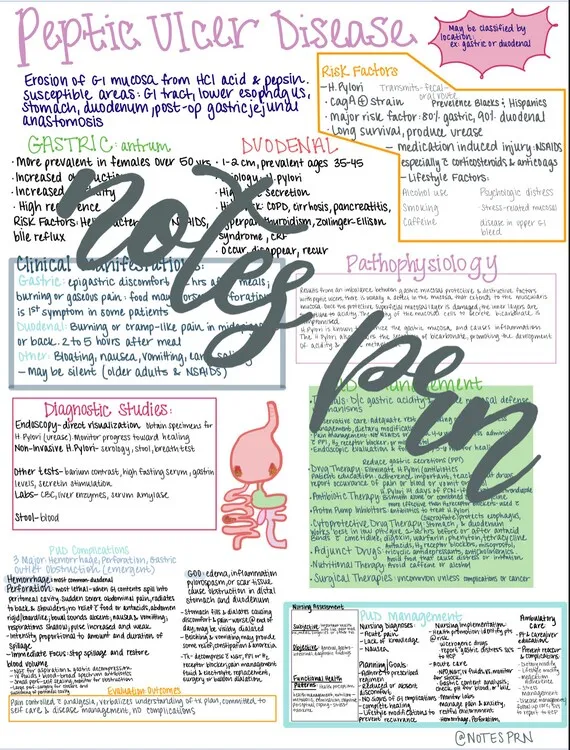
Peptic ulcer disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peptic ulcer disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peptic ulcer disease US Medical PG Question 1: A 56-year-old woman with a longstanding history of gastroesophageal reflux presents for follow-up evaluation of endoscopically confirmed gastric and duodenal ulcers. Her symptoms have been unresponsive to proton pump inhibitors and histamine receptor antagonists in the past. Results for H. pylori infection are still pending. Which of the following changes is expected in the patient's duodenum, given her peptic ulcer disease?
- A. Proliferation of secretin-releasing S cells
- B. Increased secretions from crypts of Lieberkühn
- C. Increased glucose-dependent insulinotropic peptide (GIP) release from K cells
- D. Expansion of gastrointestinal lymphoid tissue
- E. Hyperplasia of submucosal bicarbonate-secreting glands (Correct Answer)
Peptic ulcer disease Explanation: ***Hyperplasia of submucosal bicarbonate-secreting glands***
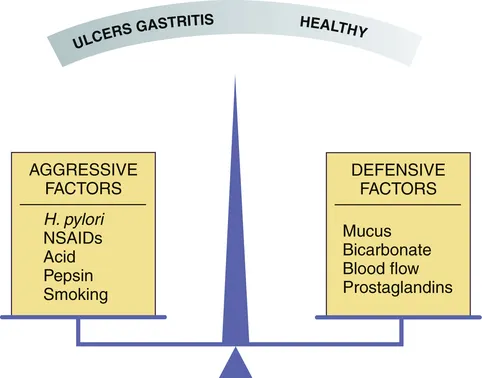
- The duodenum attempts to protect itself from excessive acid due to gastric and duodenal ulcers by increasing **bicarbonate secretion**.
- **Bicarbonate-secreting glands (Brunner's glands)** in the duodenum undergo hyperplasia to neutralize the acidic chyme entering from the stomach, especially when peptic ulcers are present.
*Proliferation of secretin-releasing S cells*
- While secretin is released in response to acid in the duodenum and stimulates bicarbonate secretion, **S cell proliferation** itself is not a primary expected histological change in peptic ulcer disease.
- The main adaptation is the increased functional capacity of bicarbonate-secreting glands, rather than an increase in the number of secretin-producing cells.
*Increased secretions from crypts of Lieberkühn*
- The **crypts of Lieberkühn** are involved in fluid and electrolyte secretion, as well as cell turnover in the small intestine.
- While they contribute to the intestinal environment, their primary role is not to counteract the high acid load seen in peptic ulcer disease, and their secretions are not predominantly bicarbonate-rich.
*Increased glucose-dependent insulinotropic peptide (GIP) release from K cells*
- **GIP** is released from K cells in response to glucose and fat in the duodenum, stimulating insulin secretion.
- Its release is primarily linked to nutrient absorption and glucose homeostasis, not a direct compensatory mechanism for acid-induced peptic ulcer disease.
