Cardiomyopathies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiomyopathies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiomyopathies US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
Cardiomyopathies Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
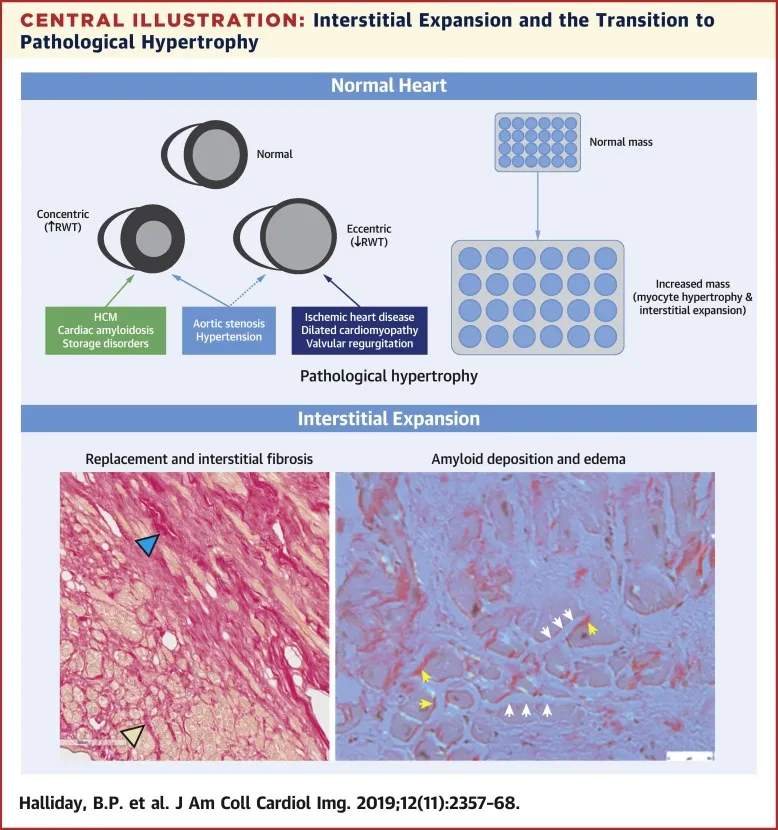
Cardiomyopathies US Medical PG Question 2: A 45-year-old African American woman presents to her family physician for a routine examination. Past medical history is positive for amyloidosis and non-rhythm-based cardiac abnormalities secondary to the amyloidosis. Which of the following cardiac parameters would be expected in this patient?
- A. Increased ejection fraction and decreased compliance
- B. Preserved ejection fraction and increased compliance
- C. Preserved ejection fraction and decreased compliance (Correct Answer)
- D. Increased ejection fraction and increased compliance
- E. Decreased ejection fraction and normal compliance
Cardiomyopathies Explanation: ***Preserved ejection fraction and decreased compliance***
- Cardiac amyloidosis typically leads to **restrictive cardiomyopathy**, where amyloid deposits stiffen the ventricular walls.
- This stiffness impairs the heart's ability to fill properly (**decreased compliance**) but often maintains contractility and thus a **preserved ejection fraction** in the early stages, classifying it as **heart failure with preserved ejection fraction (HFpEF)**.
*Increased ejection fraction and decreased compliance*
- While **decreased compliance** is characteristic of cardiac amyloidosis, an **increased ejection fraction** is generally not expected in this condition.
- A true increase in ejection fraction is rare and not a primary feature of restrictive physiology; rather, the heart struggles to fill, but ejects a normal percentage of the reduced filled volume.
*Preserved ejection fraction and increased compliance*
- **Increased compliance** means the heart chambers are easily stretched and filled, which is the opposite of what occurs in cardiac amyloidosis.
- Patients with amyloidosis have stiff hearts that are difficult to fill, leading to **decreased compliance**.
