Venous thromboembolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Venous thromboembolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Venous thromboembolism US Medical PG Question 1: A 43-year-old woman was admitted to the hospital for anticoagulation following a pulmonary embolism. She was found to have a deep venous thrombosis on further workup after a long plane ride coming back from visiting China. She denies any personal history of blood clots in her past, but she says that her mother has also had to be treated for pulmonary embolism in the recent past. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and she currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min, and respiratory rate 23/min. On physical examination, her pulses are bounding and complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 81% on room air, with a new oxygen requirement of 8 L by face mask. On day 6 of combined heparin and warfarin anticoagulation, her platelet count decreases from 182,000/mcL to 63,000/mcL. Her international normalized ratio (INR) is not yet therapeutic. What is the next best step in therapy?
- A. Continue heparin and warfarin until INR is therapeutic for 24 hours
- B. Discontinue heparin and warfarin (Correct Answer)
- C. Continue heparin and warfarin, and administer vitamin K
- D. Discontinue heparin; continue warfarin
- E. Continue heparin; discontinue warfarin
Venous thromboembolism Explanation: ***Discontinue heparin and warfarin***
- The significant drop in platelet count (from 182,000 to 63,000/mcL) on day 6 of heparin therapy strongly suggests **heparin-induced thrombocytopenia (HIT)**, an immune-mediated adverse drug reaction.
- **Immediate management requires:** (1) discontinuation of ALL heparin products, and (2) initiation of an alternative non-heparin anticoagulant such as a direct thrombin inhibitor (argatroban, bivalirudin) or fondaparinux.
- Warfarin must NOT be continued as monotherapy in HIT because it causes transient **hypercoagulability** due to depletion of protein C and S before depleting clotting factors, which can worsen thrombotic complications.
- **Among the options provided**, discontinuing both heparin and warfarin is the correct first step, with the understanding that alternative anticoagulation would be initiated immediately in practice.
*Continue heparin and warfarin until INR is therapeutic for 24 hours*
- Continuing heparin would be dangerous given the suspected **HIT**, as it could lead to further platelet activation, worsening thrombocytopenia, and an increased risk of **paradoxical thrombosis**.
- While achieving therapeutic anticoagulation is important for PE/DVT, the priority is managing the acute, life-threatening complication of HIT.
*Continue heparin and warfarin, and administer vitamin K*
- Administering vitamin K would reverse warfarin effects, which is contraindicated in a patient requiring anticoagulation for PE and DVT unless there is active bleeding or supratherapeutic INR.
- Continuing heparin in the setting of suspected **HIT** is contraindicated and would exacerbate the prothrombotic state.
*Discontinue heparin; continue warfarin*
- While discontinuing heparin is correct in suspected **HIT**, continuing warfarin alone is **dangerous** and contraindicated.
- Warfarin monotherapy in acute HIT causes transient **hypercoagulability** due to rapid depletion of protein C and S (shorter half-lives) before depletion of clotting factors II, IX, and X, leading to increased thrombotic risk including **warfarin-induced venous limb gangrene**.
- An **alternative non-heparin anticoagulant** (direct thrombin inhibitor or fondaparinux) must be initiated before warfarin can be safely restarted.
*Continue heparin; discontinue warfarin*
- Continuing heparin in the presence of a rapid and significant drop in platelet count is **contraindicated** due to the high suspicion of **HIT**.
- Discontinuing warfarin alone would leave the patient exposed to continued HIT complications while still receiving the offending agent (heparin).
Venous thromboembolism US Medical PG Question 2: A 26-year-old man presents with a 2-day history of worsening right lower leg pain. He states that he believes his right leg is swollen when compared to his left leg. Past medical history is significant for generalized anxiety disorder, managed effectively with psychotherapy. He smokes a pack of cigarettes daily but denies alcohol and illicit drug use. His father died of a pulmonary embolism at the age of 43. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, respiratory rate 14/min. On physical examination, the right lower leg is warmer than the left, and dorsiflexion of the right foot produces pain. Which of the following conditions is most likely responsible for this patient’s presentation?
