with a transition zone in the mid to distal ileum. After 24 hours of conservative management with IV fluid resuscitation, nasogastric bowel decompression, promethazine, and analgesia, his condition does not improve and a laparotomy is scheduled. During the laparotomy, two discrete strictures are noted in the mid-ileum, around 20 cm apart. Which of the following is the most appropriate next step in management?
- A. Small bowel resection with ileostomy
- B. Abdominal closure and start palliative care
- C. Small bowel resection and primary anastomosis
- D. Strictureplasty of individual strictures (Correct Answer)
- E. Ileocolectomy
IBD-related complications Explanation: ***Strictureplasty of individual strictures***
- This patient presents with **multiple strictures** in the mid-ileum causing a small bowel obstruction in the setting of **Crohn's disease**. Strictureplasty is the preferred surgical approach for *short, multiple (up to four), or recurrent Crohn's disease strictures* as it preserves bowel length.
- While small bowel resection is an option, **strictureplasty** is favored in Crohn's disease to *avoid short bowel syndrome*, especially if multiple strictures are present, as seen here.
*Small bowel resection with ileostomy*
- An ileostomy is typically created when a primary anastomosis is not safe due to high risk of leak (e.g., severe inflammation, peritonitis, patient instability) or when there is extensive disease not amenable to strictureplasty with primary anastomosis.
- Performing an ileostomy when primary anastomosis is possible unnecessarily creates a stoma, which can lead to complications and impact quality of life.
*Abdominal closure and start palliative care*
- This patient, while acutely unwell, has a surgically correctable cause for his obstruction and is not described as having an incurable or end-stage condition necessitating only palliative care.
- Palliative care would be considered for patients with widespread untreatable disease or severe comorbidities, which is not indicated here given the localized, treatable strictures.
*Small bowel resection and primary anastomosis*
- While small bowel resection is a valid treatment for isolated, non-recurrent strictures, strictureplasty is generally preferred in Crohn's disease when multiple strictures are present.
- **Resection of multiple segments** can lead to significant **short bowel syndrome**, especially in a patient with a history of prior small bowel resection, making strictureplasty a more bowel-sparing and appropriate choice.
*Ileocolectomy*
- **Ileocolectomy** involves resection of the terminal ileum and a portion of the colon. This would be indicated if the disease involves the *ileocecal valve region* or the *colon*, which is not the case in this patient, whose strictures are in the mid-ileum.
- This procedure is excessive for mid-ileal strictures and would result in unnecessary removal of healthy bowel given the location of the strictures.
IBD-related complications US Medical PG Question 4: A 22-year-old woman presents to the emergency department with a 3-day history of fever and abdominal pain. She says that the pain is located in the left lower quadrant of the abdomen and feels crampy in nature. The pain has been associated with bloody diarrhea and joint tenderness. She has no past medical history but says that she returned 2 weeks ago from vacation in Asia where she tried many new foods. Her family history is significant for multiple cancers in close relatives. Physical exam reveals swollen ulcers on her legs, and colonoscopy reveals contiguous ulcerations from the rectum through the descending colon. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Noncaseating granulomas
- B. Severe aortic stenosis
- C. Gram-negative rod
- D. HLA-DQ2 positivity
- E. Perinuclear anti-neutrophil cytoplasmic antibodies (Correct Answer)
IBD-related complications Explanation: ***Perinuclear anti-neutrophil cytoplasmic antibodies***
- The patient's presentation with **bloody diarrhea**, low-grade fever, **crampy abdominal pain**, joint tenderness, and contiguous ulcerations in the colon is highly suggestive of **ulcerative colitis**.
- **Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA)** are found in 50-70% of patients with ulcerative colitis and are associated with a more extensive disease.
*Noncaseating granulomas*
- **Noncaseating granulomas** are a characteristic histological finding in **Crohn's disease**, not ulcerative colitis.
- Crohn's disease typically presents with **skip lesions**, **transmural inflammation**, and affects any part of the GI tract, often with perianal disease.
*Severe aortic stenosis*
- **Severe aortic stenosis** is a condition of the heart valves that can lead to symptoms like chest pain, syncope, and heart failure, and is not directly associated with the patient's gastrointestinal and systemic symptoms.
- While inflammatory conditions can rarely have cardiac manifestations, there's no direct link between aortic stenosis and inflammatory bowel disease in this context.
*Gram-negative rod*
- While infections, especially from **Gram-negative rods** like *Shigella* or *Salmonella*, can cause acute bloody diarrhea, the 3-day history with joint tenderness and contiguous ulcers on colonoscopy points more towards an inflammatory bowel disease.