*Increased ejection fraction and increased compliance*
- Neither **increased ejection fraction** nor **increased compliance** is consistent with cardiac amyloidosis, which is characterized by a stiff, poorly filling ventricle.
- This combination would suggest a hyperdynamic heart with excellent filling, not restrictive cardiomyopathy.
*Decreased ejection fraction and normal compliance*
- While later stages of cardiac amyloidosis can lead to a **decreased ejection fraction** due to severe myocardial dysfunction, it is typically preceded by a stage with **preserved ejection fraction**.
- **Normal compliance** is inconsistent with amyloid infiltration, which inherently reduces the heart's ability to stretch and fill.
Cardiomyopathies US Medical PG Question 3: A 27-year-old woman comes to the physician because of a 1-year history of progressive shortness of breath. She is now unable to jog for more than 10 minutes without stopping to catch her breath. Cardiac examination shows a harsh systolic, crescendo-decrescendo murmur best heard at the lower left sternal border. The murmur increases in intensity when she moves from a squatting to a standing position and decreases when she clenches her fists. The lungs are clear to auscultation. Which of the following is the most likely cause of her condition?
- A. Myosin heavy chain defect (Correct Answer)
- B. CTG trinucleotide repeats
- C. Dystrophin defect
- D. GAA trinucleotide repeats
- E. Fibrillin-1 defect
Cardiomyopathies Explanation: ***Myosin heavy chain defect***
- The clinical presentation of **progressive shortness of breath**, a **harsh systolic crescendo-decrescendo murmur** that increases with standing and decreases with handgrip, is highly indicative of **hypertrophic cardiomyopathy (HCM)**.
- HCM is most commonly caused by genetic mutations affecting **sarcomeric proteins**, with mutations in the **beta-myosin heavy chain gene** being the most frequent.
*CTG trinucleotide repeats*
- **CTG trinucleotide repeats** are characteristic of **myotonic dystrophy type 1**, a multisystem disorder.
- While myotonic dystrophy can cause cardiac involvement (e.g., conduction abnormalities, dilated cardiomyopathy), it does not typically present with the classic murmur and dynamic changes seen in **HCM**.
*Dystrophin defect*
- A **dystrophin defect** is responsible for **Duchenne** and **Becker muscular dystrophies**, which primarily affect skeletal muscle.
- These conditions can lead to **dilated cardiomyopathy**, but not the type of obstructive outflow murmur associated with **HCM**.
*GAA trinucleotide repeats*
- **GAA trinucleotide repeats** are associated with **Friedreich ataxia**, a neurodegenerative disorder that can cause **hypertrophic cardiomyopathy** in up to 65% of patients.
- However, Friedreich ataxia presents with prominent **neurological symptoms** including progressive **ataxia, dysarthria, areflexia**, and loss of position/vibration sense, which are absent in this patient.
- The isolated cardiac presentation with no neurological findings points to **primary HCM** due to sarcomeric protein mutations rather than syndromic forms.
*Fibrillin-1 defect*
- A **fibrillin-1 defect** causes **Marfan syndrome**, a connective tissue disorder.
- Cardiac manifestations typically include **aortic root dilation** and **mitral valve prolapse**, not obstructive hypertrophic cardiomyopathy with the described murmur characteristics.
Cardiomyopathies US Medical PG Question 4: A 14-year-old boy who has been otherwise healthy presents to his doctor complaining of feeling easily winded and light-headed at basketball practice. He has never felt this way before and is frustrated because he is good enough to make varsity this year. He denies smoking, alcohol, or recreational drug use. His mother is very worried because her oldest son and brother had both died suddenly while playing sports despite being otherwise healthy. The transthoracic echocardiogram confirms the suspected diagnosis, which demonstrates a preserved ejection fraction and systolic anterior motion of the mitral valve. The patient is advised that he will need to stay hydrated and avoid intense exercise, and he will likely need an ICD due to his family history. Which of the following physical exam findings is consistent with this patient’s most likely diagnosis?