- A. Vitamin K deficiency
- B. Hemophilia A
- C. von Willebrand disease
- D. Factor V Leiden (Correct Answer)
- E. Factor XI deficiency
Venous thromboembolism Explanation: ***Factor V Leiden***
- The patient presents with classic symptoms of a **deep vein thrombosis (DVT)** in the right lower leg: pain, swelling, warmth, and pain on dorsiflexion (**Homans' sign**). His history of smoking and a family history of **pulmonary embolism (PE)** in a young father strongly suggest an underlying **thrombophilia**.
- **Factor V Leiden** is the most common inherited thrombophilia, predisposing individuals to venous thromboembolism. The constellation of symptoms and risk factors points directly to this condition.
*Vitamin K deficiency*
- **Vitamin K deficiency** primarily leads to impaired production of clotting factors II, VII, IX, and X, resulting in a **bleeding diathesis**, not thrombotic events.
- Patients would typically present with **bruising, petechiae, gastrointestinal bleeding, or hematuria**, which are not seen here.
*Hemophilia A*
- **Hemophilia A** is an X-linked recessive disorder characterized by a deficiency of **Factor VIII**, leading to severe **bleeding**.
- Symptoms include **spontaneous or prolonged bleeding** into joints (hemarthrosis), muscles, or following trauma, which is the opposite of the patient's presentation.
*von Willebrand disease*
- **Von Willebrand disease (vWD)** is the most common inherited bleeding disorder, caused by a deficiency or defect in **von Willebrand factor**.
- It primarily causes **mucocutaneous bleeding**, such as epistaxis, menorrhagia, and easy bruising, not thrombotic episodes.
*Factor XI deficiency*
- **Factor XI deficiency** is a rare inherited bleeding disorder that typically causes **mild to moderate bleeding**, often associated with trauma or surgery.
- It is not associated with an increased risk of thrombosis and would present with bleeding, not a DVT.
Venous thromboembolism US Medical PG Question 3: A 62-year-old man comes to the physician because of a 5-day history of swelling in his left arm. Two months ago, he was diagnosed with a deep venous thrombosis in the left calf. He has had a 7-kg (15-lb) weight loss in the last 3 months. He has smoked 1 pack of cigarettes daily for the past 25 years. His only medication is warfarin. Physical examination shows warm edema of the left forearm with overlying erythema and a tender, palpable cord-like structure along the medial arm. His lungs are clear to auscultation bilaterally. Duplex sonography shows thrombosis of the left basilic and external jugular veins. Which of the following is the most appropriate next step to confirm the underlying diagnosis?
- A. CT scan of the chest
- B. X-ray of the chest (Correct Answer)
- C. Transesophageal echocardiography
- D. Serum antiphospholipid antibody level
- E. Serum D-dimer level
Venous thromboembolism Explanation: **X-ray of the chest**
- The patient presents with **recurrent deep venous thrombosis (DVT)**, specifically in an unusual location (upper extremity), combined with **unexplained weight loss** and a **significant smoking history**. These are strong indicators of an underlying malignancy.
- A **chest x-ray** is a readily available and cost-effective initial screening tool to evaluate for **lung cancer**, which is common in smokers and can present with paraneoplastic phenomena like hypercoagulability (Trousseau phenomenon) leading to DVT.
*CT scan of the chest*
- While a **CT scan of the chest** is more sensitive than an X-ray for detecting lung masses, an **X-ray is the more appropriate initial step** for screening given the clinical context.
- A **CT scan** would typically be performed after an abnormal chest X-ray or if clinical suspicion remains high despite a normal X-ray.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** is primarily used to evaluate **cardiac structures**, valve function, and to detect intracardiac thrombi or vegetations.
- It is not indicated as a primary screening tool for an underlying malignancy or in the workup of a **venous thrombosis** not directly related to cardiac pathology.
*Serum antiphospholipid antibody level*
- **Antiphospholipid antibody syndrome** is a cause of recurrent thrombosis, but the patient's other symptoms (weight loss, smoking history, unusual DVT location) point more strongly towards an underlying malignancy.
- While it might be considered in a broader workup for hypercoagulability, it is not the most immediate next step given the constellation of findings strongly suggestive of cancer.
