Malabsorption syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Malabsorption syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Malabsorption syndromes US Medical PG Question 1: A 21-year-old woman comes to the physician because of a 2-month history of fatigue, intermittent abdominal pain, and bulky, foul-smelling diarrhea. She has had a 4-kg (8-lb 12-oz) weight loss during this period despite no changes in appetite. Examination of the abdomen shows no abnormalities. Staining of the stool with Sudan III stain shows a large number of red droplets. Which of the following is the most likely underlying cause of this patient’s symptoms?
- A. Ulcerative colitis
- B. Lactose intolerance
- C. Amebiasis
- D. Celiac disease (Correct Answer)
- E. Carcinoid syndrome
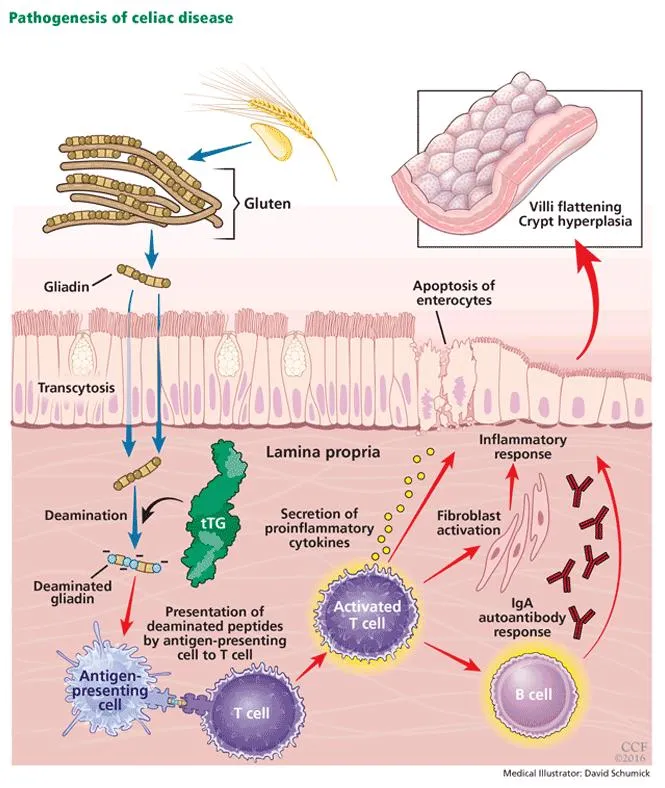
Malabsorption syndromes Explanation: ***Celiac disease***
- The combination of **fatigue, abdominal pain**, weight loss, and **bulky, foul-smelling diarrhea** suggests malabsorption [1].
- **Sudan III stain** revealing red droplets indicates **steatorrhea** (fat in stool), a hallmark of malabsorption, often seen in celiac disease due to damage to the small intestinal villi from **gluten exposure** [1].
*Ulcerative colitis*
- Characterized by **bloody diarrhea**, tenesmus, and urgency, which are not described in this patient.
- Primarily affects the **colon** and typically does not present with significant steatorrhea [2].
*Lactose intolerance*
- Causes watery diarrhea, bloating, and gas after consuming dairy products due to **lactase deficiency** [2].
- Does not typically lead to significant weight loss or steatorrhea with bulky, foul-smelling stools.
*Amebiasis*
- An infection with *Entamoeba histolytica* causing **bloody, mucoid diarrhea** (dysentery), abdominal pain, and fever.
- While it can cause weight loss, it does not typically present with steatorrhea or bulky, foul-smelling stools, and the diarrhea is often bloody.
*Carcinoid syndrome*
- Presents with symptoms such as **flushing, diarrhea**, and bronchospasm, often due to serotonin overproduction.
- While diarrhea is a prominent symptom, it is usually watery and secretory, not typically bulky, foul-smelling, or associated with steatorrhea.
