Biologic therapies for IBD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biologic therapies for IBD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biologic therapies for IBD US Medical PG Question 1: A 22-year-old woman comes to the physician because of abdominal pain and diarrhea for 2 months. The pain is intermittent, colicky and localized to her right lower quadrant. She has anorexia and fears eating due to the pain. She has lost 4 kg (8.8 lb) during this time. She has no history of a serious illness and takes no medications. Her temperature is 37.8°C (100.0°F), blood pressure 125/65 mm Hg, pulse 75/min, and respirations 14/min. An abdominal examination shows mild tenderness of the right lower quadrant on deep palpation without guarding. Colonoscopy shows small aphthous-like ulcers in the right colon and terminal ileum. Biopsy from the terminal ileum shows noncaseating granulomas in all layers of the bowel wall. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Budesonide (Correct Answer)
- B. Azathioprine
- C. Ciprofloxacin
- D. Metronidazole
- E. Rectal mesalamine
Biologic therapies for IBD Explanation: ***Budesonide***
- This patient presents with symptoms and findings (RLQ pain, aphthous ulcers, noncaseating granulomas in the terminal ileum) consistent with **Crohn's disease** isolated to the **ileum and right colon**.
- **Budesonide** is a glucocorticoid with high first-pass metabolism, making it effective for localized ileal and right colonic Crohn's disease with fewer systemic side effects than prednisone.
*Azathioprine*
- **Azathioprine** is an immunomodulator used for maintaining remission in moderate to severe Crohn's disease, not typically for acute exacerbations as first-line monotherapy.
- Its onset of action is slow (several weeks to months), making it unsuitable for immediate symptom control.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic mainly used when there is concern for bacterial overgrowth, abscess, or perianal disease in Crohn's, none of which are explicitly indicated here.
- There is no evidence suggesting a primary bacterial infection as the cause of her current symptoms.
*Metronidazole*
- **Metronidazole** is an antibiotic often used for Crohn's disease with perianal involvement or fistulas, and sometimes for active colonic disease, but less effective for ileal involvement.
- Like ciprofloxacin, it's not the primary treatment for uncomplicated flare of ileocolonic Crohn's.
*Rectal mesalamine*
- **Rectal mesalamine** is an aminosalicylate primarily used for mild to moderate **ulcerative colitis**, particularly proctitis or left-sided colitis due to its topical action.
- It is ineffective for Crohn's disease involving the terminal ileum and right colon, as it would not reach this location in sufficient concentration.
Biologic therapies for IBD US Medical PG Question 2: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Biologic therapies for IBD Explanation: ***NF-κB***
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
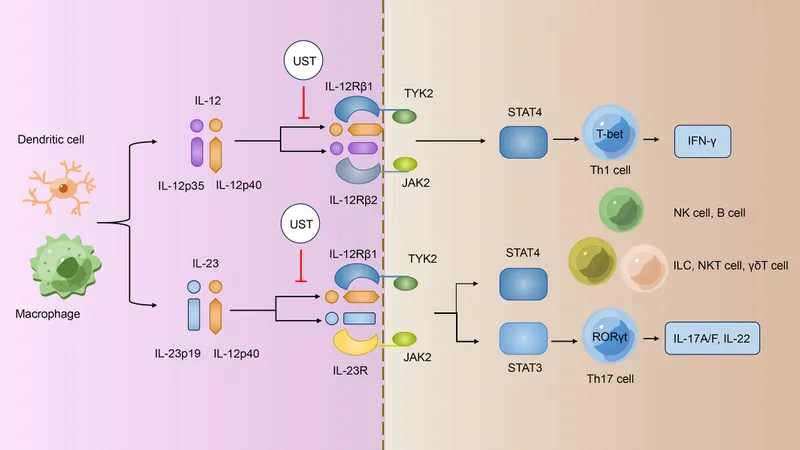
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
Biologic therapies for IBD US Medical PG Question 3: A 33-year-old woman with a history of multiple sclerosis is brought to the physician because of dizziness, urinary incontinence, loss of vision in her right eye, and numbness and weakness of the left leg. She has had recurrent episodes of neurological symptoms despite several changes in her medication regimen. An MRI of the brain shows several new enhancing lesions in the periventricular white matter and the brainstem. Treatment with a drug that binds to CD52 is initiated. Which of the following agents was most likely prescribed?
