IBD in special populations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for IBD in special populations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
IBD in special populations US Medical PG Question 1: A 33-year-old woman with Crohn’s disease colitis presents to her physician after 2 days of photophobia and blurred vision. She has had no similar episodes in the past. She has no abdominal pain or diarrhea and takes mesalazine, azathioprine, and prednisone as maintenance therapy. Her vital signs are within normal range. Examination of the eyes shows conjunctival injection. The physical examination is otherwise normal. Slit-lamp examination by an ophthalmologist shows evidence of inflammation in the anterior chamber. Which of the following is the most appropriate modification to this patient’s medication at this time?
- A. Adding infliximab
- B. Increasing dose of prednisone (Correct Answer)
- C. No modification of therapy at this time
- D. Discontinuing mesalazine
- E. Decreasing dose of azathioprine
IBD in special populations Explanation: ***Increasing dose of prednisone***
- This patient is presenting with **anterior uveitis**, a common **extraintestinal manifestation of Crohn’s disease**, characterized by photophobia, blurred vision, and inflammation of the anterior chamber.
- **Corticosteroids** (like prednisone) are the **first-line treatment for acute uveitis**, and increasing the dose will help control the inflammation effectively.
*Adding infliximab*
- While **biologics like infliximab** can be effective for refractory uveitis or systemic disease control, they are **not the immediate first-line treatment for an acute uveitis flare**, especially when corticosteroids are already part of the regimen.
- Adding a new biologic would also involve a longer onset of action and additional risks, making it less suitable for urgent symptom control compared to adjusting prednisone.
*No modification of therapy at this time*
- The patient clearly has **acute anterior uveitis**, which is a potentially serious ocular condition requiring prompt treatment to prevent complications such as synechiae, glaucoma, and vision loss.
- Doing nothing would lead to worsening inflammation and potential irreversible damage.
*Discontinuing mesalazine*
- **Mesalazine** (an aminosalicylate) is primarily used for maintaining remission in inflammatory bowel disease and is **not implicated in causing uveitis**, nor is discontinuing it a treatment for uveitis.
- It would also risk a flare of her Crohn's disease.
*Decreasing dose of azathioprine*
- **Azathioprine** is an **immunosuppressant** used to maintain remission in Crohn’s disease and is not a direct treatment for acute uveitis.
- Decreasing the dose would weaken her overall immunosuppression, potentially leading to a flare of her Crohn's disease or making her more susceptible to other issues, without directly addressing the acute ocular inflammation.
IBD in special populations US Medical PG Question 2: A 62-year-old man comes to the physician in May for a routine health maintenance examination. He feels well. He underwent a right inguinal hernia repair 6 months ago. He has hypertension and type 2 diabetes mellitus. There is no family history of serious illness. Current medications include metformin, sitagliptin, enalapril, and metoprolol. He received the zoster vaccine 1 year ago. He received the PPSV23 vaccine 4 years ago. His last colonoscopy was 7 years ago and was normal. He smoked a pack of cigarettes a day for 20 years but quit 17 years ago. He drinks two to three alcoholic beverages on weekends. He is allergic to amoxicillin. He is scheduled to visit Australia and New Zealand in 2 weeks to celebrate his 25th wedding anniversary. He appears healthy. Vital signs are within normal limits. An S4 is heard at the apex. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate recommendation at this time?
- A. Colonoscopy
- B. Influenza vaccine (Correct Answer)
- C. Pneumococcal conjugate vaccine 13
- D. Cardiac stress test
- E. Abdominal ultrasound
IBD in special populations Explanation: ***Influenza vaccine***
- Current guidelines recommend annual **influenza vaccination** for all adults, particularly those over 60 years old and those with chronic medical conditions like diabetes and hypertension.
- **Critical timing consideration**: The patient is traveling to Australia and New Zealand (Southern Hemisphere) in 2 weeks, where it will be **winter season** (May-September) with peak influenza activity.
- He is a **high-risk patient** (age >60, diabetes, hypertension, cardiovascular disease) who should receive influenza vaccine before travel to areas experiencing influenza season.
- This is the **most appropriate and time-sensitive recommendation** at this visit.
