Sickle cell disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sickle cell disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sickle cell disease US Medical PG Question 1: A 7-year-old boy is brought to the emergency department because of high-grade fever and lethargy for 4 days. He has had a severe headache for 3 days and 2 episodes of non-bilious vomiting. He has sickle cell disease. His only medication is hydroxyurea. His mother has refused vaccinations and antibiotics in the past because of their possible side effects. He appears ill. His temperature is 40.1°C (104.2°F), pulse is 131/min, and blood pressure is 92/50 mm Hg. Examination shows nuchal rigidity. Kernig and Brudzinski signs are present. A lumbar puncture is performed. Analysis of the cerebrospinal fluid (CSF) shows a decreased glucose concentration, increased protein concentration, and numerous segmented neutrophils. A Gram stain of the CSF shows gram-negative coccobacilli. This patient is at greatest risk for which of the following complications?
- A. Adrenal insufficiency
- B. Cerebral palsy
- C. Hearing loss (Correct Answer)
- D. Communicating hydrocephalus
- E. Brain abscess
Sickle cell disease Explanation: ***Hearing loss***
- The patient has bacterial meningitis, likely caused by *Haemophilus influenzae* type b given the **gram-negative coccobacilli** and his unvaccinated status.
- **Sensorineural hearing loss is the MOST COMMON long-term neurological sequela of bacterial meningitis**, occurring in 10-30% of survivors, making this the greatest risk for this patient.
- It results from inflammation of the **cochlea and eighth cranial nerve**, which can occur even with appropriate treatment.
- Children with *H. influenzae* meningitis are at particularly high risk for this complication.
*Adrenal insufficiency*
- While adrenal hemorrhage and crisis can occur with overwhelming sepsis (Waterhouse-Friderichsen syndrome), this is **classically associated with meningococcemia**, not *H. influenzae*.
- It is an acute complication of septic shock rather than a common sequela of meningitis itself.
*Cerebral palsy*
- Cerebral palsy requires significant hypoxic-ischemic injury or extensive brain damage during the acute illness.
- While possible with severe meningitis, it is a **much less common** complication compared to hearing loss.
*Communicating hydrocephalus*
- Can occur due to impaired CSF reabsorption at the arachnoid granulations following meningeal inflammation.
- This is a recognized complication but occurs in **fewer than 5-10%** of cases, making it less common than hearing loss.
*Brain abscess*
- Brain abscess represents a focal parenchymal infection and is a **rare complication** of bacterial meningitis.
- It typically occurs when infection spreads from contiguous sites or when meningitis is inadequately treated.
Sickle cell disease US Medical PG Question 2: An 18-year-old African-American woman comes to the physician for the evaluation of worsening fatigue that started 1 year ago. Physical examination shows mild jaundice and splenomegaly. Laboratory studies show:
Hemoglobin 10.4 g/dL
Mean corpuscular hemoglobin concentration 43% Hb/cell
Platelet count 220,000/mm3
Reticulocyte count 7%
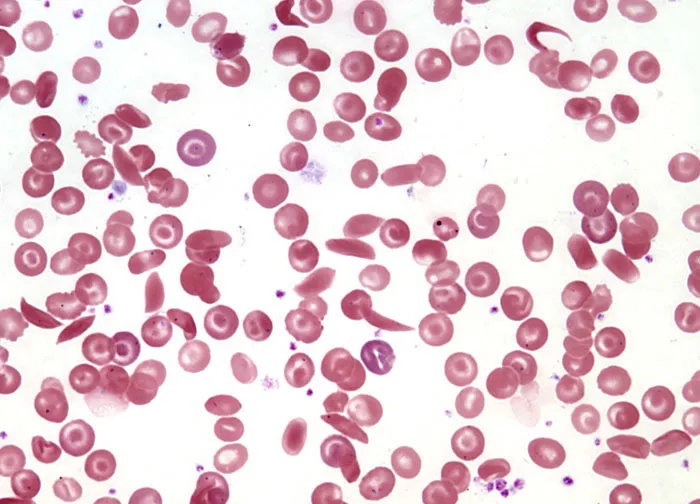
A peripheral blood smear shows target cells and erythrocytes with hemoglobin crystals. Which of the following is the most likely underlying cause of this patient's findings?
