Coagulation factor disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Coagulation factor disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Coagulation factor disorders US Medical PG Question 1: A 14-year-old boy presents with his mother complaining of a swollen, red, painful left knee. His physician aspirates the joint and discovers frank blood. The patient denies a recent history of trauma to the knee. Upon further discussion, the mother describes that her son has had multiple swollen painful joints before, often without evidence of trauma. She also mentions a history of frequent nosebleeds and gum bleeding following visits to the dentist. Which of the following is the most likely underlying diagnosis?
- A. Factor VII deficiency
- B. Hemophilia C
- C. Child abuse
- D. Hemophilia B
- E. Hemophilia A (Correct Answer)
Coagulation factor disorders Explanation: ***Hemophilia A***
- The presentation of recurrent **hemarthroses** (swollen, red, painful joints with frank blood on aspiration) without trauma, along with a history of spontaneous bleeding (nosebleeds, gum bleeding), is highly characteristic of hemophilia.
- **Hemophilia A**, caused by a deficiency in factor VIII, is the most common type of severe hemophilia and often presents in childhood with these bleeding manifestations, particularly in joints.
*Factor VII deficiency*
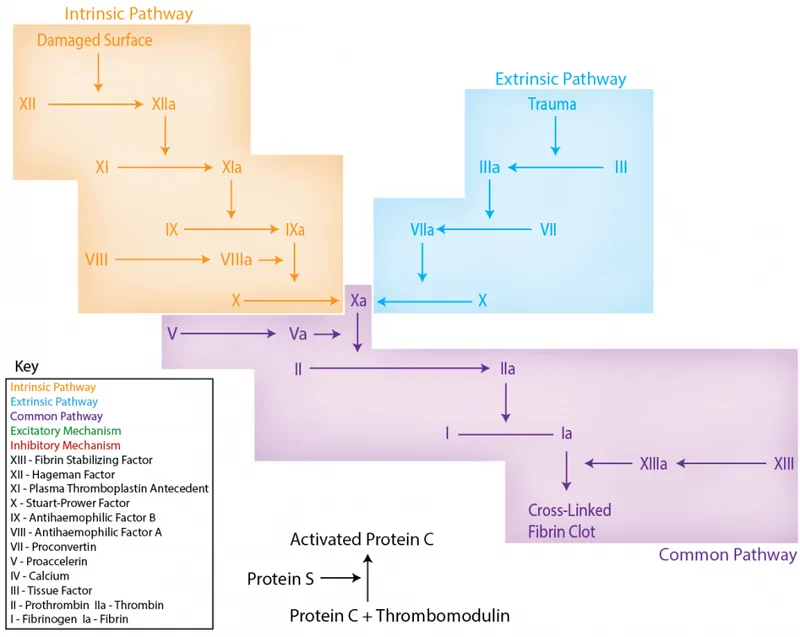
- Factor VII deficiency primarily affects the **extrinsic pathway** of coagulation and typically presents with a prolonged **prothrombin time (PT)**, while the activated partial thromboplastin time (aPTT) would be normal.
- Clinical manifestations are usually milder than hemophilia A, but can include epistaxis, menorrhagia, and occasionally hemarthroses, but not with the classic severity and frequency seen here.
*Hemophilia C*
- Hemophilia C, caused by **factor XI deficiency**, is a milder bleeding disorder, often presenting with bleeding after trauma or surgery rather than spontaneous joint bleeding.
- It mainly affects Ashkenazi Jews and typically causes a prolonged **aPTT**, but usually less severe symptoms than hemophilia A or B.
*Child abuse*
- While child abuse should always be considered in cases of unexplained trauma, the detailed history of **recurrent, spontaneous bleeding events** (hemarthroses, nosebleeds, gum bleeding post-dental work) without a clear traumatic cause is more indicative of a systemic bleeding disorder.
- The pattern of bleeding is consistent with a coagulation defect rather than isolated traumatic injuries.
*Hemophilia B*
- Hemophilia B, or Christmas disease, is caused by **factor IX deficiency** and presents with symptoms clinically indistinguishable from hemophilia A (i.e., spontaneous joint and deep tissue bleeding).
