Platelet disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Platelet disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Platelet disorders US Medical PG Question 1: A previously healthy 17-year-old boy is brought to the emergency department by his mother for further evaluation after elective removal of his wisdom teeth. During the procedure, the patient had persistent bleeding from the teeth's surrounding gums. Multiple gauze packs were applied with minimal effect. The patient has a history of easy bruising. The mother says her brother had similar problems when his wisdom teeth were removed, and that he also has a history of easy bruising and joint swelling. The patient takes no medications. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 108/74 mm Hg. Laboratory studies show:
Hematocrit 35%
Leukocyte count 8,500/mm3
Platelet count 160,000/mm3
Prothrombin time 15 sec
Partial thromboplastin time 60 sec
Bleeding time 6 min
Fibrin split products negative
Serum
Urea nitrogen 20 mg/dL
Creatinine 1.0 mg/dL
Bilirubin
Total 1.0 mg/dL
Direct 0.5 mg/dL
Lactate dehydrogenase 90 U/L
Peripheral blood smear shows normal-sized platelets. Which of the following is the most likely diagnosis?
- A. Hemophilia
- B. Bernard-Soulier syndrome
- C. Glanzmann thrombasthenia
- D. Von Willebrand disease (Correct Answer)
- E. Immune thrombocytopenia
Platelet disorders Explanation: ***Von Willebrand disease***
- This patient presents with a **history of easy bruising** and **persistent bleeding after a surgical procedure**, along with a **prolonged bleeding time** and **prolonged PTT**. The family history of similar bleeding issues and joint swelling (which can represent hemarthroses) in his maternal uncle is also highly suggestive of an inherited bleeding disorder. These findings, particularly the prolonged bleeding time with normal platelet count and the prolonged PTT (due to Factor VIII deficiency), are classic for **von Willebrand disease (vWD)**.
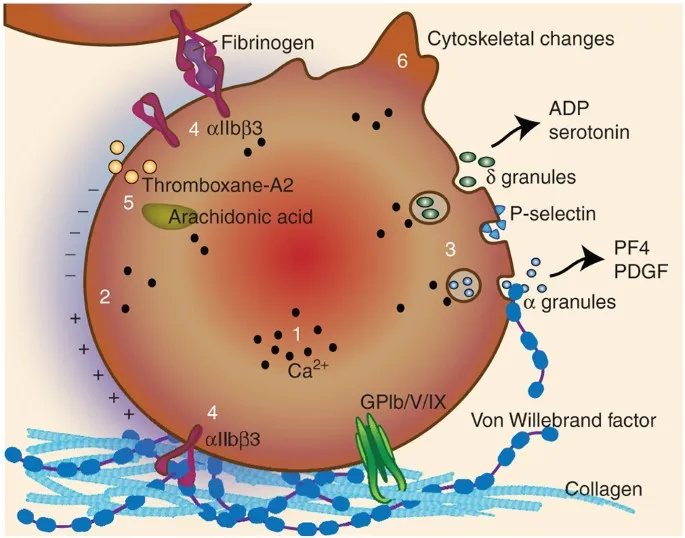
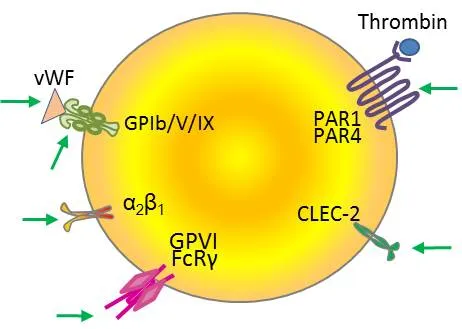
- Von Willebrand disease is the **most common inherited bleeding disorder**, characterized by a deficiency or dysfunction of **von Willebrand factor (vWF)**. vWF plays a dual role in hemostasis: it mediates platelet adhesion to the subendothelium (reflected by prolonged bleeding time) and also chaperones and protects **Factor VIII** from degradation, leading to a mild to moderate deficiency of Factor VIII (reflected by prolonged PTT).
*Hemophilia*
- Hemophilia A (Factor VIII deficiency) or Hemophilia B (Factor IX deficiency) would present with a **prolonged PTT** but a **normal bleeding time** and **platelet count**.
