Device therapy for heart failure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Device therapy for heart failure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Device therapy for heart failure US Medical PG Question 1: A 71-year old man is brought to the emergency department because of progressively worsening shortness of breath and fatigue for 3 days. During the last month, he has also noticed dark colored urine. He had an upper respiratory infection 6 weeks ago. He underwent a cholecystectomy at the age of 30 years. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. He immigrated to the US from Italy 50 years ago. Current medications include simvastatin, lisinopril, and metformin. He appears pale. His temperature is 37.1°C (98.8°F), pulse is 96/min, respirations are 21/min, and blood pressure is 150/80 mm Hg. Auscultation of the heart shows a grade 4/6 systolic murmur over the right second intercostal space that radiates to the carotids. Laboratory studies show:
Leukocyte count 9,000/mm3
Hemoglobin 8.3 g/dL
Hematocrit 24%
Platelet count 180,000/mm3
LDH 212 U/L
Haptoglobin 15 mg/dL (N=41–165)
Serum
Na+ 138 mEq/L
K+ 4.5 mEq/L
CL- 102 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 20 mg/dL
Creatinine 1.2 mg/dL
Total bilirubin 1.8 mg/dL
Stool testing for occult blood is negative. Direct Coombs test is negative. Echocardiography shows an aortic jet velocity of 4.2 m/s and a mean pressure gradient of 46 mm Hg. Which of the following is the most appropriate next step in management to treat this patient's anemia?
- A. Aortic valve replacement (Correct Answer)
- B. Administration of corticosteroids
- C. Discontinuation of medication
- D. Administration of hydroxyurea
- E. Supplementation with iron
Device therapy for heart failure Explanation: ***Aortic valve replacement***
- The patient's **severe aortic stenosis** (aortic jet velocity >4.0 m/s and mean pressure gradient >40 mmHg) is causing **shear stress** on red blood cells, leading to **microangiopathic hemolytic anemia**. This is characterized by low hemoglobin, high LDH, low haptoglobin, and negative Coombs test.
- **Aortic valve replacement** is the definitive treatment to reduce the shear stress, resolve the hemolysis, and improve the patient's symptoms of anemia and heart failure.
*Administration of corticosteroids*
- Corticosteroids are primarily used in **autoimmune hemolytic anemia** (positive Coombs test), which is not the case here as the direct Coombs test is negative.
- They would not address the underlying **mechanical destruction of red blood cells** due to aortic stenosis.
*Discontinuation of medication*
- The patient's current medications (simvastatin, lisinopril, metformin) are for managing his chronic conditions and are **not associated with hemolytic anemia**. Discontinuing them would be inappropriate and potentially harmful.
- There is no evidence to suggest a **drug-induced hemolytic anemia** in this case.
*Administration of hydroxyurea*
- Hydroxyurea is used in conditions like **sickle cell anemia** or **polycythemia vera** to modify red blood cell production or reduce cell counts, respectively.
- It has no role in treating **mechanical hemolytic anemia** caused by valvular heart disease.
*Supplementation with iron*
- While the patient has anemia, it is a **hemolytic anemia**, not an iron deficiency anemia, as indicated by the low haptoglobin and elevated LDH.
- Iron supplementation would **not stop the destruction of red blood cells** caused by the turbulent flow across the aortic valve.
Device therapy for heart failure US Medical PG Question 2: Two days after admission for myocardial infarction and subsequent coronary angioplasty, a 65-year-old man becomes distressed and diaphoretic in the cardiac intensive care unit. Suddenly he is no longer responsive. Pulse oximetry does not show a tracing. He has a history of hypertension and depression. Prior to his admission, his medication included ramipril and aripiprazole. Examination shows no carotid pulse. An ECG is shown. After beginning chest compressions, which of the following is the most appropriate step in management of the patient?