*Serum D-dimer level*
- A **serum D-dimer level** is a marker of fibrin degradation and is useful for **excluding DVT/PE** in low-probability patients.
- In this patient, a DVT has already been diagnosed by duplex sonography, so a D-dimer level would not provide additional diagnostic information regarding the presence of thrombosis, nor would it help in identifying the underlying cause of the recurrent thrombosis.
Venous thromboembolism US Medical PG Question 4: A 43-year-old woman presents to her primary care physician with complaints of mild shortness of breath and right-sided chest pain for three days. She reports that lately she has had a nagging nonproductive cough and low-grade fevers. On examination, her vital signs are: temperature 99.1 deg F (37.3 deg C), blood pressure is 115/70 mmHg, pulse is 91/min, respirations are 17/min, and oxygen saturation 97% on room air. She is well-appearing, with normal work of breathing, and no leg swelling. She is otherwise healthy, with no prior medical or surgical history, currently taking no medications. The attending has a low suspicion for the most concerning diagnosis and would like to exclude it with a very sensitive though non-specific test. Which of the following should this physician order?
- A. Obtain chest radiograph
- B. Obtain spiral CT chest with IV contrast
- C. Order a lower extremity ultrasound
- D. Order a D-dimer (Correct Answer)
- E. Obtain ventilation-perfusion scan
Venous thromboembolism Explanation: ***Order a D-dimer***
- The physician has a **low suspicion based on clinical assessment** and wants to **exclude** a concerning diagnosis (likely **pulmonary embolism** or PE) using a **sensitive test**. A negative D-dimer test can effectively rule out PE in patients with a low pre-test probability.
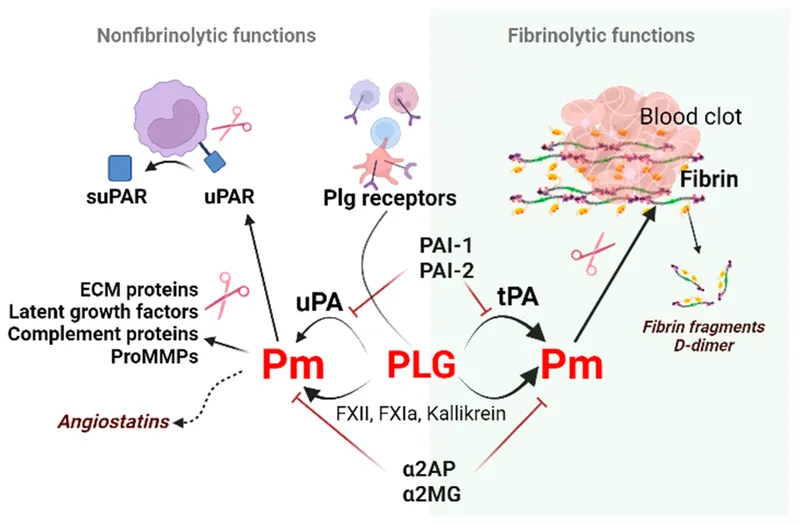
- The D-dimer is a product of **fibrin degradation** and its elevation indicates recent or ongoing **thrombus formation** and lysis. It is highly sensitive for PE but has low specificity.
*Obtain chest radiograph*
- A chest radiograph is often **normal in pulmonary embolism** or may show non-specific findings, making it unsuitable for ruling out PE.
- While useful for diagnosing other conditions like pneumonia or pleural effusions, it is **not sensitive enough to exclude PE**.
*Obtain spiral CT chest with IV contrast*
- A **spiral CT chest with IV contrast (CT pulmonary angiography)** is the gold standard for diagnosing PE, but it is **not a sensitive rule-out test** for low-probability cases.
- It involves **radiation exposure** and **contrast administration**, which are generally avoided if a less invasive, equally effective rule-out test is available for low-risk patients.
*Order a lower extremity ultrasound*
- Lower extremity ultrasound is used to diagnose **deep vein thrombosis (DVT)**, which is a common source of PE.