- While the patient has a prolonged PTT and family history of joint swelling (consistent with hemarthroses seen in hemophilia), his **prolonged bleeding time** is inconsistent with hemophilia alone.
*Bernard-Soulier syndrome*
- This syndrome is characterized by a defect in **platelet adhesion** due to a deficiency of **glycoprotein Ib (GP Ib)**, leading to **macrothrombocytopenia** (large platelets and reduced platelet count) and a **prolonged bleeding time**.
- The patient has a **normal platelet count** and **normal-sized platelets** on peripheral smear, which makes Bernard-Soulier syndrome less likely.
*Glanzmann thrombasthenia*
- This is a disorder of **platelet aggregation** due to a deficiency in **glycoprotein IIb/IIIa (GP IIb/IIIa)**, resulting in a **prolonged bleeding time** despite a normal platelet count and morphology.
- However, Glanzmann thrombasthenia typically presents with a **normal PTT**, whereas this patient has a **prolonged PTT**, making it less likely.
*Immune thrombocytopenia*
- **Immune thrombocytopenia (ITP)** is characterized by an **isolated low platelet count** (thrombocytopenia) and a **prolonged bleeding time**, with other coagulation parameters (PT, PTT) being normal.
- The patient has a **normal platelet count** (160,000/mm3) and a **prolonged PTT**, which is inconsistent with ITP.
Platelet disorders US Medical PG Question 2: A 34-year-old, previously healthy woman is admitted to the hospital with abdominal pain and bloody diarrhea. She reports consuming undercooked beef a day before the onset of her symptoms. Her medical history is unremarkable. Vital signs include: blood pressure 100/70 mm Hg, pulse rate 70/min, respiratory rate 16/min, and temperature 36.6℃ (97.9℉). Physical examination shows paleness, face and leg edema, and abdominal tenderness in the lower right quadrant. Laboratory investigation shows the following findings:
Erythrocytes 3 x 106/mm3
Hemoglobin 9.4 g/dL
Hematocrit 0.45 (45%)
Corrected reticulocyte count 5.5%
Platelet count 18,000/mm3
Leukocytes 11,750/mm3
Total bilirubin 2.33 mg/dL (39.8 µmol/L)
Direct bilirubin 0.2 mg/dL (3.4 µmol/L)
Serum creatinine 4.5 mg/dL (397.8 µmol/L)
Blood urea nitrogen 35.4 mg/dL (12.6 mmol/L)
E. coli O157: H7 was identified in the patient’s stool. Which toxin is likely responsible for her symptoms?
- A. Erythrogenic toxin
- B. Shiga toxin (Correct Answer)
- C. Enterotoxin type B
- D. α-hemolysin
- E. Exotoxin A
Platelet disorders Explanation: ***Shiga toxin***
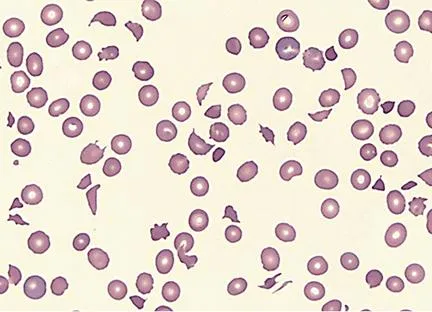
- The clinical presentation of **abdominal pain, bloody diarrhea, thrombocytopenia, microangiopathic hemolytic anemia** (indicated by low hemoglobin, elevated reticulocyte count, and elevated indirect bilirubin), and **acute kidney injury** (elevated creatinine and BUN with edema) strongly suggests **hemolytic uremic syndrome (HUS)**.
- ***E. coli* O157:H7** is a common cause of HUS, and it produces **Shiga toxins** (Stx1 and Stx2, also known as verotoxins), which cause endothelial damage leading to the characteristic features of HUS.
- Shiga toxins inhibit protein synthesis by cleaving ribosomal RNA, resulting in **endothelial cell damage, thrombotic microangiopathy**, and the classic triad of HUS.
*Erythrogenic toxin*
- This toxin is produced by **_Streptococcus pyogenes_** and is responsible for the rash seen in **scarlet fever**.