- The chronicity and systemic involvement are less typical for an acute bacterial enteritis, although such infections might trigger IBD.
*HLA-DQ2 positivity*
- **HLA-DQ2 positivity** is strongly associated with **celiac disease**, an immune-mediated enteropathy triggered by gluten.
- Celiac disease typically presents with malabsorption symptoms like fatty stools, weight loss, and iron deficiency, rather than bloody diarrhea and contiguous colonic ulcerations.
IBD-related complications US Medical PG Question 5: A 37-year-old man presents to his gastroenterologist due to a transaminitis found by his primary care physician (PCP). He reports currently feeling well and has no acute concerns. Medical history is significant for ulcerative colitis treated with 5-aminosalicylate. He recently went on a trip to Mexico and experienced an episode of mild diarrhea. The patient is 5 ft 4 in and weighs 220 lbs (99.8 kg). His temperature is 98°F (36.7°C), blood pressure is 138/88 mmHg, pulse is 90/min, and respirations are 18/min. Physical examination is unremarkable. Laboratory testing demonstrates:
Leukocyte count: 7,200 /mm^3
Alkaline phosphatase: 205 U/L
Aspartate aminotransferase (AST): 120 U/L
Alanine aminotransferase (ALT): 115 U/L
Perinuclear antineutrophil cytoplasmic antibody (pANCA): Positive
Antimitochondrial antibody: Negative
Which of the following is most likely the diagnosis?
- A. Choledocholithiasis
- B. Acute cholecystitis
- C. Acute viral hepatitis
- D. Primary sclerosing cholangitis (Correct Answer)
- E. Primary biliary cholangitis
IBD-related complications Explanation: ***Primary sclerosing cholangitis***
- The patient's history of **ulcerative colitis**, elevated **alkaline phosphatase**, and positive **pANCA** are highly suggestive of primary sclerosing cholangitis (PSC).
- PSC often presents with **asymptomatic transaminitis** in early stages and is strongly associated with inflammatory bowel disease, particularly ulcerative colitis.
*Choledocholithiasis*
- This condition is characterized by **gallstones in the common bile duct**, usually presenting with **biliary colic**, jaundice, or cholangitis.
- While it can cause elevated liver enzymes, particularly alkaline phosphatase, the chronic, asymptomatic nature and strong association with ulcerative colitis and pANCA positivity point away from choledocholithiasis as the *most likely* diagnosis.
*Acute cholecystitis*
- **Acute cholecystitis** involves inflammation of the gallbladder, typically causing **right upper quadrant pain**, fever, and leukocytosis.
- The patient is asymptomatic, afebrile, and has an unremarkable physical exam, making acute cholecystitis unlikely.
*Acute viral hepatitis*
- **Acute viral hepatitis** usually presents with significantly higher **aminotransferase levels** (often in the thousands) and symptoms like fatigue, nausea, and jaundice.
- The patient's relatively mild transaminitis, asymptomatic status, and specific risk factors (ulcerative colitis, pANCA) do not fit the typical picture of acute viral hepatitis.
*Primary biliary cholangitis*
- **Primary biliary cholangitis (PBC)** is characterized by destruction of small intrahepatic bile ducts, primarily affecting women, and is associated with **anti-mitochondrial antibodies (AMA)**.
- The patient is male, and his AMA is negative, making PBC an unlikely diagnosis, despite the elevated alkaline phosphatase.
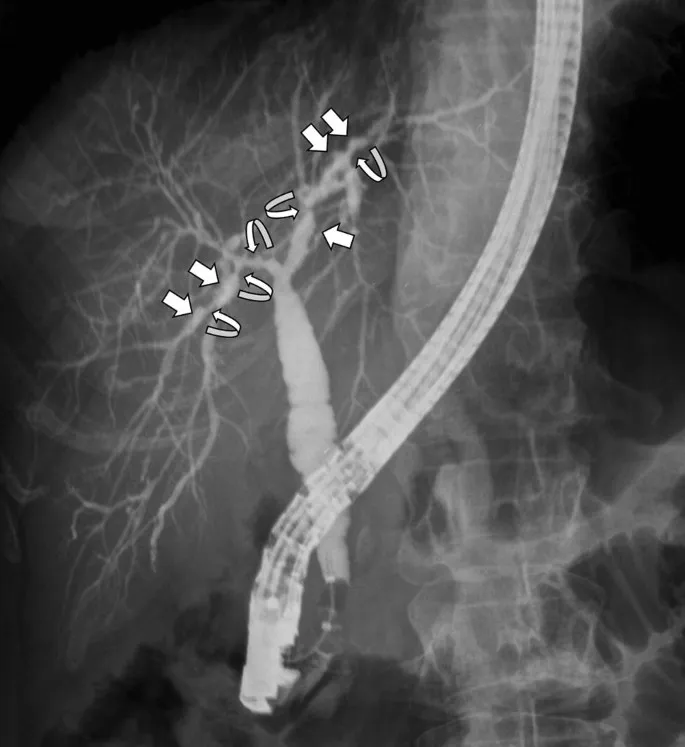
IBD-related complications US Medical PG Question 6: A 23-year-old female presents with a seven-day history of abdominal pain, and now bloody diarrhea that brings her to her primary care physician. Review of systems is notable for a 12-pound unintentional weight loss and intermittent loose stools. She has a family history notable for a father with CAD and a mother with primary sclerosing cholangitis. Upon further workup, she is found to have the following on colonoscopy and biopsy, Figures A and B respectively. Serum perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) is positive. This patient's disease is likely to also include which of the following features?
