Hypercoagulable states US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypercoagulable states. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypercoagulable states US Medical PG Question 1: A 21-year-old woman comes to the physician because of a 1-day history of right leg pain. The pain is worse while walking and improves when resting. Eight months ago, she was diagnosed with a pulmonary embolism and was started on warfarin. Anticoagulant therapy was discontinued two months ago. Her mother had systemic lupus erythematosus. On examination, her right calf is diffusely erythematous, swollen, and tender. Cardiopulmonary examination shows no abnormalities. On duplex ultrasonography, the right popliteal vein is not compressible. Laboratory studies show an elevated serum level of D-dimer and insensitivity to activated protein C. Further evaluation of this patient is most likely to show which of the following?
- A. Deficiency of protein C
- B. Protein S deficiency
- C. Elevated coagulation factor VIII levels
- D. Mutation of coagulation factor V (Correct Answer)
- E. Mutation of prothrombin
Hypercoagulable states Explanation: ***Mutation of coagulation factor V***
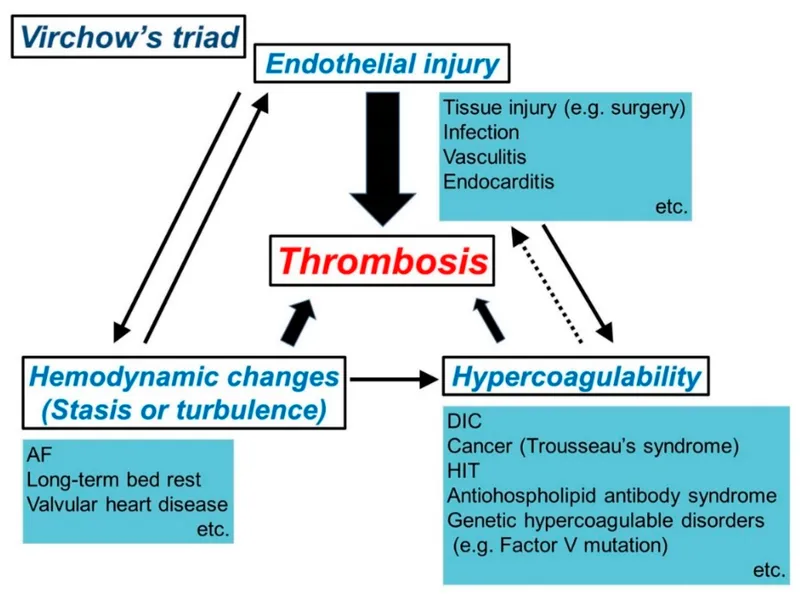
- The patient's history of **recurrent DVT/PE** at a young age, family history of autoimmune disease (mother's SLE), and laboratory finding of **insensitivity to activated protein C** strongly point towards **Factor V Leiden mutation**.
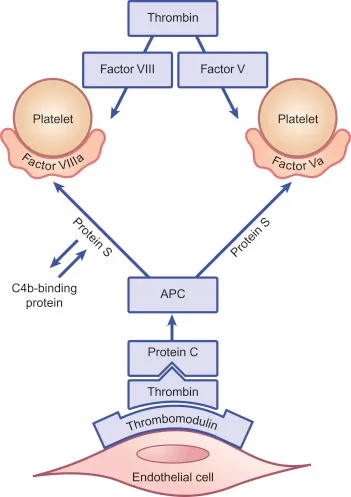
- This mutation makes **Factor V resistant to inactivation** by activated protein C, leading to a hypercoagulable state and increased risk of venous thromboembolism.
*Deficiency of protein C*
- While it also causes **insensitivity to activated protein C** and a hypercoagulable state, a true deficiency of protein C would lead to quantitative reduction, not primarily functional insensitivity.
- Protein C deficiency can cause **severe thrombotic events**, but the given lab finding of "insensitivity to activated protein C" points more directly to a defect in Factor V.
*Protein S deficiency*
- **Protein S** acts as a cofactor for activated protein C, so its deficiency would also impair the anticoagulant pathway and could lead to thrombosis.
- However, **Protein S deficiency** does not directly cause "insensitivity to activated protein C" as the primary defect; rather, it reduces the effectiveness of activated protein C.
*Elevated coagulation factor VIII levels*
- **High levels of Factor VIII** are a risk factor for VTE, but this condition would not lead to **insensitivity to activated protein C**.
- While it contributes to a hypercoagulable state, it's a distinct mechanism not indicated by the specific lab finding mentioned.
*Mutation of prothrombin*
- **Prothrombin G20210A mutation** (mutation of prothrombin) leads to increased prothrombin levels and increased thrombin generation, predisposing to thrombosis.