- A. Acquired mutation of membrane-bound glycosylphosphatidylinositol anchor
- B. Decreased conversion of oxidized glutathione into its reduced form
- C. Replacement of glutamate by valine in beta-globin chain
- D. Replacement of glutamate by lysine in beta-globin chain (Correct Answer)
- E. Reduced production of beta-globin due to a mutation in the HbB gene
Sickle cell disease Explanation: ***Replacement of glutamate by lysine in beta-globin chain***
- The combination of **mild jaundice**, **splenomegaly**, **anemia**, **elevated reticulocyte count**, and the presence of **target cells** and **hemoglobin C crystals** on peripheral smear is characteristic of **Hemoglobin C disease**.
- **Hemoglobin C** results from the **replacement of glutamate by lysine at position 6 of the beta-globin chain**, leading to abnormal hemoglobin and erythrocyte morphology.
*Acquired mutation of membrane-bound glycosylphosphatidylinositol anchor*
- This describes **Paroxysmal Nocturnal Hemoglobinuria (PNH)**, which is characterized by **hemolytic anemia**, **thrombosis**, and **bone marrow failure**.
- While it causes hemolytic anemia, the peripheral smear findings of **target cells** and **hemoglobin crystals** are not typical for PNH as seen in this patient.
*Decreased conversion of oxidized glutathione into its reduced form*
- This mechanism is characteristic of **Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency**, a cause of **hemolytic anemia**.
- G6PD deficiency typically presents with episodic hemolysis triggered by **oxidative stress**, and the characteristic peripheral smear findings are **Heinz bodies** and **bite cells**, not hemoglobin crystals.
*Replacement of glutamate by valine in beta-globin chain*
- This mutation describes **Sickle Cell Anemia**, which also causes hemolytic anemia and splenomegaly.
- While it leads to **sickle cells** on peripheral smear, **hemoglobin C crystals** and **target cells** are not the primary features; sickle cells and Howell-Jolly bodies would be expected.
*Reduced production of beta-globin due to a mutation in the HbB gene*
- This describes **Beta-thalassemia**, a group of disorders characterized by **reduced or absent beta-globin chain synthesis**.
- Beta-thalassemia typically presents with **microcytic hypochromic anemia** and **target cells**, but the presence of **hemoglobin C crystals** is not a feature.
Sickle cell disease US Medical PG Question 3: A clinical trial is being run with patients that have a genetic condition characterized by abnormal hemoglobin that can undergo polymerization when exposed to hypoxia, acidosis, or dehydration. This process of polymerization is responsible for the distortion of the red blood cell (RBC) that acquires a crescent shape and the hemolysis of RBCs. Researchers are studying the mechanisms of the complications commonly observed in these patients such as stroke, aplastic crisis, and auto-splenectomy. What kind of mutation leads to the development of the disease?
- A. Silent mutation
- B. Splice site
- C. Missense mutation (Correct Answer)
- D. Nonsense mutation
- E. Frameshift mutation
Sickle cell disease Explanation: ***Missense mutation***
- A missense mutation results in a **single nucleotide substitution** that changes the codon to code for a different amino acid, altering the protein.
- In **sickle cell disease**, a missense mutation in the beta-globin gene (GAG to GTG) leads to the substitution of **glutamic acid for valine**, causing abnormal hemoglobin (HbS) that polymerizes under deoxygenated conditions.
*Silent mutation*
- A silent mutation is a **point mutation** that results in a new codon that still codes for the **same amino acid**, meaning there is no change in the protein sequence.
- Therefore, it would not lead to an **abnormal hemoglobin** protein or the described disease phenotype.
*Splice site*
- A splice site mutation occurs at the **splice junctions** of introns and exons, leading to errors in mRNA processing.
- This can result in **incorrect protein synthesis** due to exon skipping or intron retention, but it typically does not cause the specific amino acid substitution seen in sickle cell disease.
*Nonsense mutation*
- A nonsense mutation is a point mutation that results in a **premature stop codon**, leading to a **truncated, non-functional protein**.