*Colonoscopy*
- The patient had a normal colonoscopy 7 years ago; current guidelines suggest a repeat colonoscopy every **10 years** for average-risk individuals.
- There are no new symptoms, family history, or risk factors that would necessitate an earlier repeat colonoscopy at this time.
*Pneumococcal conjugate vaccine 13*
- The patient received **PPSV23** four years ago at approximately age 58.
- Per **current CDC guidelines (2019+)**, PCV13 is **no longer routinely recommended** for immunocompetent adults ≥65 years old.
- PPSV23 alone is now the standard recommendation for adults ≥65, which this patient has already received.
- PCV13 may be considered through **shared decision-making** in specific circumstances, but is not a routine or urgent recommendation.
*Cardiac stress test*
- Although the patient has risk factors for cardiovascular disease (hypertension, diabetes, former smoker) and an **S4 heart sound** (indicating **left ventricular hypertrophy**), he is asymptomatic.
- Routine **screening stress tests** are not recommended for asymptomatic individuals without signs of active cardiac ischemia.
*Abdominal ultrasound*
- There are **no symptoms** or specific indications (e.g., abdominal aortic aneurysm screening criteria not met - would need age 65-75 with smoking history).
- The patient is 62 years old and quit smoking 17 years ago, so AAA screening criteria are not yet met.
- Routine screening abdominal ultrasounds are not indicated.
IBD in special populations US Medical PG Question 3: A 38-year-old man presents to his primary care provider for abdominal pain. He reports that he has had a dull, burning pain for several months that has progressively gotten worse. He also notes a weight loss of about five pounds over that time frame. The patient endorses nausea and feels that the pain is worse after meals, but he denies any vomiting or diarrhea. He has a past medical history of hypertension, and he reports that he has been under an unusual amount of stress since losing his job as a construction worker. His home medications include enalapril and daily ibuprofen, which he takes for lower back pain he developed at his job. The patient drinks 1-2 beers with dinner and has a 25-pack-year smoking history. His family history is significant for colorectal cancer in his father and leukemia in his grandmother. On physical exam, the patient is moderately tender to palpation in the epigastrium. A fecal occult test is positive for blood in the stool.
Which of the following in the patient’s history is most likely causing this condition?
- A. Family history of cancer
- B. Physiologic stress
- C. Medication use (Correct Answer)
- D. Smoking history
- E. Alcohol use
IBD in special populations Explanation: ***Medication use***
- The patient's daily use of **ibuprofen**, an **NSAID**, is a significant risk factor for **peptic ulcer disease**, which can cause abdominal pain, weight loss, and GI bleeding.
- NSAIDs **inhibit prostaglandin synthesis**, disrupting the protective **gastric mucosal barrier**.
*Family history of cancer*
- While a family history of colorectal cancer can increase an individual's risk, the patient's symptoms (epigastric pain, pain worse after meals, positive fecal occult) are more characteristic of an **upper GI source**, not typically colorectal cancer.
- The type of cancers in his family (colorectal, leukemia) are not directly linked to the patient's current presentation of **epigastric pain** and likely **gastric ulceration**.
*Physiologic stress*
- While stress can exacerbate gastrointestinal symptoms and is a risk factor for various GI issues, the combination of specific symptoms (burning pain, post-prandial worsening, and GI bleeding) points more strongly to an **organic cause** like an ulcer, particularly given the other risk factors.
- Stress alone is less likely to be the primary cause of a **positive fecal occult test** and the described persistent, worsening pain over several months without other clear organic pathology.
*Smoking history*
- **Smoking** is a known risk factor for **peptic ulcer disease** and an independent risk factor for many GI cancers.
- However, the direct, immediate causal link to the patient's acute presentation of symptoms and positive fecal occult test is less direct than NSAID use.
*Alcohol use*
- Moderate alcohol intake (1-2 beers daily) is generally not considered a direct or primary cause of peptic ulcer disease in the same way that NSAID use is.
- While excessive alcohol can irritate the gastric mucosa, this patient's reported intake is **not typically sufficient** to be the most likely sole cause of the described symptoms and bleeding.