- However, Hemophilia A is significantly more common than Hemophilia B (affecting about 1 in 5,000 to 10,000 live male births, compared to 1 in 25,000 to 30,000 for Hemophilia B). Therefore, Hemophilia A is the most likely diagnosis.
Coagulation factor disorders US Medical PG Question 2: An otherwise healthy 23-year-old man comes to the physician because of a 3-day history of mild persistent bleeding from the site of a tooth extraction. He has no prior history of medical procedures or surgeries and no history of easy bruising. He appears well. Vital signs are within normal limits. Laboratory studies show:
Hemoglobin 12.4 g/dL
Platelets 200,000/mm3
Serum
Prothrombin time 25 seconds
Partial thromboplastin time (activated) 35 seconds
Deficiency of which of the following coagulation factors is the most likely cause of this patient’s condition?
- A. Factor II
- B. Factor XIII
- C. Factor X
- D. Factor VII (Correct Answer)
- E. Factor V
Coagulation factor disorders Explanation: ***Factor VII***
- An **isolated prolonged PT** with a normal aPTT, platelets, and hemoglobin points to a defect in the **extrinsic pathway** of coagulation.
- **Factor VII** is the sole coagulation factor exclusively in the extrinsic pathway, making its deficiency the most likely cause.
*Factor II*
- **Factor II (prothrombin)** is a common pathway factor, so its deficiency would prolong both PT and aPTT.
- The patient's aPTT is normal, ruling out a significant deficiency of Factor II.
*Factor XIII*
- **Factor XIII** is responsible for stabilizing the fibrin clot but does not affect PT or aPTT.
- A deficiency would present with delayed bleeding or poor wound healing, not a prolonged PT.
*Factor X*
- **Factor X** is a common pathway factor, and its deficiency would prolong both PT and aPTT.
- The normal aPTT in this patient makes Factor X deficiency unlikely.
*Factor V*
- **Factor V** is a common pathway factor, and its deficiency would result in prolongation of both PT and aPTT.
- The normal aPTT makes a Factor V deficiency improbable.
Coagulation factor disorders US Medical PG Question 3: A graduate student at the biochemistry laboratory decides to research the different effects of vitamin deficiencies in mice by completely depriving the mice of one vitamin. The symptoms of this deficiency include posterior column and spinocerebellar tract demyelination, as well as hemolytic anemia. Further analysis is negative for megaloblastic anemia, hypersegmented neutrophils, and elevated serum methylmalonic acid. What characteristic of the vitamin is causing the symptoms in the mice?
- A. The vitamin is important in rod and cone cells for vision
- B. Deficiency causes the impaired production of blood clotting factors in the liver
- C. The vitamin facilitates iron absorption
- D. The vitamin controls serum calcium levels
- E. The vitamin acts as a major antioxidant protecting cell membranes from oxidative damage (Correct Answer)
Coagulation factor disorders Explanation: ***The vitamin acts as a major antioxidant protecting cell membranes from oxidative damage***
- The symptoms of **posterior column and spinocerebellar tract demyelination** and **hemolytic anemia** are classic signs of **vitamin E deficiency**.
- **Vitamin E** is a **major lipid-soluble antioxidant** that protects cell membranes (including those in neurons and red blood cells) from **oxidative damage** by free radicals.
*The vitamin is important in rod and cone cells for vision*
- This statement describes the function of **vitamin A**, which is crucial for the synthesis of **rhodopsin** in rod cells and **iodopsin** in cone cells.
- **Vitamin A deficiency** typically causes **night blindness** and **xerophthalmia**, not demyelination or hemolytic anemia.
*Deficiency causes the impaired production of blood clotting factors in the liver*
- This describes **vitamin K deficiency**, which leads to a coagulopathy due to its role in the **gamma-carboxylation** of clotting factors **II, VII, IX, and X** in the liver.
- **Vitamin K deficiency** presents with **bleeding tendencies**, not neurological symptoms or hemolytic anemia.