Malabsorption syndromes US Medical PG Question 2: A 28-year-old man presents to his primary care provider complaining of intermittent stomach pain, non-bloody diarrhea, and weight loss for the last 3 months. He has occasional abdominal pain and fever. This condition makes studying difficult. He has tried omeprazole and dietary changes with no improvement. Past medical history is significant for occasional pain in the wrists and knees for several years. He takes ibuprofen for pain relief. His temperature is 38°C (100.4°F). On mental status examination, short-term memory is impaired. Attention and concentration are reduced. Examination shows no abnormalities or tenderness of the wrists or knees. There are no abnormalities on heart and lung examinations. Abdominal examination is normal. Upper endoscopy shows normal stomach mucosa but in the duodenum, there is pale yellow mucosa with erythema and ulcerations. Biopsies show infiltration of the lamina propria with periodic acid-Schiff (PAS)-positive macrophages. Which of the following best explains these findings?
- A. Wilson’s disease
- B. Celiac disease
- C. Giardia lamblia infection
- D. Whipple’s disease (Correct Answer)
- E. Crohn’s disease
Malabsorption syndromes Explanation: ***Whipple’s disease***
- The combination of **gastrointestinal symptoms** (diarrhea, weight loss, abdominal pain) with **arthralgia**, **fever**, **neurological symptoms** (impaired short-term memory, reduced attention/concentration), and **PAS-positive macrophages** in duodenal biopsies is highly characteristic of Whipple's disease.
- This multisystemic bacterial infection, caused by *Tropheryma whipplei*, often presents with diverse, non-specific symptoms before the classic GI findings, and central nervous system involvement is common.
*Wilson’s disease*
- This is a disorder of **copper metabolism** leading to copper accumulation in organs like the liver, brain, and eyes (Kayser-Fleischer rings).
- While it can cause neurological symptoms and liver disease, the GI and biopsy findings (PAS-positive macrophages) are not consistent with Wilson's disease.
*Celiac disease*
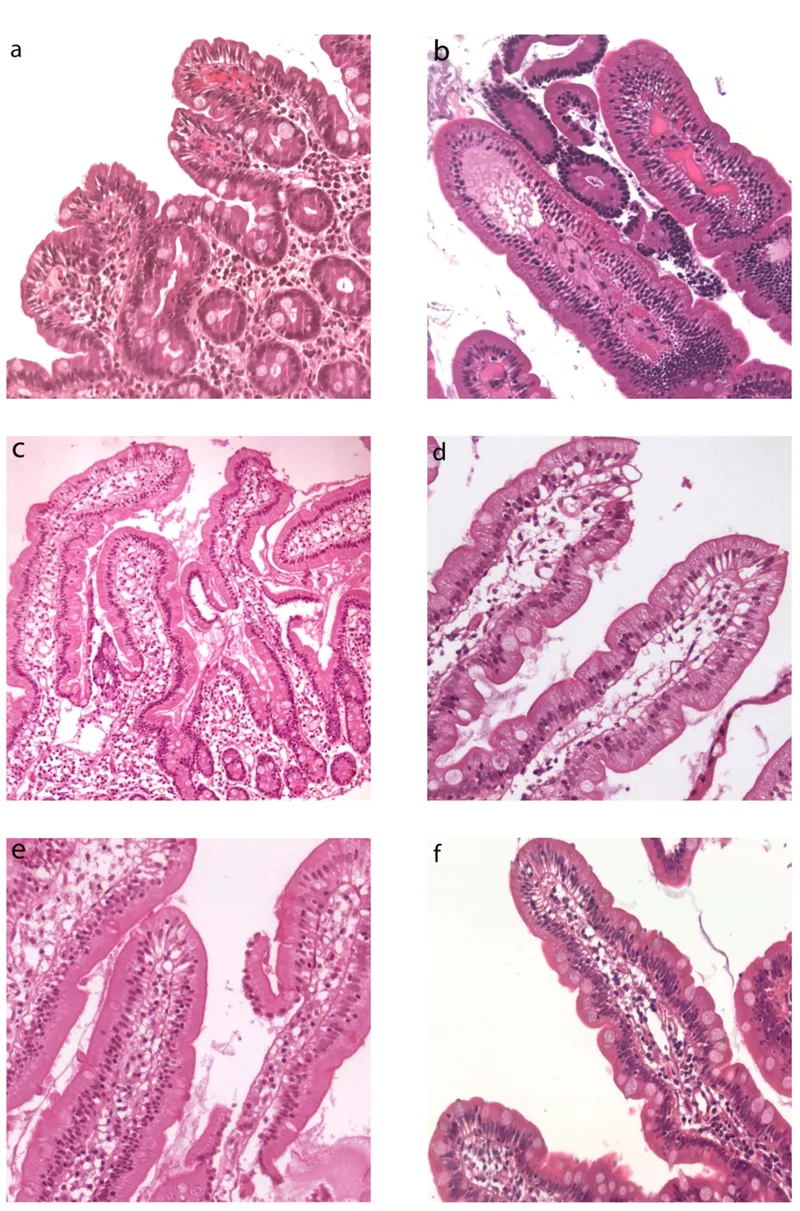
- Characterized by **malabsorption** due to an immune reaction to gluten, presenting with diarrhea, weight loss, and abdominal pain.
