Right heart failure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Right heart failure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Right heart failure US Medical PG Question 1: A 41-year-old man comes to the emergency department because of fatigue, worsening abdominal discomfort, and progressive swelling of his legs for 3 months. The swelling is worse in the evenings. His only medication is ibuprofen for occasional joint pain. The patient does not smoke and drinks 2–3 beers each weekend. His temperature is 36°C (96.8°F), pulse is 88/min, respirations are 18/min, and blood pressure is 130/80 mm Hg. Pulmonary examination shows no abnormalities. Abdominal examination shows a mildly distended abdomen with shifting dullness. The liver is palpated 2–3 cm below the right costal margin. When pressure is applied to the right upper quadrant, the patient's jugular veins become visibly distended for 15 seconds. The 2nd and 3rd metacarpophalangeal joints of both hands are tender to palpation. There is 2+ edema in the lower extremities. Which of the following is the most likely underlying cause of this patient's edema?
- A. Reduced glomerular filtration rate
- B. Macrovesicular steatosis of the liver
- C. Dermal deposition of glycosaminoglycans
- D. Impaired hepatic protein synthesis
- E. Impaired relaxation of the right ventricle (Correct Answer)
Right heart failure Explanation: ***Impaired relaxation of the right ventricle***
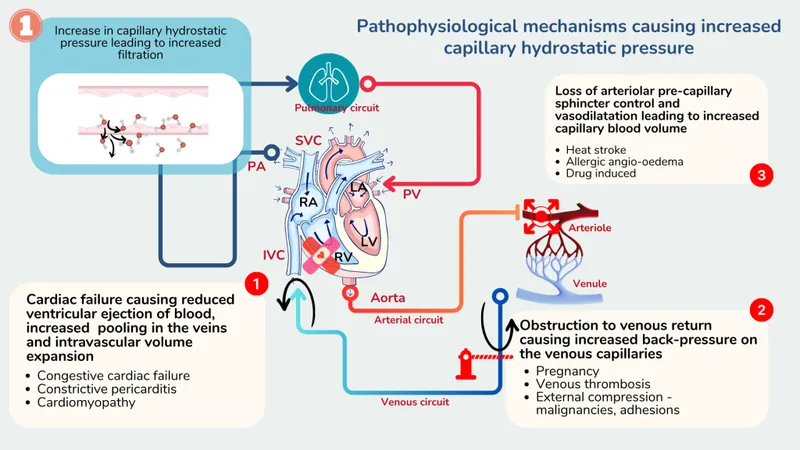
- The presence of **fatigue**, **abdominal discomfort**, **leg swelling**, **ascites with shifting dullness**, **hepatomegaly**, and particularly a positive **hepatojugular reflux** (jugular vein distension with RUQ pressure) strongly suggests **right-sided heart failure** due to impaired right ventricular relaxation, such as in **constrictive pericarditis** or **restrictive cardiomyopathy**.
- **Ibuprofen (NSAID) use** and **joint tenderness** in the metacarpophalangeal joints hint at a potential underlying inflammatory condition like rheumatoid arthritis, which can be associated with **amyloidosis** causing restrictive cardiomyopathy.
*Reduced glomerular filtration rate*
- While a reduced GFR can cause edema, it typically leads to **generalized anasarca** and is often associated with symptoms of **uremia** or significant proteinuria, which are not described.
- The prominent **hepatomegaly** and **positive hepatojugular reflux** are not primary features of renal-induced edema.
*Macrovesicular steatosis of the liver*
- **Macrovesicular steatosis** (fatty liver) itself does not directly cause significant edema or ascites unless it progresses to **cirrhosis**, which would manifest with more distinct signs of **liver failure** and portal hypertension.
- While the patient has some alcohol intake, the clinical picture with prominent hepatojugular reflux points more towards cardiac than isolated liver pathology at this stage.
