GI bleeding (upper and lower) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GI bleeding (upper and lower). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GI bleeding (upper and lower) US Medical PG Question 1: A 22-year-old woman comes to the emergency department because of chest and epigastric pain that started just after vomiting 30 minutes ago. She does not take any medications and does not drink alcohol or smoke cigarettes. While in the emergency department, the patient experiences two episodes of forceful, bloody emesis. Her temperature is 99.1°F (37.3°C), pulse is 110/minute, and blood pressure is 105/60 mm Hg. Physical examination shows dental enamel erosion and calluses on the dorsal aspect of her right hand. There is tenderness to palpation in the epigastrium. An x-ray of the chest is normal. Further evaluation of this patient is most likely to show which of the following findings?
- A. Rupture of the distal esophagus
- B. Friable mass in the distal esophagus
- C. Clean-based gastric ulcer
- D. Mucosal lacerations at the gastroesophageal junction (Correct Answer)
- E. Dilated veins in the esophageal submucosa
GI bleeding (upper and lower) Explanation: ***Mucosal lacerations at the gastroesophageal junction***
- This patient's symptoms (chest and epigastric pain after forceful vomiting, bloody emesis, hypotension) along with **dental enamel erosion** and **calluses on the dorsal aspect of the hand** (Russell's sign) are highly suggestive of **Mallory-Weiss tear** due to self-induced vomiting (bulimia nervosa).
- Mallory-Weiss syndrome involves **longitudinal mucosal lacerations** at the gastroesophageal junction caused by a sudden increase in intra-abdominal pressure during retching or vomiting, leading to gastrointestinal bleeding.
*Rupture of the distal esophagus*
- This describes **Boerhaave syndrome**, which is a transmural rupture of the esophagus, a more severe condition than a Mallory-Weiss tear.
- While also caused by forceful vomiting, Boerhaave syndrome would typically present with more severe symptoms, including **subcutaneous emphysema**, pleural effusion, and mediastinitis, and plain chest x-ray would often show **mediastinal air** or **pleural effusion**, which is normal in this patient.
*Friable mass in the distal esophagus*
- A friable mass would suggest an **esophageal carcinoma**, which is unlikely in a 22-year-old and typically presents with progressive dysphagia and weight loss, rather than acute pain and bleeding after vomiting.
- While bleeding can occur with esophageal tumors, the acute onset post-emesis and classic bulimia signs point away from malignancy.
*Clean-based gastric ulcer*
- A clean-based gastric ulcer is a potential cause of epigastric pain and GI bleeding, but the pain usually precedes vomiting or is exacerbated by food, and typically does not immediately follow intense retching.
- The dental enamel erosion and calluses on the hand strongly suggest a history of self-induced vomiting, making **Mallory-Weiss tear** a more specific diagnosis than a general gastric ulcer.
*Dilated veins in the esophageal submucosa*
- This describes **esophageal varices**, which are typically seen in patients with **portal hypertension** due to chronic liver disease (e.g., cirrhosis).
- The patient's history does not suggest liver disease, and variceal bleeding usually presents as painless, massive hematemesis, without the preceding forceful vomiting leading to a tear.
GI bleeding (upper and lower) US Medical PG Question 2: A 14-month-old boy has iron-deficiency anemia refractory to iron therapy. His stool is repeatedly positive for occult blood. The parents bring the child to the emergency room after they notice some blood in his stool. Which of the following is the diagnostic gold standard for this patient's most likely condition?
- A. Colonoscopy
- B. Technetium-99m pertechnetate scan (Correct Answer)
- C. Capsule endoscopy
- D. Abdominal CT with contrast
- E. Tagged red blood cell study
GI bleeding (upper and lower) Explanation: ***Technetium-99m pertechnetate scan***
- The clinical picture of **iron-deficiency anemia refractory to iron therapy**, **occult blood in the stool**, and visible blood in a 14-month-old strongly suggests a **Meckel's diverticulum** that contains ectopic gastric mucosa.
- This scan specifically detects **ectopic gastric mucosa**, which is the most common cause of bleeding from a Meckel's diverticulum, making it the **diagnostic gold standard**.
*Colonoscopy*
- While useful for evaluating the colon and rectum, **colonoscopy** is unlikely to identify a Meckel's diverticulum, which is located in the **small intestine**.