*Expansion of gastrointestinal lymphoid tissue*
- **Gastrointestinal lymphoid tissue (GALT)**, such as Peyer's patches, is involved in immune surveillance in the intestine.
- While chronic inflammation can lead to lymphoid hyperplasia, it is not a direct or primary protective mechanism against acid per se in peptic ulcer disease; rather, it indicates an immune response, which might occur with H. pylori infection but isn't the duodenum's main anti-acid adaptation.
Peptic ulcer disease US Medical PG Question 2: A 30-year-old man who recently emigrated from Southeast Asia presents with heartburn and a bad taste in his mouth. He says the symptoms have been present for the last 6 months and are much worse at night. He describes the pain as moderate to severe, burning in character, and localized to the epigastric region. He mentions that 1 month ago, he was tested for Helicobacter pylori back in his country and completed a course of multiple antibiotics, but there has been no improvement in his symptoms. Which of the following is the most likely diagnosis in this patient?
- A. Peptic ulcer disease
- B. Gastric MALT (mucosa-associated lymphoid tissue) lymphoma
- C. Duodenal ulcer disease
- D. Gastroesophageal reflux disease (Correct Answer)
- E. Gastric adenocarcinoma
Peptic ulcer disease Explanation: ***Gastroesophageal reflux disease***
- The patient's symptoms of **heartburn**, a **bad taste in his mouth**, and worsening symptoms at **night** are classic presentations of **Gastroesophageal Reflux Disease (GERD)**.
- The failure of **H. pylori eradication therapy** to improve symptoms suggests that H. pylori infection was not the primary cause of his dyspepsia.
*Peptic ulcer disease*
- While **epigastric pain** can be seen in peptic ulcer disease (**PUD**), the prominent symptoms of **heartburn** and a **sour taste in the mouth** are more characteristic of GERD.
- The lack of specific relief with food or worsening with particular food types (common in PUD) makes it less likely, and the failure of H. pylori treatment points away from most common PUD etiologies.
*Gastric MALT (mucosa-associated lymphoid tissue) lymphoma*
- **Gastric MALT lymphoma** is often associated with chronic **H. pylori infection**, but its symptoms are typically more vague, such as **weight loss**, **anorexia**, or **nausea**, and less specifically tied to heartburn and acid reflux.
- The prompt response to H. pylori eradication is often seen in early-stage MALT lymphoma, but the patient's symptoms persisted despite antibiotic treatment.
*Duodenal ulcer disease*
- Similar to peptic ulcer disease, **duodenal ulcers** typically present with **epigastric pain** that often improves with food and worsens 2-3 hours after meals or at night.
- The description of **heartburn** and a **sour taste** makes GERD a more direct fit than duodenal ulcer disease.
*Gastric adenocarcinoma*
- **Gastric adenocarcinoma** presents with symptoms like **weight loss**, **early satiety**, **dysphagia**, or **anemia**, which are not reported in this patient.
- While it can cause epigastric pain, the specific reflux symptoms and absence of "alarm features" like weight loss make it less likely in this young patient.
Peptic ulcer disease US Medical PG Question 3: A 28-year-old graduate student visits the university health clinic for 3-weeks of epigastric pain that worsens with meals, associated with retrosternal pain, early satiety, and bloating. She denies vomiting blood or blood in her stool. She has been consuming large volumes of caffeinated-drinks and fast-food for a month, as she has been studying for her tests. Her family and personal history are unremarkable with no history of gastrointestinal cancer. Her vital signs are within normal limits. Physical examination is only positive for a mild epigastric tenderness. Which of the following is the most appropriate approach in this case?
- A. Treatment with metoclopramide
- B. Upper endoscopy
- C. Fecal antigen testing for Helicobacter pylori (Correct Answer)
- D. Treatment with omeprazole
- E. Barium swallow radiograph
Peptic ulcer disease Explanation: ***Fecal antigen testing for Helicobacter pylori***
- The patient presents with **dyspeptic symptoms** (epigastric pain, early satiety, bloating) and no **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia).
- Given her age (< 60 years) and lack of alarm symptoms, a "test-and-treat" strategy for **Helicobacter pylori** is recommended, with fecal antigen testing being a non-invasive and accurate option.
*Treatment with metoclopramide*
- Metoclopramide is a **prokinetic agent** used for conditions like gastroparesis, not primarily for initial management of undiagnosed dyspepsia.
