Anemia of chronic disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anemia of chronic disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anemia of chronic disease US Medical PG Question 1: A 78-year-old man presents with fatigue and exertional dyspnea. The patient says that symptoms onset gradually 4 weeks ago and have not improved. He denies any history of anemia or nutritional deficiency. Past medical history is significant for ST-elevation myocardial infarction 6 months ago, status post coronary artery bypass graft, complicated by recurrent hemodynamically unstable ventricular tachycardia. Current medications are rosuvastatin, aspirin, and amiodarone. His blood pressure is 100/70 mm Hg, the pulse is 71/min, the temperature is 36.5°C (97.7°F), and the respiratory rate is 16/min. On physical examination, patient appears lethargic and tired. Skin is dry and coarse, and there is generalized pitting edema present. A complete blood count (CBC) and a peripheral blood smear show evidence of normochromic, normocytic anemia. Additional laboratory tests reveal decreased serum level of iron, decreased TIBC (total iron-binding capacity) and increased serum level of ferritin. Which of the following is the most likely etiology of the anemia in this patient?
- A. Iron deficiency anemia
- B. Thalassemia
- C. Pernicious anemia
- D. Anemia of chronic disease (Correct Answer)
- E. Hemolytic anemia
Anemia of chronic disease Explanation: ***Anemia of chronic disease***
- The patient's history of **ST-elevation myocardial infarction** and **ventricular tachycardia**, combined with his current medications and symptoms, points to an underlying chronic inflammatory state.
- Lab findings of **normochromic, normocytic anemia**, **decreased serum iron**, **decreased total iron-binding capacity (TIBC)**, and **increased ferritin** are classic for anemia of chronic disease.
*Iron deficiency anemia*
- This condition is characterized by **decreased serum iron**, **increased TIBC**, and **decreased ferritin**, which is inconsistent with this patient's labs.
- The patient denies any history of anemia or nutritional deficiency, and no sources of blood loss are mentioned despite the use of **aspirin**.
*Thalassemia*
- Thalassemia typically presents with **microcytic, hypochromic anemia**, which contradicts the patient's **normocytic, normochromic anemia**.
- It is a genetic disorder usually identified earlier in life, unlike this patient's gradual onset of symptoms in old age.
*Pernicious anemia*
- Pernicious anemia is a type of **macrocytic anemia** (due to B12 deficiency), which is inconsistent with the patient's **normocytic anemia**.
- It would typically involve **neurological symptoms** and **megaloblastic changes** on a peripheral smear, none of which are reported.
*Hemolytic anemia*
- Hemolytic anemia is characterized by evidence of **red blood cell destruction**, such as elevated reticulocyte count, increased LDH, decreased haptoglobin, and increased indirect bilirubin, none of which are mentioned.
- The patient's history and lab findings are not typical for a primary hemolytic process.
Anemia of chronic disease US Medical PG Question 2: A 39-year-old woman presents with progressive weakness, exercise intolerance, and occasional dizziness for the past 3 months. Past medical history is unremarkable. She reports an 18-pack-year smoking history and drinks alcohol rarely. Her vital signs include: temperature 36.6°C (97.8°F), blood pressure 139/82 mm Hg, pulse 98/min. Physical examination is unremarkable. Her laboratory results are significant for the following:
Hemoglobin 9.2 g/dL
Erythrocyte count 2.1 million/mm3
Mean corpuscular volume (MCV) 88 μm3
Mean corpuscular hemoglobin (MCH) 32 pg/cell
Leukocyte count 7,500/mm3
Which of the following is the best next step in the management of this patient’s condition?
- A. Serum ferritin level
- B. Direct antiglobulin test
- C. C-reactive protein (CRP)
- D. Bone marrow biopsy
- E. Reticulocyte count (Correct Answer)
Anemia of chronic disease Explanation: ***Reticulocyte count***
- A **normocytic anemia** (MCV 88) with signs of weakness and exercise intolerance requires evaluation of **red blood cell production**.
- A reticulocyte count helps differentiate between **hypoproliferative** (low count) and **hyperproliferative** (high count) anemias, guiding further diagnostic steps.
*Serum ferritin level*
- While often low in **iron-deficiency anemia**, this patient’s **normocytic MCV** makes iron deficiency less likely as the primary cause without other features.
