GI motility disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GI motility disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GI motility disorders US Medical PG Question 1: A 25-year-old man presents to his gastroenterologist for trouble swallowing. The patient states that whenever he eats solids, he regurgitates them back up. Given this patient's suspected diagnosis, the gastroenterologist performs a diagnostic test. Several hours later, the patient presents to the emergency department with chest pain and shortness of breath. His temperature is 99.5°F (37.5°C), blood pressure is 130/85 mmHg, pulse is 60/min, respirations are 12/min, and oxygen saturation is 99% on room air. On physical exam, the patient demonstrates a normal cardiopulmonary exam. His physical exam demonstrates no tenderness of the neck, a normal oropharynx, palpable crepitus above the clavicles, and minor lymphadenopathy. Which of the following is the best next step in management?
- A. Barium swallow
- B. Gastrografin swallow (Correct Answer)
- C. Urgent surgery
- D. Ultrasound
GI motility disorders Explanation: ***Gastrografin swallow***
- This patient likely has an **esophageal perforation** following a diagnostic procedure, possibly **endoscopy or manometry** for suspected achalasia given the dysphagia, regurgitation, and subsequent symptoms.
- A **Gastrografin swallow** is the best initial diagnostic step because it is water-soluble, allowing for detection of a leak without causing severe complications if aspirated into the lungs or mediastinum.
*Barium swallow*
- This is generally not recommended for suspected esophageal perforation as **barium** is a corrosive agent that can cause a severe inflammatory reaction known as **mediastinitis** if it leaks into the mediastinum.
- While it offers superior mucosal detail, the risks associated with extravasation outweigh its benefits in this emergent setting.
*Urgent surgery*
- While **surgical repair** is the definitive treatment for significant esophageal perforations, it should only be performed after definitive diagnosis and localization of the perforation.
- Performing surgery without imaging confirmation would be inappropriate and potentially lead to unnecessary intervention or missing the actual site of injury.
*Ultrasound*
- **Ultrasound** has limited utility in diagnosing esophageal perforation due to the location of the esophagus behind the trachea and sternum, making it largely inaccessible to acoustic waves.
- It also cannot effectively detect the leakage of contrast material from the esophageal lumen.
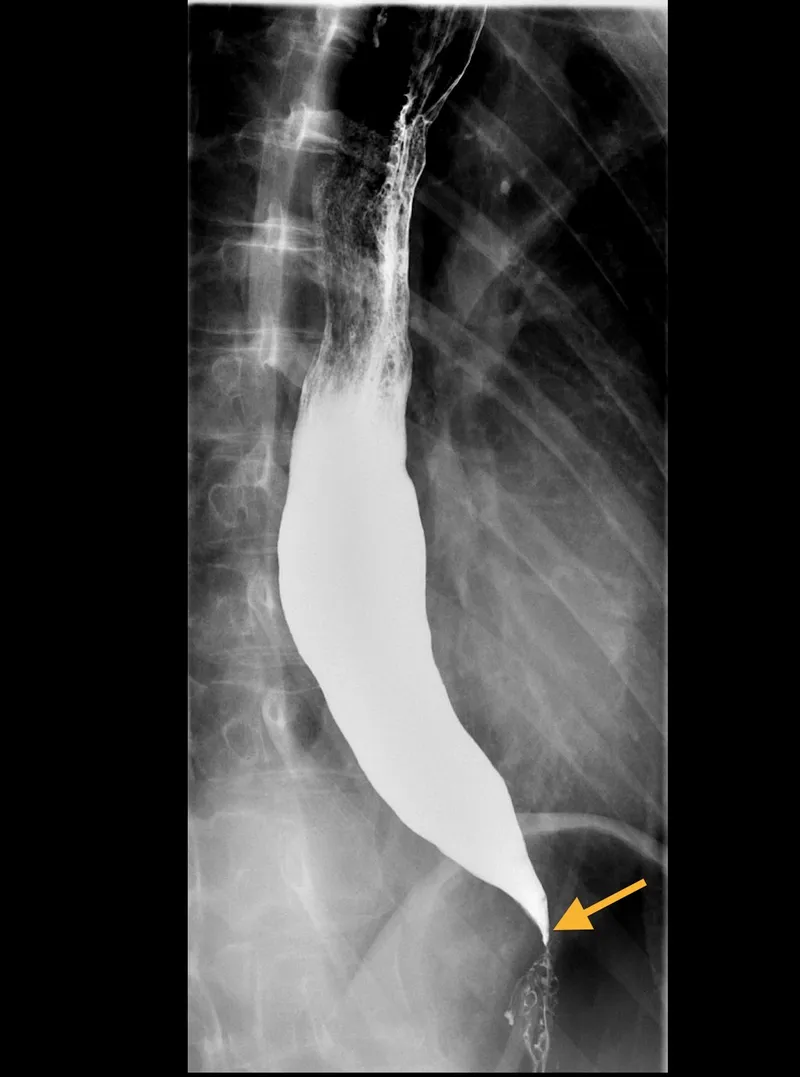
