Acute decompensated heart failure US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute decompensated heart failure. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute decompensated heart failure US Medical PG Question 1: An investigator is studying patients with acute decompensated congestive heart failure. He takes measurements of a hormone released from atrial myocytes, as well as serial measurements of left atrial and left ventricular pressures. The investigator observes a positive correlation between left atrial pressures and the serum level of this hormone. Which of the following is most likely the mechanism of action of this hormone?
- A. Increases potassium excretion at the collecting ducts
- B. Constricts afferent renal arteriole
- C. Decreases sodium reabsorption at the collecting tubules (Correct Answer)
- D. Decreases reabsorption of bicarbonate in the proximal convoluted tubules
- E. Increases free water reabsorption from the distal tubules
Acute decompensated heart failure Explanation: ***Decreases sodium reabsorption at the collecting tubules***
- The hormone described, exhibiting a positive correlation with left atrial pressure and released from atrial myocytes, is **Atrial Natriuretic Peptide (ANP)**.
- ANP promotes **natriuresis** (sodium excretion) and **diuresis** by directly inhibiting sodium reabsorption in the collecting tubules, thereby reducing blood volume and cardiac preload.
*Increases potassium excretion at the collecting ducts*
- While ANP does promote fluid and electrolyte excretion, its primary effect is on sodium and water, not a direct increase in **potassium excretion**. **Aldosterone**, not ANP, primarily increases potassium secretion in the collecting ducts.
- This option describes a mechanism more consistent with **mineralocorticoid activity**, which is counteracted by ANP.
*Constricts afferent renal arteriole*
- ANP generally causes **vasodilation** of the afferent arteriole and constriction of the efferent arteriole, increasing glomerular filtration rate (GFR).
- **Angiotensin II** is a primary constrictor of the afferent and efferent renal arterioles, which is the opposite effect of ANP.
*Decreases reabsorption of bicarbonate in the proximal convoluted tubules*
- This mechanism is primarily involved in **acid-base balance** and is influenced by factors like parathyroid hormone or respiratory/metabolic acidosis/alkalosis.
- ANP's main action is on **sodium and water balance**, not directly on bicarbonate reabsorption.
*Increases free water reabsorption from the distal tubules*
- **Vasopressin (Antidiuretic Hormone, ADH)** is responsible for increasing free water reabsorption in the distal tubules and collecting ducts.
- ANP's action is to *increase* water excretion, working in opposition to ADH to reduce circulating fluid volume.
Acute decompensated heart failure US Medical PG Question 2: The serum brain natriuretic peptide and N-terminal pro-BNP are elevated. A diagnosis of heart failure with preserved ejection fraction is made. In addition to supplemental oxygen therapy, which of the following is the most appropriate initial step in management?
- A. Intravenous dobutamine
- B. Intravenous furosemide therapy (Correct Answer)
- C. Intravenous morphine therapy
- D. Thoracentesis
- E. Intermittent hemodialysis
Acute decompensated heart failure Explanation: ***Intravenous furosemide therapy***
- Heart failure with **preserved ejection fraction (HFpEF)** often presents with **pulmonary congestion** due to elevated filling pressures.
- **Furosemide**, a loop diuretic, effectively reduces fluid overload and associated symptoms by increasing renal excretion of sodium and water.
*Intravenous dobutamine*
- **Dobutamine** is an inotropic agent that increases myocardial contractility and heart rate.
- It is typically used for **acute decompensated heart failure with low cardiac output** and is generally avoided in HFpEF unless there is significant hypoperfusion, as it can worsen myocardial oxygen demand and diastolic dysfunction.
*Intravenous morphine therapy*
- **Morphine** can be used in acute heart failure to reduce preload and anxiety, but it is not a primary treatment for the underlying fluid overload.
- It can cause respiratory depression and hypotension, and its use is typically reserved for patients with severe pain or dyspnea not adequately managed by other therapies.