- A normal ferritin doesn't rule out other causes of anemia, and a high ferritin could indicate **anemia of chronic disease**, but further understanding of RBC production is needed first.
*Direct antiglobulin test*
- This test is used to diagnose **autoimmune hemolytic anemia**, which typically presents with **jaundice**, **splenomegaly**, and elevated **lactate dehydrogenase (LDH)**, none of which are noted here.
- While anemia can result from hemolysis, the initial presentation doesn't strongly suggest an immune-mediated destruction process, and determining the bone marrow's response is more immediate.
*C-reactive protein (CRP)*
- CRP is a marker of **inflammation**, and elevated levels could suggest **anemia of chronic disease**.
- However, knowing the **reticulocyte count** will provide more direct information about bone marrow function, which is crucial for characterizing the anemia.
*Bone marrow biopsy*
- A bone marrow biopsy is an **invasive procedure** typically reserved for complex anemias where initial, less invasive tests have failed to provide a diagnosis or when conditions like **aplastic anemia** or **myelodysplastic syndromes** are strongly suspected.
- It is not the appropriate **first diagnostic step** in evaluating an undifferentiated normocytic anemia like this.
Anemia of chronic disease US Medical PG Question 3: A 55-year-old woman presents with fatigue. She says her symptoms are present throughout the day and gradually started 4 months ago. Her past medical history is significant for rheumatoid arthritis–treated with methotrexate, and diabetes mellitus type 2–treated with metformin. The patient is afebrile, and her vital signs are within normal limits. A physical examination reveals pallor of the mucous membranes. Initial laboratory tests show hemoglobin of 7.9 g/dL, hematocrit of 22%, and mean corpuscular volume of 79 fL. Which of the following is the best next diagnostic step in this patient?
- A. Serum ferritin level and total iron-binding capacity (TIBC)
- B. Serum ferritin and serum iron levels
- C. Serum ferritin and soluble transferrin receptor levels (Correct Answer)
- D. Serum iron level
- E. Serum ferritin level
Anemia of chronic disease Explanation: ***Serum ferritin and soluble transferrin receptor levels***
- This patient has **anemia** (hemoglobin 7.9 g/dL) with **microcytic** (MCV 79 fL) and **hypochromic** features, suggesting either **iron deficiency anemia (IDA)** or **anemia of chronic disease (ACD)**. Given her history of **rheumatoid arthritis**, ACD is highly likely, but co-existing IDA needs to be excluded.
- **Serum ferritin** is an acute-phase reactant, so it can be elevated in ACD masking a co-existing iron deficiency. **Soluble transferrin receptor (sTfR)** levels are increased in IDA and remain normal or only mildly elevated in ACD, making it a reliable marker to differentiate between these two conditions when ferritin is uninterpretable due to inflammation.
*Serum ferritin level and total iron-binding capacity (TIBC)*
- While these tests are useful for diagnosing iron deficiency, **ferritin** can be falsely elevated in the context of inflammation (e.g., from **rheumatoid arthritis**), making it unreliable for diagnosing IDA in this patient.
- **TIBC** can be decreased in ACD, complicating its interpretation for IDA when inflammation is present.
*Serum ferritin and serum iron levels*
- As mentioned, **serum ferritin** is an acute-phase reactant and may be elevated due to **rheumatoid arthritis**, potentially masking **iron deficiency**.
- **Serum iron levels** fluctuate significantly and are not a reliable standalone indicator for iron status, especially in the context of chronic disease.
*Serum iron level*
- **Serum iron levels** are highly variable and not sufficient for diagnosing **iron deficiency** or differentiating it from **anemia of chronic disease**.
- A low serum iron can be seen in both IDA and ACD but does not provide definitive diagnostic information on its own.
*Serum ferritin level*
- Measuring **serum ferritin** alone is insufficient because it is an **acute-phase reactant** that can be elevated due to the patient's **rheumatoid arthritis**, even if she has co-existing **iron deficiency anemia**.
- A normal or high ferritin level in this context does not rule out **iron deficiency**.
Anemia of chronic disease US Medical PG Question 4: A 63-year-old man with a history of stage 4 chronic kidney disease (CKD) has started to develop refractory anemia. He denies any personal history of blood clots in his past, but he says that his mother has also had to be treated for deep venous thromboembolism in the past. His past medical history is significant for diabetes mellitus type 2, hypertension, non-seminomatous testicular cancer, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and he currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 17/min. On physical examination, the pulses are bounding, the complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air, with a new oxygen requirement of 2 L by nasal cannula. His primary care physician refers him to a hematologist, who is considering initiating the erythropoietin-stimulating agent (ESA), darbepoetin. Which of the following is true regarding the use of ESA?
