Helicobacter pylori infection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Helicobacter pylori infection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Helicobacter pylori infection US Medical PG Question 1: A 45-year-old woman has a history of mild epigastric pain, which seems to have gotten worse over the last month. Her pain is most severe several hours after a meal and is somewhat relieved with over-the-counter antacids. The patient denies abnormal tastes in her mouth or radiating pain. She does not take any other over-the-counter medications. She denies bleeding, anemia, or unexplained weight loss, and denies a family history of gastrointestinal malignancy. Which of the following is the best next step in the management of this patient?
- A. Barium swallow
- B. Urease breath test (Correct Answer)
- C. Esophageal pH monitoring
- D. Empiric proton pump inhibitor therapy
- E. Upper endoscopy with biopsy of gastric mucosa
Helicobacter pylori infection Explanation: ***Urease breath test***
- The patient's symptoms of **epigastric pain** that is worse several hours after a meal and relieved by antacids are highly suggestive of a **peptic ulcer**.
- Given her age (45) and the absence of alarm symptoms (bleeding, weight loss, dysphagia), testing for **_H. pylori_ infection** with a non-invasive method like the **urease breath test** [1] is the most appropriate initial step.
- Identifying and eradicating _H. pylori_ is the cornerstone of therapy for peptic ulcers to relieve symptoms and prevent recurrence [1].
*Barium swallow*
- A **barium swallow** is primarily used to evaluate **structural abnormalities** of the esophagus, stomach, and duodenum.
- It is less effective for diagnosing **mucosal pathology** like peptic ulcers or _H. pylori_ infection compared to endoscopy or breath tests.
*Esophageal pH monitoring*
- **Esophageal pH monitoring** is the gold standard for diagnosing **gastroesophageal reflux disease (GERD)**.
- The patient's symptoms are more consistent with peptic ulcer disease, especially the pain pattern and relief with antacids, rather than typical GERD symptoms like heartburn or regurgitation.
*Empiric proton pump inhibitor therapy*
- While empiric PPI therapy can be considered for **GERD** or **dyspepsia**, it's generally not the first line when **_H. pylori_** is a strong possibility, especially in a patient with symptoms suggestive of a peptic ulcer.
- Identifying and eradicating _H. pylori_ is crucial for ulcer healing and preventing recurrence, and this would be missed with just empiric PPI therapy [1].
*Upper endoscopy with biopsy of gastric mucosa*
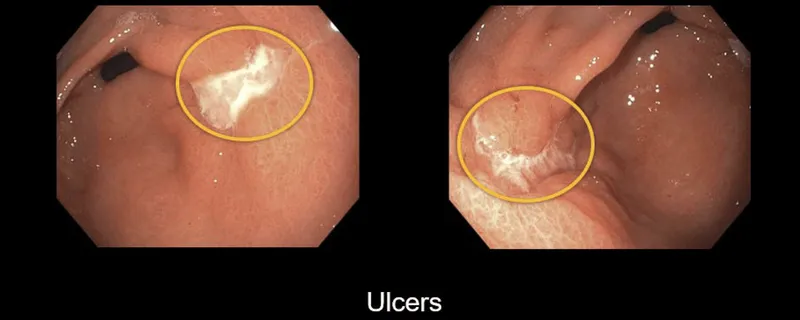
- **Upper endoscopy** is indicated when **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, anemia) [2] are present, or in older patients (>60 years) with new-onset dyspepsia.
- For a 45-year-old with non-alarming symptoms, a **non-invasive _H. pylori_ test** is preferred initially before proceeding to endoscopy.