*Thoracentesis*
- **Thoracentesis** is indicated for symptomatic **pleural effusions** causing respiratory distress.
- While pleural effusions can occur in heart failure, initial management of generalized fluid overload typically involves diuretics, making thoracentesis a secondary intervention if diuretic therapy is insufficient.
*Intermittent hemodialysis*
- **Intermittent hemodialysis** is an invasive procedure primarily used for severe renal failure or refractory fluid overload that has not responded to maximal diuretic therapy.
- It is not the initial step in managing heart failure with preserved ejection fraction and would only be considered in highly selected cases with **acute kidney injury** or diuretic resistance.
Acute decompensated heart failure US Medical PG Question 3: A 54-year-old man is brought to the emergency department 1 hour after the sudden onset of shortness of breath, epigastric pain, and sweating. He has no history of similar symptoms. He has hypertension and type 2 diabetes mellitus. Current medications include amlodipine and metformin. He has smoked one pack of cigarettes daily for 20 years. He appears weak and pale. His pulse is 56/min, respirations are 18/min, and blood pressure is 100/70 mm Hg. Cardiac examination shows normal heart sounds. The lungs are clear to auscultation. The skin is cold to the touch. An ECG is shown. Bedside transthoracic echocardiography shows normal left ventricular function. High-dose aspirin is administered. Administration of which of the following is most appropriate next step in management?
- A. Intravenous atropine
- B. Intravenous morphine
- C. Normal saline bolus (Correct Answer)
- D. Phenylephrine infusion
- E. Sublingual nitroglycerin
Acute decompensated heart failure Explanation: ***Normal saline bolus***
- This patient presents with symptoms concerning for an inferior wall myocardial infarction (MI) which commonly affects the **right ventricle (RV)**. The ECG shows **ST elevation in leads II, III, and aVF**, confirming an inferior STEMI. Given his **hypotension (100/70 mm Hg)** and **bradycardia (56/min)**, he is likely experiencing RV involvement and is preload-dependent.
- A **normal saline bolus** is crucial to increase preload and improve cardiac output, especially in RV infarcts where reduced preload significantly impairs RV function and, consequently, left ventricular filling.
*Intravenous atropine*
- While the patient has bradycardia, it is secondary to the inferior MI affecting the **right coronary artery**, which often supplies the **AV node**.
- Atropine is used for symptomatic bradycardia but a fluid bolus should be prioritized in RV MI with hypotension to restore preload before considering pharmacologic interventions for heart rate.
*Intravenous morphine*
- Morphine is used for pain relief in acute MI but can cause **vasodilation**, which would worsen this patient's **hypotension**.
- In cases of RV infarction, where preload dependence is critical, morphine should be used with extreme caution or avoided due to its potential to further reduce blood pressure.
*Phenylephrine infusion*
- Phenylephrine is a **pure alpha-agonist** that causes **vasoconstriction** and increases systemic vascular resistance, thereby increasing afterload.
- Increasing afterload in the setting of an acute MI, especially one with potential RV involvement and preload dependence, can severely compromise cardiac function and worsen the patient's condition.
*Sublingual nitroglycerin*
- Nitroglycerin causes **vasodilation**, reducing both preload and afterload.
- In a patient with an **inferior wall MI** and **hypotension**, nitroglycerin is contraindicated as it can profoundly reduce preload, leading to a significant drop in blood pressure and worsening shock, especially if the right ventricle is involved.
Acute decompensated heart failure US Medical PG Question 4: An 81-year-old man is admitted to the hospital due to acute decompensated heart failure. He has type 2 diabetes mellitus, hypertension, coronary artery disease, and congestive heart failure. Current medications include lisinopril, metformin, and low-dose aspirin. He has smoked one pack of cigarettes daily for 45 years. His temperature is 37.6°C (99.7°F), pulse is 105/min and regular, respirations are 21/min, and blood pressure is 103/64 mm Hg. Laboratory studies show:
Hemoglobin 13.7 g/dL
Leukocyte count 8200/mm3
Serum
Na+ 128 mEq/L
Cl- 98 mEq/L
K+ 4.9 mEq/L
Urea nitrogen 58 mg/dL
Glucose 200 mg/dL
Creatinine 2.2 mg/dL
Which of the following changes in the medication regimen is most appropriate in this patient at this time?