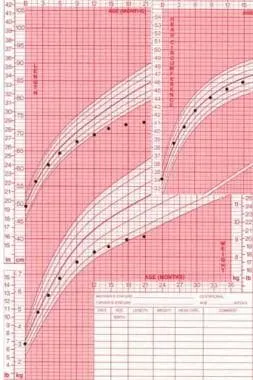
IBD in special populations US Medical PG Question 4: An 11-month-old boy is brought to a pediatrician by his parents for evaluation of vomiting and watery diarrhea over the last day. The mother informs the pediatrician that the boy had consumed an apple bought from a fruit vendor on the previous day, but that otherwise there has been no recent change in his diet. There is no history of blood in the stool, flatulence, irritability, or poor appetite. There is no history of recurrent or chronic diarrhea or any other gastrointestinal symptoms. On physical examination, his temperature is 37.6°C (99.6°F), pulse is 120/min, respirations are 24/min, and blood pressure is 92/60 mm Hg. General examination reveals a playful infant with normal skin turgor and no sunken eyes. The pediatrician explains to the parents that he most likely has acute gastroenteritis and that no specific medication is indicated at present. He also instructs the parents about his diet during the illness and reviews the danger signs of dehydration. He suggests a follow-up evaluation after 48 hours or earlier if any complications arise. Which of the following dietary recommendations did the pediatrician make?
- A. Plenty of juices and carbonated sodas
- B. Age-appropriate diet (Correct Answer)
- C. Diluted formula milk
- D. Lactose-free diet
- E. BRAT diet
IBD in special populations Explanation: ***Age-appropriate diet***
- For **mild acute gastroenteritis** without significant dehydration, the latest recommendations advise continuing **age-appropriate feeding** to support nutritional requirements and promote gut recovery.
- This approach helps to prevent malnutrition and does not prolong the course of diarrhea.
*Plenty of juices and carbonated sodas*
- **High sugar content** in juices and sodas can worsen diarrhea due to their **osmotic effect**, drawing more water into the intestine.
- These beverages also lack essential **electrolytes** needed for rehydration.
*Diluted formula milk*
- Diluting formula can lead to **insufficient caloric intake** and nutritional deficiencies, which is generally not recommended for mild gastroenteritis.
- Undiluted formula is usually well-tolerated, as most infants with acute gastroenteritis do not develop significant **lactose intolerance**.
*Lactose-free diet*
- Routine use of **lactose-free diets** is generally not recommended unless there is strong evidence of **secondary lactase deficiency**, which typically presents with increased flatulence, bloating, and worsening diarrhea.
- The majority of children with acute gastroenteritis can tolerate their usual milk intake.
*BRAT diet*
- The **B**ananas, **R**ice, **A**pplesauce, **T**oast (BRAT) diet is **nutritionally restrictive**, providing inadequate protein and fat, which can hinder recovery and growth in infants.
- Current guidelines no longer recommend the BRAT diet for acute gastroenteritis.
IBD in special populations US Medical PG Question 5: A 31-year-old man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. His vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 87/min, and respiratory rate is 15/min. Rectal examination reveals a small amount of bright red blood. Lower endoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate initial treatment for this patient's underlying disease?
- A. Azathioprine
- B. Mesalamine (Correct Answer)
- C. Systemic corticosteroids
- D. Total proctocolectomy
- E. Sulfasalazine
IBD in special populations Explanation: ***Mesalamine***
- The patient's symptoms (bloody diarrhea, abdominal pain, erythema, pseudopolyps, and inflammation extending from the rectum to the splenic flexure) are highly suggestive of **ulcerative colitis (UC) affecting the left colon (distal colitis)**.
- **Mesalamine** (a 5-aminosalicylic acid or 5-ASA derivative) is the first-line treatment for mild to moderate UC, especially for proctitis and left-sided colitis. Its anti-inflammatory action is exerted topically on the colonic mucosa.
*Azathioprine*
- Azathioprine is an **immunomodulator** used for maintaining remission in UC or in cases where patients are steroid-dependent or refractory to 5-ASAs.
- It is not typically used as a first-line agent for acute, mild to moderate disease.
*Systemic corticosteroids*
- **Systemic corticosteroids** are used for moderate to severe UC or for severe flares, not for initial mild to moderate disease, due to their significant side effect profile.