- While this can cause severe disease, it would typically lead to a complete absence or severe deficiency of functional hemoglobin rather than a structurally altered hemoglobin like HbS.
*Frameshift mutation*
- A frameshift mutation involves the **insertion or deletion of nucleotides** (not in multiples of three), which shifts the reading frame of the mRNA.
- This typically leads to a completely **altered amino acid sequence** downstream of the mutation and usually results in a premature stop codon, leading to a non-functional protein rather than a specific single amino acid substitution.
Sickle cell disease US Medical PG Question 4: An 8-year-old African American girl is brought to the clinic by her mother for her regular blood exchange. They come in every 2–3 months for the procedure. The child is in good health with no symptoms. Her last trip to the emergency department was 6 months ago due to bone pain. She was treated with morphine and oxygen and a blood transfusion. She takes hydroxyurea and folic acid daily. She has an uncle that also has to get blood exchanges. Today, her heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature is 37.0°C (98.6°F). She calmly waits for the machine to be set up and catheters inserted into both of her arms. She watches a movie as her blood is slowly replaced with 6 L of red blood cells. Based on this history, which of the following mechanisms most likely explains this patient's condition?
- A. Nonsense mutation
- B. Amino acid substitution (Correct Answer)
- C. Enzyme deficiency
- D. Amino acid deletion
- E. Trinucleotide repeat
Sickle cell disease Explanation: ***Amino acid substitution***
- This patient's symptoms (bone pain requiring emergency treatment, need for chronic exchange transfusions, hydroxyurea therapy, African American ethnicity, family history) are characteristic of **sickle cell disease**
- Sickle cell disease is caused by a **single point mutation** (GAG → GTG) in the beta-globin gene, resulting in substitution of **glutamic acid with valine at position 6** of the beta-globin chain
- This amino acid substitution causes hemoglobin to polymerize under low oxygen conditions, leading to **sickling of red blood cells** and vaso-occlusive crises
*Nonsense mutation*
- A nonsense mutation creates a **premature stop codon**, resulting in a **truncated, nonfunctional protein**
- This mechanism causes conditions like **beta-thalassemia major** (some cases), but is not the mechanism of sickle cell disease
- Sickle cell involves a missense mutation (amino acid substitution), not a nonsense mutation
*Enzyme deficiency*
- Enzyme deficiencies such as **glucose-6-phosphate dehydrogenase (G6PD) deficiency** or **pyruvate kinase deficiency** can cause hemolytic anemias
- However, these typically present with episodic hemolysis triggered by oxidative stress, not chronic vaso-occlusive crises requiring regular exchange transfusions
- The mechanism in sickle cell disease is a **structural hemoglobin defect**, not an enzyme deficiency
*Amino acid deletion*
- An amino acid deletion involves **removal of one or more amino acids** from the protein sequence
- This mechanism causes conditions like **cystic fibrosis** (ΔF508 deletion in CFTR protein)
- Sickle cell disease involves **substitution**, not deletion of an amino acid
*Trinucleotide repeat*
- Trinucleotide repeat disorders involve **expansion of a three-nucleotide sequence** within a gene, showing anticipation across generations
- Examples include **Huntington disease (CAG repeats)**, **myotonic dystrophy (CTG repeats)**, and **fragile X syndrome (CGG repeats)**
- These affect neurological or muscular function and are unrelated to hemoglobinopathies
Sickle cell disease US Medical PG Question 5: A 15-year-old boy is brought to the physician by his father because he has been waking up frequently during the night to urinate. Apart from occasional headaches, he has no other complaints. His family recently emigrated from Tanzania and his medical history is unknown. His father was diagnosed with sickle cell disease at the age of 5. Physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 14.5 g/dL
Hematocrit 44%
MCV 90 fL
Reticulocytes 1.5%
A hemoglobin electrophoresis shows:
HbA 55%
HbS 43%
HbF 1%
This patient is at greatest risk for which of the following conditions?