- A. Alemtuzumab (Correct Answer)
- B. Eculizumab
- C. Abciximab
- D. Rituximab
- E. Bevacizumab
Biologic therapies for IBD Explanation: ***Alemtuzumab***
- **Alemtuzumab** is a monoclonal antibody that targets **CD52**, a glycoprotein found on the surface of mature lymphocytes (T and B cells), monocytes, and macrophages, leading to their depletion.
- It is used in **highly active relapsing-remitting multiple sclerosis (RRMS)**, especially when other disease-modifying therapies have failed, which aligns with the patient's history of recurrent neurological symptoms and new enhancing lesions.
*Eculizumab*
- **Eculizumab** targets the **C5 complement protein** and is used for conditions like **paroxysmal nocturnal hemoglobinuria** and **atypical hemolytic uremic syndrome**, not multiple sclerosis.
- It works by inhibiting the complement cascade, which is not the primary mechanism of action for MS treatment involving lymphocyte depletion.
*Abciximab*
- **Abciximab** is a **glycoprotein IIb/IIIa inhibitor** that prevents platelet aggregation and is used as an antiplatelet agent in acute coronary syndromes and percutaneous coronary intervention.
- Its mechanism of action and primary indication are unrelated to the immunological processes involved in multiple sclerosis.
*Rituximab*
- **Rituximab** targets **CD20** on B cells and is used in conditions like **non-Hodgkin lymphoma**, **chronic lymphocytic leukemia**, and certain autoimmune diseases like **rheumatoid arthritis** and **vasculitis**.
- While it's a B-cell depleting agent and has shown efficacy in MS, the question specifically asks for a drug that binds to **CD52**, not CD20.
*Bevacizumab*
- **Bevacizumab** is an anti-VEGF antibody that inhibits **angiogenesis** and is primarily used in the treatment of various cancers, such as colorectal, lung, and renal cell carcinoma.
- Its mechanism of action involving inhibition of vascular endothelial growth factor (VEGF) is not indicated for the management of multiple sclerosis.
Biologic therapies for IBD US Medical PG Question 4: A 22-year-old man comes to the physician for a follow-up evaluation for chronic lower back pain. He has back stiffness that lasts all morning and slowly improves throughout the day. He has tried multiple over-the-counter medications, including ibuprofen, without any improvement in his symptoms. Physical examination shows tenderness over the iliac crest bilaterally and limited range of motion of the lumbar spine with forward flexion. The results of HLA-B27 testing are positive. An x-ray of the lumbar spine shows fusion of the lumbar vertebrae and sacroiliac joints. The physician plans to prescribe a new medication but first orders a tuberculin skin test to assess for the risk of latent tuberculosis reactivation. Inhibition of which of the following is the most likely primary mechanism of action of this drug?
- A. mTOR kinase
- B. Calcineurin
- C. NF-κB
- D. Inosine monophosphate dehydrogenase
- E. TNF-α (Correct Answer)
Biologic therapies for IBD Explanation: **TNF-α**
- The clinical presentation with **chronic lower back pain**, morning stiffness, **limited lumbar spine range of motion**, positive **HLA-B27**, and **fusion of lumbar vertebrae and sacroiliac joints** is highly suggestive of **ankylosing spondylitis**.
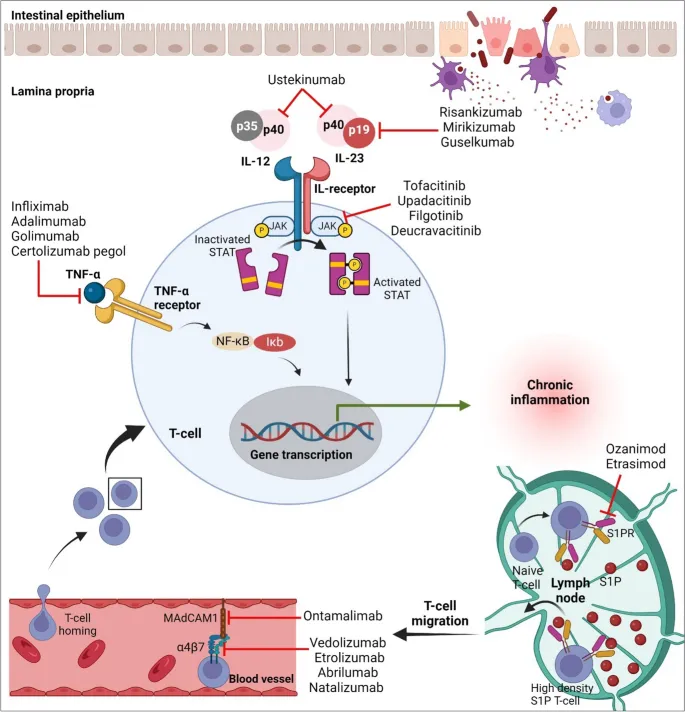
- Biologic medications, specifically **TNF-α inhibitors**, are a cornerstone of treatment for ankylosing spondylitis, especially when conventional therapies like NSAIDs fail. The mention of screening for latent tuberculosis reactivation strongly points to the use of a TNF-α inhibitor, as these drugs increase the risk of TB reactivation.
