Anticoagulation management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anticoagulation management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anticoagulation management US Medical PG Question 1: A 43-year-old woman was admitted to the hospital for anticoagulation following a pulmonary embolism. She was found to have a deep venous thrombosis on further workup after a long plane ride coming back from visiting China. She denies any personal history of blood clots in her past, but she says that her mother has also had to be treated for pulmonary embolism in the recent past. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and she currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min, and respiratory rate 23/min. On physical examination, her pulses are bounding and complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 81% on room air, with a new oxygen requirement of 8 L by face mask. On day 6 of combined heparin and warfarin anticoagulation, her platelet count decreases from 182,000/mcL to 63,000/mcL. Her international normalized ratio (INR) is not yet therapeutic. What is the next best step in therapy?
- A. Continue heparin and warfarin until INR is therapeutic for 24 hours
- B. Discontinue heparin and warfarin (Correct Answer)
- C. Continue heparin and warfarin, and administer vitamin K
- D. Discontinue heparin; continue warfarin
- E. Continue heparin; discontinue warfarin
Anticoagulation management Explanation: ***Discontinue heparin and warfarin***
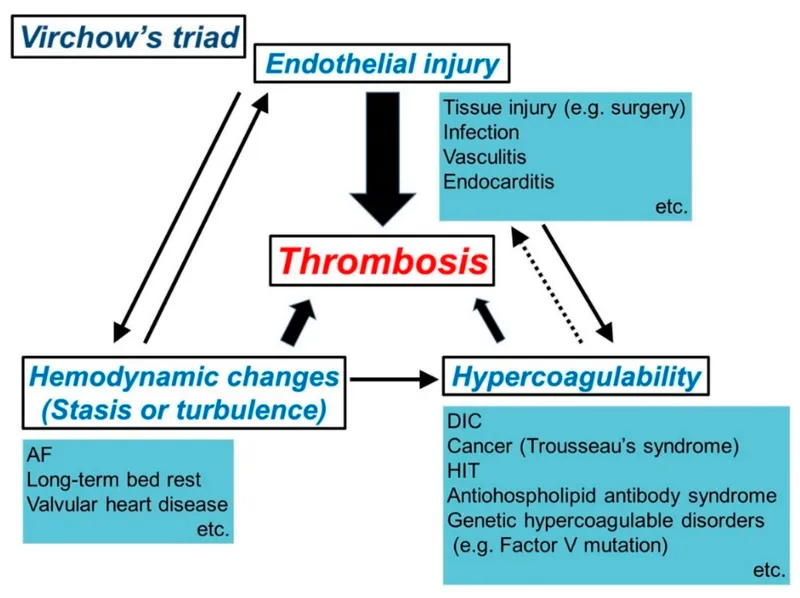
- The significant drop in platelet count (from 182,000 to 63,000/mcL) on day 6 of heparin therapy strongly suggests **heparin-induced thrombocytopenia (HIT)**, an immune-mediated adverse drug reaction.
- **Immediate management requires:** (1) discontinuation of ALL heparin products, and (2) initiation of an alternative non-heparin anticoagulant such as a direct thrombin inhibitor (argatroban, bivalirudin) or fondaparinux.
- Warfarin must NOT be continued as monotherapy in HIT because it causes transient **hypercoagulability** due to depletion of protein C and S before depleting clotting factors, which can worsen thrombotic complications.
- **Among the options provided**, discontinuing both heparin and warfarin is the correct first step, with the understanding that alternative anticoagulation would be initiated immediately in practice.
*Continue heparin and warfarin until INR is therapeutic for 24 hours*
- Continuing heparin would be dangerous given the suspected **HIT**, as it could lead to further platelet activation, worsening thrombocytopenia, and an increased risk of **paradoxical thrombosis**.
- While achieving therapeutic anticoagulation is important for PE/DVT, the priority is managing the acute, life-threatening complication of HIT.
*Continue heparin and warfarin, and administer vitamin K*
- Administering vitamin K would reverse warfarin effects, which is contraindicated in a patient requiring anticoagulation for PE and DVT unless there is active bleeding or supratherapeutic INR.
- Continuing heparin in the setting of suspected **HIT** is contraindicated and would exacerbate the prothrombotic state.
*Discontinue heparin; continue warfarin*
- While discontinuing heparin is correct in suspected **HIT**, continuing warfarin alone is **dangerous** and contraindicated.