*Dermal deposition of glycosaminoglycans*
- Dermal deposition of **glycosaminoglycans** is characteristic of **myxedema** (hypothyroidism), which causes non-pitting edema and is usually associated with other symptoms like **cold intolerance**, **bradycardia**, and **dry skin**, none of which are mentioned.
- The pitting edema observed in this patient is inconsistent with myxedema.
*Impaired hepatic protein synthesis*
- Impaired hepatic protein synthesis, leading to **hypoalbuminemia**, can cause edema and ascites due to reduced **oncotic pressure**.
- However, the significant **hepatomegaly** and the distinct **hepatojugular reflux** are more indicative of a circulatory issue affecting the liver, rather than primary intrinsic liver failure.
Right heart failure US Medical PG Question 2: A 38-year-old woman comes to the physician because of an 8-week history of shortness of breath and dull chest pain. She has a history of antiphospholipid syndrome. Physical examination shows jugular venous distention. Right heart catheterization shows a mean pulmonary arterial pressure of 30 mm Hg and a pulmonary capillary wedge pressure of 10 mm Hg. Further evaluation is most likely to show which of the following?
- A. Constriction of the renal afferent arteriole
- B. Hemosiderin-laden macrophages (Correct Answer)
- C. Mitral valve leaflet thickening
- D. Dilation of the coronary sinus
- E. Decreased left ventricular contractility
Right heart failure Explanation: ***Hemosiderin-laden macrophages***
- The patient's history of **antiphospholipid syndrome** and symptoms of **shortness of breath**, **chest pain**, and **jugular venous distention** suggest **pulmonary hypertension**.
- **Right heart catheterization** results (**mean pulmonary arterial pressure 30 mm Hg**, **pulmonary capillary wedge pressure 10 mm Hg**) confirm **pulmonary arterial hypertension (PAH)**, which, in the context of antiphospholipid syndrome, strongly indicates **chronic thromboembolic pulmonary hypertension (CTEPH)**. **Hemosiderin-laden macrophages** ("heart failure cells") are characteristic findings in the lungs of patients with chronic pulmonary congestion or recurrent pulmonary hemorrhage, which can occur in CTEPH due to the impact of chronic emboli on the pulmonary vasculature, leading to microhemorrhages and subsequent iron deposition.
*Constriction of the renal afferent arteriole*
- This is characteristic of conditions like **hypertensive nephrosclerosis** or involvement in systemic vasculitides, but it is not directly related to the primary pulmonary pathology described.
- While patients with antiphospholipid syndrome can develop renal complications (e.g., microangiopathy), it is not the most likely finding explained by the pulmonary symptoms and hemodynamic measurements.
*Mitral valve leaflet thickening*
- **Mitral valve leaflet thickening** and stenosis would lead to an **elevated pulmonary capillary wedge pressure (PCWP)**, indicating **post-capillary pulmonary hypertension**.
- The patient's PCWP is 10 mm Hg, which is within the normal range, ruling out significant left-sided heart disease as the primary cause of her pulmonary hypertension.
*Dilation of the coronary sinus*
- **Dilation of the coronary sinus** typically occurs due to conditions causing **elevated right atrial pressure** or **shunting from the left side of the heart**, such as an unroofed coronary sinus or persistent left superior vena cava.
- While right heart pressures are elevated, this finding is not a direct or specific consequence of the suspected CTEPH.
*Decreased left ventricular contractility*
- **Decreased left ventricular contractility** would lead to **elevated left ventricular end-diastolic pressure** and, consequently, an **elevated pulmonary capillary wedge pressure**.
- The normal PCWP of 10 mm Hg rules out significant left ventricular systolic dysfunction as the cause of the patient's pulmonary hypertension.