- A. Worse disease severity near the ileocecal valve
- B. Cobblestoning and skip lesions
- C. Fistulae and stricture formation
- D. Perianal disease
- E. Continuous progression beginning in the rectum (Correct Answer)
IBD-related complications Explanation: ***Continuous progression beginning in the rectum***
- The patient's presentation with abdominal pain, bloody diarrhea, weight loss, and **positive P-ANCA** is highly suggestive of **ulcerative colitis**.
- **Ulcerative colitis** characteristically presents with **continuous inflammation** that begins in the **rectum** and extends proximally through the colon.
*Worse disease severity near the ileocecal valve*
- This feature is more characteristic of **Crohn's disease**, where the **ileocecal region** is a common site of severe involvement.
- In **ulcerative colitis**, inflammation is typically confined to the colon and does not disproportionately affect the ileocecal valve unless there is backwash ileitis.
*Cobblestoning and skip lesions*
- **Cobblestoning** and **skip lesions** are classic endoscopic findings in **Crohn's disease**, reflecting the patchy, transmural inflammation.
- **Ulcerative colitis** is characterized by diffuse, superficial inflammation without skip lesions.
*Fistulae and stricture formation*
- The formation of **fistulae** (abnormal connections between organs) and **strictures** (narrowing of the bowel lumen) are hallmarks of **Crohn's disease** due to its transmural inflammation.
- These complications are rare in **ulcerative colitis**, which primarily affects the mucosal layer.
*Perianal disease*
- **Perianal disease**, including **fissures**, **abscesses**, and **fistulae**, is a common extraintestinal manifestation and complication of **Crohn's disease**.
- While other extraintestinal manifestations like **primary sclerosing cholangitis** can occur in both, perianal disease itself is less typical for uncomplicated **ulcerative colitis**.
IBD-related complications US Medical PG Question 7: A 22-year-old Caucasian female presents with severe right lower quadrant pain, malaise, and diarrhea. The physician performs an endoscopy and finds disease involvement in the terminal ileum, noting that the disease process is patchy with normal intervening mucosa. The entire wall of the region is thickened and inflamed, which may directly lead to formation of:
- A. Paneth cell metaplasia
- B. Toxic megacolon
- C. Plummer-Vinson syndrome
- D. Widening of the intestinal lumen
- E. Fistulas (Correct Answer)
IBD-related complications Explanation: ***Fistulas***
- **Transmural inflammation**, characteristic of **Crohn's disease**, means the entire wall of the intestine is affected, leading to deep ulcerations and sinus tracts that can bore through tissues.
- This deep, penetrating inflammation often results in the formation of **fistulas** (abnormal connections between organs or to the skin) or **abscesses**.
*Paneth cell metaplasia*
- This is a histological change where **Paneth cells**, normally found in the small intestine, appear in regions they shouldn't, such as the colon.
- While it can occur in **inflammatory bowel disease**, it is a microscopic change and not a direct consequence of the described gross pathology (transmural inflammation leading to a larger structural complication like a fistula).
*Toxic megacolon*
- This is a severe complication characterized by **colonic dilation** and systemic toxicity, usually seen in **ulcerative colitis**, not typically Crohn's disease limited to the terminal ileum.
- It arises from acute, severe inflammation that extends to the muscularis propria, causing paralysis of the colon, which is distinct from the **transmural inflammation** in Crohn's leading to fistulas.
*Plummer-Vinson syndrome*
- This syndrome is characterized by a triad of **iron-deficiency anemia**, **dysphagia** (due to esophageal webs), and **glossitis**, which is unrelated to inflammatory bowel disease.