- Warfarin monotherapy in acute HIT causes transient **hypercoagulability** due to rapid depletion of protein C and S (shorter half-lives) before depletion of clotting factors II, IX, and X, leading to increased thrombotic risk including **warfarin-induced venous limb gangrene**.
- An **alternative non-heparin anticoagulant** (direct thrombin inhibitor or fondaparinux) must be initiated before warfarin can be safely restarted.
*Continue heparin; discontinue warfarin*
- Continuing heparin in the presence of a rapid and significant drop in platelet count is **contraindicated** due to the high suspicion of **HIT**.
- Discontinuing warfarin alone would leave the patient exposed to continued HIT complications while still receiving the offending agent (heparin).
Anticoagulation management US Medical PG Question 2: A 66-year-old man with coronary artery disease and hypertension comes to the emergency department because of intermittent retrosternal chest pain, lightheadedness, and palpitations. He has smoked one pack of cigarettes daily for 39 years. His pulse is 140/min and irregularly irregular, respirations are 20/min, and blood pressure is 108/60 mm Hg. An ECG shows an irregular, narrow-complex tachycardia with absent P waves. A drug with which of the following mechanisms of action is most likely to be effective in the long-term prevention of embolic stroke in this patient?
- A. Irreversible inhibition of cyclooxygenase
- B. Interference with carboxylation of glutamate residues (Correct Answer)
- C. Binding and activation of antithrombin III
- D. Irreversible blockade of adenosine diphosphate receptors
- E. Activation of the conversion of plasminogen to plasmin
Anticoagulation management Explanation: ***Interference with carboxylation of glutamate residues***
- The patient's presentation with **irregularly irregular pulse**, **narrow-complex tachycardia**, and **absent P waves** on ECG is highly suggestive of **atrial fibrillation**.
- **Atrial fibrillation** increases the risk of **thromboembolic stroke**, and long-term prevention requires **anticoagulation**.
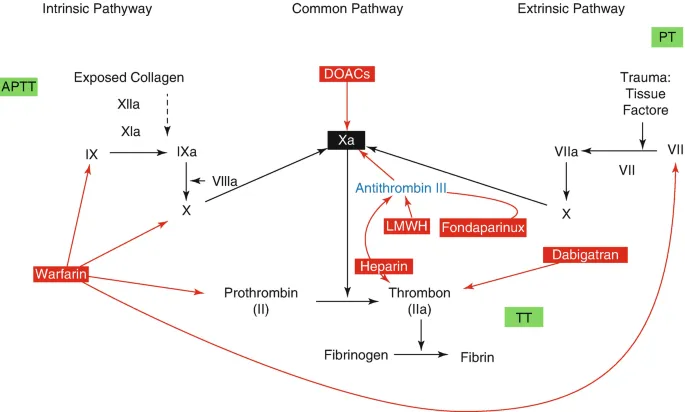
- This mechanism describes **warfarin**, a vitamin K antagonist that inhibits the **carboxylation of glutamate residues** in clotting factors (II, VII, IX, X), preventing their activation.
- While **direct oral anticoagulants (DOACs)** are now often preferred as first-line therapy, warfarin remains an effective and widely used option for stroke prevention in atrial fibrillation, particularly when DOACs are contraindicated or unavailable.
*Irreversible inhibition of cyclooxygenase*
- This mechanism describes **aspirin**, an **antiplatelet agent**.
- While aspirin provides some cardiovascular protection, it is **significantly less effective than anticoagulants** like warfarin or DOACs for stroke prevention in patients with atrial fibrillation.
- Antiplatelet agents alone are generally reserved for patients who cannot tolerate anticoagulation.
*Binding and activation of antithrombin III*
- This mechanism is characteristic of **unfractionated heparin** and **low molecular weight heparins (LMWH)**.
- These agents are primarily used for **acute anticoagulation** (e.g., bridging therapy) and require parenteral administration.
- They are not suitable for long-term oral stroke prevention in atrial fibrillation.
*Irreversible blockade of adenosine diphosphate receptors*
- This mechanism describes **P2Y12 inhibitors** like clopidogrel, prasugrel, and ticagrelor, which are **antiplatelet agents**.
- Like aspirin, P2Y12 inhibitors are **not sufficient as monotherapy** for stroke prevention in atrial fibrillation.