- A. Tricuspid regurgitation
- B. Systolic ejection murmur that radiates to the carotids
- C. S3 heart sound
- D. Mitral regurgitation
- E. Systolic ejection murmur that worsens with the Valsalva maneuver (Correct Answer)
Cardiomyopathies Explanation: ***Systolic ejection murmur that worsens with the Valsalva maneuver***
- The patient's presentation with **syncope/lightheadedness during exertion**, family history of **sudden cardiac death in athletes**, and echocardiogram findings of **systolic anterior motion (SAM) of the mitral valve** are classic for **hypertrophic cardiomyopathy (HCM)**.
- The murmur of HCM is typically a **systolic ejection murmur** that **worsens with maneuvers that decrease preload**, such as the **Valsalva maneuver** or standing, because this reduction in ventricular volume exacerbates the left ventricular outflow tract (LVOT) obstruction.
*Tricuspid regurgitation*
- This is typically associated with **right heart failure** or **pulmonary hypertension**, which are not indicated by the patient's symptoms or echo findings.
- While it can be heard as a **systolic murmur**, it usually accentuates with inspiration (Carvallo's sign) and does not worsen with the Valsalva maneuver in the context of hypertrophic cardiomyopathy.
*Systolic ejection murmur that radiates to the carotids*
- A systolic ejection murmur radiating to the carotids is characteristic of **aortic stenosis**, which involves a fixed obstruction of the aortic valve.
- While both HCM and aortic stenosis cause systolic murmurs, HCM's murmur has different auscultatory behavior with preload-altering maneuvers (worsening with Valsalva) compared to aortic stenosis (which often softens or is unchanged).
*S3 heart sound*
- An **S3 heart sound** is typically a low-pitched diastolic sound associated with **volume overload** and **heart failure with reduced ejection fraction**, indicating rapid ventricular filling into a dilated ventricle.
- The patient's echocardiogram shows a **preserved ejection fraction**, and his symptoms are related to outflow obstruction, not volume overload.
*Mitral regurgitation*
- While **mitral regurgitation (MR)** can occur in HCM due to systolic anterior motion (SAM) of the mitral valve causing malcoaptation, the primary murmur heard due to the **LVOT obstruction** is a **systolic ejection murmur**.
- The murmur of MR is typically a **holosystolic murmur** that radiates to the axilla and usually **softens with the Valsalva maneuver** as reduced preload can decrease the severity of regurgitation.
Cardiomyopathies US Medical PG Question 5: A 54-year-old woman presents to the emergency ward with a chief complaint of chest pain. The pain is sharp and present in the anterior part of the chest. There is no radiation of the pain; however, the intensity is decreased while sitting and leaning forward. There is no associated shortness of breath. Vital signs are the following: blood pressure is 132/84 mm Hg; pulse rate is 82/min, rhythmic, and regular. Lungs are clear on auscultation and cardiovascular examination demonstrates scratchy and squeaking sounds at the left sternal border. Kussmaul sign is positive and ECG shows new widespread ST segment elevation and PR depression. The most likely cause for these findings in this patient is?
- A. Restrictive cardiomyopathy
- B. Acute pericarditis (Correct Answer)
- C. Pleurisy
- D. Right ventricular myocardial infarction
- E. Cardiac tamponade
Cardiomyopathies Explanation: ***Acute pericarditis***
- The classic presentation includes **sharp, pleuritic chest pain** that **improves with leaning forward** and **worsens with lying down**. The presence of a **pericardial friction rub** (scratchy and squeaking sounds) and specific ECG findings like **widespread ST elevation** and **PR depression** are highly indicative.
- **Kussmaul sign** (paradoxical rise in jugular venous pressure on inspiration) is unusual in uncomplicated acute pericarditis but may suggest associated pericardial effusion or early constrictive physiology. The clinical picture remains most consistent with acute pericarditis given the characteristic chest pain, friction rub, and ECG changes.
