Cancer risk and surveillance in IBD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cancer risk and surveillance in IBD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cancer risk and surveillance in IBD US Medical PG Question 1: A 38-year-old man presents with concerns after finding out that his father was recently diagnosed with colon cancer. Family history is only significant for his paternal grandfather who also had colon cancer. A screening colonoscopy is performed, and a polyp is found in the ascending (proximal) colon, which on biopsy shows adenocarcinoma. A mutation in a gene that is responsible for which of the following cellular functions is the most likely etiology of this patient’s cancer?
- A. DNA mismatch repair (Correct Answer)
- B. Signal transduction
- C. Cytoskeletal stability
- D. Inhibits progression from G1 to S phase
- E. Inhibitor of apoptosis
Cancer risk and surveillance in IBD Explanation: ***DNA mismatch repair***
- The patient's presentation with **early-onset colon cancer** (38 years old), location in the **proximal colon** (ascending colon), and a **strong family history** of colon cancer in his father and paternal grandfather are highly suggestive of **Lynch syndrome (hereditary non-polyposis colorectal cancer or HNPCC)**.
- Lynch syndrome is caused by inherited mutations in **DNA mismatch repair (MMR) genes**, such as *MLH1, MSH2, MSH6*, and *PMS2*, leading to microsatellite instability and an increased risk of various cancers, particularly colorectal and endometrial.
*Signal transduction*
- Mutations in **signal transduction genes (e.g., *KRAS*, *BRAF*)** are common in sporadic colorectal cancer and lead to constitutive activation of cell growth pathways through the RAS/MAPK signaling cascade.
- While mutations in these genes are important in colorectal cancer pathogenesis, they typically do not explain the **familial aggregation, early onset, and proximal location** seen in this patient, which are hallmarks of Lynch syndrome.
*Cytoskeletal stability*
- Genes involved in cytoskeletal stability are crucial for cell structure and migration, but their primary dysfunction is not the direct cause of inherited colorectal cancer syndromes like Lynch syndrome.
- While some advanced cancers may show changes in cytoskeletal proteins, this is not the fundamental genetic defect underlying this specific familial cancer presentation.
*Inhibits progression from G1 to S phase*
- Proteins that inhibit progression from G1 to S phase are typically **tumor suppressor genes**, such as **retinoblastoma protein (Rb)** or **p53**.
- Loss of function in these genes promotes uncontrolled cell division, but mutations in *Rb* or *p53* are not the primary cause of Lynch syndrome; rather, it is characterized by defects in **DNA repair**.
*Inhibitor of apoptosis*
- Genes that inhibit apoptosis (programmed cell death) are often **oncogenes** (e.g., *BCL-2*) or genes that, when mutated, lead to resistance to apoptotic signals.
- While resistance to apoptosis is a hallmark of cancer, the fundamental defect in Lynch syndrome is impaired **DNA repair**, not primarily a direct inhibition of apoptosis.
Cancer risk and surveillance in IBD US Medical PG Question 2: A 72-year-old man presents to the emergency department with a complaint of rectal bleeding. He describes blood mixed in with the stool, which is associated with a change in his normal bowel habit such that he is going more frequently than normal. He also has some crampy left-sided abdominal pain and weight loss. His symptoms started 2 months ago, but he thought they are due to lack of dietary fiber intake and excess consumption of red meat. He has had type 2 diabetes mellitus for 35 years for which he takes metformin. He also uses daily low-dose aspirin for cardioprotection and occasional naproxen for knee pain. His family history is irrelevant. On examination, his abdomen and digital rectal examination are normal. Colonoscopy shows an ulcerating mucosal lesion with a narrow bowel lumen and biopsy shows a moderately differentiated adenocarcinoma. Which of the following is the greatest risk factor for colorectal cancer in this patient?