GI motility disorders US Medical PG Question 2: A 62-year-old man is referred to a gastroenterologist because of difficulty swallowing for the past 5 months. He has difficulty swallowing both solid and liquid foods, but there is no associated pain. He denies any shortness of breath or swelling in his legs. He immigrated from South America 10 years ago. He is a non-smoker and does not drink alcohol. His physical examination is unremarkable. A barium swallow study was ordered and the result is given below. Esophageal manometry confirms the diagnosis. What is the most likely underlying cause of this patient’s condition?
- A. Pharyngoesophageal diverticulum
- B. Chagas disease (Correct Answer)
- C. Esophageal rupture
- D. Gastroesophageal reflux disease
- E. Squamous cell carcinoma of the esophagus
GI motility disorders Explanation: ***Chagas disease***
- The patient's history of living in **South America** and presenting with **dysphagia for both solids and liquids** (suggesting a motility disorder), along with the **barium swallow image showing esophageal dilation and a 'bird's beak' appearance** at the gastroesophageal junction, are highly characteristic of achalasia caused by Chagas disease.
- Chagas disease, caused by *Trypanosoma cruzi*, leads to the destruction of **myenteric plexus neurons** in the esophagus, resulting in achalasia (failure of the lower esophageal sphincter to relax) and megaesophagus.
*Pharyngoesophageal diverticulum*
- This typically presents as **Zenker's diverticulum**, causing **difficulty initiating a swallow**, regurgitation of undigested food, and sometimes halitosis, which is different from the described dysphagia for both solids and liquids.
- A Zenker's diverticulum would appear as a **pouch-like protrusion** in the posterior pharynx, not the diffuse esophageal dilation seen in the image.
*Esophageal rupture*
- Esophageal rupture (Boerhaave syndrome) is an acute, life-threatening condition associated with **severe chest pain, vomiting, and crepitus**, not a chronic, progressive dysphagia without pain.
- Imaging would reveal **extravasation of contrast** into the mediastinum or pleural space, not the smooth dilation and distal narrowing observed.
*Gastroesophageal reflux disease*
- While chronic GERD can lead to **strictures** and dysphagia, it typically causes **heartburn**, regurgitation, and sometimes odynophagia, and the dysphagia is usually progressive for solids first.
- The barium swallow would show reflux or a stricture, not the **classic achalasia findings** of a dilated esophagus tapering to a narrow distal segment.
*Squamous cell carcinoma of the esophagus*
- Squamous cell carcinoma usually presents with **progressive dysphagia, initially for solids**, and is often associated with weight loss, smoking, and alcohol use, none of which are present in this patient.
- A tumor would typically appear as an **irregular, focal narrowing or mass** on barium swallow, not the smooth, diffuse dilation seen in this image.