*mTOR kinase*
- **mTOR inhibitors** (e.g., sirolimus, everolimus) are primarily used as **immunosuppressants** in organ transplantation and in some cancers.
- They are not a first-line or common treatment for ankylosing spondylitis or other spondyloarthropathies.
*Calcineurin*
- **Calcineurin inhibitors** (e.g., cyclosporine, tacrolimus) are potent **immunosuppressants** used in transplant rejection prevention and some autoimmune diseases.
- While they can have immunosuppressive effects, they are not the primary target for the treatment of ankylosing spondylitis.
*NF-κB*
- **NF-κB** is a crucial transcription factor involved in inflammation and immune responses. While relevant to inflammatory conditions, directly targeting NF-κB is not the primary mechanism of action for the most effective biologic therapies used in ankylosing spondylitis.
- **Glucocorticoids** can inhibit NF-κB, but they are not the main long-term treatment for ankylosing spondylitis, and the context points to a biologic.
*Inosine monophosphate dehydrogenase*
- **Inosine monophosphate dehydrogenase (IMPDH) inhibitors** (e.g., mycophenolate mofetil) block purine synthesis, thus inhibiting lymphocyte proliferation.
- These drugs are used in **transplantation** and some **autoimmune diseases** (e.g., lupus, vasculitis) but are not typically used for ankylosing spondylitis.
Biologic therapies for IBD US Medical PG Question 5: A 38-year-old woman comes to the physician for a follow-up examination. Two years ago, she was diagnosed with multiple sclerosis. Three weeks ago, she was admitted and treated for right lower leg weakness with high-dose methylprednisone for 5 days. She has had 4 exacerbations over the past 6 months. Current medications include interferon beta and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 116/74 mm Hg. Examination shows pallor of the right optic disk. Neurologic examination shows no focal findings. She is anxious about the number of exacerbations and repeated hospitalizations. She is counseled about the second-line treatment options available to her. She consents to treatment with natalizumab. However, she has read online about its adverse effects and is concerned. This patient is at increased risk for which of the following complications?
- A. Tuberculosis
- B. Syndrome of inappropriate antidiuretic hormone
- C. Parkinsonism
- D. Progressive multifocal leukoencephalopathy (Correct Answer)
- E. Aplastic anemia
Biologic therapies for IBD Explanation: ***Progressive multifocal leukoencephalopathy***
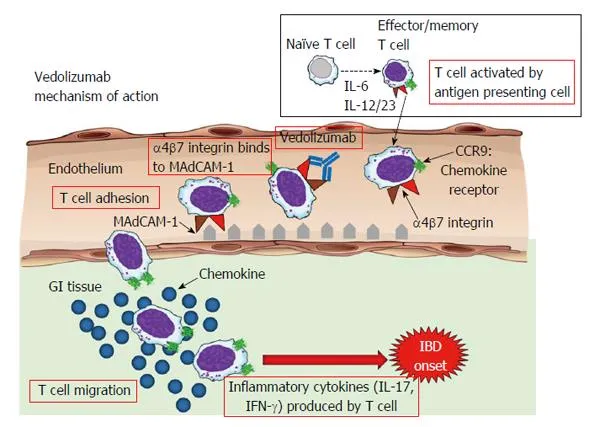
- **Natalizumab** is a monoclonal antibody that blocks the binding of leukocytes to endothelial cells, preventing their entry into the central nervous system. This immunosuppressive effect increases the risk of **progressive multifocal leukoencephalopathy (PML)**, especially in patients who are positive for the **JC virus**.