- A. Lack of dietary fiber intake
- B. Low-dose aspirin use
- C. Naproxen use
- D. Increasing age (Correct Answer)
- E. Metformin use
Cancer risk and surveillance in IBD Explanation: ***Increasing age***
- **Age** is the most significant **non-modifiable risk factor** for colorectal cancer, with incidence rising sharply after age 50.
- The patient's age of **72 years** places him in a high-risk category for developing colorectal cancer.
*Lack of dietary fiber intake*
- While a **low-fiber diet** is considered a risk factor for colorectal cancer, its impact is generally less significant compared to age.
- This is a **modifiable risk factor**, and its absence doesn't outweigh the inherent risk associated with advanced age.
*Low-dose aspirin use*
- **Low-dose aspirin** is known to have a **protective effect** against colorectal cancer, particularly with long-term use.
- Therefore, it would *decrease*, rather than increase, the risk in this patient.
*Naproxen use*
- **Naproxen**, an NSAID, is also associated with a **reduced risk** of colorectal cancer.
- Similar to aspirin, its use would generally be considered protective, not a risk factor.
*Metformin use*
- Studies suggest that **metformin**, used for type 2 diabetes, may have a **protective effect** against colorectal cancer.
- This medication is unlikely to be a risk factor and might even contribute to a lower risk.
Cancer risk and surveillance in IBD US Medical PG Question 3: An 18-year-old man presents with bloody diarrhea and weight loss. He undergoes endoscopic biopsy which shows pseudopolyps. Biopsies taken during the endoscopy show inflammation only involving the mucosa and submucosa. He is diagnosed with an inflammatory bowel disease. Which of the following characteristics was most likely present?
- A. Cobblestone mucosa
- B. Skip lesions
- C. Fistulas and strictures
- D. Noncaseating granuloma
- E. Rectal involvement (Correct Answer)
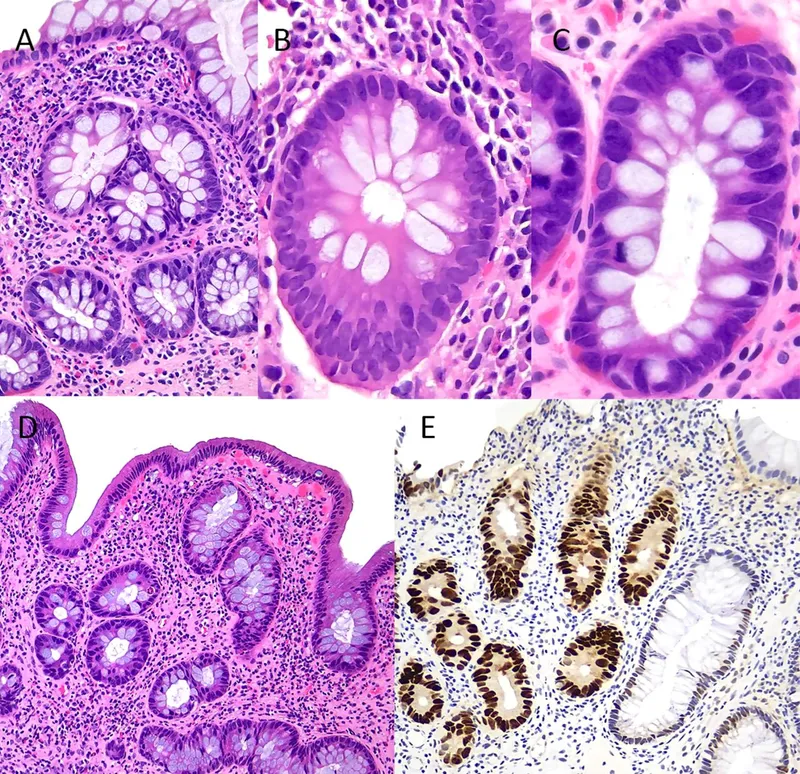
Cancer risk and surveillance in IBD Explanation: **_Rectal involvement_**
- The description of **bloody diarrhea** and **pseudopolyps** on endoscopy, along with inflammation limited to the **mucosa and submucosa**, is highly characteristic of **ulcerative colitis (UC)**. UC invariably involves the rectum and extends proximally in a continuous fashion.