- While she has early satiety, the primary approach should be to rule out common causes of dyspepsia like **H. pylori** before considering symptomatic treatments for motility issues.
*Upper endoscopy*
- An **upper endoscopy** is indicated if the patient is older (typically > 60 years) or has **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, persistent vomiting).
- This 28-year-old patient lacks any alarm symptoms and is below the age threshold for an immediate endoscopic evaluation for dyspepsia.
*Treatment with omeprazole*
- While a **proton pump inhibitor (PPI)** like omeprazole can treat dyspeptic symptoms, it is not the most appropriate *initial* approach without first testing for **H. pylori**.
- Empiric PPI therapy can **mask H. pylori infection**, potentially delaying appropriate eradication therapy if the test-and-treat strategy is not followed.
*Barium swallow radiograph*
- A **barium swallow** is primarily used to evaluate structural abnormalities of the **esophagus**, such as strictures, diverticula, or achalasia, and is less effective for diagnosing mucosal diseases of the stomach or duodenum.
- It is not the preferred diagnostic test for evaluating dyspepsia or identifying **H. pylori** infection.
Peptic ulcer disease US Medical PG Question 4: A 51-year-old man with a recent diagnosis of peptic ulcer disease currently treated with an oral proton pump inhibitor twice daily presents to the urgent care center complaining of acute abdominal pain which began suddenly less than 2 hours ago. On physical exam, you find his abdomen to be mildly distended, diffusely tender to palpation, and positive for rebound tenderness. Given the following options, what is the next best step in patient management?
- A. Serum gastrin level
- B. Urgent CT abdomen and pelvis (Correct Answer)
- C. H. pylori testing
- D. Abdominal radiographs
- E. Upper endoscopy
Peptic ulcer disease Explanation: ***Urgent CT abdomen and pelvis***
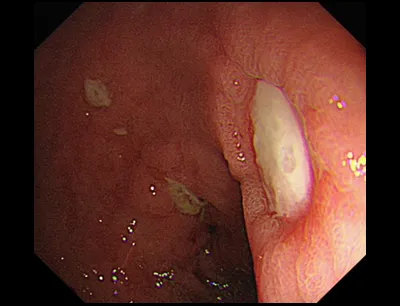
- The sudden onset of severe abdominal pain, diffuse tenderness, and **rebound tenderness** in a patient with a history of peptic ulcer disease (PUD) suggests a **perforated ulcer**, which is a surgical emergency.
- A CT scan is the **most sensitive imaging modality** for detecting **free air** (pneumoperitoneum) and can confirm the diagnosis with >95% sensitivity, helping to localize the perforation and identify complications such as abscess formation.
- CT also helps evaluate alternative diagnoses in the acute abdomen and provides detailed anatomic information for surgical planning.
*Serum gastrin level*
- This test is primarily used in the diagnosis of **Zollinger-Ellison syndrome**, a rare condition characterized by gastrinomas leading to severe, refractory PUD.
- It is not indicated in an acute emergency setting with signs of perforation, as it would delay critical diagnostic imaging and management.
*H. pylori testing*
- **_H. pylori_ infection** is a common cause of PUD, but testing for it is part of routine initial management or follow-up for chronic disease.
- Testing would not address the immediate life-threatening complication of suspected perforation and would delay definitive diagnosis.
*Abdominal radiographs*
- An upright chest X-ray or abdominal radiograph can detect **free air under the diaphragm** in cases of perforation and is a reasonable initial imaging test.
- However, plain radiographs have lower sensitivity (75-80%) compared to CT scan and may miss smaller perforations or provide insufficient information about the location and extent of injury.
- In modern practice with readily available CT, cross-sectional imaging is preferred for its superior diagnostic accuracy in evaluating the acute abdomen.
*Upper endoscopy*
- **Upper endoscopy** is a valuable diagnostic and therapeutic tool for stable PUD but is **absolutely contraindicated** in cases of suspected or confirmed hollow viscus perforation.
- Introducing an endoscope with air insufflation could worsen the perforation and lead to further contamination of the peritoneal cavity, increasing morbidity and mortality.
Peptic ulcer disease US Medical PG Question 5: A 45-year-old man is brought to the emergency department because of severe abdominal pain for the past 2 hours. He has a 2-year history of burning epigastric pain that gets worse with meals. His pulse is 120/min, respirations are 22/min, and blood pressure is 60/40 mm Hg. Despite appropriate lifesaving measures, he dies. At autopsy, examination shows erosion of the right gastric artery. Perforation of an ulcer in which of the following locations most likely caused this patient's findings?