- However, jejunal biopsies would show **villous atrophy** and crypt hyperplasia, not PAS-positive macrophages, and neurological findings are less common and typically peripheral in nature.
*Giardia lamblia infection*
- This parasitic infection causes **diarrhea**, abdominal cramps, and malabsorption.
- Diagnosis is usually made by identifying **trophozoites or cysts** in stool samples or duodenal aspirates/biopsies, not PAS-positive macrophages.
*Crohn’s disease*
- An **inflammatory bowel disease** characterized by transmural inflammation, skip lesions, and granulomas, which can affect any part of the GI tract.
- While it can present with abdominal pain, diarrhea, weight loss, and arthralgia, the presence of **PAS-positive macrophages** in the duodenum and neurological involvement are not typical features of Crohn's disease.
Malabsorption syndromes US Medical PG Question 3: A 23-year-old man presents to the office complaining of weight loss and fatigue for the past 2 months. He states that he has been experiencing foul-smelling, light-colored stools but thinks it is because he hasn’t been eating well, recently. He has a past medical history significant for cystic fibrosis, which is well-controlled medically. He denies any shortness of breath, chest or abdominal pain, nausea, vomiting, or melena. On physical examination, his skin is pale and dry. Which of the following would be the most likely etiology of a malabsorption syndrome giving rise to this patient’s current condition?
- A. Decreased recycling of bile acids
- B. Pancreatic insufficiency (Correct Answer)
- C. Autoimmune damage to parietal cells
- D. Chronic damage to intestinal mucosa
- E. Damage to intestinal brush border
Malabsorption syndromes Explanation: ***Pancreatic insufficiency***
- Cystic fibrosis typically causes **exocrine pancreatic insufficiency** due to thick secretions blocking the pancreatic ducts, leading to malabsorption of fats and fat-soluble vitamins.
- **Foul-smelling, light-colored stools** (steatorrhea) are a classic symptom of fat malabsorption resulting from inadequate lipase production.
*Decreased recycling of bile acids*
- This typically results in **fat malabsorption**, but it is commonly associated with diseases affecting the **terminal ileum** (e.g., Crohn's disease, resection).
- While it can cause steatorrhea, it is not the primary or most common cause of malabsorption in cystic fibrosis.
*Autoimmune damage to parietal cells*
- This condition leads to **pernicious anemia** due to a lack of intrinsic factor and subsequent **vitamin B12 malabsorption**.
- It does not typically cause **steatorrhea** or generalized fat malabsorption, and it is not directly associated with cystic fibrosis.
*Chronic damage to intestinal mucosa*
- This points towards conditions like **celiac disease** or severe inflammatory bowel disease, which impair nutrient absorption through mucosal injury.
- While cystic fibrosis can have gastrointestinal manifestations, primary mucosal damage is not the leading cause of malabsorption, and the patient's symptoms are more consistent with fat malabsorption.
*Damage to intestinal brush border*
- This is characteristic of conditions like **lactase deficiency** or **celiac disease**, which affect the absorption of specific nutrients (e.g., carbohydrates).
- While it causes malabsorption, the patient's presentation with **steatorrhea** points more specifically to fat malabsorption, which is primarily due to pancreatic enzyme deficiency in cystic fibrosis.
Malabsorption syndromes US Medical PG Question 4: A 63-year-old man comes to the physician with a 4-week history of fatigue, crampy abdominal pain, watery diarrhea, and pain in his mouth and gums. He returned from a 2-week trip to the Dominican Republic 2 months ago. He has smoked one pack of cigarettes daily for 45 years. Examination shows three 1.5-cm, painful ulcers in the mouth. Abdominal examination shows mild tenderness to palpation in the right lower quadrant without guarding or rebound. His hemoglobin concentration is 11.2 g/dL, mean corpuscular volume is 75 fL, and leukocyte count is 11,900/mm³. Colonoscopy shows a cobblestone mucosa. A photomicrograph of a biopsy specimen is shown. Which of the following is the most likely diagnosis?