*The vitamin facilitates iron absorption*
- This describes **vitamin C (ascorbic acid)**, which enhances **non-heme iron absorption** by reducing ferric iron (Fe3+) to ferrous iron (Fe2+).
- **Vitamin C deficiency** causes **scurvy**, characterized by **gingivitis**, **petechiae**, and impaired wound healing, not the symptoms listed.
*The vitamin controls serum calcium levels*
- This function is primarily attributed to **vitamin D**, which plays a critical role in **calcium and phosphate homeostasis** by regulating their absorption from the gut and reabsorption from the kidneys.
- **Vitamin D deficiency** causes **rickets** in children and **osteomalacia** in adults, primarily affecting bone health.
Coagulation factor disorders US Medical PG Question 4: A 46-year-old man diagnosed with pancreatic adenocarcinoma is admitted with fever, malaise, and dyspnea. He says that symptoms onset 2 days ago and have progressively worsened. Past medical history is significant for multiple abdominal surgeries including stenting of the pancreatic duct. Current inpatient medications are rosuvastatin 20 mg orally daily, aspirin 81 mg orally daily, esomeprazole 20 mg orally daily, oxycontin 10 mg orally twice daily, lorazepam 2 mg orally 3 times daily PRN, and ondansetron 10 mg IV. On admission, his vital signs include blood pressure 105/75 mm Hg, respirations 22/min, pulse 90/min, and temperature 37.0°C (98.6°F). On his second day after admission, the patient acutely becomes obtunded. Repeat vital signs show blood pressure 85/55 mm Hg, respirations 32/min, pulse 115/min. Physical examination reveals multiple ecchymoses on the trunk and extremities and active bleeding from all IV and venipuncture sites. There is also significant erythema and swelling of the posterior aspect of the left leg. Laboratory findings are significant for thrombocytopenia, prolonged PT and PTT, and an elevated D-dimer. Blood cultures are pending. Which of the following is most likely responsible for this patient’s current condition?
- A. Factor VIII inhibitor
- B. von Willebrand disease
- C. Vitamin K deficiency
- D. Disseminated intravascular coagulation (Correct Answer)
- E. Antiphospholipid syndrome
Coagulation factor disorders Explanation: ***Disseminated intravascular coagulation***
- The patient's presentation with **acute obtundation**, **hypotension**, **tachycardia**, multiple **ecchymoses**, bleeding from venipuncture sites, and swelling of the left leg, along with laboratory findings of **thrombocytopenia**, **prolonged PT and PTT**, and **elevated D-dimer**, are all classic signs of **disseminated intravascular coagulation (DIC)**.
- DIC is a life-threatening condition often triggered by underlying conditions such as **sepsis** (indicated by fever, malaise, dyspnea, and potential infection associated with pancreatic duct stenting) or **malignancy** (pancreatic adenocarcinoma), leading to widespread uncontrolled activation of coagulation followed by consumption of clotting factors and platelets.
*Factor VIII inhibitor*
- While a **Factor VIII inhibitor** can cause bleeding and prolonged PTT, it would not typically cause **thrombocytopenia** or markedly elevated D-dimer.
- It's a rare acquired condition, usually presenting as isolated bleeding, not the systemic collapse seen here.
*von Willebrand disease*
- **Von Willebrand disease** is a genetic bleeding disorder characterized by mucocutaneous bleeding and prolonged PTT if severe, but it does **not typically cause thrombocytopenia**, normal PT, or greatly elevated D-dimer.
- The acute, severe, systemic nature of the patient's symptoms is not consistent with VWD.
*Vitamin K deficiency*
- **Vitamin K deficiency** can prolong PT and PTT, leading to bleeding, but it does **not cause thrombocytopenia** or elevated D-dimer.
- This condition is often seen in malabsorption or liver disease, and while the patient has pancreatic cancer, the specific lab abnormalities point away from isolated vitamin K deficiency.
*Antiphospholipid syndrome*
- **Antiphospholipid syndrome** typically causes **thrombotic events** (clots) rather than bleeding, although it can be associated with some thrombocytopenia.