- While effective in inducing remission, their long-term use is limited, and they are not considered a maintenance therapy.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical option reserved for severe, refractory UC that does not respond to medical therapy, or in cases of dysplasia/cancer.
- It is an invasive procedure and not an appropriate initial treatment for a patient presenting with symptoms of mild to moderate disease.
*Sulfasalazine*
- **Sulfasalazine** is an older 5-ASA compound that is also effective for mild to moderate UC.
- However, it has a **higher incidence of side effects** (e.g., GI upset, headaches, hypersensitivity) compared to mesalamine, making mesalamine generally preferred for better tolerability.
IBD in special populations US Medical PG Question 6: Three days after admission to the hospital with a clinical diagnosis of ischemic colitis, a 65-year-old man has recovered from his initial symptoms of bloody diarrhea and abdominal pain with tenderness. He feels well at this point and wishes to go home. He has a 15-year history of diabetes mellitus. Currently, he receives nothing by mouth, and he is on IV fluids, antibiotics, and insulin. His temperature is 36.7°C (98.1°F), pulse is 68/min, respiratory rate is 13/min, and blood pressure is 115/70 mm Hg. Physical examination of the abdomen shows no abnormalities. His most recent laboratory studies are all within normal limits, including glucose. Which of the following is the most appropriate next step in management?
- A. Laparoscopy
- B. Discharge home with follow-up in one month
- C. Laparotomy
- D. Total parenteral nutrition
- E. Colonoscopy (Correct Answer)
IBD in special populations Explanation: ***Colonoscopy***
- A colonoscopy is crucial for **evaluating the extent of ischemic damage**, identifying strictures, and ruling out other pathologies like inflammatory bowel disease or malignancy.
- While the patient is clinically stable, direct visualization of the colonic mucosa a few days after the acute event is necessary to **assess healing** and guide future management.
*Laparoscopy*
- **Laparoscopy is an invasive surgical procedure** primarily used for diagnosis and intervention in acute abdominal conditions, which are not present here.
- Given the patient's stable condition and resolution of symptoms, a less invasive diagnostic tool like colonoscopy is more appropriate at this stage.
*Discharge home with follow-up in one month*
- Discharging the patient without further investigation is **premature** as the full extent of the ischemic injury and potential long-term complications are unknown.
- There is a risk of **stricture formation** or recurrent ischemia, necessitating a comprehensive assessment before discharge.
*Laparotomy*
- **Laparotomy is a major open surgical procedure** reserved for cases with severe ischemia, perforation, or peritonitis, none of which are indicated by the patient's current status.
- The patient's stable vital signs and resolution of initial symptoms make this overly aggressive and unnecessary.
*Total parenteral nutrition*
- **Total parenteral nutrition (TPN) is used when the gastrointestinal tract cannot be used** for an extended period, such as in severe short bowel syndrome or prolonged postoperative ileus.
- The patient is currently on IV fluids and is NPO, but there's no indication of long-term inability to use his gut, and the nutritional support does not address the need for structural assessment of the colon.
IBD in special populations US Medical PG Question 7: A 34-year-old woman comes to the emergency department because of decreased appetite, nausea, vomiting, and episodic abdominal pain for the past two months. The pain is sharp, colicky, and lasts about an hour after meals. Her stools are light in appearance and difficult to flush. Physical examination shows tenderness in the right upper quadrant. Without treatment, this patient is at greatest risk for developing which of the following?
- A. Steatohepatitis
- B. Megaloblastic anemia
- C. Delayed wound healing
- D. Low bone mineral density (Correct Answer)
- E. Glossitis
IBD in special populations Explanation: ***Low bone mineral density***
- This patient presents with symptoms highly suggestive of **gallstones** (cholelithiasis) leading to **biliary obstruction** or **cholestasis**, evidenced by episodic postprandial colicky pain, nausea, vomiting, and light-colored, difficult-to-flush stools (steatorrhea due to **fat malabsorption**).
- Chronic fat malabsorption inhibits the absorption of **fat-soluble vitamins** (A, D, E, K). A deficiency in **vitamin D** is a significant risk factor for **low bone mineral density** and **osteoporosis** over time.
*Steatohepatitis*
- **Steatohepatitis** (fatty liver inflammation) is typically associated with **metabolic syndrome**, chronic alcohol use, or rapid weight loss, which are not directly indicated here.
