Diagnostic approach to IBD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic approach to IBD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic approach to IBD US Medical PG Question 1: A 33-year-old man has a history of intermittent bloody diarrhea, tenesmus, fever, fatigue, and lower abdominal cramps for the past 2 weeks. On physical examination, he is lethargic and appears lean and pale. He has aphthous stomatitis, red congested conjunctiva, and tender swollen joints. At the doctor’s office, his pulse is 114/min, blood pressure is 102/76 mm Hg, respirations are 20/min, and his temperature is 39.4°C (102.9°F). There is vague lower abdominal tenderness and frank blood on rectal examination. Laboratory studies show:
Hemoglobin 7.6 g/dL
Hematocrit 33%
Total leucocyte count 22,000/mm3
Stool assay for C.difficile is negative
Abdominal X-ray shows no significant abnormality
He is symptomatically managed and referred to a gastroenterologist, who suggests a colonoscopy and contrast (barium) study for the diagnosis. Which of the following is the most likely combination of findings in his colonoscopy and barium study?
- A. Colonoscopy: Multiple vascular malformations that resemble telangiectasias on the colon wall, Barium study: Normal
- B. Colonoscopy: Patches of mucosal erosions with pseudomembrane formation, Barium study: Cobblestone appearance with strictures
- C. Colonoscopy: Discontinuous transmural ‘skip lesions’ with aphthoid linear ulcers and transverse fissures, non-caseating granulomas, and strictures, Barium study: Cobblestone appearance with strictures
- D. Colonoscopy: Normal, Barium study: Lead pipe colon appearance
- E. Colonoscopy: Continuous ulcerated lesions involving the mucosa and submucosa, granular mucosa, crypt abscess, and pseudopolyps, Barium study: Lead pipe colon appearance (Correct Answer)
Diagnostic approach to IBD Explanation: ***Colonoscopy: Continuous ulcerated lesions involving the mucosa and submucosa granular mucosa, crypt abscess, and pseudopolyps, Barium study: Lead pipe colon appearance***
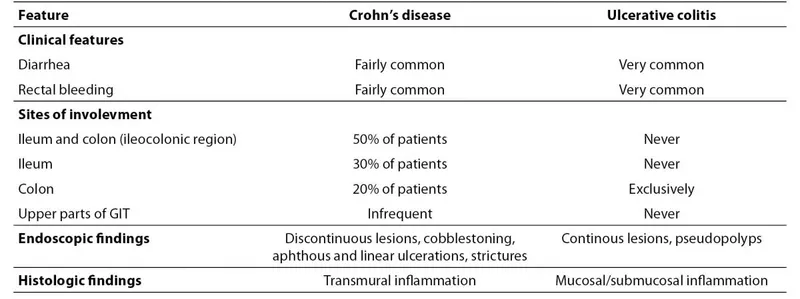
- The patient's symptoms (bloody diarrhea, tenesmus, fever, fatigue, weight loss, aphthous stomatitis, red congested conjunctiva, tender swollen joints, anemia, high WBC count) are highly suggestive of **Ulcerative Colitis (UC)**.
- **UC** on colonoscopy is characterized by **continuous mucosal and submucosal inflammation**, granular mucosa, crypt abscesses, and **pseudopolyps**. The barium study finding of a **"lead pipe" colon** is classic for long-standing UC due to loss of haustrations.
*Colonoscopy: Multiple vascular malformations that resemble telangiectasias on the colon wall, Barium study: Normal*
- **Angiodysplasia** presents with vascular malformations, but it typically causes painless lower GI bleeding, not the inflammatory symptoms described.
- The patient's severe systemic symptoms (fever, weight loss, anemia, high WBC) are inconsistent with angiodysplasia.
*Colonoscopy: Patches of mucosal erosions with pseudomembrane formation, Barium study: Cobblestone appearance with strictures*
- **Pseudomembrane formation** is characteristic of **_Clostridioides difficile_ infection**, which has been ruled out by the stool assay.