- A. Intravenous procainamide
- B. Cardiac catheterization
- C. Intravenous amiodarone
- D. Intravenous magnesium sulfate
- E. Defibrillation (Correct Answer)
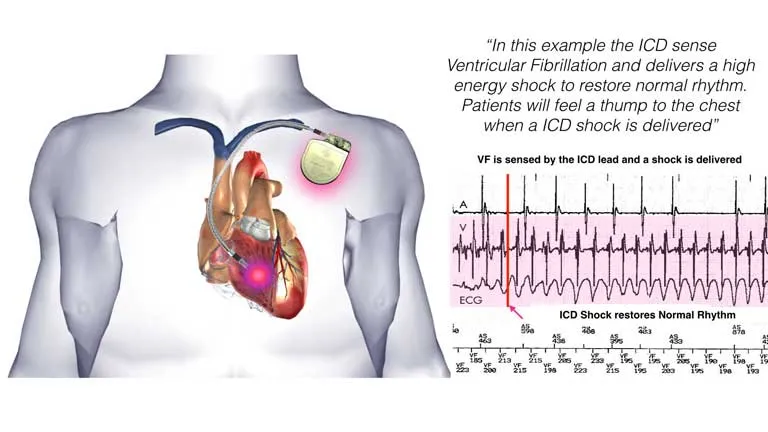
Device therapy for heart failure Explanation: ***Defibrillation***
- The ECG shows a **wide complex tachycardia** consistent with either **ventricular fibrillation (VF)** or **pulseless ventricular tachycardia (VT)**.
- In a patient who is **unresponsive and pulseless**, both VF and pulseless VT are treated identically with **immediate unsynchronized defibrillation** after initiating CPR, according to **ACLS guidelines**.
- **Defibrillation** is the definitive treatment to restore a perfusing rhythm and is the priority intervention after chest compressions have begun.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic drug used for certain types of **stable ventricular tachycardia** or wide-complex tachycardia of uncertain type when the patient has a pulse.
- It is **contraindicated** in pulseless arrhythmias like VF or pulseless VT, where electrical therapy (defibrillation) is paramount.
- Administration would cause dangerous delay in definitive treatment.
*Cardiac catheterization*
- **Cardiac catheterization** is an invasive diagnostic and interventional procedure typically performed to evaluate and treat coronary artery disease.
- It is **not an immediate life-saving intervention** for a patient in **cardiac arrest**, which requires immediate electrical therapy.
- Catheterization may be considered after return of spontaneous circulation (ROSC) to address underlying ischemia.
*Intravenous amiodarone*
- **Amiodarone** is an antiarrhythmic agent used in **VF/pulseless VT that is refractory to initial defibrillation attempts** and after epinephrine administration.
- It is administered **after initial defibrillation attempts have failed**, not as the primary or first-line treatment.
- The ACLS algorithm recommends amiodarone after the third shock if VF/pulseless VT persists.
*Intravenous magnesium sulfate*
- **Magnesium sulfate** is the treatment of choice for **Torsades de Pointes**, a polymorphic ventricular tachycardia often associated with **prolonged QT interval**.
- The clinical presentation and ECG do not suggest Torsades de Pointes, and magnesium is not indicated as the initial treatment for VF or monomorphic VT.
- Magnesium may also be considered for refractory VF/VT with suspected hypomagnesemia.
Device therapy for heart failure US Medical PG Question 3: A 32-year-old woman comes to the physician because of worsening fatigue and shortness of breath. Her symptoms began 8 months ago and have progressively worsened since then. She had recurrent episodes of joint pain and fever during childhood. She does not smoke or drink alcohol. She emigrated from the Congo with her parents when she was 12 years old. Her temperature is 37.4°C (99.3°F), pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/90 mm Hg. There is an opening snap followed by a diastolic murmur at the fifth left intercostal space in the midclavicular line. If left untreated, this patient is at greatest risk for which of the following complications?