- They are more commonly used in acute coronary syndromes, after percutaneous coronary intervention, or in dual antiplatelet therapy.
*Activation of the conversion of plasminogen to plasmin*
- This mechanism describes **thrombolytic agents** (e.g., tissue plasminogen activator - tPA, alteplase), which are used to **dissolve existing clots** in acute scenarios like ischemic stroke or ST-elevation myocardial infarction.
- They are not used for long-term prevention of embolic stroke due to their **significant bleeding risk** and lack of prophylactic benefit.
Anticoagulation management US Medical PG Question 3: A 21-year-old woman comes to the physician because of a 1-day history of right leg pain. The pain is worse while walking and improves when resting. Eight months ago, she was diagnosed with a pulmonary embolism and was started on warfarin. Anticoagulant therapy was discontinued two months ago. Her mother had systemic lupus erythematosus. On examination, her right calf is diffusely erythematous, swollen, and tender. Cardiopulmonary examination shows no abnormalities. On duplex ultrasonography, the right popliteal vein is not compressible. Laboratory studies show an elevated serum level of D-dimer and insensitivity to activated protein C. Further evaluation of this patient is most likely to show which of the following?
- A. Deficiency of protein C
- B. Protein S deficiency
- C. Elevated coagulation factor VIII levels
- D. Mutation of coagulation factor V (Correct Answer)
- E. Mutation of prothrombin
Anticoagulation management Explanation: ***Mutation of coagulation factor V***
- The patient's history of **recurrent DVT/PE** at a young age, family history of autoimmune disease (mother's SLE), and laboratory finding of **insensitivity to activated protein C** strongly point towards **Factor V Leiden mutation**.
- This mutation makes **Factor V resistant to inactivation** by activated protein C, leading to a hypercoagulable state and increased risk of venous thromboembolism.
*Deficiency of protein C*
- While it also causes **insensitivity to activated protein C** and a hypercoagulable state, a true deficiency of protein C would lead to quantitative reduction, not primarily functional insensitivity.
- Protein C deficiency can cause **severe thrombotic events**, but the given lab finding of "insensitivity to activated protein C" points more directly to a defect in Factor V.
*Protein S deficiency*
- **Protein S** acts as a cofactor for activated protein C, so its deficiency would also impair the anticoagulant pathway and could lead to thrombosis.
- However, **Protein S deficiency** does not directly cause "insensitivity to activated protein C" as the primary defect; rather, it reduces the effectiveness of activated protein C.
*Elevated coagulation factor VIII levels*
- **High levels of Factor VIII** are a risk factor for VTE, but this condition would not lead to **insensitivity to activated protein C**.
- While it contributes to a hypercoagulable state, it's a distinct mechanism not indicated by the specific lab finding mentioned.
*Mutation of prothrombin*
- **Prothrombin G20210A mutation** (mutation of prothrombin) leads to increased prothrombin levels and increased thrombin generation, predisposing to thrombosis.
- However, this mutation would not result in **insensitivity to activated protein C**, which is the key laboratory finding in this patient.
Anticoagulation management US Medical PG Question 4: A 28-year-old woman, gravida 1, para 0, at 32 weeks' gestation is evaluated for vaginal bleeding. Five days ago, she was admitted to the hospital and started on treatment for a deep vein thrombosis in the right leg. Her pulse is 125/min and blood pressure is 95/67 mm Hg. Physical examination shows large hematomas on the upper limbs and swelling in the right calf. There is a large amount of bright red blood in the vaginal vault. Laboratory studies show a hemoglobin of 8.9 mg/dL, platelet count of 185,000/mm3, and activated partial thromboplastin time of 160 seconds. Which of the following is the most appropriate pharmacotherapy to rapidly reverse this patient's coagulopathy?
- A. Vitamin K
- B. Prothrombin complex concentrate
- C. Fresh frozen plasma
- D. Protamine sulfate (Correct Answer)
- E. Alteplase
Anticoagulation management Explanation: ***Protamine sulfate***
- The patient's prolonged **aPTT (160 seconds)**, combined with recent treatment for DVT, strongly suggests **heparin overdose** or sensitivity.
- **Protamine sulfate** is the specific antidote for **heparin**, forming a stable salt that neutralizes its anticoagulant effect.
*Vitamin K*
- **Vitamin K** is the antidote for **warfarin** and helps in the synthesis of clotting factors II, VII, IX, and X.