- A. Begin vancomycin therapy
- B. Discontinue aspirin therapy
- C. Begin nitroprusside therapy
- D. Discontinue metformin therapy (Correct Answer)
- E. Begin hydrochlorothiazide therapy
Acute decompensated heart failure Explanation: ***Discontinue metformin therapy***
- The patient has **acute decompensated heart failure** with **acute kidney injury** (creatinine 2.2 mg/dL, BUN 58 mg/dL). Metformin is **contraindicated in acute kidney injury** due to the significantly increased risk of **lactic acidosis**.
- With renal failure, metformin excretion is impaired, leading to drug accumulation and dangerous elevations in lactic acid levels. **Immediate discontinuation** is critical to prevent this life-threatening complication.
- Current guidelines recommend avoiding metformin when eGFR <30 mL/min or creatinine >1.5 mg/dL in males.
*Begin vancomycin therapy*
- There is **no indication of bacterial infection** (normal leukocyte count 8200/mm³, only mild temperature elevation to 37.6°C, no localizing signs).
- Initiating broad-spectrum antibiotics like vancomycin without clear evidence of infection contributes to **antibiotic resistance** and potential adverse effects.
*Discontinue aspirin therapy*
- The patient has a history of **coronary artery disease** and **congestive heart failure**, making him high risk for acute coronary events.
- Aspirin provides crucial **antiplatelet therapy** for secondary prevention of cardiovascular events in this patient population and should be continued.
*Begin nitroprusside therapy*
- Nitroprusside is a potent vasodilator used in **hypertensive emergencies** or severe heart failure with elevated blood pressure.
- This patient currently has **hypotension** (BP 103/64 mm Hg), and nitroprusside would further lower blood pressure, potentially causing cardiovascular collapse and end-organ hypoperfusion.
*Begin hydrochlorothiazide therapy*
- While diuretics are used in heart failure, hydrochlorothiazide is a **thiazide diuretic** primarily effective with preserved renal function (eGFR >30 mL/min).
- This patient has **elevated creatinine (2.2 mg/dL)**, indicating acute kidney injury, which would significantly limit the efficacy of hydrochlorothiazide. **Loop diuretics** (furosemide) would be more appropriate if diuresis is needed in the setting of renal impairment.
Acute decompensated heart failure US Medical PG Question 5: A 70-year-old Caucasian male visits your office regularly for treatment of New York Heart association class IV congestive heart failure. Which of the following medications would you add to this man's drug regimen in order to improve his overall survival?
- A. Spironolactone (Correct Answer)
- B. Furosemide
- C. Amiloride
- D. Acetazolamide
- E. Hydrochlorothiazide
Acute decompensated heart failure Explanation: ***Spironolactone***
- **Spironolactone** is an **aldosterone antagonist** that has been shown to reduce mortality and morbidity in patients with **NYHA Class III and IV heart failure**.
- It works by blocking the harmful effects of **aldosterone** on the heart, such as **fibrosis** and remodeling, improving cardiac function and survival.
*Furosemide*
- **Furosemide** is a **loop diuretic** primarily used to relieve **symptoms of congestion** (edema, dyspnea) in heart failure by promoting fluid excretion.
- While it improves symptoms, **furosemide** alone does not significantly improve long-term survival in patients with heart failure.
*Amiloride*
- **Amiloride** is a **potassium-sparing diuretic** that works by blocking sodium channels in the collecting duct, leading to modest diuresis.
- It is often used to prevent **hypokalemia** caused by other diuretics but does not have the same proven mortality benefit in heart failure as spironolactone.