- A. Pulmonary edema
- B. Systemic thromboembolism
- C. Pulmonary hypertension
- D. Right heart failure
- E. Atrial fibrillation (Correct Answer)
Device therapy for heart failure Explanation: ***Atrial fibrillation***
- The patient's history of **recurrent joint pain and fever in childhood**, originating from the Congo, points towards a diagnosis of **rheumatic heart disease** causing **mitral stenosis**.
- **Mitral stenosis** leads to increased left atrial pressure and dilation, which are significant risk factors for developing **atrial fibrillation**. The presence of an **opening snap and diastolic murmur** further supports mitral stenosis.
*Pulmonary edema*
- While **pulmonary edema** can be a complication of severe **mitral stenosis** due to increased left atrial pressure and elevated pulmonary venous pressures, it is often precipitated by an acute event or occurs later in the disease course.
- **Atrial fibrillation** significantly exacerbates intra-atrial pressures and worsens symptoms, often preceding or coexisting with pulmonary edema, making it a more immediate and common long-term risk.
*Systemic thromboembolism*
- **Systemic thromboembolism** is a serious complication of untreated **mitral stenosis**, particularly when complicated by **atrial fibrillation**, due to stasis of blood in the dilated left atrium.
- However, the primary mechanism leading to an increased risk of thromboembolism in this context is the development of **atrial fibrillation**, which sets the stage for clot formation.
*Pulmonary hypertension*
- **Pulmonary hypertension** is a common consequence of chronic **mitral stenosis** as elevated left atrial pressures are transmitted to the pulmonary vasculature.
- While a severe complication that contributes to symptoms like shortness of breath, **atrial fibrillation** is a critical arrhythmia that can both worsen pulmonary hypertension and lead to other life-threatening complications.
*Right heart failure*
- **Right heart failure** eventually develops in severe, long-standing **mitral stenosis** due to sustained **pulmonary hypertension**, which increases the afterload on the right ventricle.
- While it represents an advanced stage of the disease, **atrial fibrillation** is a more immediate and common rhythm disturbance that contributes to the hemodynamic compromise and often predates overt right heart failure.
Device therapy for heart failure US Medical PG Question 4: A 72-year-old man is taken to the emergency room after losing consciousness. According to his wife, he suddenly complained of fluttering in his chest, lightheadedness, and profuse sweating while walking to the grocery store. He then turned gray, lost consciousness, and collapsed onto the ground. His medical history is significant for a prior anterior wall myocardial infarction 2 years ago that was complicated by severe left ventricular systolic dysfunction. His blood pressure is 80/50 mm Hg, the temperature is 36.7°C (98.0°F), and the carotid pulse is not palpable. An ECG was obtained and the results are shown in the picture. Cardiopulmonary resuscitation is initiated and the patient is cardioverted to sinus rhythm with an external defibrillator. The patient regains consciousness and states there was no antecedent chest discomfort. Cardiac enzymes are negative and serum electrolytes are normal. Which of the following is the best next step for this patient?
- A. Intravenous magnesium sulphate
- B. Intravenous adenosine
- C. Implantable cardioverter-defibrillator (Correct Answer)
- D. Intravenous metoprolol
- E. Temporary or permanent cardiac pacing
Device therapy for heart failure Explanation: ***Implantable cardioverter-defibrillator***
- The patient experienced **sudden cardiac arrest (SCA)** due to a **lethal ventricular arrhythmia (ventricular tachycardia progressing to ventricular fibrillation)**, suggested by the syncopal episode, unrecordable pulse, and successful defibrillation.
- Given the history of severe **left ventricular systolic dysfunction** (LVEF <35-40%) post-MI, he is at high risk for recurrence, making an **ICD** the most appropriate intervention for secondary prevention of SCA.
*Intravenous magnesium sulphate*
- **Magnesium sulfate** is primarily used for the treatment of **Torsades de Pointes**, a polymorphic VT often associated with a prolonged QT interval.
- The provided ECG (though not visible here, the clinical context implies a monomorphic VT or VF) and history do not specifically suggest Torsades de Pointes.