- PML is a serious and often fatal opportunistic infection of the brain caused by the **JC virus**, which demyelinates axons and leads to severe neurological deficits.
*Tuberculosis*
- While some immunosuppressants can reactivate **latent tuberculosis**, natalizumab is not typically associated with an increased risk of TB compared to other immunomodulatory drugs like TNF-alpha inhibitors.
- The mechanism of action of natalizumab (alpha-4 integrin blocker) does not directly impede the immune response responsible for containing mycobacterial infections to the same extent as other treatments.
*Syndrome of inappropriate antidiuretic hormone*
- **SIADH** is not a known adverse effect of natalizumab.
- SIADH is characterized by excessive secretion of **antidiuretic hormone**, leading to hyponatremia, and is often associated with certain medications (e.g., SSRIs, carbamazepine) or underlying conditions like malignancy or pulmonary disease.
*Parkinsonism*
- Parkinsonism involves symptoms like **bradykinesia**, rigidity, and tremor, and is a neurodegenerative disorder.
- There is **no evidence** suggesting a causal link between natalizumab treatment and the development of Parkinsonism.
*Aplastic anemia*
- **Aplastic anemia** is a rare but severe condition where the bone marrow fails to produce blood cells.
- This adverse effect is not associated with natalizumab; it is more commonly linked to certain **chemotherapeutic agents**, radiation, or specific antimicrobial drugs like chloramphenicol.
Biologic therapies for IBD US Medical PG Question 6: For which patient would isoniazid monotherapy be most appropriate?
- A. 50-year-old male with positive PPD, active tuberculosis and poor compliance to multidrug regimens
- B. 25-year-old female with positive PPD and acid-fast bacilli on sputum stain
- C. 41-year-old female with positive PPD and a Ghon complex on chest radiograph
- D. 37-year-old male with positive PPD and no clinical signs or radiographic evidence of disease (Correct Answer)
- E. 31-year-old male with negative PPD but recent exposure to someone with active tuberculosis
Biologic therapies for IBD Explanation: ***37-year-old male with positive PPD and no clinical signs or radiographic evidence of disease***
- This patient has **latent tuberculosis infection (LTBI)**, characterized by a positive PPD (indicating immune response to TB exposure) with no symptoms or radiographic findings of active disease.
- **Isoniazid monotherapy** (6-9 months) is the standard treatment for LTBI to prevent progression to active tuberculosis.
- This is the classic indication for isoniazid monotherapy.
*50-year-old male with positive PPD, active tuberculosis and poor compliance to multidrug regimens*
- This patient has **active tuberculosis**, which absolutely requires **multidrug therapy** (minimum 4 drugs: isoniazid, rifampin, pyrazinamide, and ethambutol) regardless of compliance issues.
- Isoniazid monotherapy in active TB would rapidly lead to **drug resistance** and treatment failure.
- Poor compliance is managed with directly observed therapy (DOT), not by simplifying to monotherapy.
*25-year-old female with positive PPD and acid-fast bacilli on sputum stain*
- **Acid-fast bacilli on sputum stain** confirms **active pulmonary tuberculosis**, which requires multidrug therapy.
- Isoniazid monotherapy would be inadequate and promote drug resistance.
*41-year-old female with positive PPD and a Ghon complex on chest radiograph*
- A **Ghon complex** (calcified granuloma with associated lymph node) represents a **healed primary TB infection**.
- While this patient may have LTBI (positive PPD), the presence of radiographic findings requires further evaluation to rule out active or reactivation TB before considering monotherapy.
- Standard practice would include additional workup (sputum cultures, clinical assessment) rather than proceeding directly to monotherapy.
*31-year-old male with negative PPD but recent exposure to someone with active tuberculosis*
- A **negative PPD** can occur during the **window period** (initial 8-10 weeks after exposure before the immune response develops).
- While **post-exposure prophylaxis** may be considered in recent close contacts per CDC guidelines (with repeat testing in 8-10 weeks), the patient with documented LTBI (positive PPD without active disease) remains the most clear-cut indication for isoniazid monotherapy.
- The correct answer represents the most straightforward and standard indication.
