Valvular heart disease and heart failure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Valvular heart disease and heart failure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Valvular heart disease and heart failure US Medical PG Question 1: A 68-year-old man comes to the emergency department because of a 1-week history of difficulty breathing. He has had recurrent palpitations over the past 2 years. During this time, he has also had several episodes of anxiety despite no change in his daily life. He has occasional sharp chest pain localized to the left upper sternal border. He has no abdominal pain or leg swelling. Two years ago, he had streptococcal pharyngitis, which was promptly treated with a 10-day course of penicillin. He has never traveled outside of the country. His temperature is 36.5°C (97.7°F), pulse is 82/min, and blood pressure is 140/85 mm Hg. Physical examination shows a 3/6 holosystolic murmur that is loudest at the apex and radiates to the axilla with a mid-systolic click. Bilateral fine crackles are heard on lung auscultation. Which of the following is the most likely cause of this patient's symptoms?
- A. Inflammatory valve degeneration
- B. Ectopic production of serotonin
- C. Myxomatous valve degeneration (Correct Answer)
- D. Calcific valve degeneration
- E. Overproduction of catecholamines
Valvular heart disease and heart failure Explanation: ***Myxomatous valve degeneration***
- The presence of a **mid-systolic click** followed by a **holosystolic murmur** at the apex radiating to the axilla is highly characteristic of **mitral valve prolapse (MVP)** with **mitral regurgitation (MR)**.
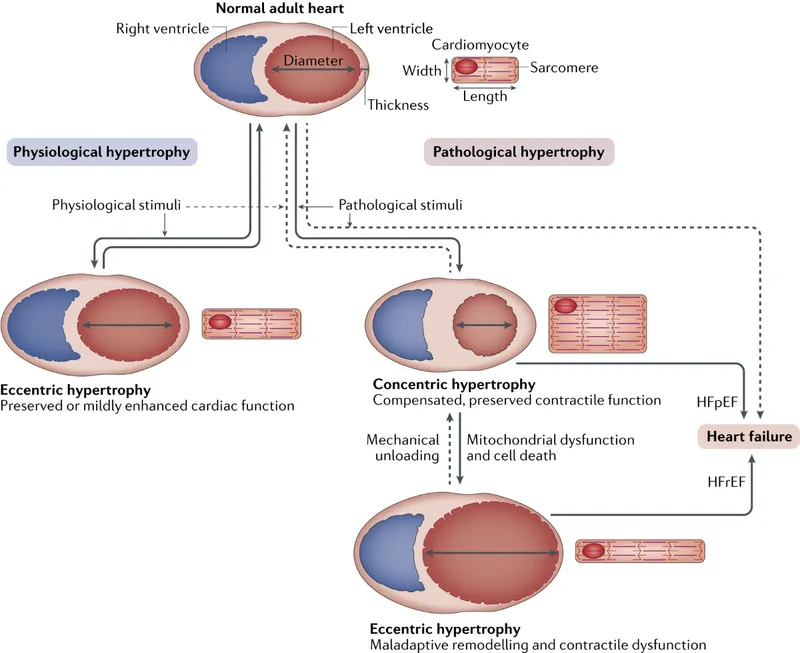
- MVP is most commonly caused by **myxomatous degeneration** of the mitral valve leaflets, leading to their billowing into the left atrium during systole. The patient's recurrent palpitations, anxiety, and non-exertional chest pain are common symptoms associated with MVP, while difficulty breathing and crackles suggest **heart failure** from chronic MR.
*Inflammatory valve degeneration*
- **Inflammatory valve degeneration**, such as that seen in rheumatic heart disease, typically presents with a history of recurrent streptococcal infections leading to valvular scarring and dysfunction (e.g., mitral stenosis).
- While the patient had streptococcal pharyngitis, it was treated, and the clinical presentation with a mid-systolic click is more indicative of myxomatous changes rather than rheumatic inflammation.