Helicobacter pylori infection US Medical PG Question 2: A 45-year-old man comes to the emergency department because of a 1-day history of black, tarry stools. He has also had upper abdominal pain that occurs immediately after eating and a 4.4-kg (9.7-lb) weight loss in the past 6 months. He has no history of major medical illness but drinks 3 beers daily. His only medication is acetaminophen. He is a financial consultant and travels often for work. Physical examination shows pallor and mild epigastric pain. Esophagogastroduodenoscopy shows a bleeding 15-mm ulcer in the antrum of the stomach. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Alcohol consumption
- B. Age above 40 years
- C. Helicobacter pylori infection (Correct Answer)
- D. Acetaminophen use
- E. Work-related stress
Helicobacter pylori infection Explanation: ***Helicobacter pylori infection***
- The patient presents with classic symptoms of a **peptic ulcer disease** including **melena**, **epigastric pain** immediately after eating, and **weight loss**. While not explicitly mentioned, **H. pylori infection** is the most common cause of gastric and duodenal ulcers, especially in the absence of NSAID use.
- The chronic nature of the symptoms and the location of the ulcer in the **antrum** further support H. pylori as the primary predisposing factor, as it leads to mucosal inflammation and damage.
*Alcohol consumption*
- While **chronic alcohol consumption** can irritate the gastric mucosa and contribute to gastritis, it is generally considered a minor risk factor for peptic ulcer disease compared to H. pylori or NSAID use.
- The patient's 3 beers daily is likely not sufficient to directly cause a bleeding gastric ulcer of this magnitude.
*Age above 40 years*
- **Age** itself is not a direct predisposing factor for peptic ulcers, although the incidence of ulcers tends to increase with age.
- This is more likely due to the cumulative exposure to risk factors like H. pylori and NSAIDs over time, rather than age being an independent cause for ulcer formation.
*Acetaminophen use*
- **Acetaminophen (paracetamol)** is generally considered safe for the gastric mucosa and does not cause ulcers in therapeutic doses, unlike NSAIDs.
- It works through a different mechanism of action and does not inhibit cyclooxygenase-1 (COX-1) in the gastric lining, which is responsible for ulcer formation with NSAIDs.
*Work-related stress*
- While **stress** can exacerbate symptoms of gastrointestinal conditions, it has not been scientifically proven to be a direct cause of peptic ulcer formation.
- The role of psychological stress in ulcer genesis is considered minimal compared to established factors like H. pylori and NSAIDs.
Helicobacter pylori infection US Medical PG Question 3: A 49-year-old man being treated for Helicobacter pylori infection presents to his primary care physician complaining of lower back pain. His physician determines that a non-steroidal anti-inflammatory drug (NSAID) would be the most appropriate initial treatment. Which of the following is the most appropriate NSAID for this patient?
- A. Aspirin
- B. Ibuprofen
- C. Celecoxib (Correct Answer)
- D. Naproxen
- E. Diclofenac
Helicobacter pylori infection Explanation: **Celecoxib**
- This patient is being treated for a *Helicobacter pylori* infection, indicating a potential risk for **gastrointestinal complications** like ulcers. **Celecoxib** is a selective **COX-2 inhibitor**, which has a lower risk of causing GI side effects compared to non-selective NSAIDs.
- Its selective inhibition of COX-2 helps reduce pain and inflammation while largely sparing the **COX-1 enzyme**, which is responsible for maintaining the **gastric mucosal lining**.
*Aspirin*
- **Aspirin** is a non-selective NSAID that inhibits both **COX-1** and **COX-2** enzymes.
- Inhibition of COX-1 can lead to a significant increase in the risk of **gastrointestinal bleeding** and **ulcer formation**, which is particularly concerning for a patient with an *H. pylori* infection.
*Ibuprofen*
- **Ibuprofen** is a non-selective NSAID that can cause **gastrointestinal irritation** and damage by inhibiting **COX-1**.
- Its use would increase the risk of worsening the patient's existing **gastrointestinal vulnerability** due to the *H. pylori* infection.
*Naproxen*
- **Naproxen** is another non-selective NSAID with a relatively long half-life, making its **gastrointestinal side effects** potentially more prolonged and severe than some other non-selective NSAIDs.
- It carries a **higher risk for GI bleeding** and ulcers compared to selective COX-2 inhibitors, especially in patients with pre-existing GI issues.
*Diclofenac*
- **Diclofenac** is a non-selective NSAID that carries a risk of **gastrointestinal adverse events**, although some studies suggest it might have a slightly better GI safety profile than other non-selective NSAIDs at lower doses.