- A. Avascular osteonecrosis
- B. Renal papillary necrosis (Correct Answer)
- C. Clear cell renal carcinoma
- D. Functional asplenia
- E. Ischemic stroke
Sickle cell disease Explanation: ***Renal papillary necrosis***
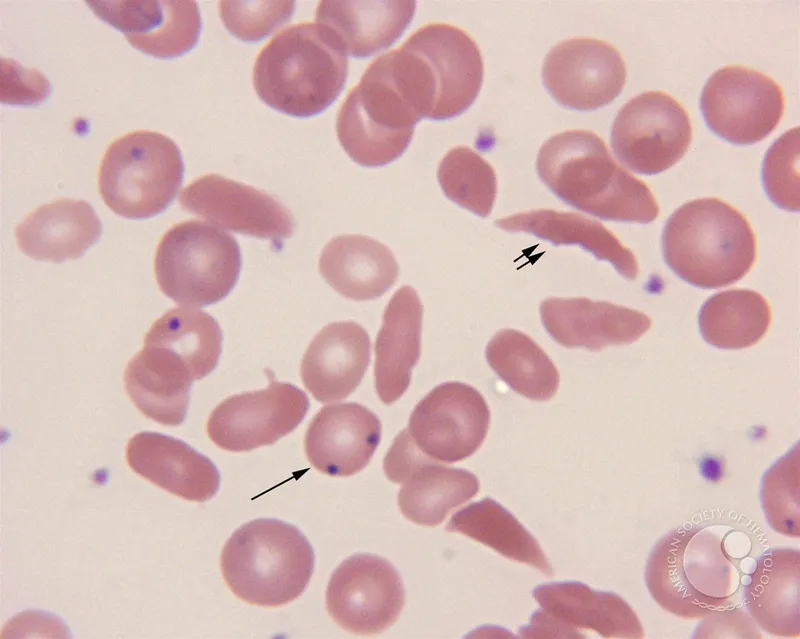
- The patient has **sickle cell trait (HbAS)**, evidenced by **55% HbA** and **43% HbS**. Individuals with sickle cell trait are at increased risk for **renal papillary necrosis** due to vaso-occlusive events in the renal medulla, exacerbated by the hypoxic, hyperosmolar, and acidic environment.
- Clinical manifestations of renal papillary necrosis include **hematuria**, **flank pain**, and **polyuria/nocturia**, which aligns with the patient's presenting symptom of frequent nighttime urination.
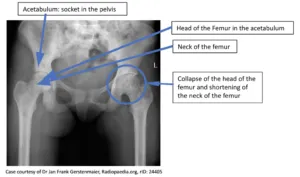
*Avascular osteonecrosis*
- While individuals with **sickle cell disease (HbSS)** are at high risk for **avascular osteonecrosis** due to bone infarction, it is *less common* in those with sickle cell trait.
- The patient's hemoglobin electrophoresis results (HbA 55%, HbS 43%) confirm **sickle cell trait**, not sickle cell disease.
*Clear cell renal carcinoma*
- **Clear cell renal carcinoma** is not directly associated with sickle cell trait.
- While other renal malignancies like **renal medullary carcinoma** can occur in sickle cell trait patients, clear cell renal carcinoma typically presents later in life and is not the most likely complication given the patient's symptoms and genetic profile.
*Functional asplenia*
- **Functional asplenia** is a common and serious complication of **sickle cell disease (HbSS)**, leading to increased susceptibility to encapsulated bacterial infections.
- It is *not typically seen* nor is it a major risk in individuals with **sickle cell trait**.
*Ischemic stroke*
- **Ischemic stroke** is a significant complication in patients with **sickle cell disease (HbSS)** due to chronic hemolysis and vaso-occlusion.
- While there might be a *slightly increased risk* in sickle cell trait compared to the general population, it is *not as pronounced* as in sickle cell disease, and the presenting symptoms do not suggest an acute stroke.
Sickle cell disease US Medical PG Question 6: An 8-year-old African-American boy is brought into the emergency department by his mother due to intense abdominal pain and pain in his thighs. The mother states that she also suffers from the same disease and that the boy has been previously admitted for episodes such as this. On exam, the boy is in 10/10 pain. His vitals are HR 110, BP 100/55, T 100.2F, RR 20. His CBC is significant for a hemoglobin of 9.5 and a white blood cell count of 13,000. His mother asks if there is anything that can help her child in the long-term. Which of the following can decrease the frequency and severity of these episodes?