*Ectopic production of serotonin*
- **Ectopic production of serotonin** occurs in settings like **carcinoid syndrome**, which typically involves flushing, diarrhea, bronchospasm, and can affect the right-sided heart valves primarily.
- The patient's symptoms are centered on left-sided heart issues and do not align with the broader systemic features of carcinoid syndrome.
*Calcific valve degeneration*
- **Calcific valve degeneration** commonly affects the **aortic valve** leading to **aortic stenosis** in older adults, characterized by a systolic ejection murmur heard at the right upper sternal border.
- It does not typically cause a mid-systolic click or affect the mitral valve in this manner, and the murmur description is inconsistent with aortic stenosis.
*Overproduction of catecholamines*
- **Overproduction of catecholamines**, as seen in conditions like **pheochromocytoma**, causes symptoms such as paroxysmal hypertension, palpitations, sweating, and anxiety.
- While some symptoms like palpitations and anxiety overlap, the specific cardiac murmur and signs of heart failure are not directly explained by catecholamine excess alone; a structural heart problem is more likely.
Valvular heart disease and heart failure US Medical PG Question 2: A 31-year-old man comes to the physician because of a 5-day history of fever, chills, and dyspnea. His temperature is 38.9°C (102°F) and pulse is 90/min. Cardiac examination shows a murmur. In addition to other measures, cardiac catheterization is performed. A graph showing the results of the catheterization is shown. This patient most likely has which of the following valvular heart defects?
- A. Mitral regurgitation
- B. Aortic regurgitation (Correct Answer)
- C. Mitral stenosis
- D. Pulmonary regurgitation
- E. Aortic stenosis
Valvular heart disease and heart failure Explanation: ***Aortic regurgitation***
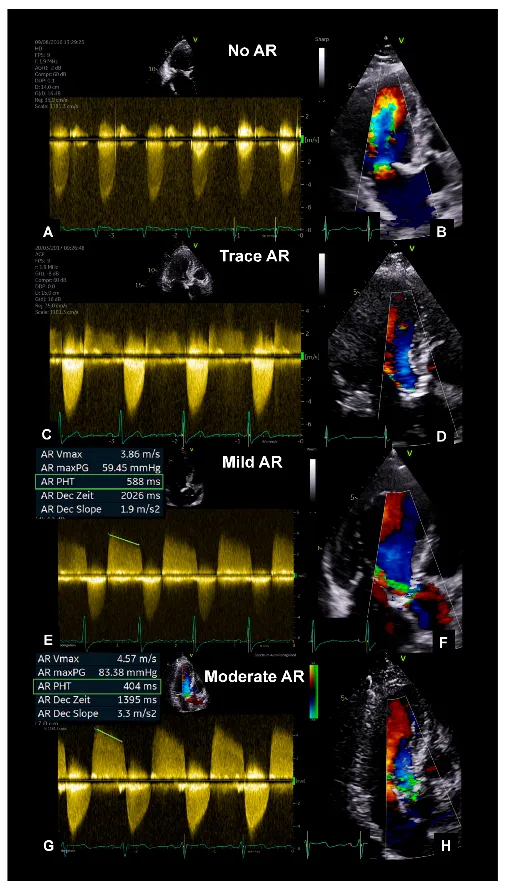
- Aortic regurgitation is characterized by a high-pitched **diastolic decrescendo murmur**, best heard at the left sternal border.