- The presence of **pseudopolyps** is common in UC due to cycles of mucosal ulceration and regeneration.
*Cobblestone mucosa*
- **Cobblestone mucosa** is a classic endoscopic finding in **Crohn's disease**, resulting from deep ulcerations interspersed with islands of edematous, non-ulcerated mucosa.
- This feature points to a transmural pattern of inflammation, which is inconsistent with the superficial inflammation confined to the **mucosa and submucosa** described.
*Skip lesions*
- **Skip lesions** refer to discontinuous areas of inflammation separated by healthy tissue, a hallmark feature of **Crohn's disease**.
- **Ulcerative colitis** (implied by the superficial inflammation) is characterized by continuous inflammation extending proximally from the rectum without skipped areas.
*Fistulas and strictures*
- **Fistulas** (abnormal connections between organs or to the skin) and **strictures** (narrowing of the intestinal lumen) are complications typically associated with **Crohn's disease**, due to its **transmural inflammation**.
- These are rare in **ulcerative colitis**, which primarily affects the superficial layers of the colon.
*Noncaseating granuloma*
- The presence of **noncaseating granulomas** on biopsy is a key histological feature distinguishing **Crohn's disease** from ulcerative colitis.
- The inflammation described as restricted to the **mucosa and submucosa** makes granulomas less likely, as they often imply a transmural process.
Cancer risk and surveillance in IBD US Medical PG Question 4: A 47-year-old man presents to the clinic with a 10-day history of a sore throat and fever. He has a past medical history significant for ulcerative colitis and chronic lower back pain. He smokes at least 1 pack of cigarettes daily for 10 years. The father of the patient died of colon cancer at the age of 50. He takes sulfasalazine and naproxen. The temperature is 38.9°C (102.0°F), the blood pressure is 131/87 mm Hg, the pulse is 74/min, and the respiratory rate is 16/min. On physical examination, the patient appears tired and ill. His pharynx is erythematous with exudate along the tonsillar crypts. The strep test comes back positive. In addition to treating the bacterial infection, what else would you recommend for the patient at this time?
- A. Fecal occult blood testing
- B. Flexible sigmoidoscopy
- C. Low-dose CT
- D. PSA and digital rectal exam
- E. Colonoscopy (Correct Answer)
Cancer risk and surveillance in IBD Explanation: ***Colonoscopy***
- This patient has a history of **ulcerative colitis**, a condition known to increase the risk of **colorectal cancer**. Regular surveillance **colonoscopy** is recommended for these patients, especially with a family history of colon cancer.
- Furthermore, his father died of colon cancer at age 50, which strongly suggests a familial predisposition, making colonoscopy an urgent consideration for **cancer screening and prevention**.
*Fecal occult blood testing*
- While this test screens for **colorectal cancer**, it is generally **less sensitive and specific** than a colonoscopy, especially in high-risk individuals like this patient.
- It detects blood, which can be present due to various reasons, and a negative result does not reliably rule out **colorectal cancer** in someone with ulcerative colitis and a strong family history.
*Flexible sigmoidoscopy*
- This procedure examines only the **distal part of the colon**, which may miss lesions located in the **proximal colon**.
- For patients with **ulcerative colitis** who have an increased risk of pan-colonic cancer, a **full colonoscopy** is preferred for comprehensive surveillance.
*Low-dose CT*
- **Low-dose CT** is primarily used for **lung cancer screening** in heavy smokers, given this patient's 10-year, 1-pack-per-day history.
- While smoking is a risk factor for various cancers, it does not directly address the immediate and more significant risk for **colorectal cancer** related to his ulcerative colitis and family history.
*PSA and digital rectal exam*
- **PSA testing** and **digital rectal exams** are screening tools for **prostate cancer**.