- While DVT can lead to PE, a negative lower extremity ultrasound **does not rule out PE** itself, as the clot may have already embolized or originated from elsewhere.
*Obtain ventilation-perfusion scan*
- A **ventilation-perfusion (V/Q) scan** is an alternative to CT angiography for diagnosing PE, particularly in patients with contraindications to contrast.
- However, it is **less definitive than CTPA** and is typically used when suspicion for PE is moderate or higher, rather than as a primary rule-out test for low-probability patients.
Venous thromboembolism US Medical PG Question 5: A 45-year-old man presents to the emergency department with complaints of right-sided weakness and slurring of speech for 1 hour. There is no history of head trauma, myocardial infarction, recent surgery, gastrointestinal or urinary bleeding. He has hypertension, chronic atrial fibrillation, and a 20 pack-year cigarette smoking history. The medication list includes valsartan and rivaroxaban. The vital signs include: blood pressure 180/92 mm Hg, pulse 144/min and irregular, and temperature 37.2°C (99.0°F). On physical examination, there is a facial asymmetry with a deviation of angle of mouth to the left side on smiling. Muscle strength is reduced in both upper and lower limbs on the right side while on the left side it’s normal. Random blood glucose is 104 mg/dL. A complete blood count is normal. A CT scan of the head is shown in the image. What is the most appropriate next step in the management of this patient?
- A. Heparin
- B. Amiodarone
- C. Metoprolol
- D. Tissue plasminogen activator
- E. Aspirin (Correct Answer)
Venous thromboembolism Explanation: ***Aspirin***
- The patient presents with acute onset **neurological deficits** (right-sided weakness, slurred speech) consistent with an **ischemic stroke** in the setting of **atrial fibrillation**.
- The CT scan shows no evidence of hemorrhage (hypodense or normal appearance), confirming **ischemic stroke**.
- While the patient is on **rivaroxaban**, the question addresses the **within-window acute management**. In the acute setting (within 1 hour of symptom onset), after ruling out hemorrhage on CT, **aspirin 325 mg** is considered as initial antiplatelet therapy for ischemic stroke.
- **Note:** Current guidelines suggest holding rivaroxaban temporarily and avoiding dual therapy (anticoagulation + antiplatelet) due to bleeding risk. However, aspirin remains the safest acute intervention among the choices provided for confirmed ischemic stroke.
*Tissue plasminogen activator (tPA)*
- **tPA** is the preferred thrombolytic for acute ischemic stroke **within 3-4.5 hours** of symptom onset.
- However, it is **absolutely contraindicated** in patients on **direct oral anticoagulants** (like rivaroxaban) due to **dramatically increased risk of intracranial hemorrhage** (up to 10-fold increase).
- Even with normal PT/INR, patients on DOACs cannot receive tPA safely without reversal agents.
*Heparin*
- **Heparin** provides additional anticoagulation on top of rivaroxaban, which would **significantly increase bleeding risk** (both intracranial and systemic).
- Not indicated in acute ischemic stroke management, especially when patient is already therapeutically anticoagulated.
- May be considered in specific scenarios (e.g., crescendo TIAs, arterial dissection) but not first-line here.
*Metoprolol*
- **Metoprolol** is a beta-blocker used for **rate control in atrial fibrillation** (patient has pulse 144/min - rapid ventricular response).
- While rate control is important, **acute blood pressure lowering in ischemic stroke can worsen cerebral perfusion** and extend the infarct.
- Current guidelines recommend **permissive hypertension** in acute stroke (allow BP up to 220/120 unless giving tPA).
- Rate control can be addressed after acute stroke management is initiated.
*Amiodarone*
- **Amiodarone** is an antiarrhythmic used for rhythm control in atrial fibrillation.
- Does **not treat the acute stroke** and is not indicated for emergency management of stroke.
- Rhythm control is not the priority in the acute stroke setting; the focus is on salvaging brain tissue and preventing further ischemia.