- It is a condition of the upper gastrointestinal tract and has no direct link to the pathology described in the terminal ileum.
*Widening of the intestinal lumen*
- The **transmural inflammation** described in Crohn's disease typically leads to **thickening of the bowel wall** and, more commonly, **strictures** (narrowing) of the lumen rather than widening.
- The inflammatory process usually causes fibrosis and scarring, which reduces the luminal diameter, particularly in chronic disease.
IBD-related complications US Medical PG Question 8: A 32-year-old woman presents to her family physician with a long history of depression, irritability, and, more recently, personality changes. As her partner comments, she has stopped engaging in activities she used to enjoy like dancing, drumming lessons, and yoga. The patient denies changes in skin pigmentation and assures she keeps a balanced diet low in fat and carbohydrates. During the physical examination, jaundice and dark rings encircling the iris of the eye are noted, as well as hepatomegaly and gait disturbances. For a follow-up visit, the patient brings a battery of laboratory tests that includes a complete blood count showing normocytic normochromic anemia, a negative Coombs, normal iron levels, normal fasting glucose levels, elevated aminotransferases from the liver biochemical tests, bilirubin, and decreased serum ceruloplasmin levels. Antinuclear antibodies are negative. What is the most likely diagnosis?
- A. Primary sclerosing cholangitis
- B. Wilson disease (Correct Answer)
- C. Hemochromatosis
- D. Nonalcoholic fatty liver disease
- E. Autoimmune hepatitis
IBD-related complications Explanation: ***Wilson disease***
- The combination of **neuropsychiatric symptoms** (depression, irritability, personality changes, gait disturbances), **liver disease** (jaundice, hepatomegaly, elevated aminotransferases, hyperbilirubinemia), and **Kayser-Fleischer rings** in the eyes is pathognomonic for Wilson disease.
- **Decreased serum ceruloplasmin** levels further confirm the diagnosis, as ceruloplasmin is the main copper-carrying protein in the blood, and its deficiency leads to copper accumulation.
*Primary sclerosing cholangitis*
- Characterized by inflammation and fibrosis of the **bile ducts**, leading to cholestasis and can be associated with inflammatory bowel disease, which is not mentioned here.
- While it causes jaundice and elevated liver enzymes, it does not typically present with the neurological or psychiatric symptoms, or **Kayser-Fleischer rings** seen in Wilson disease.
*Hemochromatosis*
- This disorder involves excessive **iron accumulation** in the body, leading to symptoms like fatigue, joint pain, impotence, and liver damage (cirrhosis, hepatomegaly).
- The patient's **normal iron levels** and the absence of classic bronze skin pigmentation, along with the presence of Kayser-Fleischer rings and neuropsychiatric symptoms, rule out hemochromatosis.
*Nonalcoholic fatty liver disease*
- Primarily associated with **metabolic syndrome** (obesity, diabetes, hyperlipidemia) and is characterized by fat accumulation in the liver.
- While it can cause hepatomegaly and elevated liver enzymes, it does not typically manifest with neurological or psychiatric symptoms, nor **Kayser-Fleischer rings**, and the patient describes a balanced diet.
*Autoimmune hepatitis*
- Involves **immune-mediated inflammation of the liver** and can present with elevated aminotransferases, hyperbilirubinemia, and hepatomegaly, often with positive autoantibodies (e.g., ANA, anti-smooth muscle antibodies).
- The patient's **negative ANA** and the presence of **Kayser-Fleischer rings** and prominent neuropsychiatric symptoms are not characteristic of autoimmune hepatitis.
IBD-related complications US Medical PG Question 9: A 72-year-old female presents to the emergency department complaining of severe abdominal pain and several days of bloody diarrhea. Her symptoms began with intermittent bloody diarrhea five days ago and have worsened steadily. For the last 24 hours, she has complained of fevers, chills, and abdominal pain. She has a history of ulcerative colitis, idiopathic hypertension, and hypothyroidism. Her medications include hydrochlorothiazide, levothyroxine, and sulfasalazine.
In the ED, her temperature is 39.1°C (102.4°F), pulse is 120/min, blood pressure is 90/60 mmHg, and respirations are 20/min. On exam, the patient is alert and oriented to person and place, but does not know the day. Her mucus membranes are dry. Heart and lung exam are not revealing. Her abdomen is distended with marked rebound tenderness. Bowel sounds are hyperactive.
Serum:
Na+: 142 mEq/L
Cl-: 107 mEq/L
K+: 3.3 mEq/L
HCO3-: 20 mEq/L
BUN: 15 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.2 mg/dL
Calcium: 10.1 mg/dL
Hemoglobin: 11.2 g/dL
Hematocrit: 30%
Leukocyte count: 14,600/mm^3 with normal differential
Platelet count: 405,000/mm^3
What is the next best step in management?