Right heart failure US Medical PG Question 3: Six days after undergoing a left hemicolectomy for colorectal carcinoma, a 59-year-old man collapses in the hospital hallway and is unconscious for 30 seconds. Afterwards, he complains of shortness of breath and chest pain with deep inhalation. He has hypertension and hyperlipidemia. He smoked one pack of cigarettes daily for 35 years but quit prior to admission to the hospital. He does not drink alcohol. He is in distress and appears ill. His temperature is 36.5°C (97.7°F), blood pressure is 80/50 mm Hg, and pulse is 135/min and weak. Oxygen saturation is 88% on room air. Physical examination shows elevated jugular venous distention. Cardiac examination shows a regular, rapid heart rate and a holosystolic murmur that increases during inspiration. His abdomen is soft and mildly tender to palpation around the surgical site. Examination of his extremities shows pitting edema of the left leg. His skin is cold and clammy. Further examination is most likely to reveal which of the following findings?
- A. Reduced regional ventricular wall motion
- B. Rapid, aberrant contractions of the atria
- C. Stenosis of the carotid arteries
- D. Dilated right ventricular cavity (Correct Answer)
- E. Anechoic space between pericardium and epicardium
Right heart failure Explanation: ***Dilated right ventricular cavity***
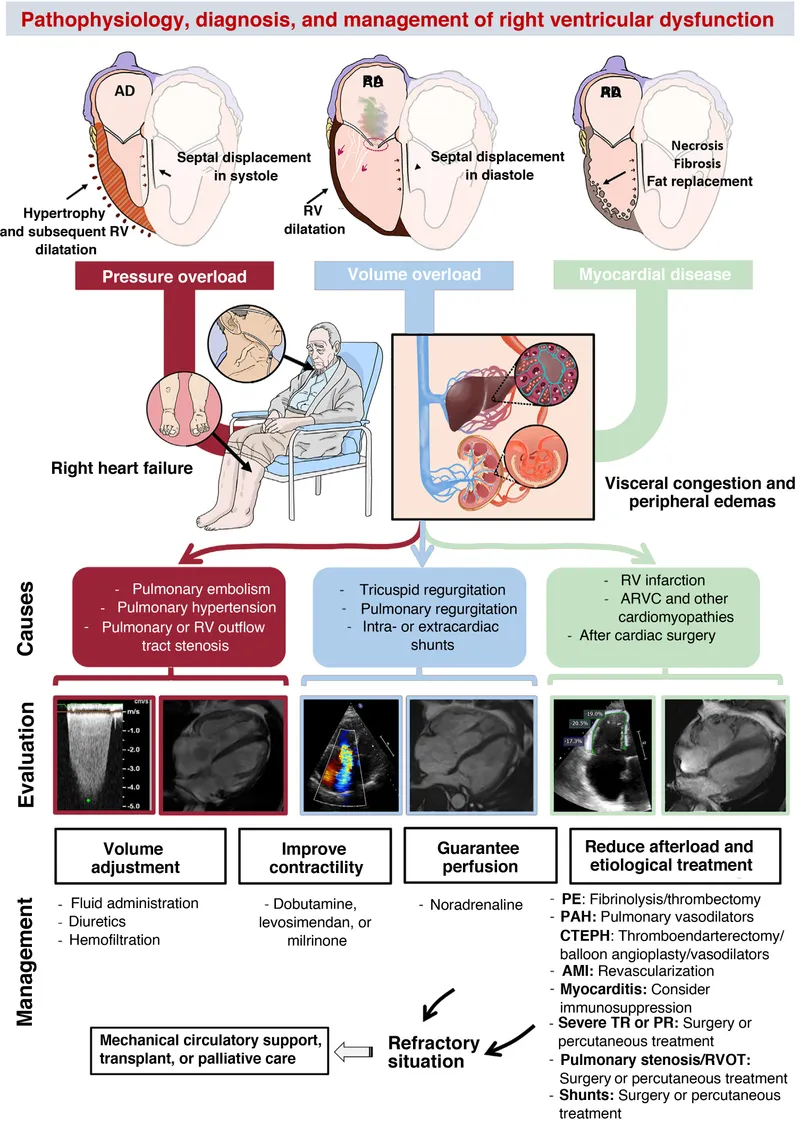
- The patient's symptoms (shortness of breath, chest pain with deep inspiration, hypotension, tachycardia, hypoxemia, elevated JVD, holosystolic murmur increasing with inspiration, and leg edema) are highly suggestive of **acute pulmonary embolism (PE)**.