- However, this mutation would not result in **insensitivity to activated protein C**, which is the key laboratory finding in this patient.
Hypercoagulable states US Medical PG Question 2: A 3-week-old boy is brought to the pediatrician by his parents for a circumcision. The circumcision was uncomplicated; however, after a few hours, the diaper contained blood, and the bleeding has not subsided. A complete blood count was ordered, which was significant for a platelet count of 70,000/mm3. On peripheral blood smear, the following was noted (figure A). The prothrombin time was 12 seconds, partial thromboplastin time was 32 seconds, and bleeding time was 13 minutes. On platelet aggregation studies, there was no response with ristocetin. This result was not corrected with the addition of normal plasma. There was a normal aggregation response with the addition of ADP. Which of the following is most likely true of this patient's underlying disease?
- A. Protein C resistance
- B. Decreased GpIb (Correct Answer)
- C. Responsive to desmopressin
- D. Adding epinephrine would not lead to platelet aggregation
- E. Decreased GpIIb/IIIa
Hypercoagulable states Explanation: ***Decreased GpIb***
- The presentation of **persistent severe bleeding** after circumcision, **thrombocytopenia (70,000/mm3)**, and **giant platelets** on blood smear are classic findings for **Bernard-Soulier syndrome**.
- **Bernard-Soulier syndrome** is characterized by a defect in the platelet glycoprotein Ib-IX-V (GpIb) complex, which is crucial for **platelet adhesion** to **von Willebrand factor (vWF)** on exposed subendothelium. The **lack of aggregation response to ristocetin** (which induces vWF binding to GpIb) and its **non-correction with normal plasma** further confirm this diagnosis.
*Protein C resistance*
- **Protein C resistance** is associated with an **increased risk of thrombosis**, not bleeding, and is typically due to a mutation in **Factor V (Factor V Leiden)**, which makes it resistant to inactivation by activated Protein C.
- This condition would manifest with **venous thromboembolism** or recurrent miscarriages, which contradicts the patient's bleeding symptoms.
*Responsive to desmopressin*
- **Desmopressin** (DDAVP) primarily acts by releasing **von Willebrand factor (vWF)** and **Factor VIII** from endothelial cells. It is effective in certain types of **von Willebrand disease** and **mild hemophilia A**.
- Since the issue here is with the **platelet receptor (GpIb)** for vWF, and not with vWF quantity or quality, desmopressin would **not be an effective treatment** for Bernard-Soulier syndrome.
*Adding epinephrine would not lead to platelet aggregation*
- In **Bernard-Soulier syndrome**, the defect is specific to the **GpIb-vWF interaction**. Platelet aggregation responses to other agonists like **ADP, collagen, and epinephrine** are typically **normal** or at least partially preserved, although the defect in GpIb can subtly impair secondary aggregation.
- The aggregation studies showing a **normal response to ADP** in this patient support that other aggregation pathways are intact, making this statement incorrect.
*Decreased GpIIb/IIIa*
- **Decreased GpIIb/IIIa** (or qualitative defects in it) is characteristic of **Glanzmann thrombasthenia**, another inherited platelet disorder.
- Patients with Glanzmann thrombasthenia also present with **bleeding** and **impaired platelet aggregation**, but their platelets are usually **normal in size and count**, and they show **absent aggregation to ADP, collagen, and epinephrine**, while aggregation to ristocetin is normal, which is different from this patient's findings.
Hypercoagulable states US Medical PG Question 3: A 29-year-old woman comes to the office with her husband because she has had 4 spontaneous abortions. Regarding her medical history, she was diagnosed with systemic lupus erythematosus 9 years ago, had a stroke 3 years ago, and was diagnosed with deep vein thrombosis in the same year. She has no relevant family history. Her vital signs include: heart rate 78/min, respiratory rate 14/min, temperature 37.5°C (99.5°F), and blood pressure 120/85 mm Hg. The physical examination is unremarkable. The complete blood count results are as follows:
Hemoglobin 12.9 g/dL
Hematocrit 40%
Leukocyte count 8,500/mm3
Neutrophils 55%
Bands 2%
Eosinophils 1%
Basophils 0%
Lymphocytes 29%
Monocytes 2%
Platelet count 422,000/mm3
Her coagulation test results are as follows:
Partial thromboplastin time (activated) 50.9 s
Prothrombin time 13.0 s
A VDRL test is done, and the result is positive. Mixing studies are performed, and they fail to correct aPTT. What is the most likely cause in this patient?