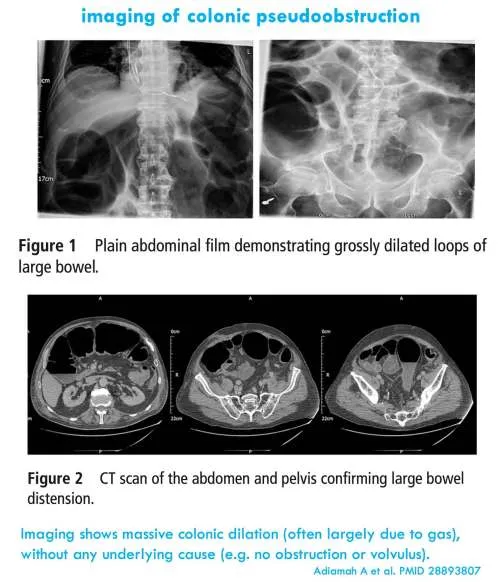
GI motility disorders US Medical PG Question 3: A 46-year-old woman comes to the emergency department because of intermittent abdominal pain and vomiting for 2 days. The abdominal pain is colicky and diffuse. The patient's last bowel movement was 3 days ago. She has had multiple episodes of upper abdominal pain that radiates to her scapulae and vomiting over the past 3 months; her symptoms subsided after taking ibuprofen. She has coronary artery disease, type 2 diabetes mellitus, gastroesophageal reflux disease, and osteoarthritis of both knees. Current medications include aspirin, atorvastatin, rabeprazole, insulin, and ibuprofen. She appears uncomfortable. Her temperature is 39°C (102.2°F), pulse is 111/min, and blood pressure is 108/68 mm Hg. Examination shows dry mucous membranes. The abdomen is distended and tympanitic with diffuse tenderness; bowel sounds are high-pitched. Rectal examination shows a collapsed rectum. Her hemoglobin concentration is 13.8 g/dL, leukocyte count is 14,400/mm3, and platelet count is 312,000/mm3. An x-ray of the abdomen is shown. Which of the following is the most likely cause of this patient's findings?
- A. Cecal torsion
- B. Viscus perforation
- C. Colonic diverticular inflammation
- D. Cholecystoenteric fistula (Correct Answer)
- E. Bowel infarction
GI motility disorders Explanation: ***Cholecystoenteric fistula***
- The patient's history of recurrent upper abdominal pain radiating to the scapula, responsive to NSAIDs, is highly suggestive of **biliary colic** due to **cholelithiasis**.
- The diffuse colicky pain, vomiting, distended abdomen with high-pitched bowel sounds, and particularly the **pneumobilia** (air in the biliary tree, visible as branching lucency in the hepatic area on X-ray, indicated by red arrows) along with signs of **small bowel obstruction** (dilated small bowel loops and air-fluid levels, indicated by green arrows), are classic features of **gallstone ileus** resulting from a cholecystoenteric fistula.
*Cecal torsion*
- While cecal torsion can cause a large bowel obstruction with colicky pain and distension, it typically presents with a **dilated cecum** and a characteristic "coffee-bean" appearance on X-ray, often without pneumobilia.
- The history of recurrent biliary pain and the presence of pneumobilia are not typical for cecal torsion.
*Viscus perforation*
- A viscus perforation would likely cause **sudden, severe onset abdominal pain**, signs of peritonitis, and usually **free air under the diaphragm** on an upright chest X-ray.
- While the patient has diffuse tenderness, the X-ray findings do not show free intraperitoneal air; instead, they show pneumobilia and small bowel obstruction.
*Colonic diverticuli inflammation*
- **Diverticulitis** typically presents with **left lower quadrant pain**, fever, and changes in bowel habits, though diffuse pain can occur with complications.
- It does not explain the history of recurrent upper abdominal pain radiating to the scapula or the radiologic findings of pneumobilia and small bowel obstruction.
*Bowel infarction*
- Bowel infarction often presents with **severe, disproportionate abdominal pain** (pain out of proportion to exam findings), bloody diarrhea, and signs of sepsis.
- While the patient has some signs of systemic inflammation (fever, leukocytosis), the X-ray findings of pneumobilia and typical small bowel obstruction, without signs of portal venous gas or extensive bowel wall thickening, make infarction less likely as the primary cause.
GI motility disorders US Medical PG Question 4: A 37-year-old man presents to the physician because of dysphagia and regurgitation for the past 5 years. In recent weeks, it has become very difficult for him to ingest solid or liquid food. He has lost 3 kg (6 lb) during this time. He was admitted to the hospital last year because of pneumonia. Three years ago, he had an endoscopic procedure which partially improved his dysphagia. He takes amlodipine and nitroglycerine before meals. His vital signs are within normal limits. BMI is 19 kg/m2. Physical examination shows no abnormalities. A barium swallow X-ray is shown. Which of the following patterns of esophageal involvement is the most likely cause of this patient’s condition?