- While gallstones can be linked to obesity, they do not directly cause steatohepatitis in the way described by the patient's acute symptoms.
*Megaloblastic anemia*
- **Megaloblastic anemia** is primarily caused by deficiencies in **vitamin B12** or **folate**.
- While malabsorption can lead to B12 deficiency (e.g., in pancreatic insufficiency affecting intrinsic factor activity), biliary obstruction directly impacts fat-soluble vitamin absorption, not primarily B12 or folate.
*Delayed wound healing*
- **Delayed wound healing** can be a symptom of **vitamin C** or **zinc deficiency**, or overall malnutrition.
- Although chronic malabsorption can lead to general malnutrition, vitamin D deficiency and its impact on bone health are a more specific and immediate long-term risk associated with the described symptoms.
*Glossitis*
- **Glossitis** (inflammation of the tongue) is typically associated with deficiencies in **vitamin B group** vitamins (e.g., B12, folate, niacin, riboflavin) or **iron deficiency**.
- While this patient might eventually develop general nutritional deficiencies, biliary obstruction leading to fat malabsorption does not directly or primarily cause these specific B vitamin deficiencies.
IBD in special populations US Medical PG Question 8: A 33-year-old primigravid visits the clinic at the 22 weeks’ gestation with concerns about several episodes of loose watery stool over the past 4 months, which are sometimes mixed with blood. Use of over-the-counter antidiarrheal medications has not been helpful. She also reports having painful ulcers in her mouth for the last 2 months. Pregnancy has been otherwise uncomplicated so far. On physical examination, the blood pressure is 110/60 mm Hg, the pulse rate is 90/min, the respiratory rate is 19/min, and the temperature is 36.6°C (97.8°F). There is bilateral conjunctival redness. Abdominal examination shows minimal tenderness but no guarding or rebound tenderness. Fundal height is proportionate to 22 weeks of gestation, and fetal heart sounds are audible. Colonoscopy shows focal areas of inflammation in the ileum, separated by normal mucosa, with rectal sparing. Based on the colonoscopy results, which of the following complications is the patient at risk for?
- A. Carcinoid syndrome
- B. Metastasis to the liver
- C. Intestinal obstruction (Correct Answer)
- D. Paralytic ileus
- E. Primary sclerosing cholangitis
IBD in special populations Explanation: ***Intestinal obstruction***
- Crohn's disease, characterized by **transmural inflammation** in the **ileum** with skipped lesions, often leads to **stricture formation** and **fibrosis**, increasing the risk of bowel obstruction.
- The patient's symptoms of chronic diarrhea and blood in the stool, coupled with oral ulcers and conjunctivitis, indicate **Crohn's disease**, which commonly affects the terminal ileum and can lead to complications such as strictures and subsequently, intestinal obstruction.
*Carcinoid syndrome*
- Carcinoid syndrome is caused by neuroendocrine tumors that secrete **vasoactive substances**, leading to symptoms like **flushing**, **diarrhea**, and **right-sided heart valve disease**.
- There is no evidence of neuroendocrine tumor activity or related systemic symptoms beyond the gastrointestinal manifestations common in inflammatory bowel disease.
*Metastasis to the liver*
- Metastasis to the liver implies a primary malignancy, and while patients with inflammatory bowel disease have an increased risk of certain cancers, there is **no direct evidence or typical presentation** in this case to suggest liver metastases.
- The patient's symptoms are more indicative of an **inflammatory process** like Crohn's disease rather than a malignant one with liver involvement.
*Paralytic ileus*
- Paralytic ileus involves a **temporary arrest of bowel motility** without mechanical obstruction, often due to abdominal surgery, peritonitis, or metabolic derangements.
- The chronic nature of the patient's symptoms and the specific colonoscopy findings pointing to **focal inflammation and strictures** are more consistent with a mechanical obstruction caused by Crohn's disease, not paralytic ileus.
*Primary sclerosing cholangitis*
- Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease often associated with **ulcerative colitis**, characterized by inflammation and fibrosis of the bile ducts.
- While PSC can be associated with inflammatory bowel disease, it is more commonly linked to **ulcerative colitis** rather than Crohn's disease, and there are no signs of cholestasis or liver involvement in this patient's presentation.