- A. ESAs show efficacy with low iron levels
- B. ESAs can improve survival in patients with breast and cervical cancers
- C. ESAs are generally initiated when the hemoglobin level is < 10 g/dL (Correct Answer)
- D. The highest-tolerated dose should be used in patients with chronic kidney disease
- E. ESAs are utilized in patients receiving myelosuppressive chemotherapy with an anticipated curative outcome
Anemia of chronic disease Explanation: ***ESAs are generally initiated when the hemoglobin level is < 10 g/dL***
- Clinical guidelines recommend **considering** erythropoietin-stimulating agents (ESAs) when the hemoglobin level falls below **10 g/dL** to manage anemia in chronic kidney disease, balancing benefits and risks.
- Using ESAs at higher hemoglobin targets (e.g., >11.5 g/dL) has been associated with increased risks of **cardiovascular events**, **stroke**, and **thrombosis**.
- Treatment decisions should be individualized, considering symptoms, transfusion requirements, and patient preferences.
*ESAs show efficacy with low iron levels*
- **Iron deficiency** is a common cause of **ESA hyporesponsiveness**, meaning ESAs are less effective when iron stores are low.
- Adequate **iron supplementation** is crucial before and during ESA therapy to maximize treatment efficacy and reduce the required ESA dose.
*ESAs can improve survival in patients with breast and cervical cancers*
- ESAs have shown **no survival benefit** and may even worsen outcomes in patients with certain cancers, including **breast** and **cervical cancers**.
- Their use in cancer patients is generally restricted to managing **chemotherapy-induced anemia** to avoid transfusions, not to improve cancer-specific survival.
*The highest-tolerated dose should be used in patients with chronic kidney disease*
- The goal in CKD patients is to use the **lowest effective ESA dose** to achieve and maintain a hemoglobin level sufficient to avoid transfusions, typically between 10 and 11.5 g/dL.
- Using the highest-tolerated dose is **not recommended** due to increased risks of cardiovascular events, stroke, and **thromboembolism**.
*ESAs are utilized in patients receiving myelosuppressive chemotherapy with an anticipated curative outcome*
- ESAs are generally **contraindicated** in patients receiving myelosuppressive chemotherapy with an anticipated curative outcome, especially in non-myeloid malignancies.
- This is because ESAs may promote **tumor growth** and are linked to **inferior outcomes**, including reduced locoregional control and survival, in this specific population.
Anemia of chronic disease US Medical PG Question 5: A 7-year-old boy is brought to the pediatrician by his parents for concern of general fatigue and recurrent abdominal pain. You learn that his medical history is otherwise unremarkable and that these symptoms started about 3 months ago after they moved to a different house. Based on clinical suspicion labs are obtained that reveal a microcytic anemia with high-normal levels of ferritin. Examination of a peripheral blood smear shows findings that are demonstrated in the figure provided. Which of the following is the most likely mechanism responsible for the anemia in this patient?