Biologic therapies for IBD US Medical PG Question 7: A 34-year-old man with a 2-year history of rheumatoid arthritis is being evaluated on a follow-up visit. He is currently on methotrexate and celecoxib for pain management and has shown a good response until now. However, on this visit, he mentions that the morning stiffness has been getting progressively worse. On physical examination, both his wrists are erythematous and swollen, nodules on his elbows are also noted. Rheumatoid factor is 30 (normal reference values: < 15 IU/mL), ESR is 50 mm/h, anti-citrullinated protein antibodies is 55 (normal reference values: < 20). What is the next best step in the management of this patient?
- A. Sulfasalazine
- B. Adalimumab monotherapy
- C. Methotrexate and Corticosteroids
- D. Methotrexate and Infliximab (Correct Answer)
- E. Infliximab monotherapy
Biologic therapies for IBD Explanation: **Methotrexate and Infliximab**
- The patient is experiencing a **flare-up of rheumatoid arthritis** despite being on methotrexate, indicated by worsening morning stiffness, active synovitis (erythematous and swollen wrists), elevated ESR, and positive rheumatoid factor and anti-CCP. This suggests a need for more aggressive therapy, and adding a **biologic agent like infliximab (an anti-TNF agent)** to methotrexate is a standard approach for moderate to severe RA that is not adequately controlled by methotrexate monotherapy.
- Combination therapy with **methotrexate and a biologic DMARD** (e.g., TNF inhibitors like infliximab) has been shown to be more effective than monotherapy for controlling disease activity and preventing joint damage in refractory RA.
*Sulfasalazine*
- **Sulfasalazine** is a conventional synthetic DMARD that is generally used as a **first-line agent or in combination therapy** for mild to moderate RA.
- Given the patient's ongoing active disease despite methotrexate and the severity of his symptoms, sulfasalazine is unlikely to be sufficient to achieve disease control.
*Adalimumab monotherapy*
- While adalimumab (another anti-TNF biologic) is an effective treatment for RA, **biologic monotherapy is generally less effective** than combination therapy with methotrexate.
- Current guidelines and clinical practice favor combining biologic DMARDs with methotrexate for optimal outcomes in RA management, especially in patients with active disease.
*Methotrexate and Corticosteroids*
- **Corticosteroids** are effective in rapidly reducing inflammation and can be used for **short-term management of RA flares**.
- However, corticosteroids are not recommended for long-term use due to significant side effects and do not address the underlying disease progression as comprehensively as biologic DMARDs in patients refractory to methotrexate.
*Infliximab monotherapy*
- Similar to adalimumab monotherapy, **infliximab is typically more effective when combined with methotrexate**.
- Using infliximab alone would be a less optimal choice for this patient whose disease is clearly not controlled by methotrexate, as it may lead to a suboptimal response and potentially increase the risk of developing anti-drug antibodies.
Biologic therapies for IBD US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Biologic therapies for IBD Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Biologic therapies for IBD US Medical PG Question 9: A 21-year-old woman presents with malaise, joint pains, and a rash that worsens with sun exposure. Examination reveals an erythematous facial rash with edema. Her complete blood count shows lymphocytopenia. In addition to the most likely diagnosis, which of the following disorders can also cause lymphocytopenia? I. HIV II. Autoimmune disorders III. Tuberculosis IV. Lymphoma V. Hypersplenism
- A. I, II, IV, V (Correct Answer)
- B. III, V
- C. I, II, III
- D. III, IV
- E. I, III, V
Biologic therapies for IBD Explanation: ***I, II, IV, V***
- The patient's symptoms (malar rash, photosensitivity, joint pains, malaise, lymphocytopenia) are highly suggestive of **Systemic Lupus Erythematosus (SLE)**, an **autoimmune disorder** (II).
- **HIV (I)** directly destroys CD4+ T lymphocytes, causing profound lymphocytopenia.
- **Autoimmune disorders (II)** like SLE, rheumatoid arthritis, and Sjögren's syndrome cause lymphocytopenia via antibody-mediated destruction.
- **Lymphoma (IV)** causes lymphocytopenia through bone marrow infiltration, increased consumption, or sequestration.
- **Hypersplenism (V)** causes sequestration and destruction of lymphocytes along with other blood cells.