- It's primarily used for conditions like colonic polyps, inflammatory bowel disease, or lower gastrointestinal bleeding from the large bowel.
*Capsule endoscopy*
- **Capsule endoscopy** can visualize the small bowel mucosa and detect bleeding, but it does not specifically identify **ectopic gastric mucosa** and may miss a Meckel's diverticulum, especially if it's not actively bleeding at the time of the study.
- It is also less commonly used in very young children due to issues with capsule passage and retention.
*Abdominal CT with contrast*
- An **abdominal CT with contrast** can identify some structural abnormalities and inflammation but is generally not the primary diagnostic tool for a Meckel's diverticulum.
- It has **limited sensitivity** for detecting ectopic gastric mucosa or the diverticulum itself, particularly if it's small or not inflamed.
*Tagged red blood cell study*
- A **tagged red blood cell study** can detect the site of active gastrointestinal bleeding, but it does not identify the **underlying cause** of the bleeding, such as a Meckel's diverticulum.
- It requires active bleeding at a rate of at least 0.1 mL/min to be positive, and may be less specific than a Meckel's scan for this particular pathology.
GI bleeding (upper and lower) US Medical PG Question 3: A 57-year-old man is brought to the emergency department by his family because of several episodes of vomiting of blood in the past 24 hours. He has a history of alcoholic cirrhosis and is being treated for ascites with diuretics and for encephalopathy with lactulose. His vital signs include a temperature of 36.9°C (98.4°F), pulse of 85/min, and blood pressure of 80/52 mm Hg. On examination, he is confused and unable to give a complete history. He is noted to have jaundice, splenomegaly, and multiple spider angiomas over his chest. Which of the following is the best initial management of this patient?
- A. Endoscopic surveillance
- B. Non-selective beta-blockers
- C. Combined vasoactive and endoscopic therapy (Correct Answer)
- D. Balloon tamponade
- E. Transjugular intrahepatic portosystemic shunt (TIPS)
GI bleeding (upper and lower) Explanation: ***Combined vasoactive and endoscopic therapy***
- The patient presents with **hematemesis**, **hypotension**, and signs of decompensated **alcoholic cirrhosis** (jaundice, splenomegaly, spider angiomas). This clinical picture is highly suggestive of **esophageal variceal bleeding**, a life-threatening emergency.
- **Combined vasoactive drug therapy** (e.g., octreotide to reduce splanchnic blood flow) and **endoscopic therapy** (e.g., variceal ligation or sclerotherapy) are the recommended initial management for **active variceal bleeding** to control hemorrhage and prevent rebleeding.
*Endoscopic surveillance*
- **Endoscopic surveillance** is performed for patients with known varices who are **not actively bleeding** to identify varices at high risk of rupture and to initiate primary prophylaxis.
- This patient is actively bleeding, making surveillance an inappropriate initial step.
*Non-selective beta-blockers*
- **Non-selective beta-blockers** (e.g., propranolol, carvedilol) are used for **primary and secondary prophylaxis** of variceal bleeding by reducing portal pressure.
- They are **not appropriate for acute bleeding management**, as their onset of action is too slow to control active hemorrhage.
*Balloon tamponade*
- **Balloon tamponade** (e.g., with a Sengstaken-Blakemore tube) is a **temporary measure** used to control massive, refractory variceal bleeding when endoscopic therapy is unsuccessful or immediately unavailable.
- It is a **bridge to definitive management** and carries significant risks, such as **esophageal rupture** or **aspiration**, so it is not the first-line initial treatment.
*Transjugular intrahepatic portosystemic shunt (TIPS)*
- **TIPS** is typically reserved for patients with **refractory variceal bleeding** that cannot be controlled by endoscopic and pharmacologic therapy, or for those with **recurrent bleeding despite optimal secondary prophylaxis**.
- It is an **invasive procedure** and not the immediate initial intervention for acute variceal hemorrhage.
GI bleeding (upper and lower) US Medical PG Question 4: A 25-year-old man presents to the emergency department after numerous episodes of vomiting. The patient states that he thinks he ‘ate something weird’ and has been vomiting for the past 48 hours. He says that he came to the hospital because the last few times he "threw up blood". He is hypotensive with a blood pressure of 90/55 mm Hg and a pulse of 120/min. After opening an intravenous line, a physical examination is performed which is normal except for mild epigastric tenderness. An immediate endoscopy is performed and a tear involving the mucosa and submucosa of the gastroesophageal junction is visualized. Which of the following is the most likely diagnosis?