- It is not associated with **_E. coli_ O157:H7 infection** or the development of HUS.
*Enterotoxin type B*
- **Enterotoxin type B** is typically associated with **_Staphylococcus aureus_** and acts as a **superantigen** causing food poisoning with symptoms like vomiting and diarrhea.
- It does not cause HUS or the specific hematological and renal manifestations described in the patient.
*α-hemolysin*
- **Alpha-hemolysin** is a pore-forming cytolytic toxin produced by various bacteria, including **_Staphylococcus aureus_** and **_E. coli_**.
- While some *E. coli* strains produce alpha-hemolysin, it is not the primary toxin responsible for HUS caused by **_E. coli_ O157:H7**.
*Exotoxin A*
- **Exotoxin A** is produced by **_Pseudomonas aeruginosa_** and inhibits protein synthesis by ADP-ribosylation of elongation factor-2 (EF-2).
- It is not produced by *E. coli* O157:H7 and is not associated with HUS or the clinical presentation in this patient.
Platelet disorders US Medical PG Question 3: A 66-year-old woman presents to the emergency department complaining of palpitations. She says that she has been experiencing palpitations and lightheadedness for the past 6 months, but before this morning the episodes usually resolved on their own. The patient's medical history is significant for a transient ischemia attack 2 months ago, hypertension, and diabetes. She takes aspirin, metformin, and lisinopril. She states her grandfather died of a stroke, and her mom has a "blood disorder." An electrocardiogram is obtained that shows an irregularly irregular rhythm with rapid ventricular response, consistent with atrial fibrillation. She is given intravenous metoprolol, which resolves her symptoms. In addition to starting a beta-blocker for long-term management, the patient meets criteria for anticoagulation. Both unfractionated heparin and warfarin are started. Five days later, the patient begins complaining of pain and swelling of her left lower extremity. A Doppler ultrasound reveals thrombosis in her left popliteal and tibial veins. A complete blood count is obtained that shows a decrease in platelet count from 245,000/mm^3 to 90,000/mm^3. Coagulation studies are shown below:
Prothrombin time (PT): 15 seconds
Partial thromboplastin time (PTT): 37 seconds
Bleeding time: 14 minutes
Which of the following is the most likely diagnosis?
- A. Thrombotic thrombocytopenic purpura
- B. Type I heparin-induced thrombocytopenia
- C. Warfarin toxicity
- D. Idiopathic thrombocytopenia purpura
- E. Type II heparin-induced thrombocytopenia (Correct Answer)
Platelet disorders Explanation: ***Type II heparin-induced thrombocytopenia***
- This diagnosis is strongly supported by the patient's **recent heparin exposure**, a significant **drop in platelet count** (from 245,000 to 90,000/mm^3, a >50% reduction), and new onset **thrombosis** (popliteal and tibial vein thrombosis).
- Type II HIT involves antibody formation against **heparin-platelet factor 4 (PF4) complexes**, leading to platelet activation, aggregation, and paradoxical thrombosis, often occurring 5-10 days after heparin initiation.
*Thrombotic thrombocytopenic purpura*
- While TTP involves microangiopathic hemolytic anemia, thrombocytopenia, and organ damage including neurological symptoms, the prompt onset of thrombosis after heparin strongly points away from TTP and towards **heparin-related complications**.
- This patient’s symptoms are primarily thrombotic, and typical TTP findings like **schistocytes on blood smear** and **severe ADAMTS13 deficiency** are not mentioned.
*Type I heparin-induced thrombocytopenia*
- Type I HIT is characterized by a **mild, non-immune-mediated platelet drop** (usually not below 100,000/mm^3) that occurs within the first 2 days of heparin therapy.
- It is **rarely associated with thrombosis**, which makes it an unlikely diagnosis given the severe platelet drop and new thromboses.
*Warfarin toxicity*
- Warfarin toxicity typically causes **bleeding complications** due to over-anticoagulation, rather than thrombosis, and is characterized by a **prolonged PT/INR**.
- Although the patient's bleeding time is prolonged, the thrombotic events and significant platelet drop point away from warfarin toxicity as the primary diagnosis.