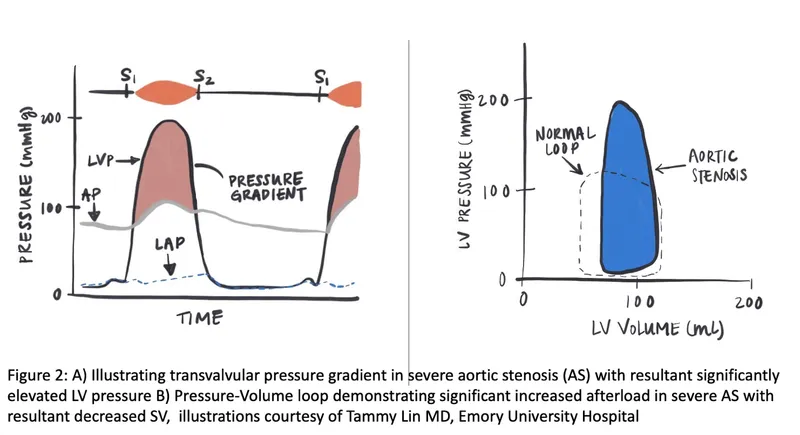
- The catheterization graph shows a **rapid decline in aortic pressure during diastole**, signifying blood flowing back into the left ventricle, which is characteristic of aortic regurgitation.
*Mitral regurgitation*
- Mitral regurgitation would cause a **pansystolic murmur** and a large **V wave in the pulmonary capillary wedge pressure tracing**, neither of which is implied by the provided information.
- Its primary hemodynamic feature is blood flowing back into the **left atrium during systole**, not diastolic aortic pressure changes.
*Mitral stenosis*
- Mitral stenosis typically presents with a **diastolic rumble** and an **opening snap**, which are different from the findings described.
- Hemodynamically, it would show an **elevated left atrial pressure** and a pressure gradient across the mitral valve during diastole.
*Pulmonary regurgitation*
- Pulmonary regurgitation involves the flow of blood from the pulmonary artery back into the **right ventricle during diastole**.
- This condition would lead to characteristic changes in **right ventricular and pulmonary artery pressures**, not the left-sided heart pressures shown in the graph.
*Aortic stenosis*
- Aortic stenosis causes a **systolic crescendo-decrescendo murmur**, often with radiation to the carotids.
- Hemodynamically, it would show a **significant pressure gradient across the aortic valve during systole** and a delayed carotid upstroke.
Valvular heart disease and heart failure US Medical PG Question 3: A 27-year-old woman, who recently immigrated from Bangladesh, presents to her primary care physician to discuss birth control. During a review of her past medical history, she reports that as a child she had a recurrent sore throat and fever followed by swollen and aching hip and knee joints. These symptoms returned every season and were never treated but went away on their own only to return with the next typhoon season. When asked about any current complaints, the patient says that she sometimes has shortness of breath and palpitations that do not last long. A physical exam is performed. In which of the auscultation sites will a murmur most likely be heard in this patient?
- A. Point 5 (Correct Answer)
- B. Point 4
- C. Point 2
- D. Point 3
- E. Point 1
Valvular heart disease and heart failure Explanation: ***Point 5***
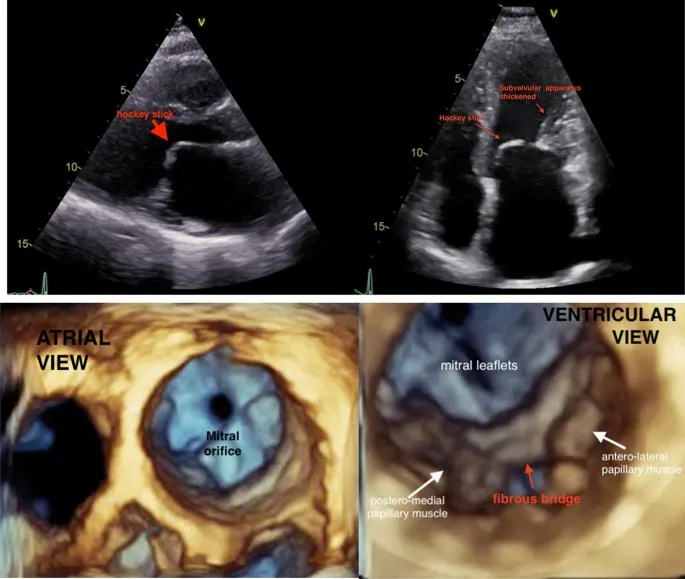
- The patient's history of recurrent sore throat, fever, and migratory polyarthritis (swollen and aching hip and knee joints) followed by intermittent shortness of breath and palpitations is highly suggestive of **rheumatic fever** with subsequent **rheumatic heart disease**.