- While important for men in a certain age range, there is **no indication** in the patient's history to suggest an urgent need for prostate cancer screening over colorectal cancer screening.
Cancer risk and surveillance in IBD US Medical PG Question 5: A 31-year-old man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. His vital signs are as follows: blood pressure is 121/81 mm Hg, heart rate is 87/min, and respiratory rate is 15/min. Rectal examination reveals a small amount of bright red blood. Lower endoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate initial treatment for this patient's underlying disease?
- A. Azathioprine
- B. Mesalamine (Correct Answer)
- C. Systemic corticosteroids
- D. Total proctocolectomy
- E. Sulfasalazine
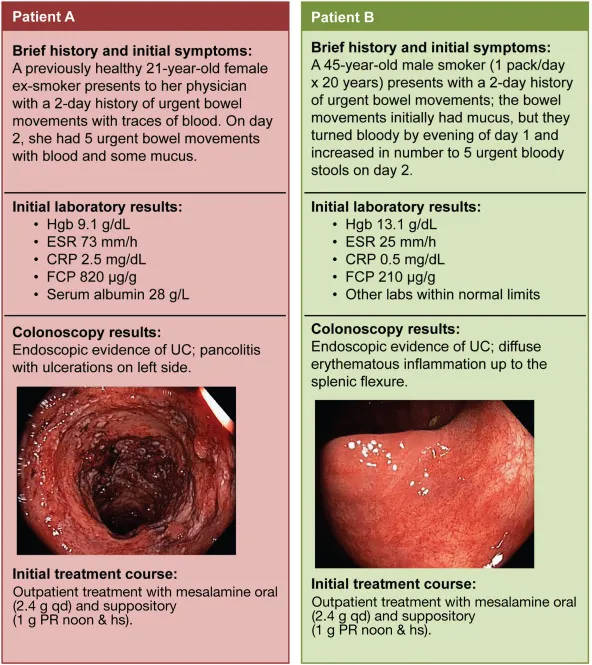
Cancer risk and surveillance in IBD Explanation: ***Mesalamine***
- The patient's symptoms (bloody diarrhea, abdominal pain, erythema, pseudopolyps, and inflammation extending from the rectum to the splenic flexure) are highly suggestive of **ulcerative colitis (UC) affecting the left colon (distal colitis)**.
- **Mesalamine** (a 5-aminosalicylic acid or 5-ASA derivative) is the first-line treatment for mild to moderate UC, especially for proctitis and left-sided colitis. Its anti-inflammatory action is exerted topically on the colonic mucosa.
*Azathioprine*
- Azathioprine is an **immunomodulator** used for maintaining remission in UC or in cases where patients are steroid-dependent or refractory to 5-ASAs.
- It is not typically used as a first-line agent for acute, mild to moderate disease.
*Systemic corticosteroids*
- **Systemic corticosteroids** are used for moderate to severe UC or for severe flares, not for initial mild to moderate disease, due to their significant side effect profile.
- While effective in inducing remission, their long-term use is limited, and they are not considered a maintenance therapy.
*Total proctocolectomy*
- **Total proctocolectomy** is a surgical option reserved for severe, refractory UC that does not respond to medical therapy, or in cases of dysplasia/cancer.
- It is an invasive procedure and not an appropriate initial treatment for a patient presenting with symptoms of mild to moderate disease.
*Sulfasalazine*
- **Sulfasalazine** is an older 5-ASA compound that is also effective for mild to moderate UC.
- However, it has a **higher incidence of side effects** (e.g., GI upset, headaches, hypersensitivity) compared to mesalamine, making mesalamine generally preferred for better tolerability.