*Idiopathic thrombocytopenia purpura*
- ITP is an autoimmune disorder causing **isolated thrombocytopenia** (often severe) and **bleeding**, but it is generally *not* associated with paradoxical thrombosis.
- The temporal relationship with heparin exposure and the thrombotic events are inconsistent with a primary diagnosis of unprovoked ITP.
Platelet disorders US Medical PG Question 4: A 3-year-old girl is brought to her pediatrician because of a nosebleed that will not stop. Her parents say that she started having a nosebleed about 1 hour prior to presentation. Since then they have not been able to stop the bleeding. Her past medical history is remarkable for asthma, and she has a cousin who has been diagnosed with hemophilia. Physical exam reveals diffuse petechiae and purpura. A panel of bleeding tests are obtained with the following results:
Bleeding time: 11 minutes
Prothrombin time: 14 seconds
Partial thromboplastin time: 32 seconds
Platelet count: 195,000/mm^3
Peripheral blood smear shows normal cell morphology. Which of the following characteristics is most likely true about this patient?
- A. Mutation in glycoprotein IIb/IIIa (Correct Answer)
- B. Mutation in glycoprotein Ib
- C. Production of anti platelet antibodies
- D. Production of antibodies against ADAMTS13
- E. Decreased levels of von Willebrand factor
Platelet disorders Explanation: ***Mutation in glycoprotein IIb/IIIa***
- The patient's symptoms (nosebleed, petechiae, purpura) and laboratory findings (prolonged **bleeding time**, normal platelet count, normal PT/PTT) are characteristic of **Glanzmann's thrombasthenia**, which is caused by a qualitative defect in **glycoprotein IIb/IIIa**.
- **Glycoprotein IIb/IIIa** is crucial for platelet aggregation, and a mutation in this protein prevents platelets from forming a stable clot.
*Mutation in glycoprotein Ib*
- A mutation in **glycoprotein Ib** leads to **Bernard-Soulier syndrome**, characterized by prolonged bleeding time, normal platelet count, and **abnormally large platelets** on peripheral smear, which are not seen here.
- Glycoprotein Ib is involved in platelet adhesion to von Willebrand factor, not aggregation.
*Production of anti platelet antibodies*
- This describes **Immune Thrombocytopenic Purpura (ITP)**, which would typically present with a **low platelet count**, not a normal count as seen in this patient.
- While ITP can cause petechiae and bleeding, the normal platelet count rules it out.
*Production of antibodies against ADAMTS13*
- This condition is **Thrombotic Thrombocytopenic Purpura (TTP)**, characterized by a **low platelet count**, microangiopathic hemolytic anemia, renal failure, neurological symptoms, and fever, none of which fully align with this patient's presentation.
- TTP usually has significant **thrombocytopenia** and normal bleeding time, despite symptoms of bleeding.
*Decreased levels of von Willebrand factor*
- **Von Willebrand disease (vWD)** would typically show a **prolonged bleeding time** and, depending on the type, may also have a prolonged PTT (due to low factor VIII).
- However, the diffuse petechiae and purpura with a normal platelet count and normal PT/PTT point more strongly towards a platelet function defect rather than a primary coagulation factor deficiency or vWD.
Platelet disorders US Medical PG Question 5: Seven days after undergoing bilateral total knee arthroplasty, a 65-year-old man comes to the physician with a dark discoloration and blisters on his abdomen. Current medications include simvastatin, aspirin, and low molecular weight heparin. His vital signs are within normal limits. Examination of the skin shows multiple coalescing blisters with areas of necrosis around the umbilicus. Laboratory studies show a platelet count of 32,000/mm3. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Antibody-platelet antigen complex formation
- B. Deficiency in ADAMTS13 activity
- C. Anti-desmoglein antibody formation
- D. Decreased production of GpIb
- E. Antibody formation against heparin-PF4 complex (Correct Answer)
Platelet disorders Explanation: ***Antibody formation against heparin-PF4 complex***
- This clinical scenario describes **Heparin-Induced Thrombocytopenia (HIT) type II**, characterized by thrombocytopenia and paradoxical thrombosis or skin necrosis, often at the injection sites.