*Restrictive cardiomyopathy*
- Characterized by **diastolic dysfunction** and impaired ventricular filling, leading to symptoms like dyspnea and edema. While Kussmaul sign can be present, the chest pain characteristics, friction rub, and widespread ST elevation with PR depression are not typical.
- The ECG findings in restrictive cardiomyopathy usually involve **low voltage** and non-specific ST-T wave changes, not diffuse ST elevation and PR depression.
*Pleurisy*
- Pleurisy causes **sharp, pleuritic chest pain** that can worsen with breathing and movement, similar to pericarditis. However, it does not typically present with a pericardial friction rub or the characteristic ECG changes of widespread ST elevation and PR depression.
- Pleurisy is an inflammation of the pleura, often indicated by **pleural friction rubs** and usually associated with pulmonary conditions, which are not suggested by this patient's findings.
*Right ventricular myocardial infarction*
- While it can cause chest pain and positive Kussmaul sign due to elevated right atrial pressure, the chest pain is typically more anginal-like and not relieved by leaning forward.
- The ECG would show **ST elevation primarily in right-sided leads (V4R)** and inferior leads (II, III, aVF), but would **not typically show widespread ST elevation or PR depression** in multiple lead distributions or a pericardial friction rub.
*Cardiac tamponade*
- Characterized by the **Beck's triad** (hypotension, muffled heart sounds, and elevated jugular venous pressure) and pulsus paradoxus. Chest pain can be present, but the pain's amelioration with leaning forward and the specific ECG changes with widespread ST elevation and PR depression are not typical.
- While a pericardial friction rub might precede tamponade, **cardiac tamponade itself typically develops from a significant pericardial effusion**, leading to compression of the heart and does not directly manifest with diffuse ST elevation and PR depression.
Cardiomyopathies US Medical PG Question 6: A 38-year-old woman comes to the physician because of frequent headaches and blurring of vision. She also complains of weight gain, menstrual irregularities, and excessive growth of body hair. She says that, for the first time since she turned 18, her shoe and ring sizes have increased, and also complains that her voice has become hoarser. She does not smoke or drink alcohol. She takes no medications. Vital signs are within normal limits. Physical examination shows prominent frontal bossing, a protuberant mandible with spaces between the teeth, and large hands and feet. Serum studies show:
Na+ 140 mEq/L
Cl− 102 mEq/L
K+ 4.1 mEq/L
Ca2+ 10.6 mg/dL
Phosphorus 4.7 mg/dL
Glucose 180 mg/dL
Which of the following is the most likely sequela of this patient's condition?
- A. Deposition of mucopolysaccharides in the myocardium
- B. Thickening of the coronary artery walls
- C. Prolongation of the QT interval on ECG
- D. Left ventricular hypertrophy (Correct Answer)
- E. Reduced cardiac output
Cardiomyopathies Explanation: ***Left ventricular hypertrophy***
- **Left ventricular hypertrophy (LVH)** is the **most common cardiac complication** of acromegaly, occurring in 60-90% of patients with chronic growth hormone (GH) excess.
- The pathophysiology involves direct effects of **GH** and **insulin-like growth factor 1 (IGF-1)** on cardiac myocytes, leading to hypertrophy and interstitial fibrosis, along with increased afterload from hypertension.
- LVH typically manifests early in the disease course and can progress to **diastolic dysfunction** and eventually systolic dysfunction if untreated.
- This patient's clinical features (frontal bossing, prognathism, acral enlargement, hyperglycemia) are classic for **acromegaly**, making LVH the most likely cardiac sequela.
*Reduced cardiac output*
- While **acromegalic cardiomyopathy** can eventually progress to systolic dysfunction with reduced cardiac output and heart failure, this represents a **late-stage complication** occurring in <20% of cases.