Cancer risk and surveillance in IBD US Medical PG Question 6: A 42-year-old man comes to the physician because of a 6-week history of intermittent fever, abdominal pain, bloody diarrhea, and sensation of incomplete rectal emptying. He also has had a 4.5-kg (10-lb) weight loss over the past 3 months. Abdominal examination shows diffuse tenderness. Colonoscopy shows circumferential erythematous lesions that extend without interruption from the anal verge to the cecum. A biopsy specimen taken from the rectum shows mucosal and submucosal inflammation with crypt abscesses. This patient is most likely at risk of developing colon cancer with which of the following characteristics?
- A. Low-grade lesion
- B. Unifocal lesion
- C. Non-polypoid dysplasia (Correct Answer)
- D. Late p53 mutation
- E. Early APC mutation
Cancer risk and surveillance in IBD Explanation: ***Non-polypoid dysplasia***
- The patient's symptoms (bloody diarrhea, abdominal pain, crypt abscesses, continuous inflammation extending to the cecum) are highly suggestive of **ulcerative colitis (UC)**.
- In UC, the chronic inflammation causes a field defect across the colonic mucosa, leading to a higher risk of **non-polypoid (flat) dysplasia** and subsequent colon cancer (colitis-associated cancer).
*Low-grade lesion*
- While dysplasia can be low-grade, the primary characteristic of colon cancer development in UC is the **type of growth** (flat/non-polypoid) rather than simply its grade.
- The presence and progression of **dysplasia** (regardless of initial grade) are critical for risk stratification in UC.
*Unifocal lesion*
- Colitis-associated cancer in UC often arises from widespread field changes due to chronic inflammation, making **multifocal or diffuse dysplasia** more common than a single, isolated lesion.
- The diffuse nature of UC inflammation across the colon makes a unifocal cancerous change less typical compared to sporadic colon cancer.
*Late p53 mutation*
- **p53 mutations** are commonly found in colitis-associated colon cancer and are generally considered an **early event** in the progression from dysplasia to invasive carcinoma, rather than a late one.
- Mutations in tumor suppressor genes like **p53** contribute to genomic instability early in the neoplastic process.
*Early APC mutation*
- **APC mutations** are a hallmark of **sporadic colorectal cancer** and familial adenomatous polyposis (FAP), where they typically initiate the adenoma-carcinoma sequence.
- In **colitis-associated cancer**, APC mutations are less frequently the initiating event and often occur later, with other pathways (e.g., p53, microsatellite instability) being more prominent in early carcinogenesis.
Cancer risk and surveillance in IBD US Medical PG Question 7: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Cancer risk and surveillance in IBD Explanation: ***Start annual colonoscopy starting in 8 years***
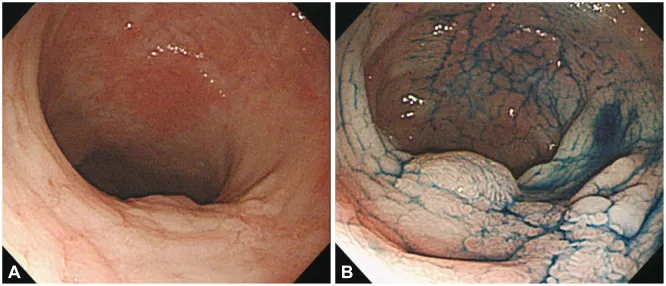
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Cancer risk and surveillance in IBD US Medical PG Question 8: A 19-year-old woman presents to the physician for a routine health maintenance examination. She has a past medical history of gastroesophageal reflux disease. She recently moved to a new city to begin her undergraduate studies. Her father was diagnosed with colon cancer at age 46. Her father's brother died because of small bowel cancer. Her paternal grandfather died because of stomach cancer. She takes a vitamin supplement. Current medications include esomeprazole and a multivitamin. She smoked 1 pack of cigarettes daily for 3 years but quit 2 years ago. She drinks 1–2 alcoholic beverages on the weekends. She appears healthy. Vital signs are within normal limits. Physical examination shows no abnormalities. Colonoscopy is unremarkable. Germline testing via DNA sequencing in this patient shows mutations in DNA repair genes MLH1 and MSH2. Which of the following will this patient most likely require at some point in her life?