- A. Behcet disease
- B. Tropical sprue
- C. Ulcerative colitis
- D. Crohn disease (Correct Answer)
- E. Whipple disease
Malabsorption syndromes Explanation: ***Crohn disease***
- The combination of **crampy abdominal pain**, **watery diarrhea**, **oral ulcers**, and **cobblestone mucosa** seen on colonoscopy strongly suggests Crohn disease. Crohn disease can affect any part of the gastrointestinal tract from mouth to anus, and oral manifestations like aphthous ulcers are common.
- The **microcytic anemia** (hemoglobin 11.2 g/dL, MCV 75 fL) is consistent with **chronic blood loss** and **iron malabsorption** often seen in Crohn disease. The elevated leukocyte count (11,900/mm³) indicates inflammation.
*Behcet disease*
- Behcet disease is characterized by recurrent **oral aphthous ulcers**, genital ulcers, and uveitis. While oral ulcers are present, the significant **gastrointestinal symptoms** (crampy abdominal pain, watery diarrhea, cobblestone mucosa) are not typical primary features of Behcet disease.
- Although it can rarely involve the GI tract, it typically doesn't present with extensive bowel involvement resembling inflammatory bowel disease to this degree, nor does it typically cause microcytic anemia from chronic GI blood loss.
*Tropical sprue*
- Tropical sprue typically presents with chronic **malabsorption**, foul-smelling diarrhea, and weight loss, occurring after travel to tropical regions. While the patient visited the Dominican Republic, the key findings of **oral ulcers** and **cobblestone mucosa** are not characteristic of tropical sprue.
- Tropical sprue is primarily a disease of the small intestine characterized by villous atrophy, not typically presenting with the "cobblestone" appearance associated with transmural inflammation seen in Crohn’s.
*Ulcerative colitis*
- Ulcerative colitis is characterized by continuous inflammation of the **colon and rectum**, typically presenting with bloody diarrhea and abdominal pain. While GI symptoms are present, the patient's **oral ulcers** and the finding of **cobblestone mucosa** strongly argue against ulcerative colitis.
- Ulcerative colitis affects only the colon and does not cause oral ulcers or skip lesions or transmural inflammation; the "cobblestone" appearance is indicative of deep fissures and ulcers separated by edematous mucosa, characteristic of Crohn disease.
*Whipple disease*
- Whipple disease is a rare systemic infection caused by *Tropheryma whipplei*, presenting with malabsorption, arthralgia, neurological symptoms, and lymphadenopathy. While GI symptoms like diarrhea and abdominal pain may occur, **oral ulcers** are not a typical feature, and the **colonoscopy findings** (cobblestone mucosa) are not characteristic of Whipple disease.
- Biopsy in Whipple disease would show **foamy macrophages** in the lamina propria that stain positive with periodic acid-Schiff (PAS), which is not indicated by the provided information.
Malabsorption syndromes US Medical PG Question 5: A 15-year-old girl is brought to the physician because of an 8-month history of fatigue, intermittent postprandial abdominal bloating and discomfort, foul-smelling, watery diarrhea, and a 7-kg (15-lb) weight loss. She developed a pruritic rash on her knees 3 days ago. Physical examination shows several tense, excoriated vesicles on the knees bilaterally. The abdomen is soft and nontender. Her hemoglobin concentration is 8.2 g/dL and mean corpuscular volume is 76 μm3. Further evaluation of this patient is most likely to show which of the following findings?
- A. IgA tissue transglutaminase antibodies (Correct Answer)
- B. Elevated serum amylase concentration
- C. Intraluminal esophageal membrane
- D. Periodic acid-Schiff-positive macrophages
- E. Positive hydrogen breath test
Malabsorption syndromes Explanation: ***IgA tissue transglutaminase antibodies***
- The patient's symptoms of **fatigue, abdominal bloating and discomfort, watery diarrhea, weight loss, iron deficiency anemia**, and a **pruritic rash (dermatitis herpetiformis)** are highly suggestive of **celiac disease**.