- However, in a patient with *H. pylori*, it still poses a significant risk for **ulcers** and bleeding compared to a COX-2 selective inhibitor.
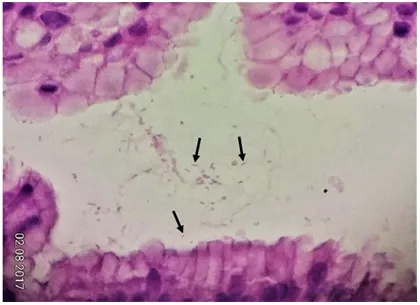
Helicobacter pylori infection US Medical PG Question 4: A 49-year-old male complains of abdominal discomfort that worsens following meals. A gastric biopsy reveals a 2 cm gastric ulcer, and immunohistochemical staining demonstrates the presence of a rod-shaped bacterium in the gastric mucosa. Which of the following is used by the infiltrating pathogen to neutralize gastric acidity?
- A. Mucinase
- B. LT toxin
- C. Flagella
- D. Bismuth
- E. Urease (Correct Answer)
Helicobacter pylori infection Explanation: ***Urease***
- The presence of a rod-shaped bacterium in the gastric mucosa causing ulcers points to **Helicobacter pylori**.
- **H. pylori** produces **urease**, an enzyme that converts urea into ammonia and carbon dioxide, creating a more alkaline environment around the bacterium, thus neutralizing gastric acid and allowing its survival.
*Mucinase*
- **Mucinase** is an enzyme produced by some bacteria that breaks down the protective mucus layer, contributing to mucosal damage.
- While contributing to pathogenesis, mucinase does not directly neutralize gastric acidity.
*LT toxin*
- **LT toxin** (heat-labile toxin) is primarily associated with **enterotoxigenic Escherichia coli (ETEC)** and causes watery diarrhea by increasing cAMP.
- This toxin is not produced by **H. pylori** and does not play a role in neutralizing gastric acid.
*Flagella*
- **Flagella** are **locomotor appendages** that allow **H. pylori** to move through the gastric mucus layer and colonize the gastric epithelium.
- While crucial for host colonization, flagella do not directly neutralize gastric acid.
*Bismuth*
- **Bismuth** is a component of some multi-drug regimens used to treat **H. pylori** infection, acting as an antimicrobial and mucosal protectant.
- It is not produced by the bacterium but is a medication given to the patient.
Helicobacter pylori infection US Medical PG Question 5: A 52-year-old man comes to the physician because of a 3-month history of upper abdominal pain and nausea that occurs about 3 hours after eating and at night. These symptoms improve with eating. After eating, he often has a feeling of fullness and bloating. He has had several episodes of dark stools over the past month. He has smoked one pack of cigarettes daily for 40 years and drinks 2 alcoholic beverages daily. He takes no medications. His temperature is 36.4°C (97.5°F), pulse is 80/min, and blood pressure is 110/70 mm Hg. Abdominal examination shows epigastric tenderness with no guarding or rebound. Bowel sounds are normal. Which of the following treatments is most appropriate to prevent further complications of the disease in this patient?
- A. Intravenous vitamin B12 supplementation
- B. Truncal vagotomy
- C. Amoxicillin, clarithromycin, and omeprazole (Correct Answer)
- D. Fundoplication, hiatoplasty, and gastropexy
- E. Distal gastrectomy with gastroduodenostomy
Helicobacter pylori infection Explanation: ***Amoxicillin, clarithromycin, and omeprazole***
- This patient's symptoms (epigastric pain 3 hours after eating and at night, improvement with eating, dark stools) are highly suggestive of a **duodenal ulcer complicated by upper gastrointestinal bleeding**. The most common cause of duodenal ulcers is *H. pylori* infection.
- The recommended first-line treatment for *H. pylori* infection involves a triple therapy regimen, including two antibiotics (like **amoxicillin and clarithromycin**) to eradicate the bacteria and a **proton pump inhibitor (omeprazole)** to reduce acid production and promote ulcer healing.