*Intravenous adenosine*
- **Adenosine** is the drug of choice for terminating **supraventricular tachycardias (SVTs)** by transiently blocking the AV node.
- It is **contraindicated** in wide-complex tachycardias of uncertain origin, especially in patients with structural heart disease, as it can worsen ventricular arrhythmias.
*Intravenous metoprolol*
- **Beta-blockers** like metoprolol are used to slow heart rate, reduce myocardial oxygen demand, and can be helpful in some forms of VT, but they are not the definitive treatment for **hemodynamically unstable** VT or for preventing future SCA in a patient with severe LV dysfunction.
- Administering a beta-blocker during an acute, unstable event could worsen hypotension.
*Temporary or permanent cardiac pacing*
- **Cardiac pacing** is indicated for **bradyarrhythmias** or some forms of **tachycardia** (e.g., overdrive pacing for recurrent VT), but it is not the primary treatment for preventing SCA from ventricular fibrillation in a patient with severe LV dysfunction like this.
- The patient's presentation was due to a fast, lethal arrhythmia, not a slow rhythm.
Device therapy for heart failure US Medical PG Question 5: You are interested in studying the etiology of heart failure reduced ejection fraction (HFrEF) and attempt to construct an appropriate design study. Specifically, you wish to look for potential causality between dietary glucose consumption and HFrEF. Which of the following study designs would allow you to assess for and determine this causality?
- A. Cross-sectional study
- B. Case series
- C. Cohort study (Correct Answer)
- D. Case-control study
- E. Randomized controlled trial
Device therapy for heart failure Explanation: ***Cohort study***
- A **cohort study** observes a group of individuals over time to identify risk factors and outcomes, allowing for the assessment of **temporal relationships** between exposure (dietary glucose) and outcome (HFrEF).
- This design is suitable for establishing a potential **causal link** as it tracks participants from exposure to outcome, enabling the calculation of incidence rates and relative risks.
*Cross-sectional study*
- A **cross-sectional study** measures exposure and outcome simultaneously at a single point in time, making it impossible to determine the **temporal sequence** of events.
- This design can only identify **associations** or correlations, not causation, as it cannot establish whether high glucose consumption preceded HFrEF.
*Case series*
- A **case series** describes characteristics of a group of patients with a particular disease or exposure, often to highlight unusual clinical features, but it lacks a **comparison group**.
- It cannot assess causality because it does not provide information on the frequency of exposure in healthy individuals or the incidence of the disease in unexposed individuals.
*Case-control study*
- A **case-control study** compares individuals with the outcome (cases) to those without the outcome (controls) to determine past exposures, which makes it prone to **recall bias**.
- While it can suggest associations, it cannot definitively establish a temporal relationship or causation as the outcome is already known when exposure is assessed.
*Randomized controlled trial*
- A **randomized controlled trial (RCT)** is the gold standard for establishing causation by randomly assigning participants to an intervention or control group, but it may not be ethical or feasible for studying long-term dietary exposures and chronic diseases like HFrEF due to the long follow-up period and complexity of diet.
- While ideal for causality, directly controlling and randomizing dietary glucose intake over decades to observe HFrEF development might be practically challenging or unethical.