- An acute PE can lead to increased pulmonary vascular resistance and **acute right ventricular (RV) overload**, causing RV dilation and dysfunction, which is often visible on echocardiography.
*Reduced regional ventricular wall motion*
- This finding is characteristic of **myocardial ischemia or infarction**, which typically presents with anginal chest pain and ECG changes; in this case, the chest pain is pleuritic and the overall picture points away from ischemia.
- While PE can cause RV dysfunction, the primary finding is RV overload and dilation, not necessarily isolated regional wall motion abnormalities often seen in left ventricular ischemia.
*Rapid, aberrant contractions of the atria*
- This describes **atrial fibrillation** or **atrial flutter**, which can occur in critically ill patients but is not the most direct consequence or expected finding from an acute pulmonary embolism in a previously stable patient.
- While atrial arrhythmias can be precipitated by acute stress, they are not the primary direct consequence of massive PE explaining these specific cardiovascular findings.
*Stenosis of the carotid arteries*
- **Carotid artery stenosis** is a risk factor for stroke but does not explain the acute cardiopulmonary collapse, hypoxemia, chest pain, and signs of right heart strain presented in the clinical scenario.
- This finding is unrelated to the acute presentation of shortness of breath, chest pain, and hemodynamic instability following surgery.
*Anechoic space between pericardium and epicardium*
- This finding represents a **pericardial effusion**, which can lead to cardiac tamponade if large and rapid in onset, but the associated holosystolic murmur increasing with inspiration and left leg edema are not typical for cardiac tamponade.
- While pericardial effusion can cause hypotension and shock, the specific constellation of symptoms, including pleuritic chest pain and signs of right heart strain, makes acute PE with RV dilation a more fitting diagnosis.
Right heart failure US Medical PG Question 4: A 70-year-old female with a history of congestive heart failure presents to the emergency room with dyspnea. She reports progressive difficulty breathing which began when she ran out of her furosemide and lisinopril prescriptions 1-2 weeks ago. She states the dyspnea is worse at night and when lying down. She denies any fever, cough, or GI symptoms. Her medication list reveals she is also taking digoxin. Physical exam is significant for normal vital signs, crackles at both lung bases and 2+ pitting edema of both legs. The resident orders the medical student to place the head of the patient's bed at 30 degrees. Additionally, he writes orders for the patient to be given furosemide, morphine, nitrates, and oxygen. Which of the following should be checked before starting this medication regimen?
- A. Basic metabolic panel (Correct Answer)
- B. Complete blood count
- C. Brain natriuretic peptide
- D. Urinalysis
- E. Chest x-ray
Right heart failure Explanation: ***Basic metabolic panel***
- A **basic metabolic panel (BMP)** is essential before starting this regimen to assess **kidney function** (creatinine, BUN) and **electrolytes**, particularly **potassium**.
- **Critical safety consideration**: The patient is on **digoxin**, which has significantly increased toxicity when potassium is low. Furosemide (a loop diuretic) causes potassium loss, making baseline potassium assessment essential to prevent life-threatening digoxin toxicity.
- **Renal function** must be checked before administering furosemide and lisinopril, both of which are renally cleared and can worsen renal function or accumulate in renal impairment.
*Complete blood count*
- A **complete blood count (CBC)** assesses for anemia, infection, and hematologic abnormalities.
- While potentially useful, it doesn't provide the immediate biochemical information (renal function, electrolytes) needed to safely initiate the prescribed heart failure medications, especially given the digoxin interaction risk.
*Brain natriuretic peptide*
- **Brain natriuretic peptide (BNP)** is a biomarker of heart failure severity and can help differentiate cardiac from non-cardiac causes of dyspnea.