- A. Antithrombin deficiency
- B. Protein S deficiency
- C. Protein C deficiency
- D. Antiphospholipid syndrome (Correct Answer)
- E. Factor V Leiden mutation
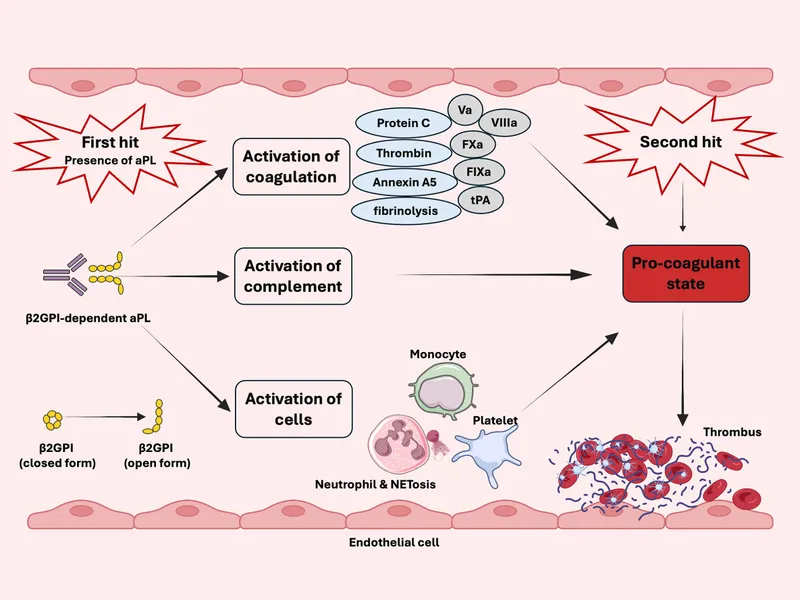
Hypercoagulable states Explanation: ***Antiphospholipid syndrome***
- The patient's history of **recurrent spontaneous abortions**, **stroke**, **deep vein thrombosis**, and a **positive VDRL** (often falsely positive in APS) in the context of SLE strongly suggests antiphospholipid syndrome.
- The **prolonged aPTT** that **fails to correct** with mixing studies indicates the presence of a circulating anticoagulant, such as the lupus anticoagulant, which is characteristic of APS.
*Antithrombin deficiency*
- Antithrombin deficiency typically presents with a tendency for **thrombosis**, but it would **not cause recurrent abortions** or a **false-positive VDRL**.
- It would also **not affect aPTT** in the manner seen here (prolonged and unresponsive to mixing).
*Factor V Leiden mutation*
- **Factor V Leiden** is a common cause of **thrombophilia** and recurrent thrombosis. However, it is **not associated with recurrent abortions**, **false-positive VDRL**, or **prolonged aPTT**.
- This mutation leads to resistance to inactivation by protein C, increasing clot risk, but does not affect coagulation tests like aPTT in this specific way.
*Protein S deficiency*
- Protein S deficiency, like Factor V Leiden, is associated with an increased risk of **venous thrombosis**. However, it is **not directly linked to recurrent abortions** or a **false-positive VDRL**.
- It also does not typically cause a **prolonged aPTT** that fails to correct with mixing studies.
*Protein C deficiency*
- Protein C deficiency is a risk factor for **venous thrombosis** and can be associated with severe complications like **warfarin-induced skin necrosis**.
- Similar to other hereditary thrombophilias, it does **not explain the recurrent abortions**, **false-positive VDRL**, or the **specific aPTT findings** observed in this patient.
Hypercoagulable states US Medical PG Question 4: A 12-year-old boy is brought by his mother to the emergency room because of a swollen, hot, and tender knee that he sustained after falling on his way home. He has never had a swollen joint before; however, he has had frequent nosebleeds throughout his life. His mother is worried because they live with her parents who are currently on blood thinners. Every morning she puts the blood thinner pill in the boy's grandfather's milk and was concerned that she may have switched it this morning. Family history reveals a number of uncles who have had bleeding disorders; however, the mother does not know the exact disorder suffered by these relatives. A hematologic panel reveals the following findings:
Bleeding time: Increased
Prothrombin time: 12 seconds
Partial thromboplastin time (PTT): 55 seconds
PTT after factor mixing study: 37 seconds
Which of the following most likely explains the abnormal partial thromboplastin time in this patient?
- A. Inhibition of reductase enzyme
- B. Antibodies to factor VIII
- C. Activation of inhibitory factors
- D. Mutation in factor VIII
- E. Mutation in carrying protein (Correct Answer)
Hypercoagulable states Explanation: ***Mutation in carrying protein***
- This scenario describes **von Willebrand disease**, characterized by an **increased bleeding time** and an **elevated PTT** that corrects with a mixing study. The **mutation in the von Willebrand factor (vWF) protein**, which carries and protects factor VIII, leads to its rapid degradation.