- A. Abnormal esophageal contraction with normal lower esophageal sphincter relaxation
- B. Severely weak peristalsis and patulous lower esophageal sphincter
- C. Poor pharyngeal propulsion and upper esophageal sphincter obstruction
- D. Sequenced inhibition followed by contraction of the musculature along the esophagus
- E. Absent peristalsis and impaired lower esophageal sphincter relaxation (Correct Answer)
GI motility disorders Explanation: ***Absent peristalsis and impaired lower esophageal sphincter relaxation***
- The patient's symptoms of **dysphagia** for solids and liquids, along with weight loss, indicate a severe esophageal motility disorder.
- This condition is **achalasia**, where the esophagus fails to propel food down and the lower esophageal sphincter doesn't relax appropriately, leading to obstruction.
- The clinical clues include progressive dysphagia for both solids and liquids, regurgitation, weight loss, history of aspiration pneumonia, and prior endoscopic intervention (likely pneumatic dilation).
*Abnormal esophageal contraction with normal lower esophageal sphincter relaxation*
- This describes **distal esophageal spasm** or **jackhammer esophagus**, where the LES relaxes normally but esophageal body contractions are abnormal.
- This does not align with the patient's **lack of peristalsis and failure of LES relaxation**, which are pathognomonic for achalasia.
*Severely weak peristalsis and patulous lower esophageal sphincter*
- While weak peristalsis indicates poor movement, a **patulous (or incompetent) lower esophageal sphincter** suggests inability to maintain closure, leading to reflux.
- The patient has **dysphagia, not typical reflux symptoms** (heartburn, regurgitation of acidic content), which are associated with a patulous sphincter and ineffective esophageal motility.
*Poor pharyngeal propulsion and upper esophageal sphincter obstruction*
- This option describes **oropharyngeal dysphagia**, affecting the **upper esophageal sphincter**.
- The patient's symptoms and barium swallow findings point to a **lower esophageal disorder** (achalasia), not upper esophageal obstruction.
*Sequenced inhibition followed by contraction of the musculature along the esophagus*
- This describes **normal esophageal peristalsis**, with coordinated inhibition and contraction waves.
- This contradicts the patient's **absent peristalsis** seen in achalasia, where there is loss of the myenteric plexus and no coordinated esophageal contractions.
GI motility disorders US Medical PG Question 5: A 7-year-old boy is brought to the physician by his mother for the evaluation of abdominal pain and trouble sleeping for the past 6 months. His mother says he complains of crampy abdominal pain every morning on school days. He started attending a new school 7 months ago and she is concerned because he has missed school frequently due to the abdominal pain. He also has trouble falling asleep at night and asks to sleep in the same room with his parents every night. He has not had fever, vomiting, diarrhea, or weight loss. He sits very close to his mother and starts to cry when she steps out of the room to take a phone call. Abdominal examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Acute stress disorder
- B. Separation anxiety disorder (Correct Answer)
- C. Normal behavior
- D. Irritable bowel syndrome
- E. Conduct disorder
GI motility disorders Explanation: ***Separation anxiety disorder***
- This child exhibits classic symptoms of **separation anxiety disorder**, including **school refusal** due to physical complaints (abdominal pain), **difficulty sleeping alone**, and **excessive distress** when separated from a primary attachment figure (mother).
- The symptoms started shortly after attending a new school, a common trigger for separation anxiety, and have persisted for 6 months, meeting the **diagnostic criteria for duration** in children (≥4 weeks).
*Acute stress disorder*
- **Acute stress disorder** typically occurs within one month of exposure to a **traumatic event** and involves symptoms like intrusive thoughts, negative mood, dissociation, and hypervigilance.
- The boy's symptoms are **chronic (6 months)** and are related to separation, not a specific traumatic event, making this diagnosis less likely.