- A. Hydroxyurea (Correct Answer)
- B. Opiates
- C. Exchange transfusion
- D. Normal saline
- E. Oxygen
Sickle cell disease Explanation: ***Hydroxyurea***
- **Hydroxyurea** increases the production of **fetal hemoglobin (HbF)**, which reduces the sickling of red blood cells and prevents vaso-occlusive crises
- By reducing sickling, it decreases the frequency and severity of pain crises, acute chest syndrome, and the need for hospitalizations in patients with sickle cell disease
- This is the **only FDA-approved disease-modifying therapy** for sickle cell disease that addresses the underlying pathophysiology
*Opiates*
- **Opiates** are used for **pain management** during acute sickle cell crises but do not address the underlying pathology or prevent future episodes
- While essential for symptom relief during vaso-occlusive crises, they do not decrease the **frequency or severity** of future episodes
*Exchange transfusion*
- **Exchange transfusion** is an acute treatment for severe complications of sickle cell disease, such as **acute chest syndrome** or **stroke**, by rapidly reducing the percentage of sickled cells
- It is not a long-term preventative measure to decrease crisis frequency or severity and carries risks like **alloimmunization** and iron overload
*Normal saline*
- **Normal saline** is used for **hydration** during sickle cell crises to improve blood flow and reduce sickling, but it is a supportive measure for acute episodes only
- It does not modify the disease course or prevent future crises, making its benefit primarily symptomatic during an acute event
*Oxygen*
- **Oxygen** therapy is indicated in sickle cell crises when the patient is **hypoxic**, as hypoxia can trigger or worsen sickling
- It is an acute supportive treatment and does not prevent the underlying pathophysiology or reduce the frequency of future crises
Sickle cell disease US Medical PG Question 7: A 13-year-old African American boy with sickle cell disease is brought to the emergency department with complaints of abdominal pain over the last 24 hours. The pain is situated in the right upper quadrant and is sharp in nature with a score of 8/10 and radiates to tip of the right scapula. He also complains of anorexia and nausea over the past 2 days. He has been admitted into the hospital several times for pain episodes involving his legs, hands, thighs, lower back, and abdomen. His last hospital admission was 4 months ago for acute chest pain, and he was treated with antibiotics, analgesics, and intravenous fluid. He takes hydroxyurea with occasional red blood cell exchange. Both of his parents are in good health. Temperature is 38°C (100.4°F), blood pressure is 133/88 mm Hg, pulse is 102/min, respiratory rate is 20/min, and BMI is 18 kg/m2. On examination, he is in pain with a tender abdomen with painful inspiration. Soft palpation of the right upper quadrant causes the patient to cry out in pain.
Laboratory test
Complete blood count
Hemoglobin 8.5 g/dL
MCV 82 fl
Leukocytes 13,500/mm3
Platelets 145,000/mm3
Basic metabolic panel
Serum Na+ 135 mEq/L
Serum K+ 3.9 mEq/L
Serum Cl- 101 mEq/L
Serum HCO3- 23 mEq/L
Liver function test
Serum bilirubin 2.8 mg/dL
Direct bilirubin 0.8 mg/dL
AST
30 U/L
ALT 35 U/L
Serum haptoglobin 23 mg/dL (41–165 mg/dL)
Ultrasonography of abdomen shows the following image. What is the pathogenesis of this ultrasound finding?
- A. Increased cholesterol secretion
- B. Chronic hemolysis (Correct Answer)
- C. Impaired gallbladder emptying
- D. Bacterial infection
- E. Decreased bile salt absorption
Sickle cell disease Explanation: ***Chronic hemolysis***
- The patient has **sickle cell disease**, which is characterized by **chronic hemolysis**, leading to increased bilirubin production.
- This increased **bilirubin** is excreted into the bile, predisposing to the formation of **pigment gallstones** (seen on ultrasound as echogenic foci with posterior shadowing, consistent with gallstones in the gallbladder).
*Increased cholesterol secretion*
- This is primarily associated with the formation of **cholesterol gallstones**, which are less common in sickle cell disease.