- A. Mallory-Weiss tear (Correct Answer)
- B. Hiatal hernia
- C. Esophageal varices
- D. Boerhaave syndrome
- E. Gastric ulcer
GI bleeding (upper and lower) Explanation: ***Mallory-Weiss tear***
- The patient's history of **repeated vomiting** followed by **hematemesis** is hallmark for a Mallory-Weiss tear. The endoscopic finding of a **mucosal and submucosal tear at the gastroesophageal junction** confirms this diagnosis.
- This condition is often precipitated by events that cause a sudden increase in intra-abdominal pressure, such as forceful retching or vomiting, leading to a linear tear.
*Hiatal hernia*
- A hiatal hernia involves the **protrusion of the stomach through the esophageal hiatus of the diaphragm** and would not typically cause acute hematemesis from a tear.
- While it can be associated with gastroesophageal reflux, it does not directly explain sudden-onset bleeding after vomiting.
*Esophageal varices*
- Esophageal varices are **dilated veins in the lower esophagus** usually due to **portal hypertension**, often seen in patients with liver cirrhosis.
- While varices can cause significant upper gastrointestinal bleeding, the endoscopy here reveals a tear, not ruptured varices, and there is no mention of underlying liver disease.
*Boerhaave syndrome*
- Boerhaave syndrome is a **transmural rupture of the esophagus** following forceful vomiting, which is a much more severe condition than a Mallory-Weiss tear.
- It would typically present with **severe chest pain**, **crepitus**, and signs of **mediastinitis** or **pleural effusion** due to esophageal contents leaking into the mediastinum, none of which are described here.
*Gastric ulcer*
- A gastric ulcer is an **erosion in the stomach lining** that can cause bleeding.
- While it can cause hematemesis, the endoscopic finding of a tear specifically at the **gastroesophageal junction** points away from a sole gastric ulcer as the cause.
GI bleeding (upper and lower) US Medical PG Question 5: A 65-year-old patient presents with acute left lower quadrant abdominal pain and is diagnosed with diverticulitis. Which of the following is most likely to have prevented this patient's condition?
- A. Anticoagulation with warfarin
- B. High-fiber diet (Correct Answer)
- C. Different antibiotic regimen for bronchitis
- D. Sitz baths and nifedipine suppositories
- E. Long-term use of aspirin
GI bleeding (upper and lower) Explanation: ***High-fiber diet***
- A **high-fiber diet** increases stool bulk and reduces intracolonic pressure, thereby preventing the formation of **diverticula** and reducing the risk of diverticulitis.
- It helps maintain **regular bowel movements** and minimizes straining, which are key in preventing diverticular disease.
*Anticoagulation with warfarin*
- **Warfarin** is an anticoagulant used to prevent blood clots; it has no direct impact on the formation of **diverticula** or the prevention of diverticulitis.
- While bleeding is a potential complication of diverticular disease, anticoagulation would generally *increase* the risk of bleeding, not prevent the condition itself.
*Different antibiotic regimen for bronchitis*
- Antibiotics treat **bacterial infections** and are irrelevant in the prevention of diverticulitis, which primarily relates to dietary and colonic pressure issues.
- Changing an antibiotic regimen for an unrelated respiratory infection like bronchitis would not affect the risk factors for **diverticular disease**.
*Sitz baths and nifedipine suppositories*
- **Sitz baths** and **nifedipine suppositories** are treatments for anorectal conditions like **hemorrhoids** or **anal fissures** and do not influence the development of diverticulitis.
- These interventions target symptoms in the anal region and have no physiological connection to the colon's diverticular disease processes.
*Long-term use of aspirin*
- **Aspirin** is an anti-inflammatory and antiplatelet agent used for pain relief and cardiovascular protection; it does not prevent the formation of **diverticula** or diverticulitis.
- Non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin can actually **increase the risk of diverticular complications**, such as bleeding or perforation, rather than prevent the disease.