Device therapy for heart failure US Medical PG Question 6: A 71-year-old woman with a past medical history of type 2 diabetes, hypercholesterolemia, and hypertension was admitted to the hospital 8 hours ago with substernal chest pain for management of acute non-ST-elevated myocardial infarction (NSTEMI). The ECG findings noted by ST-depressions and T-wave inversions on anterolateral leads, which is also accompanied by elevated cardiac enzymes. Upon diagnosis, management with inhaled oxygen therapy, beta-blockers and aspirin, and low-molecular-weight heparin therapy were initiated, and she was placed on bed rest with continuous electrocardiographic monitoring. Since admission, she required 2 doses of sublingual nitroglycerin for recurrent angina, and the repeat troponin levels continued to rise. Given her risk factors, plans were made for early coronary angiography. The telemetry nurse calls the on-call physician because of her concern with the patient's mild confusion and increasing need for supplemental oxygen. At bedside evaluation, The vital signs include: heart rate 122/min, blood pressure 89/40 mm Hg, and the pulse oximetry is 91% on 6L of oxygen by nasal cannula. The telemetry and a repeat ECG show sinus tachycardia. She is breathing rapidly, appears confused, and complains of shortness of breath. On physical exam, the skin is cool and clammy and appears pale and dull. She has diffuse bilateral pulmonary crackles, and an S3 gallop is noted on chest auscultation with no new murmurs. She has jugular venous distention to the jaw-line, rapid and faint radial pulses, and 1+ dependent edema. She is immediately transferred to the intensive care unit for respiratory support and precautions for airway security. The bedside sonography shows abnormal hypodynamic anterior wall movement and an ejection fraction of 20%, but no evidence of mitral regurgitation or ventricular shunt. The chest X-ray demonstrates cephalization of pulmonary veins and pulmonary edema. What is the most appropriate next step in the stabilization of this patient?
- A. Obtain blood cultures and start preliminary broad-spectrum antibiotics
- B. Start intravenous fluids and epinephrine therapy
- C. Intubate the patient and perform an emergency cardiocentesis
- D. Initiate dopamine therapy and diuresis (Correct Answer)
- E. Insert two large-bore intravenous catheters and start rapid fluid resuscitation
Device therapy for heart failure Explanation: ***Initiate dopamine therapy and diuresis***
- This patient is presenting with **cardiogenic shock** secondary to extensive NSTEMI, characterized by **hypotension**, signs of **end-organ hypoperfusion** (confusion, cool clammy skin), **pulmonary edema** (crackles, dyspnea, elevated jugular venous pressure), and **severely reduced ejection fraction**. Dopamine is a vasopressor that can increase cardiac output and blood pressure.
- **Diuresis** with loop diuretics such as furosemide is crucial to reduce the fluid overload contributing to the pulmonary edema and jugular venous distention.
*Obtain blood cultures and start preliminary broad-spectrum antibiotics*
- While infection is a concern in critically ill patients, there are **no signs of infection** in this clinical presentation. The patient's symptoms are clearly attributable to acute cardiac decompensation.
- A delay in treating cardiogenic shock to investigate for infection would be detrimental and potentially fatal.
*Start intravenous fluids and epinephrine therapy*
- Intravenous fluids would **worsen the existing pulmonary edema and fluid overload** in a patient with an ejection fraction of 20% and clinical signs of volume overload (crackles, JVD, S3 gallop).
- Epinephrine is a potent vasopressor but is generally reserved for more severe shock refractory to other inotropes, or in cases of **cardiac arrest**, not typically first-line for cardiogenic shock with significant pulmonary congestion.
*Intubate the patient and perform an emergency cardiocentesis*
- While the patient is confused and has respiratory distress, **intubation** should be considered after hemodynamic stabilization, if respiratory failure persists or worsens.
- **Cardiocentesis** is indicated for **cardiac tamponade**, which is not supported by the absence of an effusion on bedside sonography and the finding of hypodynamic anterior wall movement, which points to pump failure.
*Insert two large-bore intravenous catheters and start rapid fluid resuscitation*
- This patient is in **cardiogenic shock with clear evidence of fluid overload**, including pulmonary edema and elevated jugular venous pressure.
- **Rapid fluid resuscitation would exacerbate heart failure** and worsen respiratory compromise due to increased preload.