- While cholesterol secretion can contribute to gallstone formation, the underlying pathophysiology in sickle cell disease points more directly to bilirubin overload.
*Impaired gallbladder emptying*
- Impaired gallbladder emptying, or **gallbladder stasis**, can lead to the formation of gallstones and biliary sludge.
- However, it is not the primary mechanism for gallstone formation in the context of chronic hemolysis in sickle cell disease.
*Bacterial infection*
- While **bacterial infections** can lead to the formation of **pigment gallstones** containing bacterial biofilms, they are generally less common than the pigment stones formed due to chronic hemolysis.
- The patient's presentation with chronic sickle cell disease makes chronic hemolysis a more direct and primary cause.
*Decreased bile salt absorption*
- **Decreased bile salt absorption** can lead to a *reduced bile salt pool*, which in turn can increase the risk of cholesterol gallstone formation.
- It is not the main pathogenic mechanism for the formation of pigment gallstones seen in sickle cell disease.
Sickle cell disease US Medical PG Question 8: A 24-year-old African American male with sickle cell disease has been followed by a hematologist since infancy. Two years ago, he was started on hydroxyurea for frequent pain crises but has not achieved good control. The addition of a Gardos channel blocking agent is being considered. What is the mechanism of action of this class of medications?
- A. Increases water diffusion by increasing activity of aquaporin-1 receptors
- B. Increases production of hemoglobin F
- C. Encourages alkalinization of the blood by facilitating H+/K+ antiporter activity
- D. Prevents dehydration of RBCs by inhibiting Ca2+ efflux
- E. Prevents RBC dehydration by inhibiting K+ efflux (Correct Answer)
Sickle cell disease Explanation: ***Prevents RBC dehydration by inhibiting K+ efflux***
- Gardos channel blockers, like **voxelotor**, inhibit the **Gardos channel (KCCN4)** in red blood cells, which is a calcium-activated potassium channel.
- By blocking **K+ efflu**x, these agents prevent the **dehydration** and sickling of red blood cells, thereby reducing the frequency of vaso-occlusive crises in sickle cell disease.
*Increases water diffusion by increasing activity of aquaporin-1 receptors*
- **Aquaporins** are water channels, but their modulation is not the primary mechanism of action for Gardos channel blockers in **sickle cell disease**.
- The focus of Gardos channel blockers is on maintaining **RBC volume** by preventing K+ loss, not by directly increasing water diffusion across aquaporins.
*Increases production of hemoglobin F*
- **Hydroxyurea** is the medication that primarily works by increasing the production of **fetal hemoglobin (HbF)**, which is known to inhibit HbS polymerization.
- Gardos channel blockers operate through a distinct mechanism, focusing on **red blood cell hydration**, rather than HbF induction.
*Encourages alkalinization of the blood by facilitating H+/K+ antiporter activity*
- The **H+/K+ antiporter** is more relevant in gastric acid secretion and kidney physiology, not as a primary target for preventing red blood cell sickling in sickle cell disease.
- Gardos channel blockers specifically target potassium channels in RBCs to prevent **dehydration** and sickling, unconnected to H+/K+ antiporter activity.
*Prevents dehydration of RBCs by inhibiting Ca2+ efflux*
- While Gardos channels are **calcium-activated**, the Gardos channel blockers work by inhibiting the **potassium efflux** *through* the channel, rather than directly inhibiting calcium efflux.
- The primary problem in sickle cell dehydration is the loss of **potassium**, which draws water out of the cell, leading to sickling.
Sickle cell disease US Medical PG Question 9: A mother brings her son to the pediatrician because she is concerned about his health. She states that throughout her child's life he has demonstrated aggressive behavior. However, he has recently begun biting himself causing injury and bleeding. The patient has a past medical history of mental retardation and episodes of severe joint pain. His temperature is 99.5°F (37.5°C), blood pressure is 87/48 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals a child attempting to bite his arms. Which of the following is the inheritance pattern of the disease with which this patient presents?