- The **normal PT** rules out common pathway or extrinsic pathway coagulation defects, while the prolonged PTT points to an intrinsic pathway issue. The family history of bleeding disorders and frequent nosebleeds further supports this diagnosis, as vWF is essential for **platelet adhesion** and stabilizing factor VIII.
*Inhibition of reductase enzyme*
- Inhibition of the **reductase enzyme** (specifically **vitamin K epoxide reductase**) by drugs like warfarin would lead to deficiencies in **vitamin K-dependent clotting factors (II, VII, IX, X)**.
- This would result in a **prolonged PT** (due to reduced factor VII) and often a prolonged PTT, which is not seen here as PT is normal.
*Antibodies to factor VIII*
- **Antibodies to factor VIII** (acquired hemophilia) would lead to a prolonged PTT that **would not correct** with a mixing study, as the inhibitor would neutralize the added factor VIII.
- While acquired hemophilia can lead to severe bleeding, the correction with the mixing study points away from an inhibitor.
*Activation of inhibitory factors*
- **Activation of inhibitory factors** (e.g., lupus anticoagulant) would typically result in a prolonged PTT that **does not correct** with a mixing study (or only partially corrects), similar to an acquired factor VIII inhibitor.
- The complete correction of PTT in the mixing study makes this option less likely.
*Mutation in factor VIII*
- A **mutation in factor VIII** itself (hemophilia A) would cause a **prolonged PTT** that **corrects with a mixing study**, as the added normal plasma would supply the missing factor VIII.
- However, in this case, the **increased bleeding time** and the mention of a "carrying protein" point more specifically to **von Willebrand disease**, where vWF helps stabilize factor VIII.
Hypercoagulable states US Medical PG Question 5: A 35-year-old woman presents to her primary care physician for recurrent deep venous thrombosis (DVT) of her left lower extremity. She is a vegetarian and often struggles to maintain an adequate intake of non-animal based protein. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and currently denies any illicit drug use, although she endorses a history of heroin use (injection). Her past medical history is significant for 4 prior admissions for lower extremity swelling and pain that resulted in diagnoses of deep venous thrombosis. Her vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 16/min. On physical examination, her pulses are bounding, the patient's complexion is pale, breath sounds are clear, and heart sounds are normal. The spleen is mildly enlarged. She is admitted for DVT treatment and a full hypercoagulability workup. Which of the following is the best initial management for this patient?
- A. Begin heparin
- B. Begin warfarin, target INR 2.5–3.5
- C. Consult IR for IVC filter placement
- D. Begin heparin and warfarin (Correct Answer)
- E. Begin warfarin, target INR 2.0–3.0
Hypercoagulable states Explanation: ***Begin heparin and warfarin***
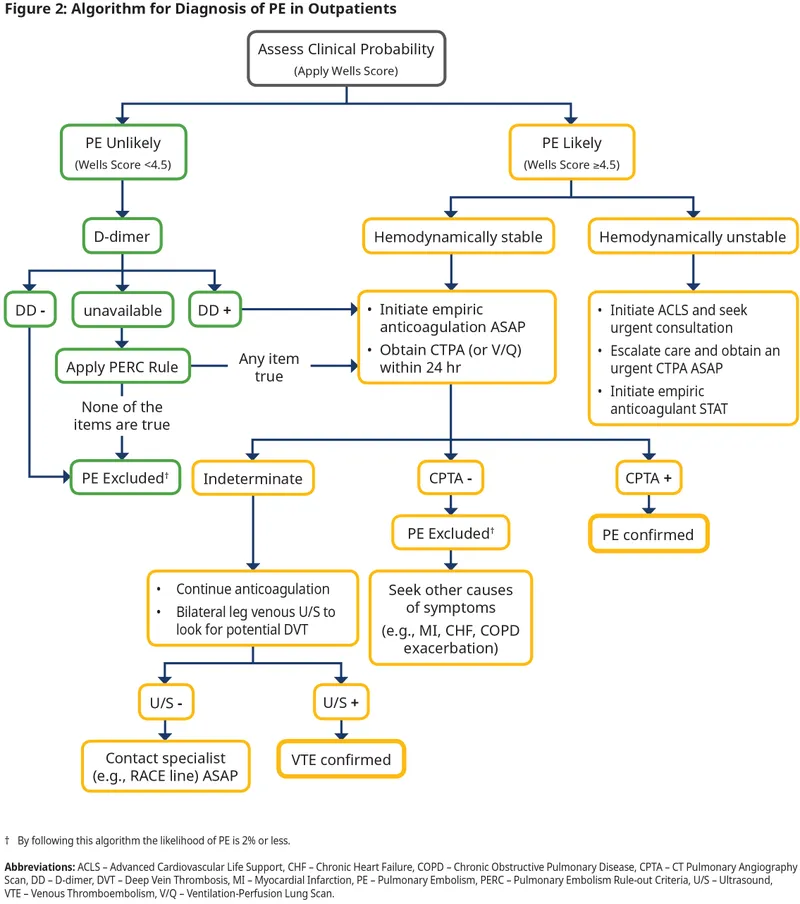
- For **acute DVT**, immediate anticoagulation with **heparin** (or another direct thrombin inhibitor/factor Xa inhibitor) is crucial to prevent clot propagation and pulmonary embolism.