- A. Deletion of beta hemoglobin gene
- B. Chronic loss of blood through GI tract
- C. Inhibition of ALA dehydratase and ferrochelatase (Correct Answer)
- D. Inflammation due to occult abdominal malignancy
- E. X-linked mutation of ALA synthetase
Anemia of chronic disease Explanation: ***Inhibition of ALA dehydratase and ferrochelatase***
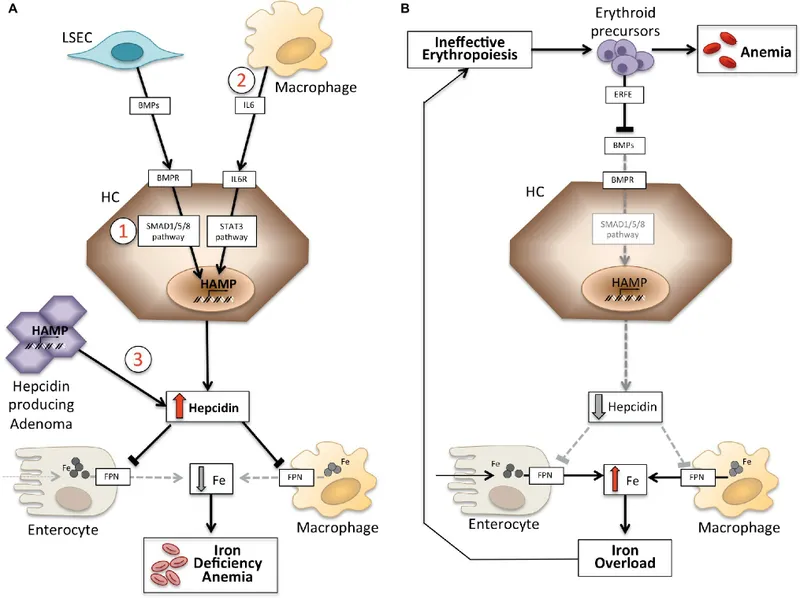
- The patient's symptoms (fatigue, abdominal pain), microcytic anemia with high-normal ferritin, and the presence of **basophilic stippling** in the peripheral blood smear (visible in the provided image as small, dark blue granules within red blood cells) are highly suggestive of **lead poisoning**.
- **Lead toxicity** primarily inhibits two key enzymes in heme synthesis: **aminolevulinate dehydratase (ALA dehydratase)** and **ferrochelatase**. This inhibition leads to impaired heme production, resulting in microcytic anemia, and accumulation of heme precursors, contributing to symptoms. The **high-normal ferritin** despite microcytic anemia is crucial as it rules out iron deficiency and points towards a heme synthesis disorder. The move to a new house 3 months ago suggests a new exposure to lead.
*Deletion of beta hemoglobin gene*
- This describes **beta-thalassemia**, which also causes microcytic anemia. However, beta-thalassemia is a genetic disorder usually presenting earlier in life or with a family history, and typically does not present with **abdominal pain** or **basophilic stippling** as its primary distinguishing feature in this context. Ferritin levels would also vary.
- While beta-thalassemia can cause microcytic anemia, a positive family history and specific hemoglobin electrophoresis findings would be expected, rather than recent onset symptoms linked to a new environment and prominent basophilic stippling.
*Chronic loss of blood through GI tract*
- **Chronic GI blood loss** would lead to **iron deficiency anemia**. While this would cause microcytic anemia, it would be characterized by **low ferritin levels** (as iron stores are depleted), not high-normal ferritin.
- The presence of basophilic stippling is not a typical finding in simple iron deficiency anemia.
*Inflammation due to occult abdominal malignancy*
- **Anemia of chronic disease** due to inflammation (e.g., from malignancy) can be microcytic or normocytic, but it is typically associated with **elevated ferritin** as ferritin is an acute phase reactant. However, this diagnosis would not explain the prominent **basophilic stippling** seen in the peripheral smear.
- Occult malignancy would likely present with other constitutional symptoms and the mechanism of anemia is related to a functional iron deficiency, not a direct inhibition of heme synthesis enzymes like in lead poisoning.
*X-linked mutation of ALA synthetase*
- An **X-linked mutation of ALA synthetase** (the rate-limiting enzyme in heme synthesis) is characteristic of **X-linked sideroblastic anemia**. This condition leads to ring sideroblasts in the bone marrow and typically presents with a microcytic or normocytic anemia.
- While it involves heme synthesis dysfunction, it's a genetic disorder, often congenital, and the sudden onset of symptoms linked to a new environment, along with the distinct feature of basophilic stippling, makes lead poisoning a more likely diagnosis in this specific clinical scenario. Furthermore, in sideroblastic anemia, iron accumulates in mitochondria, but the primary clinical picture and direct enzyme inhibition mechanism differ from lead poisoning.
Anemia of chronic disease US Medical PG Question 6: A 61-year-old man with a history of stage IIIa lung adenocarcinoma that has been treated with wedge resection and chemotherapy presents to the primary care clinic. He is largely asymptomatic, but he demonstrates a persistent microcytic anemia despite iron supplementation. Colonoscopy performed 3 years earlier was unremarkable. His past medical history is significant for diabetes mellitus type II, hypertension, acute lymphoblastic leukemia as a child, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of pinot grigio per day, and currently denies any illicit drug use. His vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 17/min. On physical examination, his pulses are bounding, complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air, with a new oxygen requirement of 2 L by nasal cannula. Which of the following lab values would suggest anemia of chronic disease as the underlying etiology?