- While "cobblestone appearance" and strictures can be seen in inflammatory bowel disease, the pseudomembranes point away from UC or Crohn's.
*Colonoscopy: Discontinuous transmural ‘skip lesions’ with aphthoid linear ulcers and transverse fissures, non-caseating granulomas, and strictures, Barium study: Cobblestone appearance with strictures*
- This description is characteristic of **Crohn's disease**, which involves **discontinuous**, **transmural inflammation** with **skip lesions**, aphthoid ulcers, and non-caseating granulomas.
- While some symptoms overlap with UC, the involvement of mucocutaneous lesions and generalized systemic symptoms fits better with the continuous inflammation of UC than the patchy disease of Crohn's.
*Colonoscopy: Normal, Barium study: Lead pipe colon appearance*
- A **normal colonoscopy** would be inconsistent with the patient's severe symptoms of bloody diarrhea, anemia, and elevated inflammatory markers.
- A "lead pipe" colon indicates chronic inflammatory changes, which would undoubtedly be visible on colonoscopy.
Diagnostic approach to IBD US Medical PG Question 2: You conduct a medical research study to determine the screening efficacy of a novel serum marker for colon cancer. The study is divided into 2 subsets. In the first, there are 500 patients with colon cancer, of which 450 are found positive for the novel serum marker. In the second arm, there are 500 patients who do not have colon cancer, and only 10 are found positive for the novel serum marker. What is the overall sensitivity of this novel test?
- A. 450 / (450 + 10)
- B. 490 / (10 + 490)
- C. 490 / (50 + 490)
- D. 450 / (450 + 50) (Correct Answer)
- E. 490 / (450 + 490)
Diagnostic approach to IBD Explanation: ***450 / (450 + 50)***
- **Sensitivity** is defined as the proportion of actual positive cases that are correctly identified by the test.
- In this study, there are **500 patients with colon cancer** (actual positives), and **450 of them tested positive** for the marker, while **50 tested negative** (500 - 450 = 50). Therefore, sensitivity = 450 / (450 + 50) = 450/500 = 0.9 or 90%.
*450 / (450 + 10)*
- This formula represents **Positive Predictive Value (PPV)**, which is the probability that a person with a positive test result actually has the disease.
- It incorrectly uses the total number of **test positives** in the denominator (450 true positives + 10 false positives) instead of the total number of diseased individuals, which is needed for sensitivity.
*490 / (10 + 490)*
- This is actually the correct formula for **specificity**, not sensitivity.
- Specificity = TN / (FP + TN) = 490 / (10 + 490) = 490/500 = 0.98 or 98%, which measures the proportion of actual negative cases correctly identified.
- The question asks for sensitivity, not specificity.
*490 / (50 + 490)*
- This formula incorrectly mixes **true negatives (490)** with **false negatives (50)** in an attempt to calculate specificity.
- The correct specificity formula should use false positives (10), not false negatives (50), in the denominator: 490 / (10 + 490).
*490 / (450 + 490)*
- This calculation incorrectly combines **true negatives (490)** and **true positives (450)** in the denominator, which does not correspond to any standard epidemiological measure.
- Neither sensitivity nor specificity uses both true positives and true negatives in the denominator.
Diagnostic approach to IBD US Medical PG Question 3: A 31-year-old woman visits the clinic with chronic diarrhea on most days for the past four months. She also complains of lower abdominal discomfort and cramping, which is relieved by episodes of diarrhea. She denies any recent change in her weight. Bowel movements are preceded by a sensation of urgency, associated with mucus discharge, and followed by a feeling of incomplete evacuation. The patient went camping several months earlier, and another member of her camping party fell ill recently. Her temperature is 37° C (98.6° F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. A routine stool examination is within normal limits and blood test results show:
Hb% 13 gm/dL
Total count (WBC): 11,000/mm3
Differential count:
Neutrophils: 70%
Lymphocytes: 25%
Monocytes: 5%
ESR: 10 mm/hr
What is the most likely diagnosis?