*Normal behavior*
- While some mild separation anxiety is normal in young children, the **severity**, **duration (6 months)**, and **functional impairment** (missing school, difficulty sleeping alone) in this 7-year-old go beyond what is considered typical developmental behavior.
- Normal separation anxiety usually resolves by preschool age or is short-lived without significant impact on daily life.
*Irritable bowel syndrome*
- **Irritable bowel syndrome (IBS)** is a common cause of recurrent abdominal pain, but it is typically associated with **changes in bowel habits** (constipation or diarrhea), which are absent in this case.
- Furthermore, the child's other symptoms, such as **school refusal**, **sleep disturbances**, and **distress upon separation**, are not characteristic of IBS and point towards a psychological rather than purely gastrointestinal etiology.
*Conduct disorder*
- **Conduct disorder** involves a persistent pattern of **aggressive behavior**, **destruction of property**, **deceitfulness or theft**, and **serious rule violations**, none of which are described in this case.
- The child's symptoms are characterized by anxiety and emotional distress related to separation, not defiant or antisocial behavior.
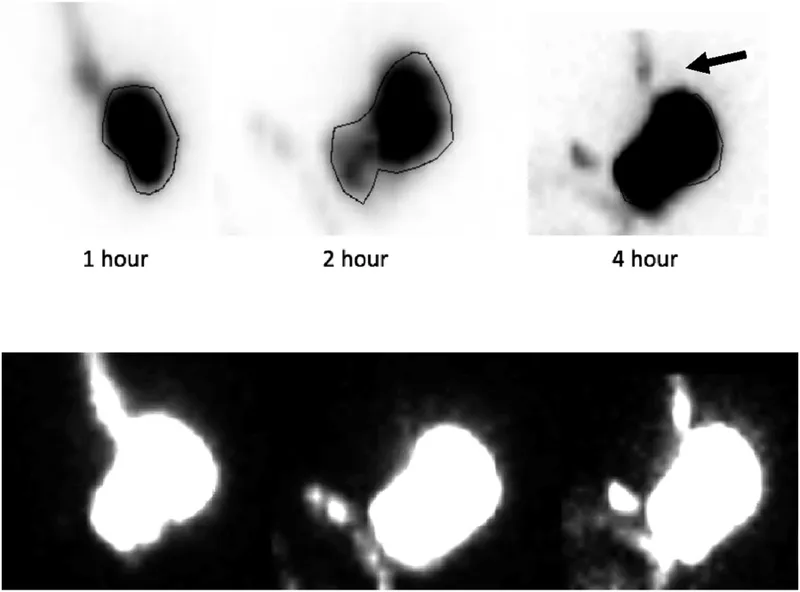
GI motility disorders US Medical PG Question 6: A 55-year-old woman with type 2 diabetes mellitus presents to her physician with intermittent nausea for the past 2 months. Her symptoms are exacerbated within one hour after eating. She has no other history of a serious illness. She takes metformin and injects insulin. Her vitals are normal. Abdominal examination is normal. An ECG shows normal sinus rhythm with no evidence of ischemia. Hemoglobin A1c is 7%. A gastric emptying scan shows 60% of her meal in the stomach 75 minutes after eating. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Dimenhydrinate
- B. Octreotide
- C. Lorazepam
- D. Metoclopramide (Correct Answer)
- E. Ondansetron
GI motility disorders Explanation: ***Metoclopramide***
- This patient presents with symptoms and gastric emptying scan results consistent with **diabetic gastroparesis**. Metoclopramide is a **prokinetic agent** that increases gastrointestinal motility and reduces nausea and vomiting.
- As a **dopamine D2 receptor antagonist**, it enhances cholinergic stimulation of the GI tract, promoting gastric emptying.
*Dimenhydrinate*
- This is an **antihistamine** primarily used for motion sickness. While it can help with nausea, it does not address the underlying **gastroparesis** and would not improve gastric emptying.
- It also has **sedative side effects** that often limit its use.
*Octreotide*
- **Octreotide** is a **somatostatin analog** used to treat conditions like VIPomas, acromegaly, and esophageal varices. It can actually *slow* gastric emptying.
- It is not indicated for the treatment of **gastroparesis** and would likely worsen symptoms.