- The patient's predominant symptoms of widespread bleeding and consumption coagulopathy are not consistent with this syndrome.
Coagulation factor disorders US Medical PG Question 5: A 2-year-old boy had increased bleeding during a circumcision. His birth and delivery were uncomplicated, and his mother had no issues with prolonged bleeding during labor. Of note, his maternal grandfather has a history of bleeding complications. The boy's vital signs are stable and physical examination is notable for scattered bruises on his lower extremities. The lab results are as follows:
Hemoglobin 12.8 gm %
Hematocrit 35.4%
WBC 8400/mm3
Platelets 215 x 109/L
PT 14 s
PTT 78 s
What is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Hemophilia A (Correct Answer)
- C. Von Willebrand disease
- D. Scurvy
- E. Bernard-Soulier syndrome
Coagulation factor disorders Explanation: ***Hemophilia A***
- The patient's presentation with increased bleeding during circumcision, scattered bruises, and a **prolonged PTT** with normal PT and platelet count is highly suggestive of **Hemophilia A**.
- The familial history of bleeding complications in the maternal grandfather points towards an **X-linked recessive inheritance pattern**, characteristic of Hemophilia A.
- Hemophilia A results from **Factor VIII deficiency**, affecting the intrinsic coagulation pathway.
*Glanzmann thrombasthenia*
- This condition involves a defect in **platelet aggregation** due to deficiency of **GPIIb/IIIa**, which would typically manifest with a **normal platelet count** but abnormal platelet function tests.
- While it causes bruising and bleeding, it would not affect the PTT, as coagulation factors are normal in this platelet function disorder.
*Von Willebrand disease*
- This is the **most common inherited bleeding disorder** and typically presents with mucocutaneous bleeding and menorrhagia in females.
- While it can cause a **mildly prolonged PTT** due to low Factor VIII levels (vWF stabilizes Factor VIII), the PTT is typically only **mildly elevated**, not as significantly prolonged as seen here (78s vs normal ~25-35s).
- The **X-linked family history** (affected maternal grandfather, not parents) strongly favors hemophilia over the **autosomal dominant** inheritance of most vWD cases.
*Scurvy*
- Scurvy results from **vitamin C deficiency** leading to impaired collagen synthesis.
- While it can cause bleeding issues like petechiae and gingival bleeding, it would not cause a **prolonged PTT** or present with significant bleeding during a circumcision.
- Coagulation tests remain normal in scurvy.
*Bernard-Soulier syndrome*
- This is a rare, inherited platelet disorder characterized by **giant platelets** and **thrombocytopenia**, resulting from a defect in the **glycoprotein Ib/IX/V complex**.
- It would present with mucocutaneous bleeding and bruising, but the patient's **platelet count is normal** (215 × 10⁹/L) and the PTT would not be prolonged in this platelet function disorder.
Coagulation factor disorders US Medical PG Question 6: A 12-year-old boy presents to the emergency department with a swollen and painful knee. He says that he was exploring with his friends when he tripped and hit his knee against the ground. He didn't feel like he hit it very hard but it started swelling and becoming very painful. His mom reports that he has always been prone to bleeding from very minor trauma and that others in the family have had similar problems. Based on clinical suspicion a coagulation panel was obtained showing a prothrombin time (PT) of 10 seconds (normal range 9-11 seconds), a partial thromboplastin time (PTT) of 45 seconds (normal 20-35 seconds), and a normal ristocetin cofactor assay (equivalent to bleeding time). Mixing tests with factor IX and XI do not show complementation, but mixing with factor VIII reverses the coagulation abnormality. Which of the following is the most likely diagnosis for this patient?
- A. Glanzmann thrombasthenia
- B. Hemophilia B
- C. von Willebrand disease
- D. Bernard-Soulier disease
- E. Hemophilia A (Correct Answer)
Coagulation factor disorders Explanation: ***Hemophilia A***
- The **prolonged PTT** that corrects with the addition of **Factor VIII** in the mixing study strongly indicates Factor VIII deficiency, which is characteristic of **Hemophilia A**.