- The **low molecular weight heparin (LMWH)** given post-surgery can induce antibodies against the heparin-platelet factor 4 (PF4) complex.
- The activation of platelets by these antibodies leads to their consumption (thrombocytopenia) and pro-thrombotic activity, resulting in skin lesions (necrosis and blisters) and potential thrombotic events.
*Antibody-platelet antigen complex formation*
- This typically refers to **Immune Thrombocytopenic Purpura (ITP)**, where antibodies are formed against platelet glycoproteins, leading to their destruction.
- ITP generally presents with mucocutaneous bleeding and does not typically cause the necrotic skin lesions seen here, nor is it directly linked to heparin administration.
*Deficiency in ADAMTS13 activity*
- This condition is characteristic of **Thrombotic Thrombocytopenic Purpura (TTP)**, presenting with microangiopathic hemolytic anemia, thrombocytopenia, renal failure, neurological symptoms, and fever (pentad).
- While TTP involves thrombocytopenia, the presentation of localized necrotic skin lesions after heparin use is not typical for TTP.
*Anti-desmoglein antibody formation*
- This is the underlying mechanism of **pemphigus vulgaris**, an autoimmune blistering skin disease.
- Pemphigus vulgaris causes widespread flaccid blisters and erosions but does not typically present with thrombocytopenia or necrosis related to heparin administration.
*Decreased production of GpIb*
- A defect in **glycoprotein Ib (GpIb)** is characteristic of **Bernard-Soulier syndrome**, a rare inherited bleeding disorder.
- This genetic disorder presents with lifelong bleeding tendencies and giant platelets, not acute thrombocytopenia and necrotic lesions triggered by medication in an older adult.
Platelet disorders US Medical PG Question 6: A previously healthy 40-year-old woman comes to the physician because of a 3-day history of fever, headaches, and fatigue. She also reports a persistent tingling sensation in her right hand and numbness in her right arm that started this morning. Physical examination shows pallor, mild scleral icterus, and petechiae on her forearms and legs. On mental status examination, she appears confused and is only oriented to person. Laboratory studies show:
Hemoglobin 11.1 g/dL
Platelet count 39,500/mm3
Bleeding time 9 minutes
Prothrombin time 14 seconds
Partial thromboplastin time 35 seconds
Serum
Creatinine 1.7 mg/dL
Total bilirubin 2.1 mg/dL
A peripheral blood smear shows fragmented erythrocytes. Which of the following is the most likely underlying cause of this patient's condition?
- A. Antibodies against double-stranded DNA
- B. Mutation of the PIGA gene
- C. Antibodies against GpIIb/IIIa
- D. Antibodies against ADAMTS13 (Correct Answer)
- E. Absence of platelet GpIIb/IIIa receptors
Platelet disorders Explanation: ***Antibodies against ADAMTS13***
- This patient presents with a classic pentad of symptoms: **fever**, **neurologic symptoms** (confusion, tingling, numbness), **renal failure** (creatinine 1.7 mg/dL), **thrombocytopenia** (platelet count 39,500/mm3), and **microangiopathic hemolytic anemia** (pallor, scleral icterus, fragmented erythrocytes on smear). This constellation of findings is highly suggestive of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is primarily caused by a deficiency of the **ADAMTS13 enzyme**, often due to **autoantibodies** that inhibit its activity. ADAMTS13 is responsible for cleaving large **von Willebrand factor (vWF) multimers**, and its deficiency leads to the accumulation of these large multimers, promoting platelet aggregation and microthrombi formation.
*Antibodies against double-stranded DNA*
- Antibodies against double-stranded DNA (**anti-dsDNA antibodies**) are characteristic of **Systemic Lupus Erythematosus (SLE)**, which can present with various systemic symptoms.
- While SLE can cause thrombocytopenia and renal involvement, it typically does not cause the severe **microangiopathic hemolytic anemia** with schistocytes or the combination of symptoms seen in this patient to the extent of TTP.
*Mutation of the PIGA gene*
- A **mutation of the *PIGA* gene** is responsible for **Paroxysmal Nocturnal Hemoglobinuria (PNH)**, a clonal stem cell disorder characterized by hemolytic anemia, thrombosis, and bone marrow failure.