- **Warfarin** is started concurrently, as it has a slower onset of action; heparin provides protection until warfarin reaches a therapeutic INR.
*Begin heparin*
- While **heparin** is the correct initial therapy for acute DVT, it is insufficient on its own for long-term management due to its short half-life and need for continuous infusion (unfractionated) or daily injections (low molecular weight).
- A long-term oral anticoagulant like warfarin or a direct oral anticoagulant (DOAC) is necessary for extended prophylaxis, especially in a patient with recurrent DVT.
*Begin warfarin, target INR 2.5–3.5*
- **Warfarin** is appropriate for long-term anticoagulation, but it has a delayed onset of action and requires several days to reach therapeutic levels, during which time the patient would be unprotected from clot extension or embolization.
- The initial target INR for most VTE is 2.0-3.0, though for recurrent events or certain conditions, a higher range might be considered later, but 2.5-3.5 is not the standard initial target.
*Consult IR for IVC filter placement*
- **IVC filters** are typically reserved for patients with an acute DVT who have a **contraindication to anticoagulation** or who experience recurrent PE despite adequate anticoagulation.
- There is no mention of contraindications to anticoagulation in this patient, and filters are not a primary treatment for acute DVT but rather a preventative measure against pulmonary embolism in specific high-risk scenarios.
*Begin warfarin, target INR 2.0–3.0*
- While **warfarin** at an INR target of 2.0-3.0 is a standard long-term therapy for DVT, beginning it alone is inappropriate for acute DVT due to its **delayed therapeutic effect**.
- Without concurrent rapid-acting anticoagulation (like heparin), the patient remains at high risk for complications while awaiting warfarin's full effect.
Hypercoagulable states US Medical PG Question 6: A 57-year-old immigrant from Nigeria presents to the emergency department for sudden, severe pain and swelling in her lower extremity. She was at a rehabilitation hospital when her symptoms became apparent. The patient has a past medical history of obesity, diabetes, bipolar disorder, and tonic-clonic seizures. Her current medications include metformin, insulin, lisinopril, and valproic acid. The patient is a prominent IV drug and alcohol user who has presented to the ED many times for intoxication. On physical exam you note anasarca and asymmetric lower extremity swelling. Based on the results of a doppler ultrasound of her swollen lower extremity, heparin is started. The patient is then transferred to the general medicine floor for continued management. Laboratory studies are shown below.
Serum:
Na+: 137 mEq/L
K+: 5.5 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 22 mg/dL
Ca2+: 5.7 mg/dL
Creatinine: 1.7 mg/dL
Glucose: 70 mg/dL
The patient's presentation includes generalized edema (anasarca) along with laboratory abnormalities. What is the most likely underlying diagnosis that explains her overall clinical presentation?
- A. Liver failure
- B. Nephrotic syndrome (Correct Answer)
- C. Antithrombin III deficiency
- D. Prothrombin gene mutation
- E. Factor V Leiden
Hypercoagulable states Explanation: ***Nephrotic syndrome***
- The patient presents with **anasarca** (generalized edema), **asymmetric lower extremity swelling**, and laboratory findings consistent with **nephrotic syndrome**.
- Classic features present: **anasarca** (from hypoalbuminemia and fluid retention), **hypercoagulable state** leading to DVT (loss of antithrombin III in urine), and **renal dysfunction** (elevated creatinine 1.7 mg/dL).
- The **hypocalcemia (5.7 mg/dL)** is explained by low albumin—total calcium appears low because ~40% of serum calcium is albumin-bound; ionized calcium is likely normal.
- Nephrotic syndrome is characterized by: heavy proteinuria (>3.5 g/day), hypoalbuminemia, hyperlipidemia, and edema—this patient's presentation fits this diagnosis.