Venous thromboembolism US Medical PG Question 6: A mother brings her 6-year-old daughter in to the pediatrician’s clinic for a wellness visit. The mother has a history of von Willebrand’s disease (vWD) and is concerned that her daughter may be affected as well. The mother tells you that she has noticed that her daughter bruises very easily, and her bruises typically are visible for a longer period of time than those of her brother. She denies any personal history of blood clots in her past, but she says that her mother has had to be treated for pulmonary embolism in the recent past. Her birth history is significant for preeclampsia, preterm birth at 32 weeks, a NICU stay of two and a half weeks, and retinopathy of prematurity. She currently eats a diet full of green vegetables, fruits, and french fries. Her vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 106/54 mm Hg; heart rate, 111/min; and respiratory, rate 23/min. On physical examination, her pulses are bounding, complexion is pale, scattered bruises throughout all extremities that are specifically scattered around the knees and elbows. After ordering a coagulation panel, which of the following would one expect to see in the lab panel of a patient with vWD?
- A. Elevated platelet count
- B. Prolonged PT
- C. Normal bleeding time
- D. Decreased factor IX
- E. Prolonged PTT (Correct Answer)
Venous thromboembolism Explanation: ***Prolonged PTT***
- **Von Willebrand factor (vWF)** stabilizes **Factor VIII**, and in vWD, reduced vWF levels lead to lower Factor VIII activity, which is reflected as a **prolonged PTT**.
- The coagulation cascade components associated with PTT (intrinsic and common pathways) are affected due to the impaired function or deficiency of vWF.
*Elevated platelet count*
- **Platelet count** is typically **normal** in vWD, as the disorder primarily affects platelet function and adhesion, not platelet production.
- Thrombocytosis is not characteristic of vWD and would suggest other primary hematologic conditions.
*Prolonged PT*
- The **prothrombin time (PT)** measures the extrinsic and common pathways of coagulation, which are typically **unaffected** in vWD.
- PT prolongation would suggest deficiencies in factors VII, X, V, or prothrombin.
*Normal bleeding time*
- **Bleeding time** is typically **prolonged** in vWD because vWF is crucial for platelet adhesion to the subendothelium and platelet plug formation.
- A normal bleeding time would argue against a platelet function disorder like vWD.
*Decreased factor IX*
- **Factor IX** deficiency is associated with **Hemophilia B**, a separate X-linked coagulopathy, and is not directly affected in vWD.
- While vWD involves coagulation factor deficiencies, the primary factor stabilized by vWF is Factor VIII, not Factor IX.
Venous thromboembolism US Medical PG Question 7: A 74-year-old man presents to the emergency department by paramedics for slurred speech and weakness in the left arm and leg for 1 hour. The patient was playing with his grandson when the symptoms started and his wife immediately called an ambulance. There is no history of head trauma or recent surgery. The patient takes captopril for hypertension. The vital signs include: pulse 110/min, respiratory rate 22/min, and blood pressure 200/105 mm Hg. The physical examination shows that the patient is alert and conscious, but speech is impaired. Muscle strength is 0/5 in the left arm and leg and 5/5 in the right arm and leg. A non-contrast CT of the head shows no evidence of intracranial bleeding. The lab results are as follows:
Serum glucose 90 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 1.3 mg/dL
Blood urea nitrogen 20 mg/dL
Cholesterol, total 240 mg/dL
HDL-cholesterol 38 mg/dL
LDL-cholesterol 100 mg/dL
Triglycerides 190 mg/dL
Hemoglobin (Hb%) 15.3 g/dL
Mean corpuscular volume (MCV) 83 fL
Reticulocyte count 0.8%
Erythrocyte count 5.3 million/mm3
Platelet count 130,000/mm3
Partial thromboplastin time (aPTT) 30 sec
Prothrombin time (PT) 12 sec
Although he is within the time frame for the standard therapy of the most likely condition, the treatment cannot be started because of which of the following contraindications?
- A. A platelet count of 130,000/mm3
- B. Age of 74 years
- C. Cholesterol level of 240 mg/dL
- D. Creatinine level of 1.3 mg/dL
- E. Systolic blood pressure of 200 mm Hg (Correct Answer)
Venous thromboembolism Explanation: ***Systolic blood pressure of 200 mm Hg***
- The patient presents with symptoms highly suggestive of an **acute ischemic stroke**, including **slurred speech** and **left-sided weakness**.