- A. X-linked dominant
- B. Autosomal dominant
- C. Autosomal recessive
- D. X-linked recessive (Correct Answer)
- E. Maternal
Sickle cell disease Explanation: ***X-linked recessive***
- This patient's presentation of **self-mutilation**, **mental retardation**, and **aggressive behavior** is highly suggestive of **Lesch-Nyhan syndrome**.
- Lesch-Nyhan syndrome is an **X-linked recessive disorder** caused by a defect in the gene for **hypoxanthine-guanine phosphoribosyltransferase (HGPRT)**, leading to a build-up of uric acid.
*X-linked dominant*
- X-linked dominant disorders affect both males and females, though males are often more severely affected or may have more prominent symptoms.
- Affected fathers transmit the trait to all their daughters but no sons, which is not characteristic of Lesch-Nyhan syndrome.
*Autosomal dominant*
- Autosomal dominant disorders are inherited equally by males and females, and an affected individual has a 50% chance of passing the condition to each child.
- This inheritance pattern does not fit the typical presentation of Lesch-Nyhan syndrome, which primarily affects males.
*Autosomal recessive*
- Autosomal recessive disorders typically require two copies of the mutated gene (one from each parent) for the disease to manifest, affecting males and females equally.
- While some metabolic disorders are autosomal recessive, Lesch-Nyhan syndrome's sex-linked pattern of inheritance rules out this option.
*Maternal*
- Maternal inheritance refers to conditions passed down through **mitochondrial DNA**, affecting all children of an affected mother regardless of sex.
- Affected fathers do not pass mitochondrial conditions to any of their children, since sperm contribute minimal mitochondria.
- Lesch-Nyhan syndrome is associated with a nuclear gene on the X chromosome, not mitochondrial DNA, making maternal inheritance incorrect.
Sickle cell disease US Medical PG Question 10: An investigator is studying the outcomes of a malaria outbreak in an endemic region of Africa. 500 men and 500 women with known malaria exposure are selected to participate in the study. Participants with G6PD deficiency are excluded from the study. The clinical records of the study subjects are reviewed and their peripheral blood smears are evaluated for the presence of Plasmodium trophozoites. Results show that 9% of the exposed population does not have clinical or laboratory evidence of malaria infection. Which of the following best explains the absence of infection seen in this subset of participants?
- A. Translocation of c-myc gene
- B. Glutamic acid substitution in the β-globin chain (Correct Answer)
- C. Inherited mutation affecting ribosome synthesis
- D. Inherited defect in erythrocyte membrane ankyrin protein
- E. Defective X-linked ALA synthase gene
Sickle cell disease Explanation: ***Glutamic acid substitution in the β-globin chain***
- This describes **sickle cell trait (heterozygous HbS)**, which confers significant protection against severe malaria, explaining the absence of infection despite exposure.
- Individuals with sickle cell trait have **abnormally shaped red blood cells** under low oxygen conditions, which are less hospitable for **Plasmodium falciparum** growth and are more rapidly cleared by the spleen.
*Translocation of c-myc gene*
- A **t(8;14) translocation of the c-myc gene** is characteristic of **Burkitt lymphoma**, a B-cell malignancy, and has no protective effect against malaria.
- This genetic alteration leads to overexpression of **c-myc**, a proto-oncogene, contributing to uncontrolled cell growth.
*Inherited mutation affecting ribosome synthesis*
- Defects in **ribosome synthesis** can lead to various **ribosomopathies**, affecting cell proliferation and function, but they are not known to provide protection against malaria.
- Such mutations often result in syndromes with **developmental abnormalities** or **bone marrow failure**.
*Inherited defect in erythrocyte membrane ankyrin protein*
- Defects in **ankyrin protein** are associated with **hereditary spherocytosis**, causing fragile, spherical red blood cells that are prematurely destroyed.
- While hereditary spherocytosis can reduce malaria severity, its role in preventing initial infection is less pronounced, and the question refers to absence of infection.
*Defective X-linked ALA synthase gene*
- A defective **X-linked ALA synthase gene** (ALAS2) is associated with **X-linked sideroblastic anemia**, causing impaired heme synthesis.
- This condition is characterized by **microcytic, hypochromic anemia** and iron overload in erythroid precursors, with no known protective effect against malaria.
More Sickle cell disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.