- However, this patient's clinical presentation (orthopnea, bilateral crackles, pitting edema, medication non-adherence) already strongly confirms acute decompensated heart failure, making BNP less critical than checking renal function and electrolytes before medication administration.
*Urinalysis*
- **Urinalysis** can detect urinary tract infections, proteinuria, or other renal abnormalities.
- This patient's symptoms are classic for acute decompensated heart failure due to medication non-adherence, making urinalysis less immediately relevant for managing her acute presentation and medication safety.
*Chest x-ray*
- A **chest x-ray** can confirm pulmonary edema (cardiomegaly, cephalization, Kerley B lines) and rule out other causes of dyspnea like pneumonia or pneumothorax.
- While important for confirming the diagnosis, it is not required **before** starting medications and does not provide the critical biochemical information (renal function, electrolytes) needed to safely administer diuretics and ACE inhibitors in a patient on digoxin.
Right heart failure US Medical PG Question 5: A 56-year-old man comes to the physician for a 5-month history of progressive bilateral ankle swelling and shortness of breath on exertion. He can no longer walk up the stairs to his bedroom without taking a break. He also constantly feels tired during the day. His wife reports that he snores at night and that he sometimes chokes in his sleep. The patient has smoked 1 pack of cigarettes daily for 25 years. He has a history of hypertension treated with enalapril. His pulse is 72/min, respirations are 16/min, and blood pressure is 145/95 mmHg. There is jugular venous distention. The lungs are clear to auscultation bilaterally. The extremities are warm and well perfused. There is 2+ lower extremity edema bilaterally. ECG shows right axis deviation. Which of the following is the most likely cause of this patient's condition?
- A. Alveolar destruction
- B. Ischemic heart disease
- C. Left ventricular hypertrophy
- D. Chronic hypoxia (Correct Answer)
- E. Chronic kidney damage
Right heart failure Explanation: ***Chronic hypoxia***
- The patient's history of **heavy smoking**, snoring with choking episodes suggestive of **sleep apnea**, and symptoms of **right-sided heart failure** (bilateral ankle swelling, JVD, right axis deviation on ECG) point to chronic hypoxia as the underlying cause.
- **Chronic hypoxia** leads to **pulmonary vasoconstriction** and subsequent pulmonary hypertension, which eventually causes **right ventricular hypertrophy** and failure (cor pulmonale).
*Alveolar destruction*
- While **alveolar destruction** (emphysema) can lead to hypoxia in smokers, the normal auscultation of the lungs makes this less likely to be the primary cause of his symptoms, although it could contribute.
- The **ECG showing right axis deviation** more strongly suggests a primary pulmonary vascular issue or sustained right ventricular strain rather than solely alveolar destruction.
*Ischemic heart disease*
- Although the patient has risk factors for **ischemic heart disease** (smoking, hypertension), his symptoms and signs (bilateral ankle swelling, JVD, right axis deviation, clear lungs) are more consistent with isolated **right-sided heart failure** due to a pulmonary issue, not acute or chronic ischemia.
- **Left-sided heart failure** due to ischemic heart disease would typically present with pulmonary congestion (crackles, dyspnea) before isolated right-sided symptoms appear.
*Left ventricular hypertrophy*
- **Left ventricular hypertrophy** (LVH) is often seen in hypertension, but the patient's presentation of **right-sided heart failure** symptoms (JVD, edema, right axis deviation) with clear lungs does not directly point to LVH as the primary cause of his current condition.
- While his hypertension could lead to LVH, the symptoms described are more consistent with **pulmonary hypertension** and cor pulmonale.
*Chronic kidney damage*
- **Chronic kidney damage** would explain the bilateral ankle swelling, but it would typically be associated with other signs like elevated creatinine, uremia, or proteinuria, which are not mentioned.
- It would also not explain the **shortness of breath on exertion**, **snoring with choking**, or the **right axis deviation** on ECG, which directly points to a cardiac or pulmonary issue.