- It would not reverse the effects of **heparin**, which works by activating antithrombin and inhibiting thrombin and factor Xa.
*Prothrombin complex concentrate*
- **PCC** contains factors II, VII, IX, and X and is used to rapidly reverse the effects of **warfarin** or in cases of severe bleeding due to factor deficiencies.
- While it could theoretically help with general coagulopathy, it is not the specific or most direct antagonist for **heparin**.
*Fresh frozen plasma*
- **FFP** contains all coagulation factors and is used for broad reversal of coagulopathy, especially in cases of **liver disease**, DIC, or multiple factor deficiencies.
- While it could provide factors, it would not directly antagonize the high levels of **heparin** that are likely causing the bleeding.
*Alteplase*
- **Alteplase** is a **thrombolytic agent** used to break down existing blood clots by converting plasminogen to plasmin.
- Administering alteplase would worsen the patient's severe bleeding and is contraindicated in this scenario.
Anticoagulation management US Medical PG Question 5: A 68-year-old man undergoes successful mechanical prosthetic aortic valve replacement for severe aortic valve stenosis. After the procedure, he is started on an oral medication and instructed that he should take for the rest of his life and that he should avoid consuming large amounts of dark-green, leafy vegetables. Which of the following laboratory parameters should be regularly monitored to guide dosing of this drug?
- A. D-dimer
- B. Anti-factor Xa activity
- C. Activated partial thromboplastin time
- D. Prothrombin time (Correct Answer)
- E. Thrombin time
Anticoagulation management Explanation: ***Prothrombin time***
- **Warfarin** is the standard chronic anticoagulant post-mechanical valve replacement, and its dosing is monitored using the **prothrombin time (PT)**, reported as the **International Normalized Ratio (INR)**.
- The avoidance of dark-green, leafy vegetables indicates a **Vitamin K antagonist**, which is warfarin.
*D-dimer*
- **D-dimer** levels are primarily used to rule out **venous thromboembolism (VTE)** and are not used for routine monitoring of chronic anticoagulation.
- Elevated D-dimer indicates recent or ongoing **fibrinolysis**, which is not directly targeted by warfarin therapy.
*Anti-factor Xa activity*
- **Anti-factor Xa activity** is used to monitor the anticoagulant effect of **low molecular weight heparins (LMWH)** or **direct oral anticoagulants (DOACs)** like rivaroxaban or apixaban.
- This patient is on a vitamin K antagonist, not an anti-Xa inhibitor.
*Activated partial thromboplastin time*
- The **activated partial thromboplastin time (aPTT)** is used to monitor patients receiving **unfractionated heparin**, not warfarin.
- While both heparin and warfarin are anticoagulants, they act on different parts of the coagulation cascade and are monitored differently.
*Thrombin time*
- **Thrombin time (TT)** measures the time it takes for plasma to clot after adding thrombin, and it is primarily used to detect inherited or acquired **fibrinogen disorders** or to monitor **direct thrombin inhibitors**.
- It is not routinely used for monitoring warfarin therapy.
Anticoagulation management US Medical PG Question 6: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
Anticoagulation management Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
Anticoagulation management US Medical PG Question 7: A 74-year-old man presents to the emergency department with shortness of breath that started about 30 minutes ago. He is also experiencing chest pain on deep inspiration. He has several significant medical conditions including chronic obstructive pulmonary disease, hypertension, and dyslipidemia. He used to smoke about 3 packs of cigarettes every day until last year when he quit. He was in the emergency room 2 weeks ago for a hemorrhagic stroke which was promptly treated. He currently weighs 97.5 kg (215 lb). His respirations are 20/min, the blood pressure is 110/80 mm Hg, and the pulse is 105/min. On physical examination, Homan's sign is positive. An ECG and chest X-ray are performed. His current oxygen saturation is at 87% and D-dimer results are positive. He is wheeled in for a CT scan. What is the most appropriate initial treatment for this patient?
- A. Subcutaneous fondaparinux
- B. Greenfield filter (Correct Answer)
- C. Surgical thrombectomy
- D. Unfractionated heparin
- E. Warfarin
Anticoagulation management Explanation: ***Greenfield filter (IVC filter)***
- This patient presents with **acute pulmonary embolism (PE)** evidenced by sudden **shortness of breath**, **pleuritic chest pain**, **tachycardia (105/min)**, **hypoxemia (87%)**, and **positive D-dimer**. The positive **Homan's sign** suggests deep vein thrombosis as the source.