- This condition most commonly affects the **mitral valve**, leading to **mitral stenosis** or regurgitation, which would produce an apical murmur heard best at point 5 (the cardiac apex).
*Point 4*
- Point 4 corresponds to the **tricuspid area** (lower left sternal border). While rheumatic heart disease can affect the tricuspid valve, it is less common than mitral valve involvement and usually occurs in conjunction with severe mitral valve disease.
- An isolated murmur here would suggest tricuspid valve pathology, which is less likely as the primary presentation in rheumatic heart disease.
*Point 2*
- Point 2 is the **pulmonic area** (left upper sternal border, second intercostal space). Murmurs heard here typically indicate pulmonary valve disease or flow murmurs.
- While pulmonary hypertension can be a complication of severe left-sided heart disease, primary pulmonic valve involvement in rheumatic heart disease is rare.
*Point 3*
- Point 3 (Erb's point, third intercostal space, left sternal border) is often used to auscultate for murmurs of **aortic regurgitation** or to hear the splitting of S2.
- While aortic valve involvement can occur in rheumatic heart disease, **mitral valve disease** is significantly more prevalent and typically presents earlier and more severely.
*Point 1*
- Point 1 is the **aortic area** (right upper sternal border, second intercostal space). Murmurs heard here are typically associated with **aortic stenosis** or regurgitation.
- Although the aortic valve can be affected by rheumatic heart disease, the mitral valve is the most commonly involved valve, making an apical murmur (Point 5) more likely for the initial and most prominent finding.
Valvular heart disease and heart failure US Medical PG Question 4: A 27-year-old woman with a history of a "heart murmur since childhood" presents following a series of syncopal episodes over the past several months. She also complains of worsening fatigue over this time period, and notes that her lips have begun to take on a bluish tinge, for which she has been using a brighter shade of lipstick. You do a careful examination, and detect a right ventricular heave, clubbing of the fingers, and 2+ pitting edema bilaterally to the shins. Despite your patient insisting that every doctor she has ever seen has commented on her murmur, you do not hear one. Transthoracic echocardiography would most likely detect which of the following?
- A. Mitral insufficiency
- B. Aortic stenosis
- C. Dynamic left ventricular outflow tract obstruction
- D. Positive bubble study (Correct Answer)
- E. Ventricular aneurysm
Valvular heart disease and heart failure Explanation: ***Positive bubble study***
- The patient's symptoms, including **cyanosis** (**bluish tinge to the lips**), **clubbing**, and **right ventricular heave**, suggest **Eisenmenger syndrome**, a late complication of a **left-to-right shunt** that has reversed due to pulmonary hypertension.
- A positive bubble study on echocardiography would confirm the presence of a **right-to-left shunt**, characteristic of Eisenmenger syndrome, by showing microbubbles crossing from the right to the left side of the heart.
*Mitral insufficiency*
- While mitral insufficiency can cause a murmur and heart failure symptoms, it does not typically lead to the **cyanosis** and **clubbing** described.
- The absence of a murmur, despite a history of one, points away from a significant current insufficiency.
*Aortic stenosis*
- Aortic stenosis is characterized by an **ejection systolic murmur** that would likely be heard on examination, contradicting the scenario where no murmur is audible.
- It usually presents with a different constellation of symptoms, such as angina, syncope, and heart failure, without the prominent cyanosis or clubbing seen here.
*Dynamic left ventricular outflow tract obstruction*
- This is characteristic of **hypertrophic obstructive cardiomyopathy (HOCM)**, which can cause exertional syncope.
- However, HOCM does not typically lead to **cyanosis**, a **right ventricular heave**, or **clubbing**, which are strong indicators of a right-to-left shunt.
*Ventricular aneurysm*
- A ventricular aneurysm is a bulging of the ventricular wall, often a complication of a **myocardial infarction**, which is unlikely in a 27-year-old with a history of a "heart murmur since childhood."