- A. Anterior duodenum
- B. Posterior duodenum
- C. Lesser curvature of the stomach (Correct Answer)
- D. Greater curvature of the stomach
- E. Fundus of the stomach
Peptic ulcer disease Explanation: ***Lesser curvature of the stomach***
- Erosion of the **right gastric artery** by a gastric ulcer is characteristic of an ulcer located on the **lesser curvature of the stomach**.
- Ulcers in this location can erode into adjacent blood vessels, leading to **severe hemorrhage** as evidenced by the patient's **hypotension** and subsequent death.
*Anterior duodenum*
- Ulcers in the **anterior duodenum** typically present with **perforation into the peritoneal cavity**, leading to generalized peritonitis, not primarily hemorrhage from a major artery.
- While bleeding can occur, it's usually from smaller duodenal arteries and less commonly involves large arteries like the right gastric artery.
*Posterior duodenum*
- Ulcers in the **posterior duodenum** are known to erode into the **gastroduodenal artery**, leading to massive upper gastrointestinal bleeding.
- This is a distinct arterial involvement compared to the erosion of the right gastric artery.
*Greater curvature of the stomach*
- Ulcers on the **greater curvature of the stomach** are less common and often associated with malignancy.
- If they bleed, it would typically involve branches of the **gastroepiploic arteries**, not the right gastric artery.
*Fundus of the stomach*
- Ulcers in the **fundus** are rare.
- If a vessel were involved, it would typically be a short gastric artery, not the right gastric artery which courses along the lesser curvature.
Peptic ulcer disease US Medical PG Question 6: A 45-year-old bank manager presents to the emergency department with abdominal pain for the last 2 weeks. The patient also vomited a few times, and in the last hour, he vomited blood as well. His pain was mild in the beginning but now he describes the pain as 8/10 in intensity, stabbing, and relentless. Ingestion of food makes it better as does the consumption of milk. He has a heart rate of 115/min. His blood pressure is 85/66 mm Hg standing, and 96/83 mm Hg lying down. He appears pale and feels dizzy. An intravenous line is started and a bolus of fluids is administered, which improved his vital signs. After stabilization, an esophagogastroduodenoscopy (EGD) is performed. There is a fair amount of blood in the stomach but after it is washed away, there are no abnormalities. A bleeding duodenal ulcer is seen located on the posteromedial wall of the duodenal bulb. Which artery is at risk from this ulcer?
- A. Superior pancreaticoduodenal artery
- B. Gastroduodenal artery (Correct Answer)
- C. Right gastroepiploic artery
- D. Inferior pancreaticoduodenal artery
- E. Dorsal pancreatic artery
Peptic ulcer disease Explanation: **Gastroduodenal artery**
- The **gastroduodenal artery (GDA)** runs immediately posterior to the **duodenal bulb** and is the most common artery eroded by posterior duodenal ulcers.
- **Bleeding** from a posterior duodenal ulcer can be severe and life-threatening due to the proximity and size of the GDA.
*Superior pancreaticoduodenal artery*
- The superior pancreaticoduodenal artery branches off the GDA and supplies the head of the pancreas and duodenum.
- While it contributes to the duodenal blood supply, it is less commonly directly eroded by a duodenal bulb ulcer compared to its parent artery, the GDA.
*Right gastroepiploic artery*
- The right gastroepiploic artery (right gastroomental artery) branches from the GDA and runs along the greater curvature of the stomach.
- It is unlikely to be affected by an ulcer in the duodenal bulb due to its anatomical location away from the posterior duodenal wall.
*Inferior pancreaticoduodenal artery*
- The inferior pancreaticoduodenal artery branches from the superior mesenteric artery and supplies the head of the pancreas and duodenum.
- It is anatomically located inferior and posterior to the duodenal bulb, making it less vulnerable to direct erosion by an ulcer in the duodenal bulb, which is typically supplied by branches of the GDA.
*Dorsal pancreatic artery*
- The dorsal pancreatic artery is a branch of the splenic artery or hepatic artery, supplying the body and tail of the pancreas.
- It is anatomically situated away from the duodenal bulb and would not be at risk from a duodenal bulb ulcer.