- Risk factors include diabetes (diabetic nephropathy is a common cause of nephrotic syndrome in adults).
*Liver failure*
- Although **anasarca** and **edema** can occur in liver failure due to decreased albumin synthesis and portal hypertension, the laboratory values do not show typical signs of severe hepatic dysfunction (e.g., elevated transaminases, bilirubin, or prolonged INR).
- The **elevated creatinine** and **hypercoagulable state with DVT** point more towards a primary renal issue rather than liver failure.
- Liver failure typically causes **hypocoagulability**, not the hypercoagulability seen here.
*Antithrombin III deficiency*
- This is a **hereditary thrombophilia** that increases the risk of **venous thromboembolism**, which could explain the DVT.
- However, it does **not explain** the patient's **anasarca**, **hypocalcemia**, **elevated creatinine**, or generalized fluid retention.
- This would be a complication of nephrotic syndrome (acquired AT-III deficiency from urinary loss), not the primary diagnosis.
*Prothrombin gene mutation*
- This is another **genetic thrombophilia** (G20210A mutation) that increases the risk of **blood clots**.
- Similar to Antithrombin III deficiency, it accounts for DVT risk but **fails to explain** the widespread edema, electrolyte abnormalities, and renal dysfunction.
*Factor V Leiden*
- The **Factor V Leiden mutation** is the most common inherited cause of **thrombophilia**, predisposing individuals to venous thromboembolism.
- While relevant to explaining DVT in isolation, it does **not explain** the patient's severe generalized edema, hypocalcemia, or renal impairment—all of which are key to this clinical presentation.
Hypercoagulable states US Medical PG Question 7: A 61-year-old man presents to the emergency room with a painful, swollen left leg. He states that his symptoms began that morning after a long flight from Australia. He denies shortness of breath, chest pain, or cough. On review of systems, he notes that he has been constipated recently and had several episodes of bright red blood per rectum. He has not noticed any weight loss, fevers, or night sweats. He has a past medical history of a deep vein thrombosis 4 years ago during a hospitalization for community acquired pneumonia and was treated with warfarin for 3 months afterward. He also has chronic hepatitis C from previous intravenous drug use. The patient has a 30 pack-year smoking history and has never had a colonoscopy. His father is 84-years-old and has chronic kidney disease from diabetes, and his mother passed away from a massive pulmonary embolus when pregnant with his younger sister. In the emergency room, his temperature is 98.7°F (37.1°C), blood pressure is 142/85 mm/Hg, pulse is 79/min, and respirations are 14/min. On exam, he is in no acute distress. His left calf is larger in caliber than the right calf which is red and tender to palpation. Dorsiflexion of the foot worsens the pain. His abdomen is soft, nontender, and nondistended without hepatomegaly. The remainder of the physical exam is unremarkable. Labs are shown below:
Hemoglobin: 13.0 g/dL
Leukocyte count: 6,000/mm^3
Platelets: 160,000/mm^3
Aspartate aminotransferase: 15 U/L
Alanine aminotransferase: 19 U/L
Alkaline phosphatase: 81 IU/L
Hepatitis C antibody: reactive
Hepatitis C titer: 0 copies/mL
Which of the following is the most likely cause of this patient’s condition?