*Intravenous vitamin B12 supplementation*
- This treatment is appropriate for **vitamin B12 deficiency**, which can occur in conditions like atrophic gastritis, pernicious anemia, or following gastric resections, but is not indicated for acute peptic ulcer disease and wouldn't address the primary pathology.
- There is no clinical indication in the patient's presentation (e.g., neurological symptoms, macrocytic anemia) to suggest a deficiency in vitamin B12.
*Truncal vagotomy*
- **Truncal vagotomy** is a surgical procedure that was historically performed to reduce gastric acid secretion by cutting the vagus nerve. It is rarely used now due to the effectiveness of medical therapies for peptic ulcer disease.
- This invasive surgical option is generally reserved for refractory cases of peptic ulcer disease not responsive to medical management, or when complications like uncontrolled bleeding or perforation necessitate surgical intervention.
*Fundoplication, hiatoplasty, and gastropexy*
- These surgical procedures are primarily used to treat **gastroesophageal reflux disease (GERD)** and **hiatal hernia**, not peptic ulcer disease.
- Fundoplication wraps the stomach fundus around the lower esophagus to reinforce the lower esophageal sphincter, addressing reflux symptoms which are not the primary complaint here.
*Distal gastrectomy with gastroduodenostomy*
- **Distal gastrectomy** is a major surgical procedure involving the removal of the distal part of the stomach. It is typically reserved for severe complications of peptic ulcer disease (e.g., perforation, obstruction, recurrent bleeding unresponsive to other treatments) or gastric cancer.
- While it might be considered in extreme cases of complicated peptic ulcer, it is not the initial or most appropriate treatment for preventing further complications in a patient who has yet to receive standard anti-*H. pylori* therapy.
Helicobacter pylori infection US Medical PG Question 6: A 48-year-old woman with a history of osteoarthritis and hypertension presents to the office complaining of persistent abdominal pain for the last 2 months. She describes the pain as 'burning and achy' that is worse when she eats, which has lead to a weight loss of 4.5 kg (10.0 lb). The patient is currently taking lisinopril and atenolol for her blood pressure and ibuprofen as needed for her osteoarthritis. Her temperature is 37.1°C (98.7°F), heart rate is 75/min, and blood pressure is 120/80 mm Hg. An endoscopy is performed and a gastric ulcer is visualized and biopsied. The biopsy reveals H. pylori infection. Which of the following is the most likely predisposing factor to this patient’s diagnosis?
- A. Chronic NSAID use (Correct Answer)
- B. Longstanding GERD
- C. Age and gender
- D. Adverse effect of beta-blockers
- E. A congenital diverticulum
Helicobacter pylori infection Explanation: ***Chronic NSAID use***
- The patient's use of **ibuprofen** for osteoarthritis is a significant risk factor for peptic ulcer disease, especially when combined with *H. pylori* infection. NSAIDs inhibit **prostaglandin synthesis**, impairing the stomach's protective mucous layer.
- The abdominal pain worsening with food and subsequent weight loss are classic symptoms of a **gastric ulcer**, which is confirmed by endoscopy and *H. pylori* biopsy.
*Longstanding GERD*
- While GERD can cause upper abdominal pain, it typically manifests as **heartburn** or **regurgitation**, not usually "burning and achy" pain made worse by eating in a way that leads to significant weight loss due to a gastric ulcer.
- GERD primarily causes esophageal damage, whereas a gastric ulcer involves the stomach lining; although there can be overlap, it's not the primary predisposing factor for a biopsy-confirmed *H. pylori* gastric ulcer.
*Age and gender*
- While peptic ulcer disease can occur at any age, the patient's age and gender are not direct predisposing factors for a **gastric ulcer** in the same way that NSAID use or *H. pylori* infection are.
- These factors do not explain the specific mechanism of ulcer formation in her case as directly as her medication history.
*Adverse effect of beta-blockers*
- **Beta-blockers** (like atenolol) are not known to cause peptic ulcers as a common or significant adverse effect.
- Their primary cardiovascular effects do not directly impact gastric mucosal integrity.