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** primarily used for glaucoma, metabolic alkalosis, and altitude sickness.
- It has a weaker diuretic effect and is not a commonly used or recommended medication for improving long-term survival in patients with heart failure.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** primarily used for hypertension and mild to moderate edema.
- While it can help manage fluid retention, it does not offer the same mortality benefit in advanced heart failure as aldosterone antagonists like spironolactone.
Acute decompensated heart failure US Medical PG Question 6: A 62-year-old man is brought to the emergency department because of progressive shortness of breath, mild chest pain on exertion, and a cough for 2 days. One week ago, he had a low-grade fever and nasal congestion. He has hypertension but does not adhere to his medication regimen. He has smoked one pack of cigarettes daily for 30 years and drinks 3–4 beers daily. His temperature is 37.1°C (98.8°F), pulse is 125/min, respirations are 29/min, and blood pressure is 145/86 mm Hg. He is in moderate respiratory distress while sitting. Pulmonary examination shows reduced breath sounds bilaterally. There is scattered wheezing over all lung fields. There is inward displacement of his abdomen during inspiration. Arterial blood gas analysis shows:
pH 7.29
PCO2 63 mm Hg
PO2 71 mm Hg
HCO3- 29 mEq/L
O2 saturation 89%
Which of the following is the most likely cause of this patient's symptoms?
- A. Acute pulmonary embolism
- B. Acute respiratory distress syndrome
- C. Acute asthma exacerbation
- D. Acute exacerbation of chronic obstructive pulmonary disease (Correct Answer)
- E. Acute decompensation of congestive heart failure
Acute decompensated heart failure Explanation: ***Acute exacerbation of chronic obstructive pulmonary disease***
- The patient's history of heavy smoking, chronic cough, and recent respiratory infection, coupled with acute shortness of breath, wheezing, and hypercapnic respiratory acidosis, is highly suggestive of an **acute exacerbation of COPD**. The inward displacement of the abdomen during inspiration indicates increased work of breathing and **diaphragmatic fatigue**.
- The arterial blood gas (ABG) showing **pH 7.29, PCO2 63 mm Hg, PO2 71 mm Hg, and HCO3- 29 mEq/L** points to an uncompensated or partially compensated **respiratory acidosis with hypoxemia**, characteristic of severe COPD exacerbation.
*Acute pulmonary embolism*
- While pulmonary embolism can cause dyspnea and hypoxemia, the presence of diffuse wheezing, a history of heavy smoking consistent with chronic lung disease, and hypercapnic respiratory acidosis (elevated PCO2) make it less likely.
- A **pulmonary embolism** typically presents with sudden onset dyspnea, pleuritic chest pain, and often significant hypoxemia, but usually without diffuse wheezing or hypercapnia unless there is underlying severe lung disease.
*Acute respiratory distress syndrome*
- ARDS is characterized by severe hypoxemia refractory to oxygen therapy and bilateral pulmonary infiltrates on chest imaging, often in the setting of a direct or indirect lung injury.
- The patient's symptoms are more consistent with an obstructive process, and the ABG showing hypercapnia with some bicarbonate compensation is not typical of ARDS, which generally presents with **respiratory alkalosis** early on, due to tachypnea.
*Acute asthma exacerbation*
- While an asthma exacerbation can cause wheezing and shortness of breath, this patient's long smoking history and chronic cough make COPD a more probable diagnosis, especially given his age.
- Although the symptoms are similar, the significant smoking history makes **COPD** more likely, and patients with long-standing asthma often respond well to bronchodilators, which is not mentioned here.