Peptic ulcer disease US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Peptic ulcer disease Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Peptic ulcer disease US Medical PG Question 8: A 46-year-old woman presents to the emergency department complaining of abdominal pain, nausea, and vomiting approximately 4 hours after a fatty meal. She reports that this has happened before, but this episode is worse. The vomit was non-bilious and did not contain any blood. She recalls frequent episodes of vague epigastric pain that often wakes her up during the night. Over the counter omeprazole and a small meal or snack would provide some relief in the past. The patient also mentions recent anorexia and early satiety. She takes over the counter ibuprofen several times a week for headaches. Blood pressure is 125/82 mm Hg, pulse is 102/min, and respiratory rate is 19/min. On physical examination, she has hypoactive bowel sounds, and her abdomen seems grossly distended and tympanic on percussion. Which of the following is most consistent with a duodenal ulcer?
- A. Early satiety
- B. Ibuprofen use
- C. Non-bilious vomiting
- D. Omeprazole provides relief of the symptoms
- E. Food ingestion provides relief of the symptoms (Correct Answer)
Peptic ulcer disease Explanation: ***Food ingestion provides relief of the symptoms***
- **Duodenal ulcer pain** is characteristically relieved by eating food, as acid is neutralized or diluted, and the pylorus may spasm, preventing acid from reaching the ulcer.
- The patient's history of relief with a "small meal or snack" is a classic presentation consistent with a duodenal ulcer.
*Early satiety*
- **Early satiety** is more commonly associated with conditions causing gastric outlet obstruction or impaired gastric emptying, such as **gastric ulcers** or malignancy.
- While possible, it is not the most consistent symptom specifically pointing to a duodenal ulcer, whose pain often *improves* with food.
*Ibuprofen use*
- **NSAID use** like ibuprofen can *cause* both gastric and duodenal ulcers by inhibiting prostaglandin synthesis, which protects the gastric and duodenal mucosa.
- However, the question asks what is *most consistent* with a duodenal ulcer among the given options; ibuprofen use is a risk factor, not a direct symptom-relief characteristic.
*Non-bilious vomiting*
- **Non-bilious vomiting** simply indicates that bile has not passed into the stomach, which can occur in various conditions, including non-obstructive causes or proximal obstructions.
- While it can be present, it is not a specific diagnostic feature distinguishing a duodenal ulcer from many other gastrointestinal issues.
*Omeprazole provides relief of the symptoms*
- **Omeprazole** is a **proton pump inhibitor (PPI)** and provides relief for symptoms related to acid production, including both **gastric and duodenal ulcers**, and **gastroesophageal reflux disease (GERD)**.
- Therefore, its effectiveness is not specific enough to definitively point to a duodenal ulcer over other acid-related conditions.
Peptic ulcer disease US Medical PG Question 9: A 42-year-old woman comes to the emergency department with gradually worsening pain in the abdomen and right flank. The abdominal pain started one week ago and is accompanied by foul-smelling, lightly-colored diarrhea. The flank pain started two days ago and is now an 8 out of 10 in intensity. It worsens on rapid movement. She has a history of intermittent knee arthralgias. She has refractory acid reflux and antral and duodenal peptic ulcers for which she currently takes omeprazole. She appears fatigued. Her pulse is 89/min and her blood pressure is 110/75 mmHg. Abdominal examination shows both epigastric and right costovertebral angle tenderness. Urine dipstick shows trace red blood cells (5–10/μL). Ultrasonography shows mobile hyperechogenic structures in the right ureteropelvic junction. Further evaluation is most likely going to show which of the following findings?
- A. Cutaneous flushing
- B. Hypercalcemia (Correct Answer)
- C. Hypertensive crisis
- D. Pulmonary stenosis
- E. QT prolongation on ECG
Peptic ulcer disease Explanation: ***Hypercalcemia***
- This patient's constellation of symptoms—kidney stones (right flank pain, hyperechogenic structures in the ureteropelvic junction), **refractory peptic ulcers**, and diarrhea—is highly suggestive of **Multiple Endocrine Neoplasia type 1 (MEN1)**.
- The refractory peptic ulcers in multiple locations (antral and duodenal) with diarrhea strongly suggest a **gastrinoma (Zollinger-Ellison syndrome)**, the most common functional pancreatic tumor in MEN1.