- A. Emergent colonoscopy
- B. Contrast enema
- C. Colectomy
- D. Plain abdominal radiograph
- E. Abdominal CT with IV contrast (Correct Answer)
IBD-related complications Explanation: ***Abdominal CT with IV contrast***
- The patient presents with **severe abdominal pain, bloody diarrhea, fever, hypotension, tachycardia, abdominal distension, rebound tenderness, and leukocytosis**, all suggestive of **toxic megacolon** complicating her ulcerative colitis.
- An **abdominal CT with IV contrast** is the most appropriate next step to confirm the diagnosis, assess the extent of colonic dilation and inflammation, and rule out complications like perforation.
*Emergent colonoscopy*
- **Colonoscopy** is generally **contraindicated** in suspected toxic megacolon due to the high risk of **perforation** of the severely inflamed and dilated colon.
- While it can diagnose ulcerative colitis, the current acute, severe presentation makes it too risky.
*Contrast enema*
- A **contrast enema** is also **contraindicated** in setting of potential **toxic megacolon** or suspected colonic perforation.
- The pressure from the contrast agent could worsen dilation or cause perforation in an already compromised colon.
*Colectomy*
- **Colectomy** is a surgical intervention reserved for cases of **toxic megacolon** that **fail medical management** or when there is evidence of **perforation** or **ischemia**.
- It is not the *immediate* next step in management without further imaging and attempts at medical stabilization.
*Plain abdominal radiograph*
- A plain abdominal radiograph can show colonic dilation and air-fluid levels, which are indicative of toxic megacolon; however, it has **limited ability to assess the extent of inflammation**, detect complications like **perforation**, or rule out other intra-abdominal pathologies.
- It might be a useful initial screen but is not as comprehensive as a CT scan, especially when a definitive diagnosis and management plan is needed.
IBD-related complications US Medical PG Question 10: A 53 year-old woman with history of ulcerative colitis presents to the emergency department with a severe flare. The patient reports numerous bloody loose stools, and has been febrile for two days. Vital signs are: T 101.9 HR 98 BP 121/86 RR 17 Sat 100%. Abdominal exam is notable for markedly distended abdomen with tympani and tenderness to palpation without guarding or rebound. KUB is shown in figure A. CT scan shows markedly dilated descending and sigmoid colon with no perforations. What is the next best step in management for this patient?
- A. IV Ondansetron
- B. Rectal 5-ASA
- C. IV hydrocortisone (Correct Answer)
- D. Oral prednisone
- E. IV Metoclopramide
IBD-related complications Explanation: ***IV hydrocortisone***
- This patient has **toxic megacolon**, a life-threatening complication of ulcerative colitis requiring aggressive medical management alongside surgical consultation.
- High-dose **IV corticosteroids** (hydrocortisone 100mg IV q6-8h or methylprednisolone) are first-line medical therapy to rapidly suppress severe colonic inflammation.
- Medical management includes IV steroids, broad-spectrum antibiotics, bowel rest (NPO), IV fluid resuscitation, and nasogastric decompression while preparing for potential **emergent colectomy** if medical therapy fails within 24-72 hours.
- IV route ensures **rapid systemic delivery** in a critically ill patient with impaired GI absorption.
*IV Ondansetron*
- An antiemetic that treats nausea/vomiting symptoms but does **not address the underlying inflammatory process** or systemic toxicity.
- Does not modify disease course or reduce the risk of **perforation** in toxic megacolon.
*Rectal 5-ASA*
- **Contraindicated in toxic megacolon** due to risk of perforation with rectal manipulation and increased intraluminal pressure.
- Local therapy is ineffective for **systemic toxicity** (fever, hemodynamic instability) and extensive colonic involvement.
- Only appropriate for mild-to-moderate distal ulcerative colitis, not severe fulminant disease.
*Oral prednisone*
- Inadequate for **acute severe/fulminant colitis** requiring hospitalization due to delayed absorption and lower bioavailability.
- IV corticosteroids provide **immediate systemic effect** necessary for life-threatening toxic megacolon.
- Oral route inappropriate in patient with severe GI symptoms and potential ileus.
*IV Metoclopramide*
- A prokinetic agent that is **absolutely contraindicated in toxic megacolon** as it increases colonic motility and can precipitate perforation.
- Does not address the **inflammatory pathophysiology** of ulcerative colitis.
- Used for gastroparesis and nausea, not for managing inflammatory bowel disease complications.
More IBD-related complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.