Device therapy for heart failure US Medical PG Question 7: A 62-year-old man with a past medical history of previous myocardial infarction, angina, hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, and below knee amputation has developed new chest pain. His medication includes insulin, hydrochlorothiazide, lisinopril, metoprolol, daily aspirin, atorvastatin, and nitroglycerin as needed. His vitals include: blood pressure 135/87 mm Hg, pulse 52/min, and respirations 17/min. Coronary arteriography shows a reduced ejection fraction, a 65% stenosis of the left anterior descending artery, and a 75% stenosis of the left circumflex artery. Which of the following is the recommended treatment for the patient?
- A. Increased beta blocker dosage
- B. Coronary artery bypass grafting (CABG) (Correct Answer)
- C. Angioplasty with stent placement
- D. Extended release nitrate therapy
- E. Heparin
Device therapy for heart failure Explanation: ***Coronary artery bypass grafting (CABG)***
- This patient has complex **multivessel coronary artery disease** (LAD and circumflex stenosis) with a **reduced ejection fraction** and a history of multiple comorbidities, making CABG the preferred revascularization strategy for improved outcomes.
- CABG offers a more complete revascularization in patients with significant disease burden and reduced left ventricular function, leading to better long-term survival and symptom relief compared to PCI in this population.
*Increased beta blocker dosage*
- The patient's current heart rate is 52/min, which is already at the lower end of the target range for beta-blocker therapy in cardiac patients, and further increasing the dose could lead to **bradycardia** and worsening symptoms.
- While beta-blockers are crucial for managing angina and improving outcomes post-MI, increasing the dose wouldn't address the underlying anatomical severe multi-vessel coronary artery disease.
*Angioplasty with stent placement*
- Although PCI (angioplasty with stent placement) can be used for coronary stenosis, in patients with **multivessel disease**, **reduced ejection fraction**, and **diabetes mellitus**, CABG generally offers superior long-term results and survival benefits.
- The complexity of the lesions (65% LAD, 75% circumflex) in a patient with significant comorbidities and extensive atherosclerotic disease makes PCI a less optimal choice here.
*Extended release nitrate therapy*
- Nitrates primarily provide **symptomatic relief** by causing vasodilation, but they do not address the severe underlying coronary stenoses or improve long-term outcomes in patients with complex, multivessel disease.
- The patient is already on PRN nitroglycerin, and while extended-release nitrates could help with angina, they are not a definitive treatment for significant arterial blockages requiring revascularization.
*Heparin*
- Heparin is an **anticoagulant** that may be used as part of initial management of acute coronary syndromes, but it provides only temporary stabilization and does not address the **definitive need for revascularization**.
- While anticoagulation plays a role in acute management, this patient requires **definitive anatomical correction** of his multivessel disease with significant stenoses, which only surgical or percutaneous revascularization can provide, with CABG being superior given his clinical profile.
Device therapy for heart failure US Medical PG Question 8: A 58-year-old man is brought to the Emergency Department after 2 days of shortness of breath, orthopnea, and lower limb edema. His past medical history is significant for hypertension and a myocardial infarction 3 years ago that required a coronary arterial bypass graft. He has not been able to take prescribed medicine in several months due to recent unemployment and issues with insurance. On admission, his blood pressure is 155/92 mmHg, heart rate is 102/min, respiratory rate is 24/min, and temperature is 36.4°C (97.5°F). On physical examination there are fine rales in both lungs, regular and rhythmic cardiac sounds with an S3 gallop and a grade II/VI holosystolic murmur. Initial laboratory tests are shown below:
Na+ 140 mEq/L
K+ 4.2 mEq/L
Cl- 105 mEq/L
BUN 20 mg/dL
Creatinine 0.8 mg/dL
The patient is stabilized and admitted to the hospital. The next day his blood pressure is 110/60 mmHg, heart rate is 110/min, respiratory rate is 18/min, and temperature is 36.4°C (97.5°F). This morning's laboratory tests are shown below:
Na+ 135 mEq/L
K+ 3.2 mEq/L
Cl- 102 mEq/L
BUN 45 mg/dL
Creatinine 1.7 mg/dL
Which of the following best explains the changes seen in this patient?