*Acute decompensation of congestive heart failure*
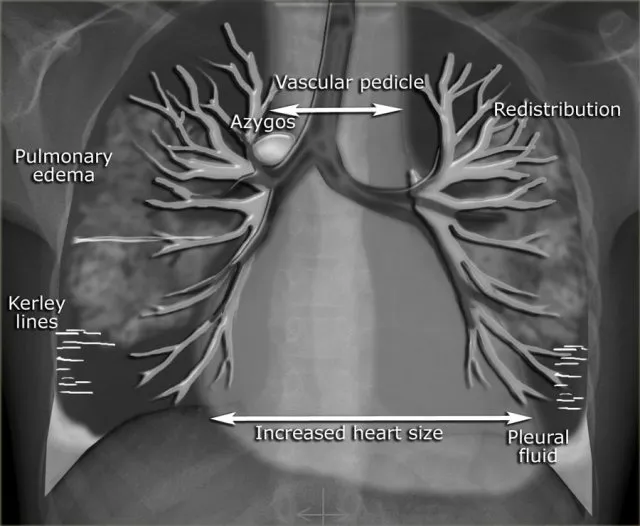
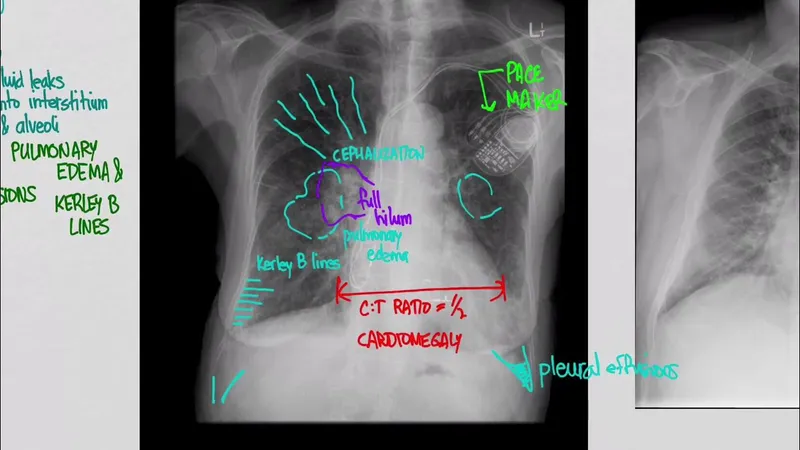
- **Congestive heart failure** typically presents with orthopnea, paroxysmal nocturnal dyspnea, and bilateral crackles on lung examination, often with peripheral edema. Wheezing, known as "cardiac asthma," can occur but is usually accompanied by other signs of fluid overload.
- The primary respiratory findings in this patient are wheezing and reduced breath sounds, with inward abdominal displacement, which point more towards an **obstructive lung process** rather than fluid overload.
Acute decompensated heart failure US Medical PG Question 7: A 59-year-old woman comes to the physician for a 3-month history of progressively worsening shortness of breath on exertion and swelling of her legs. She has a history of breast cancer, which was treated with surgery followed by therapy with doxorubicin and trastuzumab 4 years ago. Cardiac examination shows an S3 gallop; there are no murmurs or rubs. Examination of the lower extremities shows pitting edema below the knees. Echocardiography is most likely to show which of the following sets of changes in this patient?
$$$ Ventricular wall thickness %%% Ventricular cavity size %%% Diastolic function %%% Aorto-ventricular pressure gradient $$$
- A. ↓ ↑ normal normal (Correct Answer)
- B. Normal normal ↓ normal
- C. ↑ ↓ ↓ normal
- D. ↑ ↓ ↓ ↑
- E. ↓ ↑ ↓ normal
Acute decompensated heart failure Explanation: ***↓ ↑ normal normal***
- Doxorubicin is an **anthracycline** known to cause **dilated cardiomyopathy**, characterized by **decreased ventricular wall thickness**, **increased ventricular cavity size**, and **preserved diastolic function**.
- The S3 gallop and pitting edema indicate **heart failure with reduced ejection fraction (HFrEF)**, consistent with dilated cardiomyopathy.
*Normal normal ↓ normal*
- This option suggests a primary issue with **diastolic function**, which is not the typical presentation of doxorubicin-induced cardiomyopathy.