- **IgA tissue transglutaminase (tTG) antibodies** are the most sensitive and specific serological test for celiac disease.
*Elevated serum amylase concentration*
- **Elevated serum amylase** is typically indicative of **pancreatitis**, which is not supported by the patient's symptoms (e.g., severe epigastric pain radiating to the back).
- While malabsorption can lead to some pancreatic dysfunction, it would not be the primary diagnostic finding for this presentation.
*Intraluminal esophageal membrane*
- **Intraluminal esophageal membranes** or **webs** are typically associated with conditions like **Plummer-Vinson syndrome** or **eosinophilic esophagitis**, presenting with dysphagia.
- These findings do not explain the patient's prominent gastrointestinal symptoms, weight loss, rash, or anemia.
*Periodic acid-Schiff-positive macrophages*
- **Periodic acid-Schiff (PAS)-positive macrophages** in the lamina propria are characteristic of **Whipple disease**.
- Whipple disease typically presents with polyarthralgia, lymphadenopathy, and neurological symptoms in addition to malabsorption, which are not described here.
*Positive hydrogen breath test*
- A **positive hydrogen breath test** suggests **small intestinal bacterial overgrowth (SIBO)** or **lactose intolerance**.
- While SIBO can cause bloating and diarrhea, it does not explain the pruritic rash (dermatitis herpetiformis) or the severity of the anemia and weight loss as the primary diagnosis.
Malabsorption syndromes US Medical PG Question 6: A 29-year-old man presents to clinic with a complaint of fatigue that has developed over the past 6 months. Upon questioning, he endorses abdominal pain, non-bloody diarrhea, and decreased appetite over the past year. He denies recent travel outside of the country or eating uncooked meats. On exam, his temperature is 99.0°F (37.2°C), blood pressure is 126/78 mmHg, pulse is 93/min, and respirations are 12/min. Notably, the abdominal exam is unremarkable aside from some tenderness to palpation near the umbilicus. His colonoscopy demonstrates perianal inflammation with a normal rectum, and biopsies of suspicious lesions in the transverse colon reveal transmural inflammation. Which one of the following is most strongly associated with the patient’s condition?
- A. Positive serum transglutaminase antibodies
- B. Kidney stones (Correct Answer)
- C. Endocarditis
- D. Colorectal cancer
- E. Hemolytic anemia
Malabsorption syndromes Explanation: ***Kidney stones***
- Patients with **Crohn's disease**, particularly those with ileal involvement, are at increased risk for **calcium oxalate kidney stones** due to increased oxalate absorption.
- In Crohn's disease, fat malabsorption occurs because bile salts are not reabsorbed in the inflamed terminal ileum. This leads to free fatty acids in the colon that bind calcium, leaving oxalate unbound and available for absorption. The excess oxalate is then excreted in urine, promoting calcium oxalate stone formation.
- This is one of the most well-established extraintestinal complications of Crohn's disease.
*Positive serum transglutaminase antibodies*
- These antibodies are a hallmark of **celiac disease**, which is characterized by villous atrophy in the small intestine due to gluten sensitivity.
- The patient's clinical presentation and colonoscopy findings (transmural inflammation, perianal disease, skip lesions) are pathognomonic for Crohn's disease, not celiac disease.
*Endocarditis*
- **Endocarditis** is an infection of the heart valves, typically caused by bacteremia, and is not a recognized association with Crohn's disease.
- While chronic inflammatory conditions can have cardiovascular effects, endocarditis is not a characteristic or strong complication of Crohn's disease.
*Colorectal cancer*
- While patients with **ulcerative colitis** have a significantly increased risk of colorectal cancer (especially with pancolitis and longer disease duration), the risk in **Crohn's disease** is lower and less direct.
- Crohn's disease can increase colorectal cancer risk with extensive colonic involvement, but this patient's presentation shows predominantly small bowel and perianal disease, making kidney stones a much stronger and more immediate association.
*Hemolytic anemia*
- **Hemolytic anemia** is not a characteristic complication of Crohn's disease.
- Anemia in Crohn's disease is more commonly due to **iron deficiency** from chronic blood loss or malabsorption, or **anemia of chronic disease** from chronic inflammation, rather than hemolysis.