- A. Increased estrogen levels
- B. Loss of antithrombin III in urine
- C. Protein C deficiency
- D. Resistance of factor V to inactivation by protein C (Correct Answer)
- E. Malignancy
Hypercoagulable states Explanation: ***Resistance of factor V to inactivation by protein C***
- This patient has **Factor V Leiden mutation**, the most common inherited thrombophilia (present in 5% of Caucasians)
- **Key diagnostic clues**: Recurrent DVT (even if provoked events have lower thresholds in Factor V Leiden) and **strong family history** - mother with massive PE during pregnancy is highly suggestive, as pregnancy unmasks inherited thrombophilias
- Factor V Leiden causes **resistance to activated protein C**, leading to prolonged clotting and increased VTE risk
- While the rectal bleeding raises concern for malignancy, the **family history of thromboembolism** points to an inherited predisposition as the underlying cause
*Malignancy*
- Malignancy causes hypercoagulability through multiple mechanisms (tissue factor release, inflammatory cytokines, platelet activation)
- The patient's **rectal bleeding, constipation, age 61, and lack of screening colonoscopy** are concerning for colorectal cancer
- Malignancy is a strong consideration and warrants urgent colonoscopy
- However, the **family history of massive PE in mother during pregnancy** more strongly suggests an inherited thrombophilia as the primary cause, though malignancy could be a coexisting/triggering factor
*Increased estrogen levels*
- Estrogen increases synthesis of clotting factors and decreases anticoagulant proteins, raising DVT risk
- Seen with oral contraceptives, hormone replacement therapy, or pregnancy
- This patient is a **61-year-old male**, making estrogen-related thrombosis extremely unlikely
*Loss of antithrombin III in urine*
- Occurs in **nephrotic syndrome** (proteinuria >3.5 g/day, hypoalbuminemia, edema, hyperlipidemia)
- Loss of antithrombin III causes hypercoagulability
- This patient has **no proteinuria, normal liver enzymes, no edema**, and no other features of nephrotic syndrome
*Protein C deficiency*
- Hereditary protein C deficiency is a rare thrombophilia causing recurrent VTE
- While possible, **Factor V Leiden is 10-20 times more common** than protein C deficiency
- The family history pattern (mother with PE in pregnancy) is more characteristic of Factor V Leiden
Hypercoagulable states US Medical PG Question 8: A 24-year-old woman comes to the physician because of pain and swelling of her left leg over the past 24 hours. The pain is worse while walking and improves when resting. Seven months ago, she was diagnosed with a pulmonary embolism and was started on warfarin. Anticoagulant therapy was discontinued 1 month ago. Her sister has systemic lupus erythematosus. The patient does not smoke. She currently takes no medications. Her temperature is 37.8°C (100°F), pulse is 78/min, and blood pressure is 123/72 mm Hg. On physical examination, the left calf is diffusely erythematous, swollen, and tender. Dorsal flexion of the left foot elicits pain. Cardiopulmonary examination shows no abnormalities. On duplex ultrasonography, the left popliteal vein is not compressible. Laboratory studies show an elevated serum concentration of D-dimer and insensitivity to activated protein C. Further examination is most likely to show which of the following?
- A. Deficiency of protein C
- B. Mutation of prothrombin
- C. Elevated levels of homocysteine
- D. Antiphospholipid antibodies
- E. Mutation of coagulation factor V (Correct Answer)
Hypercoagulable states Explanation: ***Mutation of coagulation factor V***
- The patient presents with symptoms and signs of **deep vein thrombosis (DVT)**, recurrent as she had a previous pulmonary embolism, and an elevated D-dimer.
- The specific finding of **insensitivity to activated protein C (APC)** is highly suggestive of a **Factor V Leiden mutation**, which is the most common inherited thrombophilia.
*Deficiency of protein C*
- A deficiency in **protein C** would lead to a hypercoagulable state due to reduced inactivation of factors Va and VIIIa.
- However, while it would cause a predisposition to thrombosis, it would not directly manifest as **insensitivity to activated protein C (APC)** but rather as reduced levels of protein C activity.
*Mutation of prothrombin*
- A **prothrombin gene mutation (G20210A)** leads to elevated prothrombin levels, increasing clotting risk.
- While it causes thrombosis, it does not explain the specific finding of **insensitivity to activated protein C**.
*Elevated levels of homocysteine*
- **Hyperhomocysteinemia** can result from genetic defects (e.g., MTHFR mutation) or nutritional deficiencies (e.g., B12, folate) and is a risk factor for thrombosis.
- This condition does not directly cause **insensitivity to activated protein C** and would be reflected by elevated homocysteine levels, not an APC resistance assay.
*Antiphospholipid antibodies*
- **Antiphospholipid syndrome** is an acquired thrombophilia featuring antibodies (e.g., lupus anticoagulant, anticardiolipin) that cause thrombosis. The patient's sister has SLE, which is associated with antiphospholipid syndrome.
- While it can cause recurrent thrombosis and may be suggested by her sister's SLE, it typically causes a **prolonged PTT** *in vitro* (due to lupus anticoagulant) and does not directly cause **insensitivity to activated protein C**; rather, it often involves a different mechanism of action on the clotting cascade.
Hypercoagulable states US Medical PG Question 9: A 48-year-old man comes to the emergency department because of sudden right flank pain that began 3 hours ago. He also noticed blood in his urine. Over the past two weeks, he has developed progressive lower extremity swelling and a 4-kg (9-lb) weight gain. Examination shows bilateral 2+ pitting edema of the lower extremities. Urinalysis with dipstick shows 4+ protein, positive glucose, and multiple red cell and fatty casts. Abdominal CT shows a large right kidney with abundant collateral vessels and a filling defect in the right renal vein. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Factor V Leiden
- B. Malignant erythropoietin production
- C. Antiphospholipid antibodies
- D. Increased lipoprotein synthesis
- E. Loss of antithrombin III (Correct Answer)
Hypercoagulable states Explanation: ***Loss of antithrombin III***
- The patient presents with **nephrotic syndrome** (lower extremity edema, weight gain, 4+ proteinuria, fatty casts), which causes massive urinary loss of proteins, including **antithrombin III**, a critical inhibitor of coagulation.