- The history of **easy bleeding** from minor trauma and reports of similar problems in other family members also align with the **X-linked recessive inheritance** pattern and clinical presentation of Hemophilia A.
*Glanzmann thrombasthenia*
- This condition is characterized by a defect in **platelet aggregation** due to an abnormality in **glycoprotein IIb/IIIa**, which would typically manifest with a **normal PT and PTT** but an **abnormal bleeding time** (reflected by the ristocetin cofactor assay equivalent), which is not the case here.
- Patients typically present with **mucocutaneous bleeding** (e.g., epistaxis, petechiae) rather than deep joint bleeds.
*Hemophilia B*
- While Hemophilia B also causes a **prolonged PTT** and is inherited in an **X-linked recessive** pattern, the mixing study specifically showed correction with **Factor VIII**, not Factor IX, thus ruling out Hemophilia B (which is Factor IX deficiency).
- The clinical presentation of spontaneous bleeding into joints (hemarthrosis) is consistent with both Hemophilia A and B, but the specific lab findings differentiate them.
*von Willebrand disease*
- This disease typically presents with a **prolonged bleeding time** (or abnormal ristocetin cofactor assay), which was noted as normal in this patient.
- While it can cause a **mildly prolonged PTT** due to its role in stabilizing Factor VIII, the primary diagnostic indicator of an abnormal ristocetin cofactor is absent here.
*Bernard-Soulier disease*
- This is a rare **platelet disorder** characterized by large platelets and a deficiency or defect in the **glycoprotein Ib-IX-V complex**, leading to impaired platelet adhesion.
- It would typically present with a **normal PT and PTT** but a **prolonged bleeding time** (abnormal ristocetin cofactor assay), differentiating it from the findings in this case.
Coagulation factor disorders US Medical PG Question 7: A 68-year-old man comes to the emergency department 12 hours after the appearance of tender, purple discolorations on his thighs and lower abdomen. He began taking a medication 4 days ago after failed cardioversion for atrial fibrillation, but he cannot remember the name. Physical examination shows a tender bluish-black discoloration on the anterior abdominal wall. A photograph of the right thigh is shown. Which of the following is the most likely explanation for this patient's skin findings?
- A. Antibodies against platelet factor 4
- B. Increased levels of protein S
- C. Decreased synthesis of antithrombin III
- D. Reduced levels of protein C (Correct Answer)
- E. Deficiency of vitamin K
Coagulation factor disorders Explanation: **Reduced levels of protein C**
- The patient's presentation of **tender, purple discolorations** (skin necrosis) on the thighs and lower abdomen, developing a few days after starting a new medication for atrial fibrillation, is highly suspicious for **coumarin-induced skin necrosis**.
- This adverse event occurs most commonly with **warfarin (a coumarin derivative)**, especially in patients with a **pre-existing protein C deficiency** or when therapy is initiated without adequate bridging, leading to an initial procoagulant state due to the faster reduction of protein C compared to procoagulant factors.
*Antibodies against platelet factor 4*
- This condition describes **heparin-induced thrombocytopenia (HIT)**, where antibodies against platelet factor 4 (PF4) complexed with heparin lead to platelet activation, aggregation, and thrombosis.
- HIT presents with **thrombocytopenia** (which is not mentioned as present here) and thrombotic events, but typically not with the distinct skin necrosis pattern seen with warfarin.
*Increased levels of protein S*
- **Increased levels of protein S** would generally lead to a more effective anticoagulant state rather than a procoagulant state.
- **Protein S** acts as a cofactor for protein C, enhancing its anticoagulant activity. Its elevation would not explain the observed skin necrosis.
*Decreased synthesis of antithrombin III*
- **Antithrombin III deficiency** is a congenital or acquired thrombophilia that can lead to an increased risk of venous and arterial thrombosis.
- While it increases the risk of thrombosis, it does not specifically explain the unique presentation of **warfarin-induced skin necrosis** through its specific mechanism.