*Lorazepam*
- **Lorazepam** is a **benzodiazepine** used for anxiety and sometimes as an antiemetic due to its anxiolytic and sedative properties, not due to direct effects on gastrointestinal motility.
- It does not address the underlying pathology of **gastroparesis** and its use would be inappropriate as a primary treatment.
*Ondansetron*
- **Ondansetron** is a **5-HT3 receptor antagonist** that effectively treats chemotherapy-induced nausea and vomiting.
- While it helps with nausea, it does not improve **gastric motility** or address the delayed gastric emptying seen in gastroparesis.
GI motility disorders US Medical PG Question 7: A 47-year-old man presents with recurrent epigastric pain and diarrhea. He has had these symptoms for the last year or so and has been to the clinic several times with similar complaints. His current dosage of omeprazole has been steadily increasing to combat his symptoms. The pain seems to be related to food intake. He describes his diarrhea as watery and unrelated to his meals. Blood pressure is 115/80 mm Hg, pulse is 76/min, and respiratory rate is 19/min. He denies tobacco or alcohol use. An upper endoscopy is performed due to his unexplained and recurrent dyspepsia and reveals thickened gastric folds with three ulcers in the first part of the duodenum, all of which are negative for H. pylori. Which of the following is the best next step in this patient's management?
- A. Fasting serum gastrin levels (Correct Answer)
- B. Secretin stimulation test
- C. CT scan of the abdomen
- D. Somatostatin receptor scintigraphy
- E. Serum calcium levels
GI motility disorders Explanation: ***Fasting serum gastrin levels***
- The patient's presentation with **recurrent epigastric pain**, **multiple duodenal ulcers**, **thickened gastric folds**, and the need for **increasing dosages of omeprazole** strongly suggests **Zollinger-Ellison syndrome (ZES)**, caused by a gastrinoma.
- **Fasting serum gastrin levels** are the initial diagnostic test for ZES; elevated levels confirm excessive gastrin production.
*Secretin stimulation test*
- This test is typically performed when **fasting serum gastrin levels are equivocal** (e.g., mildly elevated) to confirm the diagnosis of ZES.
- It is not the initial best step, as **fasting gastrin levels** are simpler and often sufficient for initial diagnosis.
*CT scan of the abdomen*
- A CT scan is used for **tumor localization** after a diagnosis of ZES has been established.
- It is not the primary diagnostic test for ZES itself, as it won't directly measure gastrin levels.
*Somatostatin receptor scintigraphy*
- This imaging study is highly sensitive for **localizing gastrinomas**, especially in metastatic disease, and is often used after biochemical confirmation of ZES.
- It is not indicated as the initial diagnostic step and is part of the work-up for staging rather than diagnosis.
*Serum calcium levels*
- While **hypercalcemia** can be associated with **Multiple Endocrine Neoplasia type 1 (MEN1)**, which includes gastrinomas, it is not the best initial diagnostic test for Zollinger-Ellison syndrome itself.
- Elevated calcium would be a secondary finding, and direct measurement of gastrin is essential for diagnosing ZES.
GI motility disorders US Medical PG Question 8: A 45-year-old woman comes to the physician because of progressive difficulty swallowing solids and liquids over the past 4 months. She has lost 4 kg (9 lb) during this period. There is no history of serious illness. She emigrated to the US from Panama 7 years ago. She does not smoke cigarettes or drink alcohol. Cardiopulmonary examination shows a systolic murmur and an S3 gallop. A barium radiograph of the chest is shown. Histopathologic examination of the esophageal wall is most likely to show which of the following?
- A. Presence of intranuclear basophilic inclusions
- B. Atrophy of esophageal smooth muscle cells
- C. Infiltration of eosinophils in the epithelium
- D. Presence of metaplastic columnar epithelium
- E. Absence of myenteric plexus neurons (Correct Answer)
GI motility disorders Explanation: ***Absence of myenteric plexus neurons***
- This finding is pathognomonic for **Chagas disease** (American trypanosomiasis), caused by *Trypanosoma cruzi*, endemic to Central and South America including Panama.
- The parasite destroys the **myenteric (Auerbach's) plexus neurons** in the esophageal wall, disrupting normal peristalsis and leading to **megaesophagus**.