- **Hypercalcemia** from **primary hyperparathyroidism** is the most common (>95%) and often the **earliest biochemical manifestation** of MEN1, presenting years before pancreatic or pituitary tumors.
- Hypercalcemia leads to hypercalciuria and **calcium oxalate or calcium phosphate kidney stones**, explaining her flank pain and urinary findings.
- The intermittent knee arthralgias may represent bone/joint pain from hyperparathyroid bone disease.
*Cutaneous flushing*
- **Flushing** is characteristically associated with **carcinoid syndrome** (serotonin-secreting tumors) or **VIPoma** (vasoactive intestinal peptide-secreting tumors).
- While MEN1 can involve pancreatic neuroendocrine tumors, gastrinomas do not typically cause flushing, and this patient's presentation points to gastrinoma, not carcinoid.
*Hypertensive crisis*
- A **hypertensive crisis** with episodic severe hypertension, headaches, and palpitations suggests **pheochromocytoma**.
- Pheochromocytoma is a feature of **MEN2** (along with medullary thyroid carcinoma), not MEN1.
- This patient's blood pressure is normal (110/75 mmHg).
*Pulmonary stenosis*
- **Pulmonary stenosis** is a congenital cardiac defect seen in conditions like **Noonan syndrome** or as an isolated congenital heart disease.
- It has no association with MEN1 or endocrine neoplasia syndromes.
*QT prolongation on ECG*
- **QT prolongation** occurs with electrolyte abnormalities (hypokalemia, hypomagnesemia, hypocalcemia), certain medications, or congenital long QT syndromes.
- Notably, **hypercalcemia actually causes QT shortening**, not prolongation, making this finding unlikely in this patient.
Peptic ulcer disease US Medical PG Question 10: A 38-year-old man comes to the physician because of an 8-month history of upper abdominal pain. During this period, he has also had nausea, heartburn, and multiple episodes of diarrhea with no blood or mucus. He has smoked one pack of cigarettes daily for the past 18 years. He does not use alcohol or illicit drugs. Current medications include an antacid. The abdomen is soft and there is tenderness to palpation in the epigastric and umbilical areas. Upper endoscopy shows several ulcers in the duodenum and the upper jejunum as well as thick gastric folds. Gastric pH is < 2. Biopsies from the ulcers show no organisms. Which of the following tests is most likely to confirm the diagnosis?
- A. Urea breath test
- B. 24-hour esophageal pH monitoring
- C. Serum vasoactive intestinal polypeptide level
- D. Urine metanephrine levels
- E. Fasting serum gastrin level (Correct Answer)
Peptic ulcer disease Explanation: ***Fasting serum gastrin level***
- The patient's presentation with multiple, refractory **duodenal and jejunal ulcers**, thick gastric folds, and severely low gastric pH (<2) strongly suggests **Zollinger-Ellison syndrome (ZES)**, caused by a gastrin-secreting tumor (gastrinoma).
- Measuring **fasting serum gastrin** is the most direct way to confirm excess gastrin production characteristic of ZES.
*Urea breath test*
- This test is primarily used for diagnosing **Helicobacter pylori infection**, which can cause peptic ulcers.
- However, the presentation of **multiple, refractory ulcers** extending into the jejunum, thick gastric folds, and very low gastric pH are not typical for *H. pylori* alone, and biopsies showed no organisms, making this less likely the primary issue.
*24-hour esophageal pH monitoring*
- This test is used to diagnose **gastroesophageal reflux disease (GERD)** by measuring esophageal acid exposure.
- While heartburn is present, the widespread, severe ulcers in the duodenum and jejunum, along with thick gastric folds and very low gastric pH, point to a more systemic problem of acid hypersecretion rather than just reflux.
*Serum vasoactive intestinal polypeptide level*
- Elevated **VIP (vasoactive intestinal polypeptide) levels** are indicative of a **VIPoma**, a tumor that causes secretory diarrhea.
- While the patient has diarrhea, the prominent features of severe, widespread ulcers and gastric acid hypersecretion are not hallmarks of a VIPoma; they are characteristic of gastrinoma.
*Urine metanephrine levels*
- Measuring **urine metanephrine levels** is used to screen for **pheochromocytoma**, an adrenal tumor that secretes catecholamines.
- Pheochromocytoma symptoms typically include hypertension, palpitations, and headaches, which are not present in this patient's clinical picture of persistent acid-related symptoms and diarrhea.
More Peptic ulcer disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.