- While diastolic dysfunction can occur, doxorubicin characteristically causes **systolic dysfunction** manifesting as chamber dilation and wall thinning.
*↑ ↓ ↓ normal*
- This pattern of **increased wall thickness** and **decreased cavity size** is characteristic of **hypertrophic cardiomyopathy** or **restrictive cardiomyopathy**, which are generally not caused by doxorubicin.
- Doxorubicin typically causes **cardiac muscle fiber damage** leading to thinning and dilation.
*↑ ↓ ↓ ↑*
- This option also suggests **increased wall thickness** and **decreased cavity size**, inconsistent with doxorubicin's effects on the heart.
- The **elevated aorto-ventricular pressure gradient** might indicate outflow tract obstruction or significant aortic stenosis, which are not typical sequelae of doxorubicin.
*↓ ↑ ↓ normal*
- While doxorubicin leads to **decreased wall thickness** and **increased cavity size**, the diastolic function is usually preserved early on, not decreased.
- A decrease in diastolic function might occur in later stages, but the primary and most characteristic feature due to doxorubicin is **systolic dysfunction** and chamber remodeling.
Acute decompensated heart failure US Medical PG Question 8: A 66-year-old man presents to the emergency department with dyspnea. Two days ago, he hosted his grandchild's birthday party, and since has noticed general malaise, fever, and dry cough. He does not know if he feels more dyspneic while supine or standing but has noticed difficulty breathing even while watching television. He has a past medical history of congestive heart failure and hypertension, for which he takes aspirin, metoprolol, furosemide, lisinopril, and spironolactone as prescribed. His blood pressure is 90/50 mmHg, pulse is 120/min, and respirations are 30/min. His radial pulse is barely palpable, and his wrists and ankles are cold and clammy. Physical exam reveals a S3 and S4 with a soft holosystolic murmur at the apex, decreased breath sounds up to the middle lung fields, jugular venous distention to the auricles, and 3+ pitting edema to the mid thighs. EKG shows ST depressions consistent with demand ischemia. Bedside echocardiogram shows global akinesis with an ejection fraction (EF) of 20%; previous reports show EF at 40%. A portable chest radiograph shows bilateral pulmonary edema. Metoprolol is held, dobutamine and furosemide drips are started, and BiPAP is started at 20/5 cm H2O. After 15 minutes, the nurse reports that urine output is minimal and blood pressure is now 75/40 mmHg and pulse is 130/min. What is the best next step in management?
- A. Decrease furosemide rate
- B. Resume home metoprolol
- C. Decrease positive inspiratory pressure (Correct Answer)
- D. Decrease dobutamine rate
- E. Decrease positive end-expiratory pressure
Acute decompensated heart failure Explanation: ***Decrease positive inspiratory pressure***
- The patient is experiencing worsening **hypotension** and **tachycardia** despite initial treatment, suggesting that the current BiPAP settings, particularly a high **positive inspiratory pressure (PIP)**, might be exacerbating the hemodynamic instability.
- High intrathoracic pressure from BiPAP can decrease **venous return** and **cardiac preload**, further compromising an already struggling heart with reduced ejection fraction, leading to decreased cardiac output and worsening hypotension.
*Decrease furosemide rate*
- The patient has significant signs of **fluid overload** (pulmonary edema, JVD, pitting edema), and minimal urine output suggests inadequate diuresis, not over-diuresis.
- Decreasing the furosemide rate would likely worsen fluid overload and pulmonary congestion, which is detrimental given his acute heart failure exacerbation.
*Resume home metoprolol*
- The patient is already hypotensive (90/50 mmHg initially, dropping to 75/40 mmHg) and in **cardiogenic shock**, and beta-blockers like metoprolol are **contraindicated** in this acute setting.
- Resuming metoprolol would further depress myocardial contractility and worsen bradycardia (although he is currently tachycardic), significantly exacerbating his hypotension and shock state.