- While PNH involves hemolysis, it typically lacks the prominent neurological symptoms, severe thrombocytopenia with microangiopathic features, and renal failure seen in TTP.
*Antibodies against GpIIb/IIIa*
- **Antibodies against GpIIb/IIIa** (glycoprotein IIb/IIIa) receptors are the hallmark of **Immune Thrombocytopenic Purpura (ITP)**, causing accelerated platelet destruction.
- ITP primarily causes **isolated thrombocytopenia** and mucocutaneous bleeding, but it does not cause microangiopathic hemolytic anemia, renal failure, or neurological symptoms that are prominent in this patient.
*Absence of platelet GpIIb/IIIa receptors*
- The **absence of platelet GpIIb/IIIa receptors** is characteristic of **Glanzmann's thrombasthenia**, a rare inherited disorder of platelet function.
- Glanzmann's thrombasthenia leads to **mucocutaneous bleeding** due to impaired platelet aggregation, but it does not cause thrombocytopenia, hemolytic anemia, renal failure, or neurological symptoms.
Platelet disorders US Medical PG Question 7: A 2-year-old boy had increased bleeding during a circumcision. His birth and delivery were uncomplicated, and his mother had no issues with prolonged bleeding during labor. Of note, his maternal grandfather has a history of bleeding complications. The boy's vital signs are stable and physical examination is notable for scattered bruises on his lower extremities. The lab results are as follows:
Hemoglobin 12.8 gm %
Hematocrit 35.4%
WBC 8400/mm3
Platelets 215 x 109/L
PT 14 s
PTT 78 s
What is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Hemophilia A (Correct Answer)
- C. Von Willebrand disease
- D. Scurvy
- E. Bernard-Soulier syndrome
Platelet disorders Explanation: ***Hemophilia A***
- The patient's presentation with increased bleeding during circumcision, scattered bruises, and a **prolonged PTT** with normal PT and platelet count is highly suggestive of **Hemophilia A**.
- The familial history of bleeding complications in the maternal grandfather points towards an **X-linked recessive inheritance pattern**, characteristic of Hemophilia A.
- Hemophilia A results from **Factor VIII deficiency**, affecting the intrinsic coagulation pathway.
*Glanzmann thrombasthenia*
- This condition involves a defect in **platelet aggregation** due to deficiency of **GPIIb/IIIa**, which would typically manifest with a **normal platelet count** but abnormal platelet function tests.
- While it causes bruising and bleeding, it would not affect the PTT, as coagulation factors are normal in this platelet function disorder.
*Von Willebrand disease*
- This is the **most common inherited bleeding disorder** and typically presents with mucocutaneous bleeding and menorrhagia in females.
- While it can cause a **mildly prolonged PTT** due to low Factor VIII levels (vWF stabilizes Factor VIII), the PTT is typically only **mildly elevated**, not as significantly prolonged as seen here (78s vs normal ~25-35s).
- The **X-linked family history** (affected maternal grandfather, not parents) strongly favors hemophilia over the **autosomal dominant** inheritance of most vWD cases.
*Scurvy*
- Scurvy results from **vitamin C deficiency** leading to impaired collagen synthesis.
- While it can cause bleeding issues like petechiae and gingival bleeding, it would not cause a **prolonged PTT** or present with significant bleeding during a circumcision.
- Coagulation tests remain normal in scurvy.
*Bernard-Soulier syndrome*
- This is a rare, inherited platelet disorder characterized by **giant platelets** and **thrombocytopenia**, resulting from a defect in the **glycoprotein Ib/IX/V complex**.
- It would present with mucocutaneous bleeding and bruising, but the patient's **platelet count is normal** (215 × 10⁹/L) and the PTT would not be prolonged in this platelet function disorder.
Platelet disorders US Medical PG Question 8: An 8-year-old boy is brought to the pediatric emergency department by his parents with a complaint of abdominal pain and diarrhea for the past week. He states that for the past two days, he has noticed blood in his stool. His parents note that they attended a neighbor’s barbecue last weekend, but otherwise have not eaten any new foods or changed their usual diet. The patient is admitted to the hospital unit for further work-up. The provider team finds that the patient’s blood is positive for Shiga-like toxin and notes the following lab values: creatinine of 4.2 mg/dL, platelet count of 50,000/mm^3, and hemoglobin of 6.0 g/dL. Which of the following additional lab findings would be consistent with the diagnosis?