- A. Giardiasis
- B. Ulcerative colitis
- C. Crohn’s disease
- D. Irritable bowel syndrome (Correct Answer)
- E. Laxative abuse
Diagnostic approach to IBD Explanation: ***Irritable bowel syndrome (IBS)***
- The patient's symptoms of chronic diarrhea, abdominal discomfort relieved by defecation, urgency, and incomplete evacuation, without significant weight loss or alarming signs, are highly characteristic of **Irritable Bowel Syndrome** meeting **Rome IV criteria**.
- The camping history suggests possible infectious gastroenteritis, but the **chronic duration (4 months)**, **normal stool examination**, and **absence of systemic illness** make infectious causes unlikely.
- The mild WBC elevation and normal ESR are non-specific findings; IBS is a **functional disorder** without inflammatory markers.
*Giardiasis*
- While giardiasis can cause chronic diarrhea, it often presents with **malabsorption symptoms** such as fatty stools, weight loss, and nutrient deficiencies.
- The routine stool examination being within normal limits makes giardiasis less likely, as **Giardia cysts or trophozoites** would typically be detected on microscopy.
*Ulcerative colitis*
- Ulcerative colitis is an **inflammatory bowel disease** typically characterized by bloody diarrhea, abdominal pain, and systemic symptoms like fever and weight loss.
- The patient's symptoms include the absence of blood in stools and no weight loss, with **normal ESR**, which makes ulcerative colitis unlikely.
*Crohn's disease*
- Crohn's disease is another **inflammatory bowel disease** that can affect any part of the GI tract and presents with chronic diarrhea, abdominal pain, and often systemic symptoms like weight loss, fever, or perianal disease.
- The lack of weight loss, systemic inflammation markers (normal ESR), and absence of blood or inflammatory markers in the stool make Crohn's disease less probable.
*Laxative abuse*
- Laxative abuse can cause chronic diarrhea, but it's typically associated with a history of **eating disorders** (anorexia nervosa, bulimia nervosa) or other psychological conditions, which are not mentioned in this case.
- The patient's description of abdominal discomfort relieved by defecation, urgency, and incomplete evacuation is more consistent with **IBS** (a functional bowel disorder) rather than solely laxative-induced diarrhea.
Diagnostic approach to IBD US Medical PG Question 4: A 28-year-old man comes to the physician because of a 6-month history of progressive fatigue and intermittent diarrhea. During this time, he has had a 6-kg (13-lb) weight loss. Physical examination shows pale conjunctivae. Abdominal examination shows tenderness to palpation in the lower quadrants. An image from a colonoscopy of the descending colon is shown. Further evaluation is most likely to show which of the following findings?
- A. PAS-positive cytoplasmic granules
- B. Anti-Saccharomyces cerevisiae antibodies
- C. Positive lactose hydrogen breath test
- D. Perinuclear antineutrophil cytoplasmic antibodies (Correct Answer)
- E. Anti-tissue transglutaminase antibodies
Diagnostic approach to IBD Explanation: ***Perinuclear antineutrophil cytoplasmic antibodies***
- The image provided, combined with symptoms of **fatigue**, **intermittent diarrhea**, **weight loss**, and **abdominal tenderness**, is highly suggestive of **ulcerative colitis**.
- **p-ANCA** are found in 60-70% of patients with **ulcerative colitis** and are a valuable diagnostic marker.
- The colonoscopy showing involvement of the descending colon with continuous inflammation is characteristic of UC.
*PAS-positive cytoplasmic granules*
- **PAS-positive macrophages** are characteristic of **Whipple's disease**, which typically presents with malabsorption and arthralgia.