GI bleeding (upper and lower) US Medical PG Question 6: A 41-year-old male presents to his primary care provider after seeing bright red blood in the toilet bowl after his last two bowel movements. He reports that the second time he also noticed some blood mixed with his stool. The patient denies abdominal pain and any changes in his stool habits. He notes a weight loss of eight pounds in the last two months. His past medical history is significant for an episode of pancreatitis two years ago for which he was hospitalized for several days. He drinks 2-3 beers on the weekend, and he has never smoked. He has no family history of colon cancer. His temperature is 97.6°F (36.4°C), blood pressure is 135/78 mmHg, pulse is 88/min, and respirations are 14/min. On physical exam, his abdomen is soft and nontender to palpation. Bowel sounds are present, and there is no hepatomegaly.
Which of the following is the best next step in diagnosis?
- A. Colonoscopy (Correct Answer)
- B. Complete blood count
- C. Abdominal CT
- D. Anoscopy
- E. Barium enema
GI bleeding (upper and lower) Explanation: ***Colonoscopy***
- The patient's age combined with **rectal bleeding** (bright red blood and mixed with stool) and **unexplained weight loss** are red flags for **colorectal cancer**, necessitating a thorough endoscopic evaluation of the colon.
- A colonoscopy allows for direct visualization of the entire colon and rectum, enabling **biopsy of suspicious lesions** and removal of polyps, which is crucial for diagnosis and prevention.
*Complete blood count*
- While a CBC could reveal **anemia** due to chronic blood loss, it does not identify the **source of the bleeding** or the underlying pathology like malignant lesions.
- Anemia, if present, would be a supportive finding but insufficient for a definitive diagnosis in this scenario.
*Abdominal CT*
- An abdominal CT scan can identify masses or abnormalities in the abdomen but is **less sensitive for visualizing mucosal lesions** in the colon and rectum, which are typical presentations of early colorectal cancer.
- It also does not allow for **biopsy** or therapeutic intervention, which is critical for diagnosis.
*Anoscopy*
- Anoscopy is useful for visualizing the **anal canal and distal rectum** (up to 5-6 cm), which could identify hemorrhoids or anal fissures.
- However, the patient's symptoms (blood mixed with stool, weight loss) suggest a potentially more proximal source of bleeding that would not be visible with an anoscopy alone.
*Barium enema*
- A barium enema is a less invasive imaging technique but has **lower sensitivity** compared to colonoscopy for detecting small polyps or early cancerous lesions.
- It also **does not allow for tissue biopsy** or polyp removal, which are essential steps in the management of suspected colorectal cancer.
GI bleeding (upper and lower) US Medical PG Question 7: A 74-year-old man is brought to the emergency department after he had copious amounts of blood-stained stools. Minutes later, he turned sweaty, felt light-headed, and collapsed into his wife’s arms. Upon admission, he is found to have a blood pressure of 78/40 mm Hg, a pulse of 140/min, and oxygen saturation of 98%. His family history is relevant for both gastric and colorectal cancer. His personal history is relevant for hypertension, for which he takes amlodipine. After an initial successful resuscitation with intravenous fluids, which of the following should be the first step in approaching this case?
- A. Radionuclide imaging
- B. Mesenteric angiography
- C. Upper endoscopy (Correct Answer)
- D. Colonoscopy
- E. Nasogastric lavage
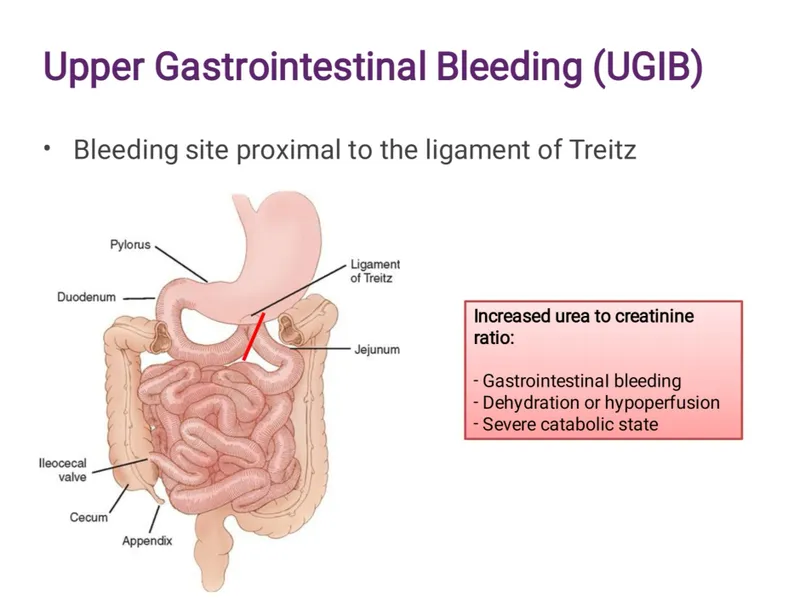
GI bleeding (upper and lower) Explanation: ***Upper endoscopy***
- After **initial hemodynamic stabilization** (as stated in the question), **early upper endoscopy** is the recommended first-line approach for patients with acute GI bleeding.