*Decrease dobutamine rate*
- **Dobutamine** is an **inotropic agent** used to improve cardiac contractility and cardiac output in patients with cardiogenic shock, especially with a low EF.
- Decreasing the dobutamine rate would reduce inotropic support, likely leading to a further decline in cardiac output and worsening his profound hypotension and shock.
*Decrease positive end-expiratory pressure*
- While PEEP can increase intrathoracic pressure, the given BiPAP setting of 20/5 cm H2O indicates a PIP of 20 cm H2O and a **PEEP of 5 cm H2O**. A PEEP of 5 cm H2O is relatively low and often beneficial for oxygenation and reducing preload in pulmonary edema.
- The primary concern for hemodynamic compromise with BiPAP is more often related to high peak inspiratory pressure reducing venous return, rather than a low PEEP which can help keep alveoli open and improve gas exchange.
Acute decompensated heart failure US Medical PG Question 9: A 71-year-old woman with a past medical history of type 2 diabetes, hypercholesterolemia, and hypertension was admitted to the hospital 8 hours ago with substernal chest pain for management of acute non-ST-elevated myocardial infarction (NSTEMI). The ECG findings noted by ST-depressions and T-wave inversions on anterolateral leads, which is also accompanied by elevated cardiac enzymes. Upon diagnosis, management with inhaled oxygen therapy, beta-blockers and aspirin, and low-molecular-weight heparin therapy were initiated, and she was placed on bed rest with continuous electrocardiographic monitoring. Since admission, she required 2 doses of sublingual nitroglycerin for recurrent angina, and the repeat troponin levels continued to rise. Given her risk factors, plans were made for early coronary angiography. The telemetry nurse calls the on-call physician because of her concern with the patient's mild confusion and increasing need for supplemental oxygen. At bedside evaluation, The vital signs include: heart rate 122/min, blood pressure 89/40 mm Hg, and the pulse oximetry is 91% on 6L of oxygen by nasal cannula. The telemetry and a repeat ECG show sinus tachycardia. She is breathing rapidly, appears confused, and complains of shortness of breath. On physical exam, the skin is cool and clammy and appears pale and dull. She has diffuse bilateral pulmonary crackles, and an S3 gallop is noted on chest auscultation with no new murmurs. She has jugular venous distention to the jaw-line, rapid and faint radial pulses, and 1+ dependent edema. She is immediately transferred to the intensive care unit for respiratory support and precautions for airway security. The bedside sonography shows abnormal hypodynamic anterior wall movement and an ejection fraction of 20%, but no evidence of mitral regurgitation or ventricular shunt. The chest X-ray demonstrates cephalization of pulmonary veins and pulmonary edema. What is the most appropriate next step in the stabilization of this patient?
- A. Obtain blood cultures and start preliminary broad-spectrum antibiotics
- B. Start intravenous fluids and epinephrine therapy
- C. Intubate the patient and perform an emergency cardiocentesis
- D. Initiate dopamine therapy and diuresis (Correct Answer)
- E. Insert two large-bore intravenous catheters and start rapid fluid resuscitation
Acute decompensated heart failure Explanation: ***Initiate dopamine therapy and diuresis***
- This patient is presenting with **cardiogenic shock** secondary to extensive NSTEMI, characterized by **hypotension**, signs of **end-organ hypoperfusion** (confusion, cool clammy skin), **pulmonary edema** (crackles, dyspnea, elevated jugular venous pressure), and **severely reduced ejection fraction**. Dopamine is a vasopressor that can increase cardiac output and blood pressure.
- **Diuresis** with loop diuretics such as furosemide is crucial to reduce the fluid overload contributing to the pulmonary edema and jugular venous distention.
*Obtain blood cultures and start preliminary broad-spectrum antibiotics*
- While infection is a concern in critically ill patients, there are **no signs of infection** in this clinical presentation. The patient's symptoms are clearly attributable to acute cardiac decompensation.
- A delay in treating cardiogenic shock to investigate for infection would be detrimental and potentially fatal.