- This develops after years of untreated disease when the initial compensatory LVH progresses to dilated cardiomyopathy.
- Since the question asks for the "most likely sequela," LVH is more appropriate as it occurs much more frequently and earlier in the disease course.
*Deposition of mucopolysaccharides in the myocardium*
- This finding is characteristic of **mucopolysaccharidoses** (e.g., Hurler syndrome, Hunter syndrome), which are lysosomal storage diseases.
- While soft tissue hypertrophy occurs in acromegaly, it is due to **increased collagen deposition and glycosaminoglycan accumulation in soft tissues**, not the myocardium specifically.
- This is not a recognized cardiac manifestation of acromegaly.
*Thickening of the coronary artery walls*
- While patients with acromegaly have increased cardiovascular risk due to **hypertension**, **diabetes mellitus**, and **dyslipidemia**, leading to accelerated atherosclerosis, this is not the primary or most characteristic cardiac sequela.
- Coronary artery disease can develop but is less specific to acromegaly than the direct cardiac effects of GH/IGF-1 excess.
*Prolongation of the QT interval on ECG*
- **QT prolongation** is associated with electrolyte abnormalities (hypocalcemia, hypomagnesemia, hypokalemia), certain medications, and specific genetic syndromes.
- This is not a recognized feature or sequela of acromegaly.
- The patient's electrolytes in this case are within normal limits.
Cardiomyopathies US Medical PG Question 7: A 14-year-old girl is brought to the physician for a follow-up examination. She has had frequent falls over the past two years. During the past six months, the patient has been unable to walk or stand without assistance and she now uses a wheelchair. Her mother was diagnosed with a vestibular schwannoma at age 52. Her vital signs are within normal limits. Her speech is slow and unclear. Neurological examination shows nystagmus in both eyes. Her gait is wide-based with irregular and uneven steps. Her proprioception and vibration sense are absent. Muscle strength is decreased especially in the lower extremities. Deep tendon reflexes are 1+ bilaterally. The remainder of the examination shows kyphoscoliosis and foot inversion with hammer toes. This patient is most likely to die from which of the following complications?
- A. Aspiration pneumonia
- B. Leukemia
- C. Renal cell carcinoma
- D. Heart failure (Correct Answer)
- E. Posterior fossa tumors
Cardiomyopathies Explanation: ***Heart failure***
- This patient's presentation with progressive ataxia, nystagmus, dysarthria, kyphoscoliosis, foot deformities, sensory deficits, and decreased deep tendon reflexes is highly suggestive of **Friedreich ataxia**.
- **Cardiomyopathy** and **congestive heart failure** are the leading causes of death in patients with Friedreich ataxia, affecting approximately 60% of patients and often leading to premature mortality.
*Aspiration pneumonia*
- While patients with **neurological deficits** like dysarthria and ataxia are at increased risk for aspiration, it is not the most common or direct cause of death in Friedreich ataxia compared to cardiac complications.
- Aspiration pneumonia is a serious complication, but **cardiac involvement** typically dictates the prognosis and survival in this condition.
*Leukemia*
- There is **no established link** between Friedreich ataxia and an increased risk of developing leukemia.
- The patient's symptoms are characteristic of a primary neurological and systemic disorder, not a hematological malignancy.
*Renal cell carcinoma*
- This type of cancer is **not associated** with Friedreich ataxia.
- The presented symptoms do not point towards any renal pathology or an increased risk for renal cell carcinoma.
*Posterior fossa tumors*
- While the mother had a vestibular schwannoma, which is a **posterior fossa tumor**, the patient's symptoms are not consistent with a tumor of the posterior fossa.
- The **progressive, diffuse neurological deficits** affecting both motor and sensory systems, along with systemic manifestations like kyphoscoliosis, are characteristic of a genetic ataxia rather than a focal tumor.