Malabsorption syndromes US Medical PG Question 7: A 19-year-old woman with a known history of malabsorption presents with a painful red tongue, red eyes, and cracked lips. She says her symptoms gradually began 4 months ago after moving away from home for college. She also complains of photophobia, spontaneous lacrimation, and itchy dermatitis. Past medical history is significant for a long-standing malabsorption syndrome, which she says that she hasn't been able to maintain her normal diet or take her vitamins regularly due to her busy schedule. The patient is afebrile and vital signs are within normal limits. On physical examination, she has a malnourished appearance with significant pallor. Conjunctival injection is present bilaterally. Which of the following diagnostic tests will be most helpful to support the diagnosis of the most likely vitamin deficiency in this patient?
- A. Measurement of erythrocyte folate levels
- B. Measurement of erythrocyte glutathione reductase activity (Correct Answer)
- C. Measurement of erythrocyte glutamic oxaloacetic transaminase activity
- D. Measurement of erythrocyte transketolase activity
- E. Measurement of serum methylmalonic acid levels
Malabsorption syndromes Explanation: ***Measurement of erythrocyte glutathione reductase activity***
- This measures the activity of an enzyme that requires **flavin adenine dinucleotide (FAD)**, a coenzyme derived from **riboflavin (vitamin B2)**. Reduced activity, especially after FAD stimulation, suggests **riboflavin deficiency**.
- The patient's symptoms (painful red tongue, red eyes, cracked lips, photophobia, spontaneous lacrimation, itchy dermatitis) are classic manifestations of **ariboflavinosis**, exacerbated by her history of malabsorption and poor dietary intake.
*Measurement of erythrocyte folate levels*
- This test is used to diagnose **folate (vitamin B9) deficiency**, which can cause **macrocytic anemia** and megaloblastic changes.
- While malabsorption can lead to folate deficiency, the patient's specific constellation of symptoms (cheilosis, glossitis, angular stomatitis, ocular symptoms) is more indicative of **riboflavin deficiency**, not folate.
*Measurement of erythrocyte glutamic oxaloacetic transaminase activity*
- This (also known as AST or Aspartate Aminotransferase) enzyme requires **pyridoxal phosphate (vitamin B6)** as a coenzyme. Measurement of its activity, particularly with and without B6 supplementation, can assess **vitamin B6 status**.
- While B6 deficiency can present with dermatitis and glossitis, the prominent ocular symptoms and cheilosis point more strongly towards **riboflavin deficiency**.
*Measurement of erythrocyte transketolase activity*
- This test assesses **thiamine (vitamin B1) status**, as transketolase requires **thiamine pyrophosphate (TPP)** as a cofactor. Reduced activity, especially after TPP stimulation, indicates **thiamine deficiency (beri-beri)**.
- Thiamine deficiency typically presents with neurological symptoms (dry beri-beri) or cardiovascular symptoms (wet beri-beri), which are not described in this patient's presentation.
*Measurement of serum methylmalonic acid levels*
- Elevated **methylmalonic acid (MMA)** levels in serum are a highly sensitive and specific indicator of **vitamin B12 deficiency**, as B12 is essential for the conversion of MMA to succinyl CoA.
- While vitamin B12 deficiency can cause glossitis and neurological symptoms, the patient's specific ocular and dermatological findings are not characteristic of B12 deficiency.
Malabsorption syndromes US Medical PG Question 8: A 54-year-old man comes to the physician because of diarrhea that has become progressively worse over the past 4 months. He currently has 4–6 episodes of foul-smelling stools per day. Over the past 3 months, he has had fatigue and a 5-kg (11-lb) weight loss. He returned from Bangladesh 6 months ago after a year-long business assignment. He has osteoarthritis and hypertension. Current medications include amlodipine and naproxen. He appears pale and malnourished. His temperature is 37.3°C (99.1°F), pulse is 76/min, and blood pressure is 140/86 mm Hg. Examination shows pale conjunctivae and dry mucous membranes. Angular stomatitis and glossitis are present. The abdomen is distended but soft and nontender. Rectal examination shows no abnormalities. Laboratory studies show:
Hemoglobin 8.9 g/dL
Leukocyte count 4100/mm3
Platelet count 160,000/mm3
Mean corpuscular volume 110 μm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/l
K+ 3.3 mEq/L
Creatinine 1.1 mg/dL
IgA 250 mg/dL
Anti-tissue transglutaminase, IgA negative
Stool culture and studies for ova and parasites are negative. Test of the stool for occult blood is negative. Fecal fat content is 22 g/day (N < 7). Fecal lactoferrin is negative and elastase is within normal limits. Which of the following is the most appropriate next step in diagnosis?