Right heart failure US Medical PG Question 6: A 70-year-old Caucasian male visits your office regularly for treatment of New York Heart association class IV congestive heart failure. Which of the following medications would you add to this man's drug regimen in order to improve his overall survival?
- A. Spironolactone (Correct Answer)
- B. Furosemide
- C. Amiloride
- D. Acetazolamide
- E. Hydrochlorothiazide
Right heart failure Explanation: ***Spironolactone***
- **Spironolactone** is an **aldosterone antagonist** that has been shown to reduce mortality and morbidity in patients with **NYHA Class III and IV heart failure**.
- It works by blocking the harmful effects of **aldosterone** on the heart, such as **fibrosis** and remodeling, improving cardiac function and survival.
*Furosemide*
- **Furosemide** is a **loop diuretic** primarily used to relieve **symptoms of congestion** (edema, dyspnea) in heart failure by promoting fluid excretion.
- While it improves symptoms, **furosemide** alone does not significantly improve long-term survival in patients with heart failure.
*Amiloride*
- **Amiloride** is a **potassium-sparing diuretic** that works by blocking sodium channels in the collecting duct, leading to modest diuresis.
- It is often used to prevent **hypokalemia** caused by other diuretics but does not have the same proven mortality benefit in heart failure as spironolactone.
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** primarily used for glaucoma, metabolic alkalosis, and altitude sickness.
- It has a weaker diuretic effect and is not a commonly used or recommended medication for improving long-term survival in patients with heart failure.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** primarily used for hypertension and mild to moderate edema.
- While it can help manage fluid retention, it does not offer the same mortality benefit in advanced heart failure as aldosterone antagonists like spironolactone.
Right heart failure US Medical PG Question 7: A 64-year-old male with a history of coronary artery disease, hypertension, hyperlipidemia, and type II diabetes presents to his primary care physician with increasing shortness of breath and ankle swelling over the past month. Which of the following findings is more likely to be seen in left-sided heart failure and less likely to be seen in right-sided heart failure?
- A. Abdominal fullness
- B. Basilar crackles on pulmonary auscultation (Correct Answer)
- C. Hepatojugular reflex
- D. Increased ejection fraction on echocardiogram
- E. Lower extremity edema
Right heart failure Explanation: ***Basilar crackles on pulmonary auscultation***
- **Left-sided heart failure** leads to increased pressure in the pulmonary veins, causing fluid to leak into the **pulmonary interstitium and alveoli**, manifesting as **basilar crackles** on auscultation.
- This symptom is a direct result of **pulmonary congestion** and edema, which is not characteristic of isolated right-sided heart failure.
*Abdominal fullness*
- **Abdominal fullness** is typically a symptom of **right-sided heart failure**, due to **venous congestion** in the splanchnic circulation, leading to hepatomegaly and ascites.
- While it can occur in severe biventricular failure, it is not a primary or earlier sign of isolated left-sided heart failure.
*Hepatojugular reflex*
- The **hepatojugular reflex** is a sign of **right ventricular dysfunction** and **elevated right atrial pressure**, indicating systemic venous congestion.
- It is elicited by applying pressure to the liver, which causes a temporary increase in jugular venous distention.
*Increased ejection fraction on echocardiogram*
- **Heart failure**, whether left- or right-sided, is characterized by a **reduced (or preserved but not increased)** ejection fraction, reflecting impaired pumping ability.
- An **increased ejection fraction** would indicate supra-normal cardiac function and is not associated with heart failure.
*Lower extremity edema*
- **Lower extremity edema** is a hallmark symptom of **right-sided heart failure**, as venous congestion leads to fluid accumulation in the peripheral tissues.
- While present in biventricular failure, it is not a primary or early symptom of isolated left-sided heart failure.