*Start intravenous fluids and epinephrine therapy*
- Intravenous fluids would **worsen the existing pulmonary edema and fluid overload** in a patient with an ejection fraction of 20% and clinical signs of volume overload (crackles, JVD, S3 gallop).
- Epinephrine is a potent vasopressor but is generally reserved for more severe shock refractory to other inotropes, or in cases of **cardiac arrest**, not typically first-line for cardiogenic shock with significant pulmonary congestion.
*Intubate the patient and perform an emergency cardiocentesis*
- While the patient is confused and has respiratory distress, **intubation** should be considered after hemodynamic stabilization, if respiratory failure persists or worsens.
- **Cardiocentesis** is indicated for **cardiac tamponade**, which is not supported by the absence of an effusion on bedside sonography and the finding of hypodynamic anterior wall movement, which points to pump failure.
*Insert two large-bore intravenous catheters and start rapid fluid resuscitation*
- This patient is in **cardiogenic shock with clear evidence of fluid overload**, including pulmonary edema and elevated jugular venous pressure.
- **Rapid fluid resuscitation would exacerbate heart failure** and worsen respiratory compromise due to increased preload.
Acute decompensated heart failure US Medical PG Question 10: A 36-year-old man presents to his primary care physician because of shortness of breath. He is an office worker who has a mostly sedentary lifestyle; however, he has noticed that recently he feels tired and short of breath when going on long walks with his wife. He also has had a hacking cough that seems to linger, though he attributes this to an upper respiratory tract infection he had 2 months ago. He has diabetes that is well-controlled on metformin and has smoked 1 pack per day for 20 years. Physical exam reveals a large chested man with wheezing bilaterally and mild swelling in his legs and abdomen. The cause of this patient's abdominal and lower extremity swelling is most likely due to which of the following processes?
- A. Excessive protease activity
- B. Damage to kidney tubules
- C. Hyperplasia of mucous glands
- D. Defective protein folding
- E. Right ventricular dysfunction secondary to pulmonary hypertension (Correct Answer)
Acute decompensated heart failure Explanation: ***Right ventricular dysfunction secondary to pulmonary hypertension***
- This patient's long history of smoking, chronic cough, and wheezing suggest significant **chronic obstructive pulmonary disease (COPD)**, which leads to **hypoxemia** and **pulmonary hypertension**.
- **Pulmonary hypertension** increases the workload on the **right ventricle**, eventually leading to **right heart failure** (cor pulmonale), characterized by peripheral edema (leg swelling) and ascites (abdominal swelling).
*Excessive protease activity*
- While excessive protease activity (e.g., elastase) is implicated in the pathogenesis of **emphysema** by destroying alveolar walls, it does not directly cause peripheral edema and ascites.
- This process primarily leads to **airflow obstruction** and **gas exchange abnormalities**, which can indirectly contribute to pulmonary hypertension but is not the direct cause of the peripheral edema.
*Damage to kidney tubules*
- **Acute tubular necrosis** or chronic kidney disease can cause edema due to impaired fluid and electrolyte balance, but the patient's symptoms (dyspnea, wheezing, smoking history) point strongly to a primary pulmonary and cardiac etiology.
- While diabetes can cause nephropathy, there is no information to suggest acute kidney injury or chronic kidney disease leading to such severe edema.
*Hyperplasia of mucous glands*
- **Hyperplasia of mucous glands** in the bronchi is characteristic of **chronic bronchitis**, contributing to the chronic cough and airway obstruction.
- This pathology primarily affects airway clearance and airflow, rather than directly causing systemic edema or ascites.
*Defective protein folding*
- **Defective protein folding**, such as in **alpha-1 antitrypsin deficiency**, can lead to early-onset emphysema and liver disease.
- While this could fit with a pulmonary presentation, it is less common than smoking-induced COPD and does not directly explain the edema and ascites caused by right heart failure.
More Acute decompensated heart failure US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.