- It typically presents with symptoms related to heart failure, arrhythmias, or embolism, and would not explain the prominent **cyanosis** and **clubbing**.
Valvular heart disease and heart failure US Medical PG Question 5: A 72-year-old man who was involved in a traffic collision is brought to the emergency room by the ambulance service. He was in shock and comatose at the time of presentation. On examination, the heart rate is 60/min, and the blood pressure is 70/40 mm Hg. The patient dies, despite resuscitative efforts. Autopsy reveals multiple internal hemorrhages and other evidence of ischemic damage affecting the lungs, kidneys, and brain. The patient’s heart shows evidence of gross anomaly similar to the picture. While acute hypovolemia is the likely cause of the ischemic changes seen in the lungs, kidneys, and brain, which of the following best explains the gross anomaly of his heart?
- A. Senile calcific aortic stenosis (Correct Answer)
- B. Accumulation of amyloid in the myocardium
- C. Mitral valve stenosis
- D. Hypertrophic cardiomyopathy
- E. Aortic valve regurgitation
Valvular heart disease and heart failure Explanation: ***Senile calcific aortic stenosis***
- The patient's age (72 years) makes **senile calcific aortic stenosis** a very likely finding, as it is a degenerative condition common in the elderly leading to stiffening and calcification of the aortic valve.
- While the immediate cause of death was **hypovolemic shock**, the presence of an underlying **cardiac anomaly** could worsen the patient's ability to compensate for significant blood loss, contributing to the rapid decompensation observed.
- Gross pathology typically shows **calcified, thickened aortic valve leaflets** that are stenotic.
*Accumulation of amyloid in the myocardium*
- While **cardiac amyloidosis** can occur in the elderly and cause restrictive cardiomyopathy, it typically presents with **heart failure symptoms** and often results in thickened ventricular walls, which is not specifically indicated as the "gross anomaly" in this context.
- The sudden, acute decompensation due to trauma does not align as strongly with the chronic progression of amyloidosis as it does with a structural valvular issue exacerbated by shock.
*Mitral valve stenosis*
- **Mitral valve stenosis** is more often associated with **rheumatic heart disease** or congenital anomalies, which are less common in this age group as a primary, sudden anomaly.
- While it can lead to heart failure, the description of a "gross anomaly" in the context of acute decompensation and the patient's age points more towards a common degenerative valvular condition like aortic stenosis.
*Hypertrophic cardiomyopathy*
- **Hypertrophic cardiomyopathy (HCM)** is a genetic condition that typically presents earlier in life with symptoms of outflow obstruction or sudden cardiac death in young athletes.
- While HCM can present in older adults, the gross pathology shows **asymmetric septal hypertrophy** rather than valvular pathology.
- In a 72-year-old, age-related degenerative valve disease is more common than first presentation of genetic cardiomyopathy.
*Aortic valve regurgitation*
- Although **aortic regurgitation** can lead to cardiac remodeling and failure, it is less likely to be referred to simply as a "gross anomaly" in this context without more specific valvular description.
- **Senile calcific aortic stenosis** is a more common degenerative anomaly in this age group, and the question implies a common, age-related finding.
Valvular heart disease and heart failure US Medical PG Question 6: A 50-year-old female presents with a holosystolic murmur heard best over the apex, radiating to the axilla. She has no signs of pulmonary hypertension or edema. What best explains her lack of symptoms?
- A. The aorta is compensating with increased compliance
- B. Mitral valve prolapse without regurgitation causes no hemodynamic changes
- C. The left atrium is compensating with increased compliance (Correct Answer)
- D. As long as preload in the left ventricle is maintained there would be no symptoms
- E. The right ventricle is compensating with decreased compliance
Valvular heart disease and heart failure Explanation: ***The left atrium is compensating with increased compliance***
- In **mitral regurgitation**, the initial compensatory mechanism involves the **left atrium stretching and increasing its compliance** to accommodate the regurgitant volume.