Right heart failure US Medical PG Question 8: A 74-year-old woman comes to the physician for a follow-up examination. Eight months ago, she underwent an emergency cardiac catheterization with stenting for myocardial infarction. At the time of discharge, her heart configuration was normal, end-diastolic volume was 300 mL and ejection fraction was 51%. For the past 8 weeks she has noticed increasing shortness of breath while playing with her 2-year-old grandson. She feels otherwise well. She has arterial hypertension, coronary artery disease, and hypercholesterolemia. She admits to rarely taking her medication as she usually feels well and has no symptoms. Her temperature is 37.3°C (99.1°F), pulse is 93/min, and blood pressure is 142/93 mm Hg. Examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. ECG shows broad, deep Q waves and T-wave inversion. Echocardiography shows left ventricular dilation and an end-diastolic volume of 370 mL; Ejection fraction is 40%. Which of the following is most likely to have prevented this patient's worsening of ventricular function?
- A. Nifedipine
- B. Atorvastatin
- C. Enalapril (Correct Answer)
- D. Diltiazem
- E. Digoxin
Right heart failure Explanation: ***Enalapril***
- Enalapril, an **ACE inhibitor**, would prevent ventricular remodeling and worsening heart failure by blocking the **renin-angiotensin-aldosterone system (RAAS)**.
- RAAS activation after an MI leads to **ventricular hypertrophy** and dilation, which ACE inhibitors effectively counteract.
*Nifedipine*
- **Nifedipine is a dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It does not have the same proven benefits in preventing ventricular remodeling or improving outcomes in **heart failure** as ACE inhibitors.
*Atorvastatin*
- **Atorvastatin is a HMG-CoA reductase inhibitor** that lowers cholesterol and stabilizes plaques.
- While essential for **secondary prevention of cardiovascular events**, it does not directly prevent ventricular remodeling or improve ejection fraction in the setting of heart failure.
*Diltiazem*
- **Diltiazem is a non-dihydropyridine calcium channel blocker** that reduces heart rate and contractility.
- It is generally **contraindicated** in patients with **reduced ejection fraction heart failure** as it can worsen cardiac function.
*Digoxin*
- **Digoxin is a positive inotrope** that can improve symptoms in heart failure but does not prevent ventricular remodeling or improve survival.
- It has a **narrow therapeutic window** and is primarily used for symptom control in advanced heart failure or for rate control in atrial fibrillation.
Right heart failure US Medical PG Question 9: A 78-year-old man presents to the clinic complaining of shortness of breath at rest and with exertion. He also complains of difficulty breathing while lying down. He also is concerned because he startles from sleep and feels like he is choking. These symptoms have been bothering him for the last several weeks and they are getting worse. He has been afebrile with no known sick contacts. 6 months ago, he had an acute myocardial infarction from which he recovered and until recently had felt well. He has a history of hyperlipidemia for which he takes atorvastatin. His temperature is 37.0°C (98.6°F), the pulse is 85/min, the respiratory rate is 14/min, and the blood pressure is 110/75 mm Hg. On physical examination, his heart has a regular rate and rhythm. He has bilateral crackles in both lungs. An echocardiogram is performed and shows a left ventricular ejection fraction of 33%. What medication should be started?
- A. Captopril (Correct Answer)
- B. Levofloxacin
- C. Verapamil
- D. Niacin
- E. Nitroglycerin
Right heart failure Explanation: ***Captopril***
- The patient presents with classic symptoms of **heart failure** (shortness of breath at rest and with exertion, orthopnea, paroxysmal nocturnal dyspnea), a history of **myocardial infarction**, and a **reduced left ventricular ejection fraction (LVEF) of 33%**.
- **ACE inhibitors** like captopril are first-line agents for heart failure with reduced ejection fraction (HFrEF) as they **improve survival**, reduce hospitalizations, and alleviate symptoms by decreasing **afterload** and **preload**, and preventing cardiac remodeling.
*Levofloxacin*
- This is an **antibiotic** used to treat bacterial infections.
- While crackles can be present in pneumonia, the patient is **afebrile**, has no sick contacts, and the clinical picture, including orthopnea and paroxysmal nocturnal dyspnea, points strongly to **heart failure**, not infection.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** predominantly used for rate control in arrhythmias or to treat hypertension and angina.