- A. Microthrombi within glomerular vessels on kidney biopsy (Correct Answer)
- B. Blunting of villi on ileal biopsy
- C. Crypt abscesses and ulcers on colonic biopsy
- D. Foamy macrophages in intestinal lamina propria on duodenal biopsy
- E. Sickling of red blood cells on peripheral blood smear
Platelet disorders Explanation: ***Microthrombi within glomerular vessels on kidney biopsy***
- The clinical presentation (bloody diarrhea, elevated **creatinine**, low **platelets**, and low **hemoglobin**), a history of recent barbecue exposure, and presence of **Shiga-like toxin** are classic for **hemolytic uremic syndrome (HUS)**, typically caused by *E. coli* O157:H7.
- **HUS** is characterized by a **microangiopathic hemolytic anemia**, **thrombocytopenia**, and **acute kidney injury**, which pathology often reveals **microthrombi** in the glomerular capillaries.
*Blunting of villi on ileal biopsy*
- **Villus blunting** is characteristic of **celiac disease** or other malabsorptive syndromes but is not directly associated with the acute presentation of bloody diarrhea, kidney injury, and thrombocytopenia seen in HUS.
- **Celiac disease** typically presents with chronic diarrhea and malabsorption, not acute onset bloody diarrhea and hemolytic markers.
*Crypt abscesses and ulcers on colonic biopsy*
- These findings are typical of **inflammatory bowel disease (IBD)**, particularly **ulcerative colitis**, or severe infectious colitis like that caused by *Clostridium difficile*.
- While there is bloody diarrhea, the presence of **Shiga-like toxin**, **thrombocytopenia**, and **acute kidney injury** points away from IBD as the primary diagnosis.
*Foamy macrophages in intestinal lamina propria on duodenal biopsy*
- The presence of **foamy macrophages** in the lamina propria is characteristic of **Whipple's disease**, a rare systemic bacterial infection.
- This disease typically presents with chronic malabsorption, arthralgias, and neurological symptoms, which are distinct from the acute presentation of HUS.
*Sickling of red blood cells on peripheral blood smear*
- **Sickling of red blood cells** is diagnostic of **sickle cell anemia** or **sickle cell disease**, a genetic disorder.
- While it can cause hemolytic anemia and kidney complications, the presence of **Shiga-like toxin** and the specific clinical picture strongly point to HUS, not sickle cell crisis.
Platelet disorders US Medical PG Question 9: A 61-year-old man presents to the primary care clinic to establish care. He has not seen a physician for many years. He has no complaints or concerns but, on further questioning, does have some vague abdominal discomfort. He has no known past medical history and takes no medications. His social history is notable for injecting heroin throughout his late-teens and 20s, but he has been clean and sober for over a decade. At the clinic, the vital signs include: heart rate 90/min, respiratory rate 17/min, blood pressure 110/65 mm Hg, and temperature 37.0°C (98.6°F). The physical exam shows a slightly distended abdomen. The laboratory studies are notable for a platelet count of 77,000/uL and an international normalized ratio (INR) of 1.7. Which of the following is the next best step in the diagnosis of this patient?
- A. Bone marrow biopsy
- B. HIV ELISA
- C. Hepatitis C antibody (Correct Answer)
- D. Platelet aggregation assay
- E. Anti-nuclear antibody test
Platelet disorders Explanation: ***Hepatitis C antibody***
- The patient's history of **intravenous drug use** and the laboratory findings of **thrombocytopenia** and **elevated INR** strongly suggest chronic liver disease, most commonly caused by **hepatitis C virus (HCV) infection**.
- An **anti-HCV antibody test** is the appropriate initial screening test for HCV infection.
*Bone marrow biopsy*
- A bone marrow biopsy would be considered for unexplained **pancytopenia** or other specific hematological disorders, but the current clinical picture points to a more likely extra-medullary cause for the cytopenias related to liver disease.