- This **prevents a significant rise in left atrial pressure**, thereby averting pulmonary congestion symptoms like edema or pulmonary hypertension.
*The aorta is compensating with increased compliance*
- **Aortic compliance** primarily affects **afterload** and is not a direct compensatory mechanism for mitral regurgitation.
- While aortic stiffening can exacerbate cardiac workload, increased compliance wouldn't specifically mitigate symptoms arising from left atrial volume overload.
*Mitral valve prolapse without regurgitation causes no hemodynamic changes*
- A **holosystolic murmur** best heard at the apex and radiating to the axilla is characteristic of **mitral regurgitation**, indicating actual blood flow back into the atrium during systole.
- **Mitral valve prolapse without regurgitation** might be silent or cause a mid-systolic click without significant hemodynamic changes, but this patient has clear evidence of regurgitation.
*As long as preload in the left ventricle is maintained there would be no symptoms*
- **Preload maintenance in the left ventricle** is important for maintaining cardiac output, but regurgitation itself diverts blood from forward flow.
- Symptoms in mitral regurgitation often arise from **increased left atrial pressure** and subsequent pulmonary congestion, even if left ventricular preload is sufficient to maintain some forward flow.
*The right ventricle is compensating with decreased compliance*
- **Right ventricular compliance** is primarily relevant to conditions affecting the pulmonary circulation or right heart.
- It would not directly compensate for left-sided volume overload in mitral regurgitation; in fact, prolonged left-sided heart failure can eventually lead to right ventricular dysfunction.
Valvular heart disease and heart failure US Medical PG Question 7: A 64-year-old woman with a history of rheumatic fever presents to her primary care clinician complaining of excessive fatigue with walking and difficulty lying flat. She had no prior physical limitations, but recently has been unable to walk more than 3 blocks without needing to stop and rest. Her cardiac exam is notable for a late diastolic murmur heard best at the apex in the left lateral decubitus position with no radiation. What is the most likely diagnosis?
- A. Aortic Stenosis
- B. Tricuspid Regurgitation
- C. Mitral Regurgitation
- D. Aortic Regurgitation
- E. Mitral Stenosis (Correct Answer)
Valvular heart disease and heart failure Explanation: ***Mitral Stenosis***
- A **late diastolic murmur heard best at the apex** in the left lateral decubitus position is a classic finding of **mitral stenosis**.
- History of **rheumatic fever** is a strong risk factor for mitral stenosis due to scarring and thickening of the mitral valve leaflets. **Fatigue with exertion** and **dyspnea on lying flat (orthopnea)** are common symptoms of left atrial enlargement and pulmonary congestion.
*Aortic Stenosis*
- Characterized by a **systolic ejection murmur** best heard at the right upper sternal border, radiating to the carotids.
- While it can cause exertional dyspnea and fatigue, the murmur timing and location do not match the patient's presentation.
*Tricuspid Regurgitation*
- Presents with a **holosystolic murmur** best heard at the left sternal border, often increasing with inspiration.
- Unlike mitral stenosis, it is more commonly associated with right-sided heart failure symptoms like peripheral edema and ascites.
*Mitral Regurgitation*
- Characterized by a **holosystolic murmur** that radiates to the axilla, best heard at the apex.
- Although also associated with rheumatic fever and causing fatigue, the timing of the murmur (systolic vs. diastolic) differentiates it from mitral stenosis.
*Aortic Regurgitation*
- Presents with an **early diastolic decrescendo murmur** best heard at the left sternal border.
- While it can cause dyspnea on exertion, its murmur is distinctly different from the late diastolic murmur described.
Valvular heart disease and heart failure US Medical PG Question 8: A 34-year-old male is brought to the emergency department. He has prior hospitalizations for opiate overdoses, but today presents with fever, chills, rigors and malaise. On physical exam vitals are temperature: 100.5 deg F (38.1 deg C), pulse is 105/min, blood pressure is 135/60 mmHg, and respirations are 22/min. You note the following findings on the patient's hands (Figures A and B). You note that as the patient is seated, his head bobs with each successive heart beat. Which of the following findings is most likely present in this patient?