- Loss of **antithrombin III** creates a **hypercoagulable state**, predisposing to **renal vein thrombosis** (RVT), which explains the acute flank pain, hematuria, enlarged kidney, and filling defect on CT.
- This is the underlying mechanism linking the nephrotic syndrome to the thrombotic complication.
*Factor V Leiden*
- This is a **genetic mutation** causing Factor V resistance to activated protein C, leading to hypercoagulability.
- While it can cause venous thrombosis, it does **not cause nephrotic syndrome** with massive proteinuria and fatty casts as seen in this patient.
- This would be a predisposing factor, not the underlying cause of the nephrotic syndrome itself.
*Antiphospholipid antibodies*
- These antibodies cause a **hypercoagulable state** and can lead to both arterial and venous thromboses, including RVT.
- However, they do **not directly cause nephrotic syndrome** with the massive proteinuria and fatty casts seen here.
- Like Factor V Leiden, this would predispose to thrombosis but doesn't explain the primary renal pathology.
*Increased lipoprotein synthesis*
- This is a **consequence** of nephrotic syndrome, where hepatic compensation for albumin loss leads to increased synthesis of all proteins, including lipoproteins, causing hyperlipidemia.
- It is a **secondary effect**, not the mechanism causing the hypercoagulable state and renal vein thrombosis.
*Malignant erythropoietin production*
- This would cause **polycythemia** (increased RBC count) and potentially thrombotic events due to hyperviscosity.
- It does **not explain** the profound nephrotic syndrome with massive proteinuria, edema, and fatty casts.
- There is no evidence of polycythemia in this clinical presentation.
Hypercoagulable states US Medical PG Question 10: A 28-year-old woman at 36 weeks gestation presents with severe headache, epigastric pain, and visual disturbances. Her blood pressure is 160/110 mmHg. Laboratory studies show a hematocrit of 32%, leukocyte count of 9,400/mm³, and platelet count of 96,000/mm³. Serum studies reveal an aspartate aminotransferase of 94 U/L and an alanine aminotransferase of 92 U/L. Which of the following is the most likely cause of this patient's condition?
- A. Overactivation of the coagulation pathway (Correct Answer)
- B. Thrombotic obstruction of hepatic veins
- C. Sequestration of platelets in the spleen
- D. Embolism of amniotic fluid into maternal circulation
- E. Viral reactivation and replication
Hypercoagulable states Explanation: ***Overactivation of the coagulation pathway***
- This patient's symptoms (severe headache, epigastric pain, visual disturbances), hypertension (160/110 mmHg), **thrombocytopenia** (platelet count 96,000/mm³), and elevated liver enzymes (AST 94 U/L, ALT 92 U/L) are classic signs of **HELLP syndrome** (Hemolysis, Elevated Liver enzymes, Low Platelet count), a severe form of preeclampsia.
- HELLP syndrome is characterized by widespread **endothelial dysfunction**, leading to microvascular damage, platelet activation, and consumption, which are consequences of overactive coagulation and fibrin deposition.
*Thrombotic obstruction of hepatic veins*
- This condition, known as **Budd-Chiari syndrome**, typically presents with **ascites**, hepatomegaly, and abdominal pain, which are not primary features in this patient.
- While it can cause elevated liver enzymes, it doesn't usually explain the widespread microangiopathic changes or severe hypertension seen in HELLP syndrome.
*Sequestration of platelets in the spleen*
- **Hypersplenism** can lead to thrombocytopenia due to increased platelet destruction or sequestration in an enlarged spleen.
- However, this condition does not explain the patient's severe hypertension, elevated liver enzymes, or visual disturbances.
*Embolism of amniotic fluid into maternal circulation*
- **Amniotic fluid embolism** is a rare and catastrophic event presenting with sudden **cardiovascular collapse**, **respiratory distress**, and coagulopathy, often immediately postpartum or during labor.
- This patient's presentation with chronic symptoms like hypertension, epigastric pain, and visual disturbances is not consistent with an acute embolic event.
*Viral reactivation and replication*
- Viral infections, such as those causing **hepatitis**, can lead to elevated liver enzymes and sometimes thrombocytopenia.
- However, they typically do not cause the severe hypertension, visual disturbances, and epigastric pain characteristic of severe preeclampsia or HELLP syndrome.
More Hypercoagulable states US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.