- The critical factor is his **recent hemorrhagic stroke 2 weeks ago**, which represents an **absolute contraindication to anticoagulation** in the acute/subacute period due to the high risk of re-bleeding.
- **IVC filter placement** is specifically indicated for patients with **venous thromboembolism (VTE) who have contraindications to anticoagulation**, which precisely describes this clinical scenario.
- The filter prevents further emboli from reaching the lungs while avoiding the bleeding risks associated with anticoagulants.
*Subcutaneous fondaparinux*
- While **fondaparinux** is a factor Xa inhibitor commonly used for PE treatment, it is still an **anticoagulant** that significantly increases bleeding risk.
- A **recent hemorrhagic stroke (2 weeks ago)** is an **absolute contraindication** to any form of anticoagulation, including fondaparinux, due to the substantial risk of intracranial re-bleeding.
- Standard guidelines recommend avoiding anticoagulation for at least 2-4 weeks (often longer) after intracranial hemorrhage.
*Unfractionated heparin*
- **Unfractionated heparin (UFH)** is a standard treatment for acute PE but is absolutely **contraindicated** in this patient due to the **recent hemorrhagic stroke**.
- UFH would carry an unacceptable risk of causing recurrent intracranial bleeding in the subacute post-stroke period.
*Surgical thrombectomy*
- **Surgical embolectomy** is reserved for patients with **massive PE causing hemodynamic instability** (cardiogenic shock, persistent hypotension) who have failed or have contraindications to thrombolysis.
- This patient is **hemodynamically stable** with a blood pressure of 110/80 mmHg, making surgical intervention unnecessarily invasive and inappropriate as initial management.
*Warfarin*
- **Warfarin** is an oral anticoagulant used for long-term VTE management but has a **slow onset of action** (requires 5-7 days to reach therapeutic levels), making it unsuitable for acute PE treatment.
- More importantly, like all anticoagulants, warfarin is **absolutely contraindicated** in this patient due to the recent hemorrhagic stroke and high re-bleeding risk.
Anticoagulation management US Medical PG Question 8: A 30-year-old man with history of intravenous drug use and methamphetamine-associated chronic thromboembolic pulmonary hypertension (CTEPH) is brought to the emergency department by his girlfriend for worsening abdominal pain and fevers. The patient said the pain was initially around his umbilicus, but he is now experiencing intense tenderness near his groin. He was initially prescribed rivaroxaban, but due to insurance issues, he was switched to warfarin for management of CTEPH two weeks ago. His temperature is 102°F (38.9°C), blood pressure is 95/60 mmHg, pulse is 95/min, respirations are 22/min. He states that his blood pressure usually runs low. His physical exam is notable for an unremarkable cardiac exam, bibasilar crackles, and RLQ tenderness with rebound tenderness when the LLQ is palpated. Laboratory results are shown below:
Hemoglobin: 11 g/dL
Hematocrit: 35 %
Leukocyte count: 16,000/mm^3 with normal differential
Platelet count: 190,000/mm^3
Serum:
Na+: 137 mEq/L
Cl-: 100 mEq/L
K+: 3.7 mEq/L
HCO3-: 23 mEq/L
BUN: 40 mg/dL
Glucose: 110 mg/dL
Creatinine: 0.8 mg/dL
Ca2+: 9.1 mg/dL
AST: 34 U/L
ALT: 45 U/L
International normalized ratio (INR): 6.2
Prothrombin time (PT): 40 seconds
Partial thromboplastin time: 70 seconds
Blood type: O
Rhesus: Positive
Antibody screen: Negative
A clinical diagnosis is made and supported by the surgical consult team in lieu of imaging. The next operating room for an add-on procedure will not be available for another 5 hours. Appropriate medical therapy is initiated. What is the best next step for surgical optimization?
- A. Fresh frozen plasma
- B. Prothrombin complex concentrate (Correct Answer)
- C. Protamine
- D. Do nothing
- E. Phytonadione
Anticoagulation management Explanation: ***Prothrombin complex concentrate***
- The patient has **warfarin over-anticoagulation (INR 6.2)** and requires **emergency surgery** for suspected appendicitis with peritonitis, necessitating rapid reversal of anticoagulation.