- A. Celecoxib or sulindac therapy
- B. Surgical removal of a desmoid tumor
- C. Prophylactic proctocolectomy with ileoanal anastomosis
- D. Annual colonoscopy beginning at 20–25 years of age (Correct Answer)
- E. Measurement of carcinoembryonic antigen and CA 19-9 yearly
Cancer risk and surveillance in IBD Explanation: ***Annual colonoscopy beginning at 20–25 years of age***
- This patient's family history of multiple cancers at young ages (father with colon cancer at 46, uncle with small bowel cancer, grandfather with stomach cancer) combined with **germline mutations in MLH1 and MSH2** is highly indicative of **Lynch syndrome (hereditary non-polyposis colorectal cancer - HNPCC)**.
- Individuals with Lynch syndrome have a significantly increased risk of colorectal cancer, and screening with **annual colonoscopies starting at a young age (20-25 years or 2-5 years younger than the earliest age of diagnosis in the family)** is crucial for early detection and prevention.
*Celecoxib or sulindac therapy*
- **NSAID therapy** (like celecoxib or sulindac) is sometimes used for **chemoprevention in familial adenomatous polyposis (FAP)** to reduce polyp burden, especially in attenuated FAP.
- However, this patient's presentation and genetic findings point to **Lynch syndrome**, for which NSAID chemoprevention is not the primary or most effective strategy compared to surveillance.
*Surgical removal of a desmoid tumor*
- **Desmoid tumors** are benign but locally aggressive soft tissue tumors that are a characteristic **extracolonic manifestation of familial adenomatous polyposis (FAP)**, especially in patients with mutations in the APC gene.
- This patient has **Lynch syndrome**, which is associated with different extracolonic cancers (e.g., endometrial, ovarian, gastric, small bowel), but **desmoid tumors are not a typical feature of Lynch syndrome**.
*Prophylactic proctocolectomy with ileoanal anastomosis*
- **Prophylactic proctocolectomy** is the standard preventive surgery for individuals with **familial adenomatous polyposis (FAP)** to prevent the inevitable development of colorectal cancer due to hundreds to thousands of polyps.
- While Lynch syndrome carries a high risk of colorectal cancer, prophylactic colectomy is generally **not recommended as the initial management** given that surveillance via colonoscopy allows for removal of precancerous polyps and early-stage cancers, reserving surgery for when clinically indicated.
*Measurement of carcinoembryonic antigen and CA 19-9 yearly*
- **Carcinoembryonic antigen (CEA) and CA 19-9** are **tumor markers** that can be elevated in certain cancers (e.g., colorectal for CEA, pancreatic/biliary for CA 19-9).
- However, these markers have **poor sensitivity and specificity for screening healthy, asymptomatic individuals** at high risk for cancer and are primarily used for monitoring disease recurrence or treatment response in diagnosed cancers. They are not recommended for routine surveillance in Lynch syndrome.
Cancer risk and surveillance in IBD US Medical PG Question 9: A 72-year-old male visits his gastroenterologist for a check-up one year following resection of a 2-cm malignant lesion in his sigmoid colon. Serum levels of which of the following can be used in this patient to test for cancer recurrence?
- A. Gamma glutamyl transferase
- B. Cancer antigen 125 (CA-125)
- C. Alpha-fetoprotein
- D. Carcinoembryonic antigen (Correct Answer)
- E. CA-19-9 tumor marker
Cancer risk and surveillance in IBD Explanation: ***Carcinoembryonic antigen***
- **Carcinoembryonic antigen (CEA)** is the most widely used **tumor marker** for monitoring **colorectal cancer recurrence** after surgical resection.
- Elevated or rising levels of CEA in a patient previously treated for colorectal cancer suggest a high probability of **disease recurrence** or metastasis.