- It has a negative **inotropic effect** and can **worsen heart failure** in patients with reduced ejection fraction, making it contraindicated in this case.
*Niacin*
- **Niacin** is used to lower **LDL cholesterol** and raise **HDL cholesterol**, often for dyslipidemia.
- While the patient has a history of hyperlipidemia, his acute symptoms and low ejection fraction indicate a need for **heart failure treatment**, not additional lipid management.
*Nitroglycerin*
- **Nitroglycerin** is a **vasodilator** primarily used for **angina** or in acute heart failure to reduce preload and afterload.
- While it might provide temporary symptomatic relief in acute decompensated heart failure, it's not a long-term foundational therapy like ACE inhibitors for **chronic HFrEF** to improve survival and prevent progression.
Right heart failure US Medical PG Question 10: A 61-year-old man comes to the physician for shortness of breath and chest discomfort that is becoming progressively worse. He has had increasing problems exerting himself for the past 5 years. He is now unable to walk more than 50 m on level terrain without stopping and mostly rests at home. He has smoked 1–2 packs of cigarettes daily for 40 years. He appears distressed. His pulse is 85/min, blood pressure is 140/80 mm Hg, and respirations are 25/min. Physical examination shows a plethoric face and distended jugular veins. Bilateral wheezing is heard on auscultation of the lungs. There is yellow discoloration of the fingers on the right hand and 2+ lower extremity edema. Which of the following is the most likely cause of this patient's symptoms?
- A. Coronary plaque deposits
- B. Chronic respiratory acidosis
- C. Increased left atrial pressure
- D. Elevated pulmonary artery pressure (Correct Answer)
- E. Decreased intrathoracic gas volume
Right heart failure Explanation: ***Elevated pulmonary artery pressure***
* The patient's long history of **heavy smoking** and progressive exertional dyspnea, wheezing, plethoric face, distended jugular veins, and lower extremity edema are highly suggestive of **cor pulmonale** due to chronic obstructive pulmonary disease (COPD).
* **COPD** leads to chronic hypoxia and vasoconstriction of pulmonary arteries, increasing **pulmonary artery pressure**, which eventually causes right ventricular failure (cor pulmonale) manifested by the systemic venous congestion symptoms.
*Coronary plaque deposits*
* While **coronary plaque deposits** can lead to chest discomfort, the prominent signs of **right-sided heart failure** (jugular venous distension, lower extremity edema) and chronic respiratory symptoms point away from isolated coronary artery disease as the primary cause.
* The patient's wheezing and long smoking history are more indicative of a **respiratory rather than purely cardiac origin** for his dyspnea.
*Chronic respiratory acidosis*
* **Chronic respiratory acidosis** can occur in severe COPD, but it is a **consequence** of impaired gas exchange, not the primary cause of the patient's presenting symptoms of shortness of breath and chest discomfort with signs of overt heart failure.
* While important, acidosis alone does not explain the **physical findings of right heart failure** such as jugular venous distention and peripheral edema.
*Increased left atrial pressure*
* **Increased left atrial pressure** is characteristic of **left-sided heart failure**, which typically presents with pulmonary edema (rales, pink frothy sputum) and symptoms like orthopnea and paroxysmal nocturnal dyspnea.
* This patient's symptoms, particularly the **plethoric face, distended jugular veins, and lower extremity edema**, are classic signs of **right-sided heart failure**, not left-sided heart failure.
*Decreased intrathoracic gas volume*
* **Decreased intrathoracic gas volume** is usually seen in restrictive lung diseases (e.g., pulmonary fibrosis), not obstructive diseases like COPD, where gas trapping leads to **increased intrathoracic gas volume**.
* The patient's wheezing and long smoking history are classic for **obstructive lung disease**, which is associated with air trapping and hyperinflation, rather than decreased lung volumes.
More Right heart failure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.