- This results in **progressive dysphagia for both solids and liquids** and weight loss, as seen in this patient.
- The **cardiac findings** (systolic murmur and S3 gallop) indicate associated **chagasic cardiomyopathy**, another manifestation of chronic Chagas disease.
*Presence of intranuclear basophilic inclusions*
- Suggestive of **cytomegalovirus (CMV) esophagitis**, typically seen in immunocompromised patients (HIV/AIDS, transplant recipients).
- This patient has no immunocompromised state, and CMV does not cause the cardiac manifestations or chronic megaesophagus seen here.
*Atrophy of esophageal smooth muscle cells*
- Not characteristic of Chagas disease or achalasia; these conditions typically show **smooth muscle hypertrophy** due to chronic obstruction.
- Muscle atrophy would not explain the dysphagia, megaesophagus, or cardiac findings.
*Infiltration of eosinophils in the epithelium*
- Indicates **eosinophilic esophagitis**, an allergic condition usually presenting with food impaction and dysphagia mainly for solids.
- Would not explain the cardiac manifestations or the epidemiological connection to Panama.
*Presence of metaplastic columnar epithelium*
- Represents **Barrett's esophagus**, a complication of chronic gastroesophageal reflux disease (GERD).
- The patient's presentation with dysphagia for both solids and liquids, cardiac disease, and megaesophagus on barium study points to a **motility disorder** (Chagas disease), not reflux disease.
GI motility disorders US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
GI motility disorders Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
GI motility disorders US Medical PG Question 10: A 55-year-old man presents to his primary care physician for trouble swallowing. The patient claims that he used to struggle when eating food if he did not chew it thoroughly, but now he occasionally struggles with liquids as well. He also complains of a retrosternal burning sensation whenever he eats. He also claims that he feels his throat burns when he lays down or goes to bed. Otherwise, the patient has no other complaints. The patient has a past medical history of obesity, diabetes, constipation, and anxiety. His current medications include insulin, metformin, and lisinopril. On review of systems, the patient endorses a 5 pound weight loss recently. The patient has a 22 pack-year smoking history and drinks alcohol with dinner. His temperature is 99.5°F (37.5°C), blood pressure is 177/98 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note an overweight man in no current distress. Abdominal exam is within normal limits. Which of the following is the best next step in management?
- A. Endoscopy (Correct Answer)
- B. Omeprazole trial
- C. Manometry
- D. Barium swallow
- E. CT scan
GI motility disorders Explanation: ***Endoscopy***
- The patient presents with **dysphagia to solids and liquids**, significant for **recent weight loss**, and a **history of smoking**, all of which are **alarm symptoms** necessitating an upper endoscopy to rule out malignancy.
- While he has **GERD symptoms** as well (retrosternal burning), the presence of alarm features mandates a direct investigation of the upper GI tract rather than empirical treatment.
*Omeprazole trial*
- An empirical trial of **PPIs** like omeprazole is appropriate for classic GERD symptoms without alarm features.
- However, **dysphagia to solids and liquids with associated weight loss**, especially in a patient with a significant **smoking history**, are alarm symptoms that require direct visualization via endoscopy, not just symptom management.
*Manometry*
- **Esophageal manometry** is used to evaluate the motility of the esophagus and diagnose conditions like achalasia or esophageal spasm.
- While the patient has dysphagia, **alarm symptoms (weight loss, smoking history)** raise concern for mechanical obstruction or malignancy, which should be investigated before motility disorders.
*Barium swallow*
- A **barium swallow** can identify structural abnormalities like strictures, masses, or webs, and also assess motility.
- However, in the context of alarm symptoms, a **barium swallow is less sensitive** for detecting subtle mucosal changes or early malignancy compared to endoscopy, and any positive findings would still prompt an endoscopy.
*CT scan*
- A **CT scan of the chest and abdomen** is useful for assessing extraluminal pathology, mediastinal involvement, or distant metastases.
- While it may eventually be part of staging if a malignancy is found, the **initial investigation for esophageal symptoms and alarm features** focuses on direct luminal visualization with endoscopy to identify the primary pathology.
More GI motility disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.