- A. CT scan of the abdomen
- B. IgG against deamidated gliadin peptide
- C. Schilling test
- D. Enteroscopy
- E. PAS-stained biopsy of small bowel (Correct Answer)
Malabsorption syndromes Explanation: ***PAS-stained biopsy of small bowel***
- The patient's history of travel to Bangladesh, chronic diarrhea, malabsorption (weight loss, fatigue, elevated fecal fat, macrocytic anemia), and negative celiac serology (anti-tissue transglutaminase IgA) are highly suggestive of **Whipple's disease**.
- **Periodic Acid-Schiff (PAS) staining** of a small bowel biopsy is the gold standard for diagnosing Whipple's disease, revealing **PAS-positive macrophages** containing *Tropheryma whipplei*.
*CT scan of the abdomen*
- While a CT scan can identify structural abnormalities or masses, it is not the most direct diagnostic test for **malabsorptive conditions** like Whipple's disease.
- It would likely show non-specific findings such as **bowel wall thickening** or **lymphadenopathy**, but not the definitive histological changes.
*IgG against deamidated gliadin peptide*
- This test is used to diagnose **celiac disease**, but the patient's IgA anti-tissue transglutaminase was already negative, and this IgG test is typically performed when IgA deficiency is suspected or in young children.
- Given the strong suspicion of an infectious etiology due to travel history and systemic symptoms, focusing solely on celiac serology is less appropriate as the first next step.
*Schilling test*
- The Schilling test is an **obsolete test** that was historically used to assess **vitamin B12 absorption** and differentiate causes of B12 deficiency (pernicious anemia, bacterial overgrowth, or pancreatic insufficiency).
- This test is **no longer performed in clinical practice** due to unavailability of radioactive B12; modern evaluation uses serum B12, methylmalonic acid, and homocysteine levels.
- While the patient has macrocytic anemia, the test would not directly address the underlying cause of fat malabsorption and systemic symptoms present.
*Enteroscopy*
- Enteroscopy allows for visualization and biopsy of the small bowel beyond the reach of a standard upper endoscopy.
- While useful for obtaining biopsies, simply performing an enteroscopy without knowing what to look for or what specific stain to request (referring to PAS) on the biopsy would be less targeted than ordering a **PAS-stained biopsy** specifically.
Malabsorption syndromes US Medical PG Question 9: A 42-year-old woman presents with exertional dyspnea and fatigue for the past 3 months. Her past medical history is significant for multiple episodes of mild diarrhea for many years, which was earlier diagnosed as irritable bowel syndrome (IBS). She denies any current significant gastrointestinal symptoms. The patient is afebrile and vital signs are within normal limits. Physical examination reveals oral aphthous ulcers and mild conjunctival pallor. Abdominal examination is unremarkable. There is a rash present on the peripheral extremities bilaterally (see image). Laboratory findings are significant for evidence of microcytic hypochromic anemia. FOBT is negative. Which of the following is the most likely diagnosis in this patient?
- A. Small intestinal bacterial overgrowth
- B. Whipple's disease
- C. Non-tropical sprue (Correct Answer)
- D. Inflammatory bowel disease
- E. Tropical sprue
Malabsorption syndromes Explanation: ***Non-tropical sprue***
- The patient's presentation with **exertional dyspnea, fatigue, oral aphthous ulcers, microcytic hypochromic anemia** (indicating **iron deficiency from malabsorption**), and a rash consistent with **dermatitis herpetiformis** (as indicated by the peripheral rash on extremities) despite no current significant GI symptoms, strongly points to **celiac disease (non-tropical sprue)**.
- Celiac disease can manifest with **extra-intestinal symptoms** like iron deficiency anemia, skin rashes, and oral ulcers due to malabsorption, even in the absence of severe gastrointestinal complaints, and its diagnosis can be often delayed due to misdiagnosis of IBS.
- **Iron deficiency anemia** is the most common hematologic manifestation of celiac disease due to impaired absorption in the proximal small intestine.