- A. Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor
- B. Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor
- C. Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor
- D. Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor (Correct Answer)
- E. Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor
Anemia of chronic disease Explanation: ***Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor***
- In **anemia of chronic disease (ACD)**, inflammation leads to increased **hepcidin** levels, which blocks iron release from stores and reduces iron absorption, resulting in **decreased serum iron and transferrin** (which reflects transferrin saturation).
- The inflammatory state also causes **ferritin** (an acute phase reactant and iron storage protein) to be **increased** or normal, as iron is sequestered. **Serum transferrin receptor** levels are typically normal, differentiating it from iron deficiency anemia.
*Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor*
- This pattern, particularly the **decreased ferritin**, is more indicative of **iron deficiency anemia**, where the body's iron stores are depleted.
- In iron deficiency, the body attempts to increase iron absorption and mobilization, thus ferritin would be low.
*Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor*
- This combination is not typical for any common anemia. **Increased serum iron and transferrin** might suggest iron overload conditions, but not iron-restricted erythropoiesis.
- While ferritin can be increased in chronic disease, the increased serum iron and transferrin are contradictory to ACD.
*Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor*
- This constellation, especially the **increased transferrin** and **decreased ferritin**, is characteristic of **iron deficiency anemia**.
- **Increased serum transferrin receptor** is a hallmark of iron deficiency, as cells upregulate receptors to capture more iron when deficient.
*Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor*
- While **decreased serum iron, decreased transferrin** (low transferrin saturation), and **increased ferritin** can be seen in ACD, the presence of an **increased serum transferrin receptor** is inconsistent.
- An increased serum transferrin receptor is usually a marker for increased erythropoietic activity or iron deficiency, which is not the primary mechanism of ACD.
Anemia of chronic disease US Medical PG Question 7: A 72-year-old woman comes to the physician because of a 1-month history of progressive fatigue and shortness of breath. Physical examination shows generalized pallor. Laboratory studies show:
Hemoglobin 5.8 g/dL
Hematocrit 17%
Mean corpuscular volume 86 μm3
Leukocyte count 6,200/mm3 with a normal differential
Platelet count 240,000/mm3
A bone marrow aspirate shows an absence of erythroid precursor cells. This patient’s condition is most likely associated with which of the following?
- A. Cold agglutinins
- B. Thymic tumor (Correct Answer)
- C. HbF persistence
- D. Parvovirus B19 infection
- E. Lead poisoning
Anemia of chronic disease Explanation: ***Thymic tumor***
- The patient's **normocytic anemia** (Hb 5.8 g/dL, Hct 17%, MCV 86 μm3) and the **absence of erythroid precursor cells** in the bone marrow aspirate are characteristic findings of **pure red cell aplasia (PRCA)**.
- **Pure red cell aplasia (PRCA)** in adults is frequently associated with an underlying **thymoma**, with up to 50% of adult PRCA cases linked to this condition.
*Cold agglutinins*
- Cold agglutinins are characteristic of **cold agglutinin disease**, an **autoimmune hemolytic anemia**.
- This condition typically presents with signs of **hemolysis** (e.g., elevated reticulocytes, bilirubin, LDH) and would not show an **absence of erythroid precursor cells** in the bone marrow.
*HbF persistence*
- **Hereditary persistence of fetal hemoglobin (HPFH)** is a benign condition where **HbF** production continues into adulthood.
- It is not associated with anemia or bone marrow aplasia and usually results in normal hematological parameters, except for elevated HbF.
*Parvovirus B19 infection*
- **Parvovirus B19** can cause transient **aplastic crisis** by infecting and destroying erythroid precursors.
- While it causes PRCA-like features, it is typically an acute self-limiting condition, particularly in immunocompetent individuals, and is less likely to be an ongoing chronic cause in a 72-year-old without other risk factors for chronic infection or immunodeficiency.
*Lead poisoning*
- **Lead poisoning** typically causes a **microcytic hypochromic anemia** with **basophilic stippling** on peripheral blood smear.
- It primarily interferes with **heme synthesis** and would not cause a complete absence of erythroid precursor cells in the bone marrow.