IBD in special populations US Medical PG Question 9: Five days after undergoing an open abdominal aortic aneurysm repair, a 68-year-old woman has crampy abdominal pain. During this period, she has also had two episodes of loose, bloody stools. Her surgery was complicated by severe blood loss requiring the administration of vasopressors and multiple transfusions. Cefazolin was administered as a perioperative antibiotic. The patient has hypertension, hypercholesterolemia, and coronary artery disease. The patient has smoked 2 packs of cigarettes daily for 50 years and drinks 3–4 glasses of wine every week. Her current medications include hydrochlorothiazide, atorvastatin, amlodipine, aspirin, and metoprolol. She appears ill. Her temperature is 38.0°C (100.4°F), pulse is 110/min, and blood pressure is 96/58 mm Hg. Physical examination shows a distended abdomen with absent bowel sounds. The abdomen is exquisitely tender to palpation in all quadrants. The lungs are clear to auscultation. Cardiac examination shows an S4 gallop. An x-ray of the abdomen shows air-filled distended bowel. Which of the following is the most likely diagnosis?
- A. Abdominal aortic aneurysm rupture
- B. Postoperative ileus
- C. Ischemic colitis (Correct Answer)
- D. Abdominal compartment syndrome
- E. Pseudomembranous colitis
IBD in special populations Explanation: ***Ischemic colitis***
- The patient's history of **severe blood loss**, requiring **vasopressors** and transfusions during **abdominal aortic aneurysm repair**, significantly increases the risk of **mesenteric ischemia**. The current presentation with **crampy abdominal pain**, **bloody stools**, **distended abdomen**, and **absent bowel sounds** is highly consistent with ischemic colitis, particularly given the systemic signs of illness (fever, tachycardia, hypotension).
- The use of **vasopressors** can lead to **splanchnic vasoconstriction**, reducing blood flow to the colon, especially the **watershed areas** (e.g., splenic flexure, rectosigmoid junction). This makes the colon vulnerable to ischemia following a hypotensive or hypoperfusion event.
*Abdominal aortic aneurysm rupture*
- This patient already underwent an open abdominal aortic aneurysm repair, meaning the aneurysm has been addressed. While a graft complication could occur, a new rupture of the *original* aneurysm as the primary diagnosis five days post-op is unlikely in this context.
- Abdominal aortic aneurysm rupture typically presents with **acute, severe abdominal or back pain**, often radiating to the groin or flank, and profound **hypotension** or shock due to massive blood loss into the retroperitoneum or peritoneum. There would also likely be pulsatile abdominal mass or signs of retroperitoneal hemorrhage.
*Postoperative ileus*
- **Postoperative ileus** is common after abdominal surgery and presents with **abdominal distention**, **nausea**, **vomiting**, and **absent bowel sounds**. However, it typically does not cause **bloody stools** or the systemic signs of illness like hypotension and fever seen in this patient, and it is usually not associated with exquisite tenderness in all quadrants.
- The presence of **bloody stools** strongly suggests a more serious pathology involving mucosal damage, such as ischemia or inflammation, rather than just functional bowel paralysis.
*Abdominal compartment syndrome*
- **Abdominal compartment syndrome** typically presents with progressively increasing **intra-abdominal pressure**, leading to **abdominal distention**, **tense abdomen**, and **organ dysfunction** (e.g., oliguria, respiratory compromise). While the patient has distention and severe tenderness, there's no mention of specific signs of organ compression, and bloody stools are not a primary feature.
- It usually develops acutely (within 24-48 hours) after major abdominal surgery, trauma, or massive fluid resuscitation. Although the patient had a complicated surgery, the delayed onset with bloody stools points away from isolated abdominal compartment syndrome as the primary issue.
*Pseudomembranous colitis*
- **Pseudomembranous colitis**, caused by *Clostridioides difficile* infection, is a possibility given the recent **antibiotic use (cefazolin)**. However, while it causes **crampy abdominal pain** and **diarrhea** (often bloody in severe cases), the presence of **hypotension** and the direct link to the **hypoperfusion event** during surgery make ischemic colitis a more immediate and likely diagnosis.