*Small intestinal bacterial overgrowth*
- While SIBO can cause malabsorption and diarrhea, it **does not typically present with oral aphthous ulcers or a rash consistent with dermatitis herpetiformis**.
- **Anemia** can occur due to long-standing SIBO, but the overall constellation of findings is more suggestive of another diagnosis.
*Whipple's disease*
- Whipple's disease is a rare systemic infection that can cause **malabsorption, arthralgias, ocular symptoms**, and **neurological abnormalities**.
- However, **oral aphthous ulcers and dermatitis herpetiformis are not characteristic features** of Whipple's disease, and the skin lesions in Whipple's are usually hyperpigmentation.
*Inflammatory bowel disease*
- While Crohn's disease (a type of IBD) can be associated with **oral aphthous ulcers** and **anemia**, the rash on the extremities is not typical for IBD except for **erythema nodosum or pyoderma gangrenosum** which do not match the expected dermatitis herpetiformis pattern.
- The patient's long history of episodic diarrhea diagnosed as IBS, but with evolving extra-intestinal symptoms, makes celiac disease a more fitting diagnosis.
*Tropical sprue*
- **Tropical sprue** is a malabsorption syndrome occurring in residents or visitors to tropical regions, typically presenting with **chronic diarrhea, steatorrhea, and weight loss**.
- It is **not commonly associated with oral aphthous ulcers or specific dermatological manifestations like dermatitis herpetiformis**, and the patient's history does not indicate recent travel to tropical areas.
Malabsorption syndromes US Medical PG Question 10: A previously healthy 20-year-old woman comes to the physician because of recurrent abdominal cramps, bloating, and diarrhea for 4 months. She describes her stools as greasy, foul-smelling, and difficult to flush. During this time she has had a 6-kg (13.2-lb) weight loss. She has no personal or family history of serious illness. Physical examination shows pallor and cheilitis. Laboratory studies show a hemoglobin concentration of 11 g/dL. Serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Test of the stool for occult blood is negative and stool microscopy reveals no pathogens and no leukocytes. Analysis of a 24-hour stool sample shows 12 g of fat. The patient is asked to consume 25 g of d-xylose. Five hours later, its concentration is measured in urine at 2 g (N = > 4 g/5 h). The test is repeated after a two-week course of rifaximin, but the urinary concentration of d-xylose remains the same. Which of the following is the most likely diagnosis?
- A. Exocrine pancreatic insufficiency
- B. Bacterial overgrowth in the small intestine
- C. Tropheryma whipplei infection
- D. Hypersensitivity to gliadin (Correct Answer)
- E. Lactose intolerance
Malabsorption syndromes Explanation: ***Hypersensitivity to gliadin***
* The patient's symptoms (greasy, foul-smelling stools, weight loss, abdominal cramps, bloating, diarrhea, pallor, cheilitis, iron-deficiency anemia) are highly suggestive of **malabsorption**.
* The **impaired d-xylose absorption** that does not improve after antibiotics points to an intrinsic small bowel mucosal defect rather than bacterial overgrowth, making celiac disease (hypersensitivity to gliadin) the most likely diagnosis.
*Exocrine pancreatic insufficiency*
* While it causes **steatorrhea** and malabsorption, it typically presents with normal d-xylose absorption because **d-xylose is a monosaccharide that is absorbed directly by the intestinal mucosa without requiring pancreatic enzymes**.
* The normal function of the small intestinal mucosa would allow for adequate d-xylose absorption.
*Bacterial overgrowth in the small intestine*
* Symptoms can mimic malabsorption, and d-xylose absorption may be impaired due to bacterial consumption.
* However, the patient's d-xylose test did not improve after a course of **rifaximin**, which is an antibiotic effective against bacterial overgrowth.
*Tropheryma whipplei infection*
* Whipple's disease can cause malabsorption, **steatorrhea**, and abdominal symptoms similar to those described.
* However, it also commonly presents with **arthralgia, lymphadenopathy, and neurological symptoms**, which are absent in this patient.
*Lactose intolerance*
* This condition primarily causes bloating, cramps, and diarrhea, but typically does not lead to **significant weight loss** or **steatorrhea (greasy stools)**.
* D-xylose absorption would also be expected to be normal because it is a **monosaccharide** that is absorbed directly, unlike lactose which requires lactase.
More Malabsorption syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.