Anemia of chronic disease US Medical PG Question 8: A 76-year-old woman comes in for a routine checkup with her doctor. She is concerned that she feels tired most days and has difficulty doing her household chores. She complains that she gets fatigued and breathless with mild exertion. Past medical history is significant for diabetes mellitus, chronic kidney disease from prolonged elevated blood sugar, and primary biliary cirrhosis. Medications include lisinopril, insulin, and metformin. Family medicine is noncontributory. She drinks one beer every day. Today, she has a heart rate of 98/min, respiratory rate of 17/min, blood pressure of 110/65 mm Hg, and a temperature of 37.0°C (98.6°F). General examination shows that she is pale and haggard looking. She has a heartbeat with a regular rate and rhythm and her lungs are clear to auscultation bilaterally. A complete blood count (CBC) is as follows:
Leukocyte count: 12,000/mm3
Red blood cell count: 3.1 million/mm3
Hemoglobin: 11.0 g/dL
MCV: 85 fL
MCH: 27 pg/cell
Platelet count: 450,000/mm3
Fecal occult blood test is negative. What is the most likely cause of her anemia?
- A. Chronic kidney disease (Correct Answer)
- B. Acute bleeding
- C. Alcoholism
- D. Liver disease
- E. Colorectal cancer
Anemia of chronic disease Explanation: ***Chronic kidney disease***
- **Chronic kidney disease (CKD)** is a common cause of **normocytic, normochromic anemia** due to decreased production of **erythropoietin** by the kidneys.
- This patient's history of CKD, alongside her **normocytic anemia (MCV 85 fL)**, makes this the most likely cause.
*Acute bleeding*
- Acute bleeding would typically present with signs of **hypovolemia** (e.g., hypotension, tachycardia) and potentially a **reticulocytosis** as the bone marrow compensates, neither of which are seen here.
- The **negative fecal occult blood test** and stable vital signs also argue against acute or chronic gastrointestinal bleeding.
*Alcoholism*
- Chronic alcoholism can lead to anemia, often **macrocytic** due to **folate deficiency**, or less commonly microcytic if associated with iron deficiency from GI bleeding.
- While she drinks one beer daily, this amount is unlikely to directly cause significant anemia, especially given her **normocytic MCV**.
*Liver disease*
- **Primary biliary cirrhosis (PBC)** can cause anemia through various mechanisms, including **hemolysis**, **folate deficiency**, or bleeding from **portal hypertension**.
- However, PBC-related anemia is often microcytic or macrocytic, and her **normocytic MCV** and the more direct link to CKD make it less likely to be the primary cause.
*Colorectal cancer*
- **Colorectal cancer** can cause anemia due to **chronic blood loss**, which would typically lead to **iron deficiency anemia** (microcytic anemia).
- The patient has a **normocytic anemia (MCV 85 fL)** and a **negative fecal occult blood test**, making this diagnosis highly unlikely.
Anemia of chronic disease US Medical PG Question 9: A 25-year-old woman is being evaluated due to complaint of fatigue and voiding pink urine. The laboratory results are as follows:
Hb 6.7
Red blood cell count 3.0 x 1012/L
Leukocyte count 5,000/mm3
Platelets 170 x 109/L
Reticulocyte count 6%
Hematocrit 32%
The physician thinks that the patient is suffering from an acquired mutation in hematopoietic stem cells, which is confirmed by flow cytometry analysis that revealed these cells are CD 55 and CD 59 negative. However, the physician is interested in knowing the corrected reticulocyte count before starting the patient on eculizumab. What value does the physician find after calculating the corrected reticulocyte count?
- A. 3.1%
- B. 0.4%
- C. 0.1%
- D. 0.6%
- E. 4.6% (Correct Answer)
Anemia of chronic disease Explanation: ***4.6%***
- The corrected reticulocyte count accounts for the degree of anemia by adjusting for the patient's hematocrit compared to normal.
- **Formula: Corrected Retics% = Observed Retics% × (Patient's Hct / Normal Hct)**
- Using normal Hct of 42% for women: 6% × (32/42) = 6% × 0.76 = **4.56% ≈ 4.6%**
- This reflects the actual reticulocyte production capacity adjusted for the anemic state.
*3.1%*
- This value might result from using an incorrect normal hematocrit value in the calculation.
- For example, using 6% × (32/60) would give approximately 3.2%, suggesting use of an inappropriately high reference value.