- A. Urinary tract obstruction
- B. Diuretic therapy (Correct Answer)
- C. Chronic renal failure
- D. Glomerular basement membrane damage
- E. Cholesterol emboli
Device therapy for heart failure Explanation: ***Diuretic therapy***
- The patient's initial presentation is consistent with **acute decompensated heart failure**, characterized by shortness of breath, orthopnea, lower limb edema, rales, S3 gallop, and a holosystolic murmur (likely mitral regurgitation due to ventricle dilation). The initial normal kidney function (BUN 20, creatinine 0.8) and electrolyte values support acute heart failure.
- The subsequent drop in blood pressure (155/92 to 110/60 mmHg), increase in heart rate (102 to 110/min), and significant rises in BUN (20 to 45 mg/dL) and creatinine (0.8 to 1.7 mg/dL) with a decrease in potassium (4.2 to 3.2 mEq/L) strongly suggest **diuretic-induced volume depletion** leading to worsened renal function (prerenal azotemia) and hypokalemia.
*Urinary tract obstruction*
- This would typically present with symptoms like **dysuria**, frequency, or hesitancy, and acute kidney injury with a more prominent rise in creatinine relative to BUN, none of which are described.
- Obstruction would be less likely to cause a significant drop in blood pressure and hypokalemia, as seen in this patient.
*Chronic renal failure*
- While kidney function has worsened, the initial labs showed normal kidney function, ruling out **chronic disease** as the cause of the acute deterioration.
- Chronic renal failure would typically present with elevated BUN and creatinine for an extended period, which is not the case here.
*Glomerular basement membrane damage*
- Conditions involving **glomerular damage**, such as glomerulonephritis, typically present with proteinuria, hematuria, and often hypertension, which are not detailed in this scenario.
- The acute changes in electrolytes and BUN/creatinine are more indicative of a **hemodynamic issue** rather than a primary glomerular pathology.
*Cholesterol emboli*
- While a patient with a history of CABG is at risk for **cholesterol emboli**, this condition typically causes acute kidney injury, livedo reticularis, eosinophilia, and digital ischemia, which are not described.
- It would not explain the rapid electrolyte shifts and clear signs of volume depletion seen in this patient.
Device therapy for heart failure US Medical PG Question 9: A 55-year-old woman presents with fatigue, shortness of breath during ordinary activities, and occasional fluttering in her chest. She denies chest pain or lower extremity edema. She has no prior medical history. She does not smoke but drinks alcohol socially. Her blood pressure is 110/70 mm Hg, her temperature is 36.9°C (98.4°F), and her radial pulse is 95/min and regular. On physical examination, lungs are clear to auscultation, the apical impulse is slightly displaced, and a III/VI holosystolic murmur is audible at the apex and radiates to the axilla. Transthoracic echocardiography shows the presence of mitral regurgitation and an ejection fraction of 60 %. Which of the following is the optimal therapy for this patient?
- A. ACE inhibitors, beta-blockers, diuretics, and surgery (Correct Answer)
- B. Intra-aortic balloon counterpulsation
- C. Observation and echocardiographic followup
- D. Emergency surgery
- E. Angiotensin-converting enzyme (ACE) inhibitors and beta-blockers
Device therapy for heart failure Explanation: ***ACE inhibitors, beta-blockers, diuretics, and surgery***
- This patient has **symptomatic chronic primary mitral regurgitation (MR)** with preserved ejection fraction, presenting with fatigue, dyspnea, and palpitations.
- According to **current ACC/AHA guidelines**, the definitive treatment for **symptomatic severe chronic primary MR** is **surgical intervention** (mitral valve repair or replacement).
- **Mitral valve repair** is preferred over replacement when feasible, with excellent outcomes in experienced centers.
- Medical management with **diuretics** may provide symptomatic relief for volume overload, while surgery addresses the underlying valvular pathology.