*Gamma glutamyl transferase*
- **Gamma glutamyl transferase (GGT)** is an enzyme primarily found in the liver and kidneys, and its elevation is typically indicative of **hepatobiliary disease** or **alcohol abuse**.
- It is not a specific marker for colorectal cancer and would not be used to monitor for recurrence.
*Cancer antigen 125 (CA-125)*
- **CA-125** is a tumor marker primarily associated with **ovarian cancer** and is used for monitoring its progression and recurrence.
- It does not have a role in the surveillance of colorectal cancer.
*Alpha-fetoprotein*
- **Alpha-fetoprotein (AFP)** is a primary tumor marker for **hepatocellular carcinoma** (liver cancer) and **germ cell tumors**.
- It is not used for monitoring colorectal cancer recurrence.
*CA-19-9 tumor marker*
- **CA-19-9** is primarily associated with **pancreatic cancer** and can also be elevated in some gastrointestinal cancers, but it is not the preferred marker for colorectal cancer surveillance.
- **CEA** is the standard and most reliable marker for **colorectal cancer recurrence**.
Cancer risk and surveillance in IBD US Medical PG Question 10: A 42-year-old woman presents to the physician because of an abnormal breast biopsy report following suspicious findings on breast imaging. Other than being concerned about her report, she feels well. She has no history of any serious illnesses and takes no medications. She does not smoke. She consumes wine 1–2 times per week with dinner. There is no significant family history of breast or ovarian cancer. Vital signs are within normal limits. Physical examination shows no abnormal findings. The biopsy shows lobular carcinoma in situ (LCIS) in the left breast. Which of the following is the most appropriate next step in management?
- A. Careful observation + routine mammography (Correct Answer)
- B. Left mastectomy + axillary dissection + local irradiation
- C. Lumpectomy + routine screening
- D. Lumpectomy + breast irradiation
- E. Breast irradiation + tamoxifen
Cancer risk and surveillance in IBD Explanation: ***Careful observation + routine mammography***
- **Lobular carcinoma in situ (LCIS)** is considered a **non-obligate precursor** to invasive carcinoma, meaning it indicates an increased risk for developing invasive breast cancer in either breast (approximately 1-2% per year), but it is not itself invasive.
- Management typically involves **careful surveillance** with routine clinical exams and **mammography**, as this is the most appropriate initial approach for classic LCIS.
- Surgical excision is often unnecessary due to LCIS's diffuse nature and the fact that it serves as a risk marker rather than a direct precancerous lesion requiring removal.
*Left mastectomy + axillary dissection + local irradiation*
- This aggressive approach is reserved for **invasive breast cancer** and would be excessive for LCIS, which is a non-invasive lesion and a marker of increased risk rather than an immediate threat.
- **Axillary dissection** is performed to stage nodal involvement in invasive cancer, which is not applicable here as LCIS does not metastasize.
*Lumpectomy + routine screening*
- While a **lumpectomy (excision)** may be considered for **pleomorphic LCIS** or when there is diagnostic uncertainty, it is not the standard initial management for classic LCIS.
- Classic LCIS is often multifocal and bilateral, making localized excision less effective as a risk-reduction strategy.
*Lumpectomy + breast irradiation*
- **Radiation therapy** is typically used to reduce local recurrence risk after **lumpectomy for invasive breast cancer** or **ductal carcinoma in situ (DCIS)**.
- For LCIS, irradiation is generally not recommended as it is non-invasive and does not benefit from local radiation treatment.
*Breast irradiation + tamoxifen*
- **Tamoxifen** is a selective estrogen receptor modulator (SERM) that can be **offered for risk reduction** in women with LCIS, potentially reducing the risk of invasive breast cancer by approximately 50%.
- However, tamoxifen is typically discussed as an **additional preventive option** after initial diagnosis and counseling, not as the immediate next step.
- **Breast irradiation** is not indicated for LCIS, as it is non-invasive and does not require local radiation treatment, making this combination inappropriate.
More Cancer risk and surveillance in IBD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.