*Deficiency of vitamin K*
- **Vitamin K deficiency** leads to impaired synthesis of vitamin K-dependent clotting factors (II, VII, IX, X) and anticoagulant proteins (Protein C and S), often resulting in **bleeding diathesis**, not thrombotic skin necrosis.
- While warfarin works by inhibiting vitamin K epoxide reductase, a severe general deficiency of vitamin K would present differently.
Coagulation factor disorders US Medical PG Question 8: A 29-year-old woman comes to the office with the complaints of severe bleeding after a dental extraction which required local hemostatic therapy. She has a long-term excessive menstrual bleeding and iron-deficiency anemia that required treatment with iron supplement since the age of 17. In addition, she states that her mother also has a history of frequent nosebleeds. The vital signs include: pulse rate 107/min, respiratory rate 17/min, temperature 37.2°C (99.0°F), and blood pressure 90/60 mm Hg. Her physical exam shows generalized pallor.
The complete blood count results are as follows:
Hemoglobin 10.7 g/dL
Hematocrit 41%
Leukocyte count 8,000/mm3
Neutrophils 54%
Bands 3%
Eosinophils 1%
Basophils 0%
Lymphocytes 32%
Monocytes 2%
Mean corpuscular hemoglobin 25.4 pg/cell
Mean corpuscular hemoglobin concentration 31% Hb/cell
Mean corpuscular volume 76 μm3
Platelet count 380,000/mm³
The coagulation test results are as follows:
Partial thromboplastin time (activated) 48.0 s
Prothrombin time 14.0 s
International normalized ratio 0.9
What is the most likely diagnosis?
- A. Von Willebrand disease (Correct Answer)
- B. Systemic lupus erythematosus
- C. Sideroblastic anemia
- D. Congenital thrombocytopenia
- E. Hemophilia A
Coagulation factor disorders Explanation: ***Von Willebrand disease***
- This condition presents with a history of **excessive bleeding** from mucous membranes, menorrhagia, and prolonged bleeding after dental extraction, all indicative of a **primary hemostasis defect**.
- The elevated **aPTT (48.0s)** along with normal PT and platelet count, coupled with a family history of frequent nosebleeds, strongly suggests von Willebrand disease, which affects both platelet adhesion and factor VIII activity.
*Systemic lupus erythematosus*
- This is an **autoimmune disorder** that can cause various manifestations, but **bleeding disorders** are typically due to **immune thrombocytopenia** or acquired coagulopathies, neither of which is directly supported by the normal platelet count or specific coagulation profile (normal PT/INR).
- While it can cause anemia, the **microcytic anemia** presented is better explained by iron deficiency secondary to chronic blood loss.
*Sideroblastic anemia*
- This is a type of **microcytic hypochromic anemia** characterized by a defect in **heme synthesis**, leading to iron accumulation in mitochondria.
- It does not typically present with bleeding disorders or an elevated aPTT, making it an unlikely cause of the patient's primary bleeding complaints.
*Congenital thrombocytopenia*
- This condition involves a chronically **low platelet count**, which would lead to bleeding symptoms similar to this patient's.
- However, the patient's **platelet count is normal at 380,000/mm³**, ruling out a primary platelet deficiency.
*Hemophilia A*
- Hemophilia A is an **X-linked recessive disorder** primarily affecting males, characterized by a deficiency of **Factor VIII**, leading to prolonged aPTT.
- While it explains the elevated aPTT, the patient is female, and the predominant mucous membrane bleeding (menorrhagia, dental extraction bleeding) is more typical of **platelet function defects or von Willebrand disease** than the deep tissue or joint bleeds seen in hemophilia.
Coagulation factor disorders US Medical PG Question 9: A 46-year-old female with estrogen receptor positive invasive ductal carcinoma is prescribed tamoxifen. Which of the following is the MOST concerning side effect that requires patient counseling regarding potentially life-threatening complications?
- A. Increased risk of deep vein thrombosis (Correct Answer)
- B. Hot flashes and menopausal symptoms
- C. Improved bone density in postmenopausal women
- D. Increased risk of endometrial cancer
- E. Increased risk of hypertension
Coagulation factor disorders Explanation: ***Increased risk of deep vein thrombosis***
- Tamoxifen, a **selective estrogen receptor modulator (SERM)**, has estrogen receptor agonist effects in some tissues, including the coagulation system.