- While Whipple's can cause GI symptoms, the endoscopic findings here are more consistent with **inflammatory bowel disease (IBD)** than with the diffuse mucosal changes of Whipple's disease.
*Anti-Saccharomyces cerevisiae antibodies*
- **Anti-Saccharomyces cerevisiae antibodies (ASCA)** are more commonly associated with **Crohn's disease**, where they are found in up to 60-70% of patients.
- The colonoscopy image, showing diffuse inflammation primarily in the descending colon without skip lesions, is more indicative of **ulcerative colitis** rather than Crohn's disease.
*Positive lactose hydrogen breath test*
- A positive lactose hydrogen breath test indicates **lactose intolerance**, which can cause diarrhea and abdominal discomfort.
- This does not explain the extensive inflammatory changes seen on colonoscopy or the progressive weight loss and anemia characteristic of IBD.
*Anti-tissue transglutaminase antibodies*
- **Anti-tissue transglutaminase antibodies** are highly specific for **celiac disease**, which presents with malabsorption, diarrhea, and weight loss.
- While celiac disease shares some symptoms, the colonoscopy findings are typical of **inflammatory bowel disease**, not celiac disease, which primarily affects the **small intestine** (duodenum and jejunum) rather than the colon.
Diagnostic approach to IBD US Medical PG Question 5: A 42-year-old woman comes to the physician because of increasing fatigue and difficulty concentrating at work for the last 2 months. She has hypertension and a 22-year history of Crohn disease. She has been hospitalized and treated for acute exacerbations, sometimes involving strictures, multiple times in the past. She has not had significant gastrointestinal symptoms in over a year. Current medications include mesalamine, thiazide, and bisoprolol. Her temperature is 37.2°C (99°F), pulse is 72/min, and blood pressure is 140/90 mm Hg. Examination shows a soft abdomen and pale conjunctivae. Rectal examination is unremarkable. Laboratory studies show:
Hemoglobin 9.4 g/dL
Mean corpuscular volume 112 fL
Mean corpuscular hemoglobin 37.2 pg/cell
Leukocyte count 8,700 /mm3
Platelet count 150,000 /mm3
Erythrocyte sedimentation rate 42 mm/h
Serum
Ferritin 88 ng/mL
Iron 117 μg/dL
Thyroid-stimulating hormone 3.2 μU/mL
Thyroxine 7 μg/dL
Further evaluation of this patient is most likely to reveal which of the following findings?
- A. Unexplained weight gain
- B. Impaired vision in her right eye
- C. Decreased vibratory sensation (Correct Answer)
- D. Tarry stools
- E. Dark-colored urine
Diagnostic approach to IBD Explanation: ***Decreased vibratory sensation***
- The patient's **macrocytic anemia** (elevated MCV of 112 fL) combined with a history of **Crohn's disease**, which often affects the **terminal ileum**, strongly suggests **vitamin B12 deficiency** due to malabsorption.
- **Vitamin B12 deficiency** can lead to **subacute combined degeneration** of the spinal cord, causing neurological symptoms like decreased vibratory sensation, proprioception, and ataxia.
*Unexplained weight gain*
- The patient has symptoms like fatigue and difficulty concentrating, which could be associated with systemic illness, but the lab findings point specifically to **anemia** and potential **malabsorption**, not weight gain.
- While some endocrine disorders can cause fatigue and weight gain, the specific hematological findings here are more indicative of a **nutritional deficiency**.
*Impaired vision in her right eye*
- Ocular symptoms are not typically associated with the **macrocytic anemia** or **Crohn's related malabsorption** described in this patient, although some inflammatory conditions associated with Crohn's can affect the eyes.
- The primary neurological findings in **vitamin B12 deficiency** are sensory and motor deficits, not acute vision loss.
*Tarry stools*
- **Tarry stools (melena)** indicate **upper gastrointestinal bleeding**, which typically causes **iron-deficiency anemia** (microcytic) rather than the macrocytic anemia observed.