- **Note:** ACE inhibitors and vasodilators are **not recommended** for chronic primary MR with preserved LV function per current guidelines, but may be initiated if there is concurrent hypertension or as bridge therapy before surgery.
*Angiotensin-converting enzyme (ACE) inhibitors and beta-blockers*
- **ACE inhibitors and vasodilators have no proven benefit** in chronic primary mitral regurgitation with preserved left ventricular function.
- These medications are primarily useful for **secondary (functional) MR** due to LV dysfunction or heart failure with reduced ejection fraction.
- Current guidelines **do not recommend** ACE inhibitors as primary therapy for chronic primary MR.
*Intra-aortic balloon counterpulsation*
- This therapy is used for **acute severe mitral regurgitation** or **cardiogenic shock** to improve cardiac output and reduce afterload.
- The patient has **chronic symptoms** and is **hemodynamically stable** with preserved EF, so this aggressive intervention is not indicated.
*Observation and echocardiographic followup*
- This approach is suitable for **asymptomatic patients with mild to moderate chronic primary MR** and preserved left ventricular function.
- However, this patient is experiencing **significant symptoms** (fatigue, dyspnea, palpitations), indicating that observation alone is insufficient.
*Emergency surgery*
- **Emergency surgery** is reserved for **acute, severe MR** with hemodynamic instability or pulmonary edema.
- This patient has **chronic compensated symptoms** with preserved EF, warranting **elective surgical evaluation** rather than emergency intervention.
Device therapy for heart failure US Medical PG Question 10: A 76-year-old woman seeks evaluation at a medical office for chest pain and shortness of breath on exertion of 3 months' duration. Physical examination shows bilateral pitting edema on the legs. On auscultation, diffuse crackles are heard over the lower lung fields. Cardiac examination shows jugular venous distention and an S3 gallop. Troponin is undetectable. A chest film shows cardiomegaly and pulmonary edema. Which of the following medications would be effective in lowering her risk of mortality?
- A. Propranolol
- B. Digoxin
- C. Lisinopril (Correct Answer)
- D. Furosemide
- E. Verapamil
Device therapy for heart failure Explanation: ***Lisinopril***
- The patient presents with classic signs and symptoms of **heart failure**, including dyspnea on exertion, bilateral pitting edema, jugular venous distention, S3 gallop, cardiomegaly, and pulmonary edema. **ACE inhibitors** like lisinopril are cornerstone therapy for **heart failure with reduced ejection fraction (HFrEF)** and significantly reduce mortality.
- They work by blocking the **renin-angiotensin-aldosterone system (RAAS)**, leading to **vasodilation**, reduced preload and afterload, and prevention of cardiac remodeling.
*Propranolol*
- While beta-blockers are used in heart failure, **non-selective beta-blockers** like propranolol are generally not preferred due to potential for exacerbating symptoms in acutely decompensated heart failure and lack of evidence for mortality benefit in this context.
- **Cardioselective beta-blockers** (e.g., carvedilol, metoprolol succinate) are used in stable heart failure, but propranolol's broad effects make it less suitable for this specific indication, especially when there are signs of decompensation.
*Digoxin*
- Digoxin can improve symptoms and reduce hospitalizations in heart failure, but it **does not demonstrate a mortality benefit** in patients with heart failure.
- It is primarily used for **symptom control** in patients with HFrEF, especially those with coexisting **atrial fibrillation**.
*Furosemide*
- Furosemide is a **loop diuretic** that is highly effective at reducing fluid overload and improving symptoms like pulmonary edema and peripheral edema in heart failure.
- However, while it improves symptoms and quality of life, furosemide **does not independently reduce mortality** in heart failure.
*Verapamil*
- Verapamil, a **non-dihydropyridine calcium channel blocker**, is generally **contraindicated** in heart failure with reduced ejection fraction (HFrEF) because it can worsen cardiac function and increase mortality.
- It has **negative inotropic effects**, which can further impair the already weakened pumping ability of the heart.
More Device therapy for heart failure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.