- For patients with acute ischemic stroke who are candidates for **thrombolytic therapy (e.g., alteplase)**, a **systolic blood pressure consistently >185 mm Hg or diastolic >110 mm Hg is a contraindication** due to increased risk of hemorrhagic transformation.
*A platelet count of 130,000/mm3*
- A platelet count of 130,000/mm³ is above the **contraindication threshold for thrombolytic therapy**, which is typically <100,000/mm³.
- Therefore, this platelet count would **not prevent** the initiation of tPA.
*Age of 74 years*
- While older age was once considered a relative contraindication, current guidelines **do not consider age alone (including 74 years old) as an absolute contraindication** for thrombolytic therapy in acute ischemic stroke.
- Eligibility is determined by a comprehensive risk-benefit assessment, not solely by age.
*Cholesterol level of 240 mg/dL*
- An elevated **cholesterol level** is a **risk factor for atherosclerosis** and ischemic stroke, but it is **not a contraindication for acute thrombolytic therapy**.
- It relates to the underlying cause of the stroke rather than the immediate treatment decision.
*Creatinine level of 1.3 mg/dL*
- A **creatinine level of 1.3 mg/dL** indicates **mild renal impairment**, but it is **not a contraindication for thrombolytic therapy**.
- Renal function more significantly impacts the use of certain anticoagulants, but not typically alteplase in the acute setting.
Venous thromboembolism US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Venous thromboembolism Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Venous thromboembolism US Medical PG Question 9: Four days after undergoing a craniotomy and evacuation of a subdural hematoma, a 56-year-old man has severe pain and swelling of his right leg. He has chills and nausea. He has type 2 diabetes mellitus and chronic kidney disease, and was started on hemodialysis 2 years ago. Prior to admission, his medications were insulin, enalapril, atorvastatin, and sevelamer. His temperature is 38.3°C (101°F), pulse is 110/min, and blood pressure is 130/80 mm Hg. Examination shows a swollen, warm, and erythematous right calf. Dorsiflexion of the right foot causes severe pain in the right calf. The peripheral pulses are palpated bilaterally. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 11,800/mm3
Platelet count 230,000/mm3
Serum
Glucose 87 mg/dL
Creatinine 1.9 mg/dL
Which of the following is the most appropriate next step in treatment?
- A. Urokinase therapy
- B. Iliac stenting
- C. Warfarin therapy
- D. Unfractionated heparin therapy (Correct Answer)
- E. Inferior vena cava filter
Venous thromboembolism Explanation: ***Unfractionated heparin therapy***
- The patient presents with classic symptoms of **deep vein thrombosis (DVT)**, including unilateral leg pain, swelling, warmth, erythema, and a positive Homan's sign (pain on dorsiflexion). The recent craniotomy places him at high risk for DVT.
- **Unfractionated heparin is the anticoagulant of choice** for this patient due to TWO critical factors:
1. **Recent craniotomy (4 days ago)**: Requires a rapidly reversible anticoagulant in case of intracranial bleeding; UFH can be reversed with protamine sulfate
2. **Chronic kidney disease on hemodialysis**: Low molecular weight heparin (LMWH) is contraindicated in severe renal failure (CrCl <30 mL/min) as it is renally eliminated and increases bleeding risk. UFH is not renally cleared and can be monitored with aPTT.
*Urokinase therapy*
- **Urokinase is a thrombolytic agent** used to dissolve existing clots, primarily in cases of massive pulmonary embolism or severe DVT with limb-threatening ischemia (phlegmasia cerulea dolens).
- Given the patient's **recent craniotomy and subdural hematoma evacuation**, thrombolytic therapy is **absolutely contraindicated** due to very high risk of intracranial hemorrhage. Recent neurosurgery is a contraindication for at least 2-4 weeks.
*Iliac stenting*
- **Iliac vein stenting** is a procedure typically used to treat chronic **iliac vein compression** (e.g., May-Thurner syndrome) or chronic post-thrombotic obstruction.
- This is an **acute DVT presentation** (4 days post-op) with no indication of chronic iliac vein compression or obstruction. Stenting has no role in acute DVT management.