- The patient has been free of significant gastrointestinal symptoms for over a year and her current lab values are inconsistent with active GI bleeding.
*Dark-colored urine*
- **Dark-colored urine** can be due to various causes such as **rhabdomyolysis**, **hemolysis**, or certain medications, but it is not a characteristic sign of **macrocytic anemia** or **vitamin B12 deficiency**.
- There are no other features in the patient's presentation or lab work (e.g., elevated bilirubin, signs of hemolytic anemia) to suggest a cause for dark urine.
Diagnostic approach to IBD US Medical PG Question 6: A 23-year-old female presents with a seven-day history of abdominal pain, and now bloody diarrhea that brings her to her primary care physician. Review of systems is notable for a 12-pound unintentional weight loss and intermittent loose stools. She has a family history notable for a father with CAD and a mother with primary sclerosing cholangitis. Upon further workup, she is found to have the following on colonoscopy and biopsy, Figures A and B respectively. Serum perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) is positive. This patient's disease is likely to also include which of the following features?
- A. Worse disease severity near the ileocecal valve
- B. Cobblestoning and skip lesions
- C. Fistulae and stricture formation
- D. Perianal disease
- E. Continuous progression beginning in the rectum (Correct Answer)
Diagnostic approach to IBD Explanation: ***Continuous progression beginning in the rectum***
- The patient's presentation with abdominal pain, bloody diarrhea, weight loss, and **positive P-ANCA** is highly suggestive of **ulcerative colitis**.
- **Ulcerative colitis** characteristically presents with **continuous inflammation** that begins in the **rectum** and extends proximally through the colon.
*Worse disease severity near the ileocecal valve*
- This feature is more characteristic of **Crohn's disease**, where the **ileocecal region** is a common site of severe involvement.
- In **ulcerative colitis**, inflammation is typically confined to the colon and does not disproportionately affect the ileocecal valve unless there is backwash ileitis.
*Cobblestoning and skip lesions*
- **Cobblestoning** and **skip lesions** are classic endoscopic findings in **Crohn's disease**, reflecting the patchy, transmural inflammation.
- **Ulcerative colitis** is characterized by diffuse, superficial inflammation without skip lesions.
*Fistulae and stricture formation*
- The formation of **fistulae** (abnormal connections between organs) and **strictures** (narrowing of the bowel lumen) are hallmarks of **Crohn's disease** due to its transmural inflammation.
- These complications are rare in **ulcerative colitis**, which primarily affects the mucosal layer.
*Perianal disease*
- **Perianal disease**, including **fissures**, **abscesses**, and **fistulae**, is a common extraintestinal manifestation and complication of **Crohn's disease**.
- While other extraintestinal manifestations like **primary sclerosing cholangitis** can occur in both, perianal disease itself is less typical for uncomplicated **ulcerative colitis**.
Diagnostic approach to IBD US Medical PG Question 7: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Diagnostic approach to IBD Explanation: ***Start annual colonoscopy starting in 8 years***
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Diagnostic approach to IBD US Medical PG Question 8: A 65-year-old man comes to the physician because of a 2-week history of dizziness, fatigue, and shortness of breath. He has noticed increased straining with bowel movements and decreased caliber of his stools over the past 3 months. He has no history of medical illness and takes no medications. He appears pale. Physical examination shows mild tachycardia and conjunctival pallor. Test of the stool for occult blood is positive. His hemoglobin concentration is 6.4 g/dL, and mean corpuscular volume is 74 μm3. A double-contrast barium enema study in this patient is most likely to show which of the following?
- A. Thumbprint sign of the transverse colon
- B. Filling defect of the rectosigmoid colon (Correct Answer)
- C. String sign in the terminal ileum
- D. Diverticula in the sigmoid colon
- E. Lead pipe sign of the descending colon
Diagnostic approach to IBD Explanation: ***Filling defect of the rectosigmoid colon***
- The patient's symptoms of **anemia** (dizziness, fatigue, shortness of breath, pallor, low Hb, microcytic MCV), **occult blood in stool**, and change in bowel habits (straining, decreased stool caliber) in a 65-year-old man are highly suspicious for **colorectal cancer**.