- A. A holosystolic murmur at the 4th intercostal midclavicular line
- B. A water-hammer pulse when palpating the radial artery (Correct Answer)
- C. Decreased blood pressure as measured in the lower extremities compared to the upper extremities
- D. A harsh crescendo-decrescendo systolic murmur in the right second intercostal space
- E. A consistent gallop with an S4 component
Valvular heart disease and heart failure Explanation: ***A water-hammer pulse when palpating the radial artery***
- The patient's history of **opiate overdose**, fever, chills, and the presence of **Janeway lesions** (Figures A and B) on the hands strongly suggest **infective endocarditis**. The head bobbing (Musset's sign) indicates **severe aortic regurgitation**.
- **Water-hammer pulse** (Corrigan's pulse) is a classic sign of **severe aortic regurgitation**, characterized by a rapid, forceful arterial pulse that quickly collapses due to a large stroke volume and rapid diastolic runoff.
*A holosystolic murmur at the 4th intercostal midclavicular line*
- A holosystolic murmur at the 4th intercostal midclavicular line is typically associated with **mitral regurgitation**, which is less likely given the prominent signs of aortic regurgitation.
- While endocarditis can affect the mitral valve, the specific clinical signs point towards **aortic valve involvement**.
*Decreased blood pressure as measured in the lower extremities compared to the upper extremities*
- This finding is characteristic of **coarctation of the aorta**, a congenital heart defect, which is not suggested by the patient's presentation or risk factors.
- The patient's symptoms are more consistent with an acute infectious process affecting the heart valves.
*A harsh crescendo-decrescendo systolic murmur in the right second intercostal space*
- A harsh crescendo-decrescendo systolic murmur in the right second intercostal space is typical of **aortic stenosis**.
- While aortic insufficiency is present, the murmur for uncomplicated aortic insufficiency is usually a **diastolic decrescendo murmur**, not a harsh systolic murmur.
*A consistent gallop with an S4 component*
- An S4 gallop is typically heard in conditions involving **decreased ventricular compliance** (e.g., severe hypertension, aortic stenosis, hypertrophic cardiomyopathy).
- While endocarditis can cause heart failure, an S4 gallop is not a direct or primary sign of **aortic regurgitation**. An S3 gallop is more commonly associated with **volume overload** and heart failure, which might develop in severe aortic regurgitation.
Valvular heart disease and heart failure US Medical PG Question 9: An 85-year-old man presents to his primary care provider after feeling "lightheaded." He said he helped his wife in the garden for the first time, but that while moving some bags of soil he felt like he was going to faint. He had a big breakfast of oatmeal and eggs prior to working in the garden. He has no significant past medical history and takes a baby aspirin daily. Physical exam reveals an elderly, well-nourished, well-built man with no evidence of cyanosis or tachypnea. Vital signs show normal temperature, BP 150/70, HR 80, RR 18. Cardiac exam reveals crescendo-decrescendo systolic murmur. What is the most likely cause of this patient's diagnosis?
- A. Infection
- B. Atherosclerosis
- C. Calcification (Correct Answer)
- D. Congenital defect
- E. Malnutrition
Valvular heart disease and heart failure Explanation: ***Calcification***
- The patient's age (85 years old) and the presence of a **crescendo-decrescendo systolic murmur** strongly suggest **aortic stenosis**. The most common cause of aortic stenosis in the elderly is **degenerative calcification** of the aortic valve.
- His **lightheadedness** upon exertion (moving bags of soil) is consistent with symptoms of aortic stenosis, as the narrowed valve restricts blood flow to the brain during increased demand.
*Infection*
- While infective endocarditis can cause new murmurs and systemic symptoms, it typically presents with **fever**, **fatigue**, and signs of infection, which are not described in this patient.