- **Prothrombin complex concentrate (4-factor PCC)** contains concentrated factors II, VII, IX, and X (and proteins C & S), providing **rapid and complete reversal** of warfarin's anticoagulant effects within minutes, which is crucial in emergency surgical situations.
- PCC is **preferred over FFP** per current guidelines (ACCP, AHA) for urgent warfarin reversal due to faster administration, smaller volume, and more predictable INR correction.
- **Vitamin K should be administered concurrently** to provide sustained reversal (takes 12-24 hours), but PCC is essential for immediate correction before surgery.
*Fresh frozen plasma*
- While FFP contains all coagulation factors and can reverse warfarin, it requires **larger volumes (4-6 units)**, takes longer to thaw and administer, and is **less effective** in rapidly correcting INR to normal range compared to PCC.
- Administering large volumes of FFP can lead to **volume overload** (especially concerning in CTEPH patients) and **transfusion-related complications**.
- PCC is superior for urgent reversal in patients requiring emergency surgery.
*Protamine*
- **Protamine** is used to reverse the anticoagulant effects of **unfractionated heparin** (and partially reverses low molecular weight heparin), not warfarin.
- It would have **no effect** on the patient's elevated INR due to warfarin use.
- Note: The elevated PTT (70s) in this case may suggest concurrent heparin bridging therapy or other factor deficiency, but the primary issue requiring reversal is the critical warfarin over-anticoagulation.
*Do nothing*
- This patient has **surgical peritonitis** (appendicitis with peritoneal signs) and requires emergency surgery with an INR of 6.2, creating **high risk of surgical bleeding**.
- Proceeding to surgery without reversing anticoagulation would result in **life-threatening hemorrhage**.
- Delaying treatment would likely result in further **clinical deterioration** with possible perforation and sepsis.
*Phytonadione*
- **Phytonadione (Vitamin K)** reverses warfarin's effects by restoring hepatic synthesis of vitamin K-dependent clotting factors, but its onset of action is **slow (12-24 hours for full effect)**, making it unsuitable as the sole agent for immediate reversal in patients requiring emergent surgery.
- While **Vitamin K should be administered** alongside PCC to provide sustained reversal, it is **not sufficient alone** for rapid correction in surgical emergencies.
Anticoagulation management US Medical PG Question 9: A 52-year-old man who was recently hospitalized with a pulmonary embolism is put on an unfractionated heparin drip as a bridge to chronic warfarin therapy. During morning rounds, he is found to have diffuse bruising despite minimal trauma, and his heparin infusion rate is found to be faster than prescribed. A coagulation panel is obtained, which shows a aPTT of 130 seconds (therapeutic 70-120 seconds), and the decision is made to reverse the effects of heparin. Which of the following would most likely be administered in order to do this?
- A. Vitamin K
- B. Fresh frozen plasma
- C. Protamine sulfate (Correct Answer)
- D. Platelets
- E. Aminocaproic acid
Anticoagulation management Explanation: ***Correct: Protamine sulfate***
- **Specific reversal agent for heparin** via ionic binding (positively charged protamine neutralizes negatively charged heparin)
- Rapidly reverses anticoagulant effects within minutes
- Dose: 1 mg protamine per 100 units of heparin (titrated based on time since last dose)
- **Indicated for heparin overdose** with bleeding or need for urgent reversal
*Incorrect: Vitamin K*
- Reverses **warfarin**, not heparin
- Warfarin inhibits vitamin K-dependent clotting factors (II, VII, IX, X)
- Takes hours to work (requires synthesis of new clotting factors)
*Incorrect: Fresh frozen plasma*
- Contains clotting factors for **warfarin reversal** or coagulopathy from factor deficiency
- Not specific for heparin overdose
- Would be used if protamine fails or for complex coagulopathy
*Incorrect: Platelets*
- Used for thrombocytopenia or platelet dysfunction
- Does not reverse anticoagulant effects of heparin
- This patient has normal platelet function; issue is excessive anticoagulation
*Incorrect: Aminocaproic acid*
- Antifibrinolytic agent that inhibits plasminogen activation
- Used for hyperfibrinolysis (e.g., after thrombolytic therapy)
- Does not reverse heparin's effect on the coagulation cascade
Anticoagulation management US Medical PG Question 10: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Anticoagulation management Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
More Anticoagulation management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.