- Diagnosis requires detection of *C. difficile* toxin in stool. While possible, the clinical picture strongly favors ischemia due to the preceding severe blood loss and vasopressor use, which are direct risk factors for ischemic colitis.
IBD in special populations US Medical PG Question 10: Background and Methods:
Aldosterone is important in the pathophysiology of heart failure. In a double-blind study, we enrolled 1,663 patients who had severe heart failure, a left ventricular ejection fraction of no more than 35 percent, and were being treated with an angiotensin-converting-enzyme inhibitor, a loop diuretic, and in most cases digoxin. A total of 822 patients were randomly assigned to receive 25 mg of spironolactone daily and 841 to receive placebo. The primary endpoint was death from all causes.
Results:
The trial was discontinued early, after a mean follow-up period of 24 months, because an interim analysis determined that spironolactone was efficacious. There were 386 deaths in the placebo group (46%) and 284 in the spironolactone group (35%; relative risk of death, 0.70; 95% confidence interval, 0.60 to 0.82; p<0.001). This 30 percent reduction in the risk of death among patients in the spironolactone group was attributed to a lower risk of both death from progressive heart failure and sudden death from cardiac causes. The frequency of hospitalization for worsening heart failure was 35% lower in the spironolactone group than in the placebo group (relative risk of hospitalization, 0.65; 95% confidence interval, 0.54 to 0.77; p<0.001). In addition, patients who received spironolactone had a significant improvement in the symptoms of heart failure, as assessed on the basis of the New York Heart Association functional class (p<0.001). Gynecomastia was reported in 10% of men who were treated with spironolactone, as compared with 1% of men in the placebo group (p<0.001). The incidence of serious hyperkalemia was minimal in both groups of patients.
Which of the following statements represents the most accurate interpretation of the results from the aforementioned clinical trial?
- A. The incidence of both gynecomastia and hyperkalemia was elevated in patients treated with spironolactone
- B. Spironolactone, in addition to standard therapy, substantially reduces the risk of morbidity and death in patients with severe heart failure (Correct Answer)
- C. Spironolactone did not improve all-cause morbidity and mortality in patients with severe heart failure
- D. Given the large sample size of this clinical trial, the results are likely generalizable to all patients with heart failure
- E. The addition of spironolactone significantly improved symptoms of heart failure, but not overall mortality
IBD in special populations Explanation: **Spironolactone, in addition to standard therapy, substantially reduces the risk of morbidity and death in patients with severe heart failure**
- The trial showed a **30% reduction in the risk of death** and a **35% lower frequency of hospitalization** for worsening heart failure in the spironolactone group (morbidity).
- Patients receiving spironolactone also had a **significant improvement in heart failure symptoms**, as assessed by the NYHA functional class.
*The incidence of both gynecomastia and hyperkalemia was elevated in patients treated with spironolactone*
- While **gynecomastia was elevated** (10% vs 1%), the incidence of **serious hyperkalemia was minimal** in both groups, contradicting the statement that hyperkalemia was elevated.
- The text explicitly states, "The incidence of serious hyperkalemia was minimal in both groups of patients."
*Spironolactone did not improve all-cause morbidity and mortality in patients with severe heart failure*
- This statement is **directly contradicted by the results**, which showed a significant reduction in all-cause mortality (30%) and improved morbidity (35% lower hospitalization, improved symptoms).
- The trial was, in fact, "discontinued early... because an interim analysis determined that spironolactone was efficacious."
*Given the large sample size of this clinical trial, the results are likely generalizable to all patients with heart failure*
- The study specifically enrolled patients with **severe heart failure** (ejection fraction ≤ 35%) who were already on **standard therapy** (ACE inhibitor, loop diuretic, digoxin).
- Therefore, the results are generalizable to this specific subgroup of severe heart failure patients, not necessarily *all* patients with heart failure.
*The addition of spironolactone significantly improved symptoms of heart failure, but not overall mortality*
- This statement is **incorrect** as the trial explicitly reported a **30% reduction in the risk of all-cause death** in the spironolactone group (mortality).
- Additionally, it did show improvement in symptoms, meaning the first part of the statement is true, but the latter part regarding mortality is false.
More IBD in special populations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.