- **Upper GI sources** must be ruled out first, even in patients presenting with hematochezia (blood-stained stools), as **10-15% of cases** with bright red blood per rectum originate from an upper GI source.
- Upper endoscopy is both **diagnostic and therapeutic**, allowing for immediate intervention (banding, sclerotherapy, thermal coagulation, clipping) if a bleeding source is identified.
- **Current ACG/ASGE guidelines** recommend endoscopy **within 24 hours** (ideally within 12 hours) after resuscitation in patients with acute upper GI bleeding.
- The degree of **hemodynamic instability** in this patient (BP 78/40, HR 140) suggests a brisk bleed more consistent with an upper GI source.
*Nasogastric lavage*
- NG lavage has **low sensitivity (42-84%)** for upper GI bleeding and can miss up to 15% of cases.
- It is **no longer routinely recommended** by current guidelines as it delays definitive diagnosis and treatment without providing therapeutic benefit.
- Modern practice favors proceeding directly to endoscopy after stabilization rather than performing NG lavage first.
*Radionuclide imaging*
- **Tagged RBC scan** is useful for **intermittent or slow bleeding** (0.1-0.5 mL/min) when endoscopy is non-diagnostic.
- Not appropriate as the **first step** in an acute, massive bleed requiring immediate source localization and potential intervention.
- Provides localization but no therapeutic capability.
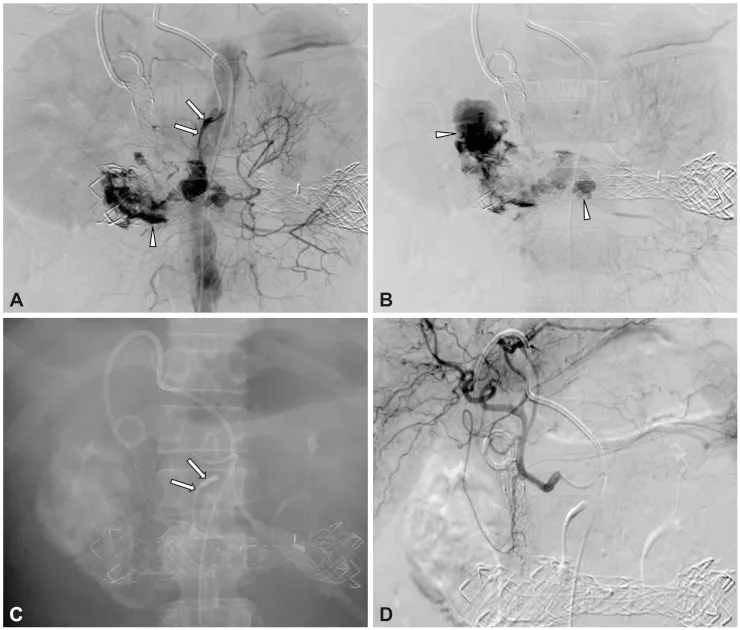
*Mesenteric angiography*
- Indicated for **active, brisk bleeding** (>0.5-1 mL/min) when endoscopy fails to identify the source or when immediate therapeutic embolization is needed.
- Can be both diagnostic and therapeutic but is typically a **second-line intervention** after endoscopy.
- Requires active bleeding at the time of the procedure to visualize the source.
*Colonoscopy*
- **Colonoscopy** is the appropriate diagnostic tool for **lower GI bleeding** after upper GI sources have been excluded.
- Should be performed **after upper endoscopy** rules out an upper source, particularly in patients with this degree of hemodynamic compromise.
- Requires adequate bowel preparation for optimal visualization, which may delay diagnosis.