*0.4%*
- This value likely results from applying the **Reticulocyte Production Index (RPI)** formula, which includes a maturation factor correction: 6% × (32/42) × (1/2.5) = 1.82%, then with further error.
- Such a low value from formula misapplication does not represent the standard corrected reticulocyte count requested.
*0.1%*
- This extremely low value would indicate **severe calculation error** or bone marrow failure, which contradicts the observed 6% reticulocyte count.
- In PNH with hemolysis, reticulocyte production is typically increased, making this value implausible.
*0.6%*
- This incorrect value could result from mathematical errors in applying correction factors or using the wrong hematocrit values in the formula.
- The standard corrected reticulocyte formula would not yield this value with the given parameters.
Anemia of chronic disease US Medical PG Question 10: A 68-year-old woman comes to the physician because of increasing heartburn for the last few months. During this period, she has taken ranitidine several times a day without relief and has lost 10 kg (22 lbs). She has retrosternal pressure and burning with every meal. She has had heartburn for several years and took ranitidine as needed. She has hypertension. She has smoked one pack of cigarettes daily for the last 40 years and drinks one glass of wine occasionally. Other current medications include amlodipine and hydrochlorothiazide. She appears pale. Her height is 163 cm (5 ft 4 in), her weight is 75 kg (165 lbs), BMI is 27.5 kg/m2. Her temperature is 37.2°C (98.96°F), pulse is 78/min, and blood pressure is 135/80 mm Hg. Cardiovascular examination shows no abnormalities. Abdominal examination shows mild tenderness to palpation in the epigastric region. Bowel sounds are normal. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.2 g/dL
Mean corpuscular volume 78 μm
Mean corpuscular hemoglobin 23 pg/cell
Leukocyte count 9,500/mm3
Platelet count 330,000/mm3
Serum
Na+ 137 mEq/L
K+ 3.8 mEq/L
Cl- 100 mEq/L
HCO3- 25 mEq/L
Creatinine 1.2 mg/dL
Lactate dehydrogenase 260 U/L
Alanine aminotransferase 18 U/L
Aspartate aminotransferase 15 U/L
Lipase (N < 280 U/L) 40 U/L
Troponin I (N < 0.1 ng/mL) 0.029 ng/mL
An ECG shows normal sinus rhythm without ST-T changes. Which of the following is the most appropriate next step in the management of this patient?
- A. 24-hour esophageal pH monitoring
- B. Esophagogastroduodenoscopy (Correct Answer)
- C. Barium swallow
- D. Trial of proton-pump inhibitor
- E. Esophageal manometry
Anemia of chronic disease Explanation: ***Esophagogastroduodenoscopy***
- This patient presents with **alarm symptoms** (weight loss, iron deficiency anemia, persistent heartburn unresponsive to ranitidine) that warrant an immediate investigation for underlying malignancy or severe mucosal damage.
- **EGD directly visualizes the esophagus, stomach, and duodenum**, allowing for biopsies of suspicious lesions, which is crucial given her risk factors (smoking, chronic GERD, age).
*24-hour esophageal pH monitoring*
- This test is primarily used to **diagnose GERD** in patients with typical symptoms but normal endoscopy, or to guide treatment for refractory GERD.
- It is not the appropriate first step here because the patient has alarm symptoms, which necessitate direct visualization and biopsy to rule out serious pathology.
*Barium swallow*
- A barium swallow can identify **structural abnormalities** such as strictures, diverticula, or large masses but has limited utility for detecting subtle mucosal changes or early malignancy.
- It does not allow for **biopsy**, which is essential for definitive diagnosis in a patient with alarm symptoms.
*Trial of proton-pump inhibitor*
- A trial of PPIs is appropriate for patients with **typical GERD symptoms** without alarm features, as a diagnostic and therapeutic intervention.
- However, this patient has already tried ranitidine (an H2 blocker) without relief and exhibits multiple **alarm symptoms**, making empirical treatment insufficient and potentially dangerous by delaying diagnosis.
*Esophageal manometry*
- Esophageal manometry assesses **esophageal motility** and sphincter function, useful for diagnosing motility disorders like achalasia or diffuse esophageal spasm.
- It is indicated if a motility disorder is suspected, usually *after* ruling out structural causes with EGD, and does not address the immediate concern of underlying malignancy or severe damage raised by the patient's alarm symptoms.
More Anemia of chronic disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.