Cardiomyopathies US Medical PG Question 8: A previously healthy 19-year-old man is brought to the emergency department by his girlfriend after briefly losing consciousness. He passed out while moving furniture into her apartment. She said that he was unresponsive for a minute but regained consciousness and was not confused. The patient did not have any chest pain, palpitations, or difficulty breathing before or after the episode. He has had episodes of dizziness when exercising at the gym. His blood pressure is 125/75 mm Hg while supine and 120/70 mm Hg while standing. Pulse is 70/min while supine and 75/min while standing. On examination, there is a grade 3/6 systolic murmur at the left lower sternal border and a systolic murmur at the apex, both of which disappear with passive leg elevation. Which of the following is the most likely cause?
- A. Prolonged QT interval
- B. Hypertrophic cardiomyopathy (Correct Answer)
- C. Mitral valve stenosis
- D. Mitral valve prolapse
- E. Bicuspid aortic valve
Cardiomyopathies Explanation: ***Hypertrophic cardiomyopathy***
- This patient's **syncope associated with exertion** (moving furniture) and episodes of **dizziness during exercise** are highly suggestive of hypertrophic cardiomyopathy (HCM).
- The presence of a **systolic murmur at the left sternal border and apex** that **decreases/disappears with passive leg elevation** indicates a dynamic left ventricular outflow tract (LVOT) obstruction that is sensitive to preload changes, a hallmark of HCM.
- Passive leg elevation **increases preload** → **increases LV volume** → **decreases LVOT obstruction** → **decreases murmur intensity**.
*Prolonged QT interval*
- While it can cause syncope, especially exertional, a prolonged QT interval generally **does not present with dynamic murmurs** that change with preload.
- ECG findings (not mentioned here) would be the primary diagnostic clue, not physical exam findings related to murmurs.
*Mitral valve stenosis*
- Mitral stenosis would typically present with a **diastolic murmur** (not systolic) and symptoms like dyspnea, fatigue, and possibly hemoptysis due to elevated left atrial pressure.
- The murmur of mitral stenosis would not characteristically change with passive leg elevation in the manner described.
*Mitral valve prolapse*
- Mitral valve prolapse often presents with a **mid-systolic click** followed by a systolic murmur, which typically **intensifies with standing** or maneuvers that decrease left ventricular volume.
- The murmur described here decreases with leg elevation (increased preload), which is the opposite behavior of a mitral prolapse murmur.
*Bicuspid aortic valve*
- A bicuspid aortic valve can cause an **aortic stenosis murmur** (a systolic ejection murmur heard best at the right upper sternal border) or regurgitation, but it generally **does not cause a dynamic murmur that changes with preload** in this characteristic fashion.
- Symptoms related to bicuspid aortic valve disease (like syncope) would more commonly be associated with significant stenosis, not with a murmur that is acutely sensitive to preload changes.
Cardiomyopathies US Medical PG Question 9: A 34-year-old woman, gravida 2, para 2, is admitted to the hospital because of shortness of breath and fatigue 2 weeks after delivery of a full-term female newborn. She has no history of major medical illness. Cardiac examination on admission shows an S3 gallop and a grade 2/6 holosystolic murmur heard best at the apex. Treatment is initiated with intravenous furosemide and captopril. Her symptoms resolve, and 3 weeks later, cardiac examination shows no murmur. Which of the following is the most likely explanation for the initial auscultation findings?
- A. Myxomatous mitral valve degeneration
- B. Mitral annular calcification
- C. Perivalvular abscess
- D. Mitral valve leaflet fibrosis
- E. Mitral annular dilatation (Correct Answer)
Cardiomyopathies Explanation: ***Mitral annular dilatation***
- The combination of **shortness of breath**, **fatigue**, **S3 gallop**, and a **holosystolic murmur** at the apex in the peripartum period is highly suggestive of **peripartum cardiomyopathy (PPCM)**.