- **Rectosigmoid colon** is a common site for colorectal cancer, and a **filling defect** indicates a mass lesion on barium enema.
*Thumbprint sign of the transverse colon*
- The **thumbprint sign** on barium enema is indicative of **ischemic colitis**, where compromised blood flow to the colon wall causes mucosal edema and hemorrhage.
- This condition typically presents with sudden onset **abdominal pain** and bloody diarrhea, not the chronic symptoms of anemia and stool changes seen here.
*String sign in the terminal ileum*
- The **string sign** is characteristic of severe **Crohn's disease**, where chronic inflammation leads to stricture formation in the terminal ileum.
- Crohn's disease typically presents with chronic diarrhea, abdominal pain, and weight loss, and does not fit the chronic presentation of anemia and altered bowel habits seen in this case.
*Diverticula in the sigmoid colon*
- **Diverticula** are outpouchings of the colon wall, common in the sigmoid colon, and are often asymptomatic or cause mild abdominal pain and constipation.
- While diverticula can bleed, they do not explain the progressive change in stool caliber or the significant anemia consistent with a chronic bleeding mass.
*Lead pipe sign of the descending colon*
- The **lead pipe sign** refers to the loss of **haustral markings** and colonic shortening seen in chronic **ulcerative colitis**.
- Ulcerative colitis presents with bloody diarrhea, abdominal pain, and tenesmus, and while it can cause anemia, the change in stool caliber and positive occult blood without frank blood are less typical.
Diagnostic approach to IBD US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Diagnostic approach to IBD Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Diagnostic approach to IBD US Medical PG Question 10: A 34-year-old woman with no significant prior medical history presents to the clinic with several days of bloody stool. She also complains of constipation and straining, but she has no other symptoms. She has no family history of colorectal cancer or inflammatory bowel disease. She does not smoke or drink alcohol. Her vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 77/min, and respiratory rate is 15/min. There is no abdominal discomfort on physical exam, and a digital rectal exam reveals bright red blood. Of the following, which is the most likely diagnosis?
- A. Colorectal cancer
- B. Ulcerative colitis
- C. Anal fissure
- D. External hemorrhoids
- E. Internal hemorrhoids (Correct Answer)
Diagnostic approach to IBD Explanation: ***Internal hemorrhoids***
- **Painless bright red blood** per rectum, especially with **constipation and straining**, is highly characteristic of internal hemorrhoids.
- Internal hemorrhoids are located **above the dentate line**, making them typically painless, and they often prolapse during defecation, causing bleeding.
*Colorectal cancer*
- While colorectal cancer can cause bloody stool, it is less likely in a **34-year-old woman with no family history** and no other systemic symptoms like weight loss or abdominal pain.
- The bright red blood associated with straining points away from an upper GI bleed, which is more typical of many colorectal cancers.
*Ulcerative colitis*
- Ulcerative colitis typically presents with bloody diarrhea, abdominal pain, and tenesmus, which are **not mentioned** in this patient's history.
- It is a chronic inflammatory condition, and the isolated symptom of bright red blood with constipation is not classic for UC.
*Anal fissure*
- An anal fissure would cause **severe pain during defecation** due to a tear in the anal canal, which is absent in this patient.
- While an anal fissure can cause bright red blood, the lack of pain makes it less likely than hemorrhoids.
*External hemorrhoids*
- **External hemorrhoids are usually painful or itchy** and located below the dentate line.
- They also can cause bleeding, but the absence of pain and bright red blood suggests internal hemorrhoids which are more likely to bleed painlessly.
More Diagnostic approach to IBD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.