*A congenital diverticulum*
- A congenital diverticulum, such as a **Meckel's diverticulum**, is typically found in the small intestine and is more associated with complications like inflammation, bleeding, or obstruction, not gastric ulcers.
- This condition is also present from birth and not related to the patient's current medications or *H. pylori* infection.
Helicobacter pylori infection US Medical PG Question 7: A 52-year-old woman presents with mild epigastric pain and persistent heartburn for the past 2 months. An endoscopy is performed and reveals inflammation of the stomach mucosa without evidence of ulceration. A biopsy is performed and reveals intestinal metaplasia with destruction of a large number of parietal cells. She is diagnosed with chronic atrophic gastritis. Which of the following is characteristic of this patient’s diagnosis?
- A. Serum gastrin levels are decreased.
- B. Caused by a gram-negative rod that is urease positive
- C. It is the most common cause of folate deficiency in the US.
- D. Destruction of the mucosa of the stomach is mediated by T cells. (Correct Answer)
- E. MALT lymphoma is a common complication.
Helicobacter pylori infection Explanation: ***Destruction of the mucosa of the stomach is mediated by T cells.***
- The type of chronic atrophic gastritis described, characterized by **parietal cell destruction** and **intestinal metaplasia**, is consistent with **autoimmune gastritis** (Type A gastritis).
- Autoimmune gastritis is mediated by **T cells** attacking gastric parietal cells, leading to their destruction and subsequent **achlorhydria** and loss of intrinsic factor.
*Serum gastrin levels are decreased.*
- Destruction of **parietal cells** leads to **achlorhydria** (lack of gastric acid), which removes the negative feedback on **G cells**.
- This results in **compensatory hypergastrinemia**, meaning serum gastrin levels are typically *elevated*, not decreased.
*Caused by a gram-negative rod that is urease positive*
- This describes **Helicobacter pylori infection**, which is the cause of **Type B gastritis** (environmental chronic atrophic gastritis) and typically affects the antrum.
- The patient's presentation with **destruction of parietal cells** and **intestinal metaplasia** is more consistent with **autoimmune (Type A) gastritis**, which is not caused by H. pylori.
*It is the most common cause of folate deficiency in the US.*
- **Folate deficiency** is more commonly associated with **poor dietary intake**, **alcoholism**, malabsorption disorders (e.g., celiac disease), and certain medications.
- While chronic atrophic gastritis can lead to **vitamin B12 deficiency** due to loss of intrinsic factor, it is not the most common cause of folate deficiency.
*MALT lymphoma is a common complication.*
- **MALT (mucosa-associated lymphoid tissue) lymphoma** is a known complication of chronic **H. pylori infection**, especially when it leads to gastritis and lymphoid follicle formation.
- While chronic inflammation is a risk factor for malignancy, MALT lymphoma is less commonly associated with **autoimmune gastritis** compared to H. pylori-induced gastritis.
Helicobacter pylori infection US Medical PG Question 8: A 67-year-old male presents to his primary care physician for evaluation of fever and an unintended weight loss of 25 pounds over the last 4 months. He also has decreased appetite and complains of abdominal pain located in the right upper quadrant. The patient has not noticed any changes in stool or urine. He emigrated from Malaysia to the United States one year prior. Social history reveals that he smokes half a pack per day and has 5-7 drinks of alcohol per day. The patient is up to date on all of his vaccinations. Physical exam findings include mild jaundice as well as an enlarged liver edge that is tender to palpation. Based on clinical suspicion, biomarker labs are sent and show polycythemia and an elevated alpha fetoprotein level but a normal CA 19-9 level. Surface antigen for hepatitis B is negative. Ultrasound reveals a normal sized gallbladder. Given this presentation, which of the following organisms was most likely associated with the development of disease in this patient?
- A. Naked DNA virus
- B. Enveloped DNA virus
- C. Curved gram-negative bacteria
- D. Acute angle branching fungus
- E. Trematode from undercooked fish (Correct Answer)
Helicobacter pylori infection Explanation: ***Trematode from undercooked fish***
- The patient's symptoms (fever, RUQ pain, weight loss, jaundice, hepatomegaly, elevated **AFP**, and normal CA 19-9) point strongly towards **hepatocellular carcinoma (HCC)**.