- In PPCM, the **left ventricle dilates**, leading to **mitral annular dilatation** and subsequent **functional mitral regurgitation**, which manifests as a holosystolic murmur. The resolution of symptoms and murmur after treatment supports PPCM.
*Myxomatous mitral valve degeneration*
- This condition is characterized by **structural changes** in the mitral valve leaflets, making them redundant or prolapsing.
- The murmur associated with this would likely be a **mid-systolic click** followed by a late systolic murmur, and it would typically be a **chronic finding** that would not resolve within weeks postpartum.
*Mitral annular calcification*
- This condition involves thickening and hardening of the **mitral valve annulus**, primarily seen in older individuals or those with significant cardiovascular risk factors.
- While it can lead to mitral regurgitation or stenosis, it is a **chronic structural change** and would not resolve spontaneously or with medical management in a few weeks.
*Perivalvular abscess*
- A perivalvular abscess is a complication of **infective endocarditis**, typically presenting with **fever**, positive **blood cultures**, and evidence of infection.
- This patient lacks fever or other signs of infection, and the rapid resolution of symptoms and murmur is inconsistent with an active infectious process requiring specific antibiotic therapy.
*Mitral valve leaflet fibrosis*
- **Mitral valve leaflet fibrosis** implies a **scarring and thickening of the valve leaflets**, often a consequence of rheumatic heart disease or other chronic inflammatory processes.
- This is a **permanent structural change** that would not resolve spontaneously within weeks after delivery, and the patient has no history to suggest such a condition.
Cardiomyopathies US Medical PG Question 10: An 80-year-old African American male presents complaining of worsening shortness of breath that occurs during his weekly round of golf. He also notes he has been waking up at night "choking and gasping for air", though he has been able to gain some relief by propping his head on a stack of pillows before he goes to bed. Upon auscultation, a low frequency, early diastolic gallop is heard over the apex while the patient rests in the left lateral decubitus position. This finding is most consistent with which of the following?
- A. Left ventricular concentric hypertrophy
- B. Right atrial hypertrophy
- C. Mitral stenosis
- D. Left atrial hypertrophy
- E. Left ventricular eccentric hypertrophy (Correct Answer)
Cardiomyopathies Explanation: ***Left ventricular eccentric hypertrophy***
- The symptoms of **dyspnea on exertion** and **paroxysmal nocturnal dyspnea** (relieved by propping up pillows) are classic for **left-sided heart failure**.
- An **early diastolic gallop** (S3 heart sound) heard best at the apex in the left lateral decubitus position is indicative of **volume overload** and a failing, dilated left ventricle, consistent with eccentric hypertrophy.
*Left ventricular concentric hypertrophy*
- Concentric hypertrophy is typically associated with **pressure overload** (e.g., hypertension, aortic stenosis) and often presents with a **late diastolic gallop (S4)** due to a stiff, non-compliant ventricle.
- While it can lead to heart failure, the presence of an **S3 gallop** points more strongly to a dilated, volume-overloaded ventricle.
*Right atrial hypertrophy*
- Right atrial hypertrophy results from **right ventricular dysfunction** or conditions like **pulmonary hypertension** and would manifest with symptoms of right heart failure (e.g., peripheral edema, jugular venous distention), not primarily left-sided symptoms.
- It is not directly associated with a left ventricular early diastolic gallop.
*Mitral stenosis*
- Mitral stenosis typically causes a **mid-diastolic murmur** with an opening snap, and its symptoms are usually related to elevated left atrial pressure leading to pulmonary congestion and dyspnea.
- An **S3 gallop** is not characteristic of mitral stenosis; it's more specific for left ventricular systolic dysfunction.
*Left atrial hypertrophy*
- Left atrial hypertrophy (enlargement) commonly results from conditions like **mitral valve disease** or **left ventricular diastolic dysfunction** but does not directly cause an S3 gallop.
- While it contributes to symptoms of left heart failure, it's a consequence rather than the primary cause of an S3.
More Cardiomyopathies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.