- The type of murmur in endocarditis is often **regurgitant** or can have a rapidly changing character, rather than the classic crescendo-decrescendo systolic murmur of aortic stenosis.
*Atherosclerosis*
- Although atherosclerosis is a common process in the elderly and can affect large vessels, it does **not** directly cause aortic stenosis. The valve pathology is primarily a **degenerative calcific process** rather than atherosclerotic plaque formation.
- While atherosclerosis and calcific aortic stenosis share some risk factors (age, hypertension, hyperlipidemia), the mechanism of valve narrowing is through progressive **calcification and fibrosis** of the valve leaflets, not atheroma formation.
*Congenital defect*
- While a **bicuspid aortic valve** is a common congenital defect that can lead to aortic stenosis, symptoms typically present much earlier in life (40s-60s) due to accelerated calcification.
- An 85-year-old presenting with new symptoms is more likely to have age-related **degenerative calcific aortic stenosis** rather than a late manifestation of an undiagnosed congenital defect.
*Malnutrition*
- Malnutrition is not directly associated with the development of a crescendo-decrescendo systolic murmur or **aortic stenosis**.
- While severe malnutrition can cause various systemic issues, it does not explain the specific cardiac findings and exertional symptoms described in this well-nourished patient.
Valvular heart disease and heart failure US Medical PG Question 10: A 36-year-old man presents to his primary care physician because of shortness of breath. He is an office worker who has a mostly sedentary lifestyle; however, he has noticed that recently he feels tired and short of breath when going on long walks with his wife. He also has had a hacking cough that seems to linger, though he attributes this to an upper respiratory tract infection he had 2 months ago. He has diabetes that is well-controlled on metformin and has smoked 1 pack per day for 20 years. Physical exam reveals a large chested man with wheezing bilaterally and mild swelling in his legs and abdomen. The cause of this patient's abdominal and lower extremity swelling is most likely due to which of the following processes?
- A. Excessive protease activity
- B. Damage to kidney tubules
- C. Hyperplasia of mucous glands
- D. Defective protein folding
- E. Right ventricular dysfunction secondary to pulmonary hypertension (Correct Answer)
Valvular heart disease and heart failure Explanation: ***Right ventricular dysfunction secondary to pulmonary hypertension***
- This patient's long history of smoking, chronic cough, and wheezing suggest significant **chronic obstructive pulmonary disease (COPD)**, which leads to **hypoxemia** and **pulmonary hypertension**.
- **Pulmonary hypertension** increases the workload on the **right ventricle**, eventually leading to **right heart failure** (cor pulmonale), characterized by peripheral edema (leg swelling) and ascites (abdominal swelling).
*Excessive protease activity*
- While excessive protease activity (e.g., elastase) is implicated in the pathogenesis of **emphysema** by destroying alveolar walls, it does not directly cause peripheral edema and ascites.
- This process primarily leads to **airflow obstruction** and **gas exchange abnormalities**, which can indirectly contribute to pulmonary hypertension but is not the direct cause of the peripheral edema.
*Damage to kidney tubules*
- **Acute tubular necrosis** or chronic kidney disease can cause edema due to impaired fluid and electrolyte balance, but the patient's symptoms (dyspnea, wheezing, smoking history) point strongly to a primary pulmonary and cardiac etiology.
- While diabetes can cause nephropathy, there is no information to suggest acute kidney injury or chronic kidney disease leading to such severe edema.
*Hyperplasia of mucous glands*
- **Hyperplasia of mucous glands** in the bronchi is characteristic of **chronic bronchitis**, contributing to the chronic cough and airway obstruction.
- This pathology primarily affects airway clearance and airflow, rather than directly causing systemic edema or ascites.
*Defective protein folding*
- **Defective protein folding**, such as in **alpha-1 antitrypsin deficiency**, can lead to early-onset emphysema and liver disease.
- While this could fit with a pulmonary presentation, it is less common than smoking-induced COPD and does not directly explain the edema and ascites caused by right heart failure.
More Valvular heart disease and heart failure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.