- The history of emigration from Malaysia and the elevated **alpha-fetoprotein (AFP)** despite negative hepatitis B antigen, suggest a parasitic infection, specifically a liver fluke (trematode), as a risk factor for HCC. **Clonorchis sinensis** and **Opisthorchis viverrini** are trematodes acquired from undercooked freshwater fish, endemic to Southeast Asia, and are known to cause cholangiocarcinoma and, less commonly, HCC.
*Naked DNA virus*
- This typically refers to viruses like **human papillomavirus (HPV)** or **adenovirus**, which are not primary causes of the described liver pathology or HCC with this specific presentation.
- While some naked DNA viruses can cause human disease, they are not typically linked to the patient's specific symptoms and lab findings (elevated AFP) in the context of liver cancer from a Southeast Asian background.
*Enveloped DNA virus*
- This category includes viruses like **Herpesviruses** and **Hepatitis B virus (HBV)**. While HBV is a major cause of HCC, the patient's hepatitis B surface antigen is negative, ruling out active or chronic HBV infection as the direct cause in this case.
- Other enveloped DNA viruses do not commonly cause this specific cluster of symptoms and risk factors for HCC.
*Curved gram-negative bacteria*
- This description often refers to bacteria like **Campylobacter** or **Helicobacter pylori**. These can cause gastrointestinal issues but are not typically associated with liver masses, jaundice, and elevated AFP in the context of HCC.
- They do not explain the patient's risk factors or presentation that strongly suggests chronic liver inflammation leading to cancer.
*Acute angle branching fungus*
- This refers to fungi like **Aspergillus**, which can cause invasive infections, particularly in immunocompromised individuals.
- While Aspergillus can cause pulmonary infections and, less commonly, disseminate to other organs including the liver, it does not typically present with the described risk factors (Southeast Asian origin, undercooked fish consumption) or lab findings (elevated AFP) for HCC, nor does it fit the general clinical picture.
Helicobacter pylori infection US Medical PG Question 9: A 23-year-old man comes to the physician for frequent and painful urination. He has also had progressive painful swelling of his right knee over the past week. He is sexually active with two female partners and uses condoms inconsistently. His mother has an autoimmune disease that involves a malar rash. Examination shows conjunctivitis bilaterally. The right knee is warm, erythematous, and tender to touch; range of motion is limited. Laboratory studies show an erythrocyte sedimentation rate of 62 mm/h. Urinalysis shows WBCs. Further evaluation of this patient is most likely to reveal which of the following?
- A. Hiking trip two months ago
- B. Recent norovirus gastroenteritis
- C. Chondrocalcinosis of the left knee
- D. Positive anti-dsDNA antibodies
- E. HLA-B27 positive genotype (Correct Answer)
Helicobacter pylori infection Explanation: ***HLA-B27 positive genotype***
- The patient's symptoms (urethritis, conjunctivitis, and arthritis) constitute the classic triad of **Reiter's syndrome**, a form of **reactive arthritis**.
- **Reactive arthritis** is strongly associated with the **HLA-B27 genotype**, which is found in a significant majority of affected individuals.
*Hiking trip two months ago*
- This information is vague and does not directly link to a specific pathogen or trigger for reactive arthritis.
- While some bacterial infections can be acquired through environmental exposure, there is no direct evidence provided in the stem to support a connection.
*Recent norovirus gastroenteritis*
- **Norovirus** typically causes acute, self-limiting gastroenteritis and is not commonly associated with the development of **reactive arthritis**.
- Reactive arthritis is primarily triggered by certain **genitourinary** or **gastrointestinal bacterial infections** (e.g., Chlamydia, Shigella, Salmonella, Campylobacter).
*Chondrocalcinosis of the left knee*
- **Chondrocalcinosis** (calcium pyrophosphate deposition disease or pseudogout) primarily affects older individuals and typically presents with acute, severe arthritis.