GI bleeding (upper and lower) US Medical PG Question 8: A 68-year-old woman presents to her primary care physician with a complaint of fatigue, difficulty breathing upon exertion, and crampy lower abdominal pain. She also noticed that her stools appear darker than usual. She has had essential hypertension for 20 years, for which she takes bisoprolol. Her family history is positive for type 2 diabetes mellitus. On physical examination, she looks pale. Complete blood count shows the following:
Hemoglobin 10 g/dL
Mean corpuscular volume (MCV) 70 fL
Mean corpuscular hemoglobin (MCH) 25 pg/cell
Mean corpuscular hemoglobin concentration (MCHC) 27 g/dL
Red cell distribution width 16%
Platelet count 350,000/mm3
Serum ferritin 9 ng/mL
Which of the following is the best initial step for this patient?
- A. Colonoscopy (Correct Answer)
- B. Red cell transfusion
- C. Rectal hydrocortisone
- D. Intra-anal glyceryl trinitrate
- E. Double-contrast barium enema
GI bleeding (upper and lower) Explanation: ***Colonoscopy***
- The patient's symptoms (fatigue, dyspnea on exertion, darker stools, crampy lower abdominal pain) and lab findings (**microcytic hypochromic anemia** with **low ferritin and elevated RDW**) are highly suggestive of **iron deficiency anemia** due to **gastrointestinal blood loss**.
- In adults over 50 years with new-onset iron deficiency anemia, the primary concern is **colorectal cancer**, making **colonoscopy** the priority initial diagnostic test.
- While iron deficiency anemia may require evaluation of both upper and lower GI tracts, in this age group (68 years) with lower abdominal symptoms, **colonoscopy should be performed first** to rule out malignancy.
- The combination of her age, anemia, and GI symptoms warrants immediate investigation for **colon cancer** or other significant lower GI pathology.
*Red cell transfusion*
- While this provides immediate **symptomatic relief** for severe anemia, it is a supportive measure and does not address the underlying cause of the bleeding.
- Her hemoglobin of 10 g/dL is not acutely life-threatening and allows time for diagnostic workup before considering transfusion.
*Rectal hydrocortisone*
- This is used to treat **inflammatory bowel disease** or proctitis, neither of which is indicated by the presented symptoms or lab findings.
- It would not help determine the source of gastrointestinal bleeding or treat iron deficiency anemia.
*Intra-anal glyceryl trinitrate*
- This medication is primarily used to treat **anal fissures** by promoting muscle relaxation and blood flow, which is not indicated in this case.
- The patient's symptoms suggest a more significant source of blood loss than an anal fissure, which typically presents with bright red blood per rectum and severe pain on defecation.
*Double-contrast barium enema*
- This imaging technique has largely been replaced by **colonoscopy** for evaluating the colon due to its lower sensitivity for detecting small lesions and inability to obtain biopsies.
- It is not considered the best initial step for investigating GI bleeding or iron deficiency anemia in the lower tract.
GI bleeding (upper and lower) US Medical PG Question 9: A 72-year-old male with a past medical history significant for aortic stenosis and hypertension presents to the emergency department complaining of weakness for the past 3 weeks. He states that, apart from feeling weaker, he also has noted lightheadedness, pallor, and blood-streaked stools. The patient's vital signs are stable, and he is in no acute distress. Laboratory workup reveals that the patient is anemic. Fecal occult blood test is positive for bleeding. EGD was performed and did not reveal upper GI bleeding. Suspecting a lower GI bleed, a colonoscopy is performed after prepping the patient, and it is unremarkable. What would be an appropriate next step for localizing a lower GI bleed in this patient?
- A. Technetium-99 labelled erythrocyte scintigraphy (Correct Answer)
- B. Flexible sigmoidoscopy
- C. Nasogastric tube lavage
- D. Ultrasound of the abdomen
- E. CT of the abdomen
GI bleeding (upper and lower) Explanation: ***Technetium-99 labelled erythrocyte scintigraphy***
- This test can detect **slow-rate lower GI bleeds** (as low as 0.2-0.5 mL/min) that may be missed by endoscopy or colonoscopy, especially when the bleeding is intermittent or subtle.
- Given the **negative EGD** and **unremarkable colonoscopy** despite evidence of an ongoing lower GI bleed, this nuclear medicine study is appropriate for localization.