- This can lead to an increased risk of **thromboembolic events**, such as **deep vein thrombosis (DVT)** and **pulmonary embolism (PE)**, which are potentially life-threatening cardiovascular/hematologic complications.
*Hot flashes and menopausal symptoms*
- While tamoxifen commonly causes **hot flashes**, night sweats, and vaginal dryness due to its anti-estrogenic effects in the hypothalamus and vaginal tissue, these are generally a quality-of-life issue and not the **most concerning cardiovascular/hematologic side effect** requiring immediate intervention or counseling regarding life-threatening complications.
- These symptoms are usually manageable and anticipated but do not pose the same acute danger as a thromboembolic event.
*Improved bone density in postmenopausal women*
- Tamoxifen has **estrogen-agonist effects on bone**, leading to improved bone mineral density in postmenopausal women.
- This is generally considered a **beneficial side effect** rather than a concerning one, especially in women at risk for osteoporosis.
*Increased risk of hypertension*
- While cardiovascular side effects can occur with tamoxifen, a significantly increased risk of **hypertension** is not one of its primary or most concerning cardiovascular/hematologic complications.
- Blood pressure needs to be monitored, but DVT/PE risk is a far greater concern.
*Increased risk of endometrial cancer*
- Tamoxifen has **estrogen-agonist effects on the endometrium**, increasing the risk of **endometrial hyperplasia** and **endometrial cancer**.
- While this is a serious and well-known side effect that requires patient counseling and monitoring, it is an oncologic complication, not a cardiovascular or hematologic one.
Coagulation factor disorders US Medical PG Question 10: A 35-year-old patient is brought into the emergency department post motor vehicle crash. Stabilization of the patient in the trauma bay requires endotracheal intubation. The patient has a laceration on the femoral artery from shrapnel and seems to have lost large quantities of blood. The patient is transfused with 13 units of packed red blood cells. His vitals are T 96.5, HR 150, BP 90/40. Even with the direct pressure on the femoral artery, the patient continues to bleed. Results of labs drawn within the last hour are pending. Which of the following is most likely to stop the bleeding in this patient?
- A. Normal saline
- B. Fresh frozen plasma and platelets (Correct Answer)
- C. Whole blood
- D. Dextrose
- E. Cryoprecipitate
Coagulation factor disorders Explanation: ***Fresh frozen plasma and platelets***
- This patient is experiencing **dilutional coagulopathy** due to massive transfusion of packed red blood cells, which lack clotting factors and platelets.
- **Fresh frozen plasma (FFP)** provides essential clotting factors, while **platelets** directly address thrombocytopenia, both crucial for **hemostasis**.
- This represents **standard component therapy** readily available in emergency departments.
*Normal saline*
- Administering normal saline would further dilute the remaining clotting factors and platelets, potentially **worsening the coagulopathy**.
- While essential for **volume resuscitation**, it does not provide any clotting components needed to stop bleeding.
*Whole blood*
- While **whole blood** contains red blood cells, plasma, and platelets in physiologic ratios, it is **not readily available** in most civilian trauma centers.
- Modern practice uses **component therapy** (FFP + platelets + PRBCs) which is more widely accessible and allows for targeted resuscitation.
- Low-titer O whole blood programs exist in some centers but are not universally available.
*Dextrose*
- **Dextrose solutions** primarily provide free water and glucose, used for hydration and hypoglycemia.
- It has **no hemostatic properties** and would further dilute clotting factors, exacerbating the bleeding.
*Cryoprecipitate*
- **Cryoprecipitate** is rich in **fibrinogen, factor VIII, factor XIII, and von Willebrand factor**.
- While useful for specific factor deficiencies or when fibrinogen is critically low in massive transfusions, it **does not replace all clotting factors or platelets** comprehensively as FFP and platelets would.
- Typically used as **adjunctive therapy** when fibrinogen levels are known to be low.
More Coagulation factor disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.