- While it can affect the knee, it is not consistently associated with the extra-articular manifestations (urethritis, conjunctivitis) seen in this patient, and its etiology is distinct from reactive arthritis.
*Positive anti-dsDNA antibodies*
- **Positive anti-dsDNA antibodies** are a hallmark of **systemic lupus erythematosus (SLE)**, an autoimmune disease.
- While SLE can cause arthritis and sometimes conjunctivitis, it does not typically cause urethritis in the manner described, nor does it fit the overall clinical picture as well as reactive arthritis.
Helicobacter pylori infection US Medical PG Question 10: A 65-year-old man is brought to the emergency department after coughing up copious amounts of blood-tinged sputum at his nursing home. He recently had an upper respiratory tract infection that was treated with antibiotics. He has a long-standing history of productive cough that has worsened since he had a stroke 3 years ago. He smoked a pack of cigarettes daily for 40 years until the stroke, after which he quit. The patient appears distressed and short of breath. His temperature is 38°C (100.4°F), pulse is 92/min, and blood pressure is 145/85 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Physical examination shows digital clubbing and cyanosis of the lips. Coarse crackles are heard in the thorax. An x-ray of the chest shows increased translucency and tram-track opacities in the right lower lung field. Which of the following is the most likely diagnosis?
- A. Aspiration pneumonia
- B. Pulmonary embolism
- C. Lung cancer
- D. Bronchiectasis (Correct Answer)
- E. Emphysema
Helicobacter pylori infection Explanation: ***Bronchiectasis***
- The patient's history of **chronic productive cough**, **hemoptysis** (blood-tinged sputum), **digital clubbing**, and recent respiratory infection suggests bronchiectasis. The chest X-ray finding of **tram-track opacities** is highly characteristic of this condition, indicating bronchial wall thickening and dilation. The history of stroke placing him at risk for aspiration, and prior smoking also contribute to the risk of chronic lung damage.
- **Bronchiectasis** is defined by **permanent dilation of the bronchi** due to chronic inflammation and infection, leading to impaired mucociliary clearance and recurrent infections. The description perfectly fits the clinical and radiological picture.
*Aspiration pneumonia*
- While the patient's history of **stroke** increases his risk for **aspiration**, the chronic nature of his symptoms (long-standing productive cough worsening since stroke) and the presence of **digital clubbing** are less consistent with acute aspiration pneumonia.
- **Aspiration pneumonia** typically presents as an acute illness with fever and cough, and while it could explain some symptoms, it doesn't fully account for the chronic changes (clubbing, tram-track opacities).
*Pulmonary embolism*
- **Pulmonary embolism** usually presents with **acute onset dyspnea** and **pleuritic chest pain**, often without a history of chronic productive cough or digital clubbing. Hemoptysis can occur but is not typically copious and is associated with infarction.
- The chest X-ray findings of **increased translucency** and **tram-track opacities** are not characteristic of pulmonary embolism, which might show an area of opacification (Westermark sign, Hampton hump) or be normal.
*Lung cancer*
- While **lung cancer** can cause cough, hemoptysis, and shortness of breath, and the patient's smoking history is a risk factor, the description of **tram-track opacities** on chest X-ray is not characteristic of lung cancer. **Digital clubbing** can be seen, but the chronic productive cough for years is more indicative of a chronic inflammatory process.
- The typical X-ray findings for lung cancer would be a **mass lesion**, nodule, or atelectasis, not diffuse bronchial wall thickening.
*Emphysema*
- **Emphysema** is characterized by **shortness of breath** and a **chronic cough**, often related to a smoking history, and the X-ray might show **increased translucency** due to hyperinflation. However, copious **blood-tinged sputum** and **digital clubbing** are not typical features of emphysema.
- The classic X-ray finding for emphysema is **hyperinflation** with flattened diaphragms, and while increased translucency is mentioned, **tram-track opacities** are not seen; these indicate bronchial wall thickening, not alveolar destruction.
More Helicobacter pylori infection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.