- Particularly useful in this patient with **aortic stenosis**, where angiodysplasia (vascular malformations, often in the small bowel) is a common cause of obscure GI bleeding (Heyde's syndrome).
*Flexible sigmoidoscopy*
- This procedure only visualizes the **rectum and a portion of the sigmoid colon**, which is insufficient given the negative full colonoscopy.
- It would not provide any new information for localizing a bleed that has already been ruled out from the accessible colon.
*Nasogastric tube lavage*
- This procedure is used to assess for **upper GI bleeding** by checking for blood in the gastric contents.
- The EGD already ruled out an upper GI bleed, making this step unnecessary and unhelpful for a suspected lower GI source.
*Ultrasound of the abdomen*
- Abdominal ultrasound is primarily used to evaluate **solid organs** (e.g., liver, gallbladder, kidneys) and potential fluid collections.
- It is generally **not effective** for localizing or diagnosing the source of active GI bleeding.
*CT of the abdomen*
- A standard CT abdomen without specialized imaging protocol has **limited sensitivity** for detecting the source of GI bleeding.
- While **CT angiography** (a different test with IV contrast timed to arterial phase) can detect active bleeding at rates >0.3-0.5 mL/min, a routine "CT of the abdomen" as listed in this option would not be adequate for localizing occult GI bleeding.
GI bleeding (upper and lower) US Medical PG Question 10: A 33-year-old man presents to the emergency department because of an episode of bloody emesis. He has had increasing dyspnea over the past 2 days. He was diagnosed with peptic ulcer disease last year. He has been on regular hemodialysis for the past 2 years because of end-stage renal disease. He skipped his last dialysis session because of an unexpected business trip. He has no history of liver disease. His supine blood pressure is 110/80 mm Hg and upright is 90/70, pulse is 110/min, respirations are 22/min, and temperature is 36.2°C (97.2°F). The distal extremities are cold to touch, and the outstretched hand shows flapping tremor. A bloody nasogastric lavage is also noted, which eventually clears after saline irrigation. Intravenous isotonic saline and high-dose proton pump inhibitors are initiated, and the patient is admitted into the intensive care unit. Which of the following is the most appropriate next step in the management of this patient?
- A. Observation in the intensive care unit
- B. Double-balloon tamponade
- C. Hemodialysis (Correct Answer)
- D. Transfusion of packed red blood cells
- E. Esophagogastroduodenoscopy
GI bleeding (upper and lower) Explanation: ***Hemodialysis***
- The patient has **end-stage renal disease** and missed his last dialysis session, leading to **uremic crisis** with **dyspnea** (fluid overload) and **asterixis** (uremic encephalopathy).
- **Uremic platelet dysfunction** also contributes to the GI bleeding, making dialysis essential to correct coagulopathy.
- Emergency hemodialysis is the most critical intervention to remove accumulated toxins, correct fluid overload, and improve hemostasis before any invasive procedures.
*Observation in the intensive care unit*
- While ICU admission is appropriate for monitoring, passive observation without addressing the underlying **uremia** will not resolve the critical issues of **fluid overload**, **uremic encephalopathy**, and **uremic coagulopathy**.
- The patient's missed dialysis session and severe symptoms necessitate active intervention, not just observation.
*Double-balloon tamponade*
- This procedure is reserved for **life-threatening variceal bleeding** that is refractory to endoscopic treatment.
- The patient's history of **peptic ulcer disease** (not cirrhosis) and the clearing of bloody lavage with saline irrigation suggest non-variceal bleeding, making tamponade inappropriate.
*Transfusion of packed red blood cells*
- While the patient shows signs of **orthostatic hypotension** and **tachycardia** suggesting hypovolemia, the GI bleeding has **stabilized** (NG lavage cleared with irrigation).
- Transfusion may be needed based on hemoglobin levels, but it does not address the **immediately life-threatening uremic crisis** with encephalopathy and platelet dysfunction.
- The most urgent priority is dialysis to stabilize the patient for subsequent procedures.
*Esophagogastroduodenoscopy*
- EGD is indicated to identify and potentially treat the source of **upper GI bleeding** in a patient with **peptic ulcer disease**.
- However, the patient's severe **uremic symptoms**, **encephalopathy**, and **coagulopathy** must be addressed first to safely perform this invasive procedure and optimize outcomes.
More GI bleeding (upper and lower) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.