*Warfarin therapy*
- **Warfarin is an oral anticoagulant** used for long-term DVT treatment but has a **delayed onset of action** (requires 5-7 days to reach therapeutic INR).
- It is **not suitable for acute initial treatment** of DVT, especially in a patient requiring rapid anticoagulation. Warfarin must be overlapped with parenteral anticoagulation (heparin) initially.
- Additionally, warfarin dosing is complex in dialysis patients due to altered vitamin K metabolism.
*Inferior vena cava filter*
- An **IVC filter** is indicated for patients with DVT who have an **absolute contraindication to anticoagulation** (e.g., active bleeding, recent hemorrhagic stroke) or who develop recurrent thromboembolism despite adequate anticoagulation.
- This patient **does not have a contraindication to anticoagulation**. While he had recent neurosurgery, unfractionated heparin is safe to use with careful monitoring and is rapidly reversible if needed.
- IVC filters have significant complications (thrombosis, filter migration, IVC perforation) and should be avoided when anticoagulation is feasible.
Venous thromboembolism US Medical PG Question 10: A 23-year-old woman with no significant past medical history currently on oral contraceptive pills presents to the emergency department with pleuritic chest pain. She states that it started today. Yesterday she had a trip and returned via plane. Her temperature is 98°F (36.7°C), blood pressure is 117/66 mmHg, pulse is 105/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals tachycardia, a normal S1 and S2, and clear breath sounds. The patient’s lower extremities are non-tender and symmetric. Chest pain is not reproducible with position changes or palpation but is worsened with deep breaths. Which of the following is the most appropriate next test for this patient?
- A. D-dimer
- B. Ultrasound of the lower extremities
- C. Ventilation-perfusion scan
- D. CT angiogram (Correct Answer)
- E. Chest radiograph
Venous thromboembolism Explanation: ***CT angiogram***
- This patient has **HIGH probability for pulmonary embolism (PE)** based on **Wells criteria**: oral contraceptive use (hypercoagulable state), recent long-haul flight (immobilization), pleuritic chest pain, and tachycardia (pulse 105/min).
- With a **Wells score ≥4**, the appropriate next step is **definitive imaging with CT pulmonary angiography (CTPA)**, which is the **gold standard** for diagnosing PE.
- **D-dimer should be bypassed** in high-probability cases, as a negative result would not adequately rule out PE, and a positive result (expected in high-probability patients) would require CTPA anyway.
- CTPA provides direct visualization of pulmonary arterial thrombi and can also identify alternative diagnoses.
*D-dimer*
- D-dimer is appropriate for **low to moderate probability PE** (Wells score <4) where a negative result can safely rule out PE and avoid unnecessary imaging.
- In this **high-probability case**, D-dimer is likely to be positive regardless, making it an unnecessary intermediate step that delays definitive diagnosis.
- Using D-dimer in high-probability patients can lead to false reassurance if negative or simply confirms the need for CTPA if positive.
*Ultrasound of the lower extremities*
- Lower extremity ultrasound diagnoses **deep vein thrombosis (DVT)**, not PE directly.
- While finding DVT in a patient with suspected PE would support anticoagulation, **absence of DVT does not rule out PE**, as thrombi may have already embolized.
- This would delay appropriate diagnosis and is not the most direct test for suspected PE.
*Ventilation-perfusion scan*
- V/Q scan is reserved for patients with **contraindications to CT contrast** (severe renal insufficiency, contrast allergy) or pregnant patients where radiation exposure should be minimized.
- This young patient has no mentioned contraindications to contrast-enhanced CT.
- V/Q scanning is less specific than CTPA and often yields indeterminate results.
*Chest radiograph*
- Chest X-ray is often **normal in PE** or shows non-specific findings (Westermark sign, Hampton's hump are rare).
- While it may help exclude alternative diagnoses like pneumothorax or pneumonia, it cannot definitively diagnose or rule out PE.
- In a patient with high clinical suspicion for PE, delaying CTPA to obtain a chest X-ray is not optimal management.
More Venous thromboembolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.