- While disseminated tuberculosis can occasionally cause lymphocytopenia, **chronic tuberculosis typically causes lymphocytosis**, making it a less reliable answer.
*III, V*
- This option is incomplete as it correctly identifies hypersplenism but omits HIV, autoimmune disorders, and lymphoma, which are more consistent causes of lymphocytopenia.
- **Tuberculosis (III)** in its chronic form typically causes **lymphocytosis**, not lymphocytopenia, though severe disseminated disease may cause lymphocytopenia.
*I, II, III*
- While HIV and autoimmune disorders are correct, including **tuberculosis (III)** is problematic as chronic TB typically causes **lymphocytosis**, not lymphocytopenia.
- This option omits lymphoma and hypersplenism, both important causes.
*III, IV*
- **Tuberculosis (III)** in chronic form typically causes **lymphocytosis** rather than lymphocytopenia, making it an unreliable choice.
- Although **lymphoma (IV)** is correct, this option excludes HIV, autoimmune disorders, and hypersplenism.
*I, III, V*
- **HIV (I)** and **hypersplenism (V)** are valid causes, but **tuberculosis (III)** is inconsistent as chronic TB typically causes lymphocytosis.
- This option incorrectly includes tuberculosis while omitting autoimmune disorders and lymphoma.
Biologic therapies for IBD US Medical PG Question 10: A 52-year-old man comes to the physician because his skin has been progressively yellowing for the past 4 weeks. He also reports low appetite and difficulty fitting into his pants because of his swollen legs over the past several months. There is no personal or family history of serious illness. He does not smoke and drinks 1 to 2 beers on special occasions. He used to be sexually active with multiple female partners but has lost interest in sexual intercourse recently. He is 178 cm (5 ft 10 in) tall and weighs 68 kg (150 lb); his BMI is 22 kg/m2. Vital signs are within normal limits. Physical examination shows yellowing of the skin and sclera as well as erythema of the palms. There is bilateral enlargement of breast tissue. Cardiopulmonary examinations show no abnormalities. The abdomen is distended. The liver is palpated 2 to 3 cm below the right costal margin. On percussion of the left abdomen, a thrill can be felt on the right side. Hepatojugular reflux is absent. There is bilateral edema below the knees. Which of the following is the most likely underlying cause of this patient's condition?
- A. Autoimmune hepatitis
- B. Congestive hepatopathy
- C. Primary biliary cirrhosis
- D. Chronic viral hepatitis (Correct Answer)
- E. Non-alcoholic steatohepatitis
Biologic therapies for IBD Explanation: ***Chronic viral hepatitis***
- The patient's history of **multiple sexual partners** and subsequent development of **jaundice**, **ascites** (distended abdomen with thrill on percussion), **palmar erythema**, **gynecomastia** (bilateral enlarged breast tissue), and **peripheral edema** are highly suggestive of **decompensated chronic liver disease**, such as **cirrhosis**.
- **Chronic viral hepatitis** (e.g., Hepatitis B or C) is a very common cause of cirrhosis, especially in patients with a history of risky behaviors like unprotected sexual intercourse.
*Autoimmune hepatitis*
- While it can cause cirrhosis, **autoimmune hepatitis** typically presents with elevated **liver enzymes** (AST, ALT) and specific **autoantibodies** (e.g., ANA, anti-smooth muscle antibodies), which are not mentioned here.
- There is no specific risk factor for autoimmune disease in this patient's history.
*Congestive hepatopathy*
- This condition results from **right-sided heart failure**, causing engorgement of the liver and potentially cirrhosis. The absence of **hepatojugular reflux** makes this diagnosis less likely.
- Symptoms like **jugular venous distention** and **cardiac murmurs** associated with heart failure would typically be present.
*Primary biliary cirrhosis*
- This is a **cholestatic liver disease** primarily affecting **middle-aged women** and is characterized by **pruritus**, **fatigue**, and elevated **alkaline phosphatase**.
- The patient's gender and lack of specific cholestatic symptoms make this less probable.
*Non-alcoholic steatohepatitis*
- While **NASH** can progress to cirrhosis, the patient's **normal BMI**, lack of significant **alcohol intake**, and no history of **diabetes** or **dyslipidemia** make this diagnosis less likely.
- NASH is strongly associated with **metabolic syndrome**.
More Biologic therapies for IBD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.