- While it could identify issues with platelet production, it's not the first step when liver dysfunction is highly suspected.
*HIV ELISA*
- While a history of intravenous drug use is a risk factor for **HIV**, the patient's current symptoms and lab findings (thrombocytopenia, elevated INR, abdominal discomfort) are more characteristic of **chronic liver disease** rather than primary HIV complications.
- HIV testing would be reasonable as part of general health screening for this patient population, but it is not the *next best step* for the presenting concerns.
*Platelet aggregation assay*
- This assay evaluates platelet function, which is useful for diagnosing qualitative platelet disorders (e.g., Glanzmann's thrombasthenia, Bernard-Soulier syndrome).
- This patient has **thrombocytopenia** (low platelet *count*), not a functional disorder, and the elevated INR points away from primary platelet dysfunction.
*Anti-nuclear antibody test*
- An **ANA test** is used to screen for autoimmune diseases like **Systemic Lupus Erythematosus (SLE)**.
- While SLE can cause thrombocytopenia, the constellation of an elevated INR and a history of intravenous drug use makes liver disease a much more probable cause of the patient's symptoms.
Platelet disorders US Medical PG Question 10: A 64-year-old man comes to the emergency department complaining of fatigue and abdominal distension. He has a remote history of intravenous drug use. Vital signs include a normal temperature, blood pressure of 120/80 mm Hg, and a pulse of 75/min. Physical examination reveals jaundice and a firm liver. Abdominal ultrasonography shows liver surface nodularity, moderate splenomegaly, and increased diameter of the portal vein. Complete blood count of the patient is shown:
Hemoglobin 14 g/dL
Mean corpuscular volume 90/μm3
Mean corpuscular hemoglobin 30 pg/cell
Mean corpuscular hemoglobin concentration 34%
Leukocyte count 7,000/mm3
Platelet count 50,000/mm3
Which of the following best represents the mechanism of low platelet count in this patient?
- A. Platelet sequestration (Correct Answer)
- B. Dilutional effect
- C. Bone marrow-based disorder
- D. Increased platelet clearance
- E. Genetic disorder
Platelet disorders Explanation: ***Platelet sequestration***
- The patient's history of IV drug use, jaundice, abdominal distension, firm liver, splenomegaly, and increased portal vein diameter are highly suggestive of **portal hypertension** due to **cirrhosis**, which often leads to **splenomegaly**.
- An enlarged spleen (splenomegaly) sequesters a disproportionately high percentage of the body's platelets, leading to **thrombocytopenia**, even if total platelet production is normal.
- **Splenic sequestration** is the **primary mechanism** of thrombocytopenia in cirrhosis with portal hypertension; up to **90% of platelets** can be sequestered in an enlarged spleen.
- Additionally, the diseased liver produces less **thrombopoietin (TPO)**, which contributes to reduced platelet production, but sequestration remains the dominant mechanism.
*Dilutional effect*
- A dilutional effect on platelet count typically occurs with **massive transfusions** of packed red blood cells and crystalloids, which is not indicated in this patient's presentation.
- While fluid overload can dilute blood components, the patient's symptoms point specifically to a **liver pathology** and related complications, not simply volume expansion.
*Bone marrow-based disorder*
- A primary bone marrow disorder would likely affect other cell lines as well, but the patient's hemoglobin and leukocyte counts are within normal limits, making a general **bone marrow suppression** less likely.
- Furthermore, the strong evidence of **cirrhosis and portal hypertension** provides a more direct and common explanation for isolated thrombocytopenia in this context.
*Increased platelet clearance*
- While increased platelet clearance can cause thrombocytopenia (e.g., in immune thrombocytopenia or thrombotic microangiopathies), there are no signs of increased destruction or consumption in this case.
- Conditions involving increased clearance usually present with other features like petechiae, purpura, or schistocytes, which are not mentioned.
- The clinical picture is most consistent with **sequestration** rather than **destruction**.
*Genetic disorder*
- Genetic disorders causing thrombocytopenia typically present much earlier in life or have a family history, which does not fit this patient's age and clinical presentation.
- The patient's history of **IV drug use** and the findings of advanced liver disease indicate an **acquired condition**, not a congenital one.
More Platelet disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.