GERD and esophageal disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GERD and esophageal disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
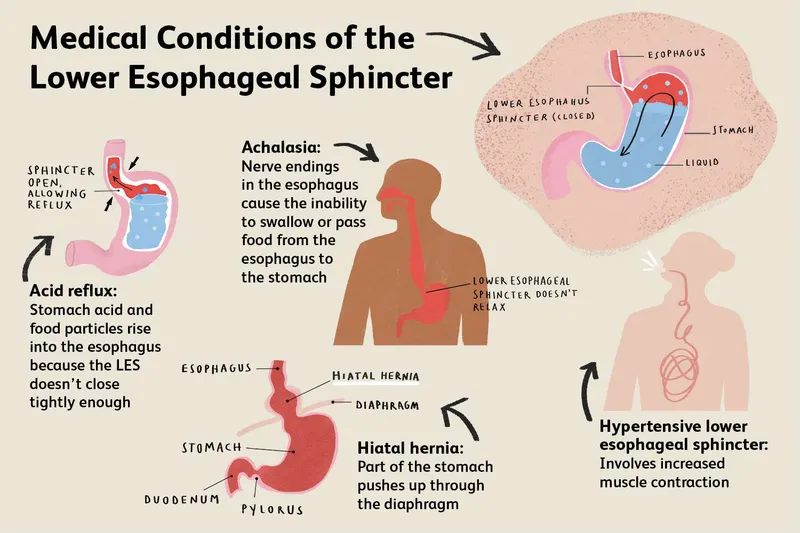
GERD and esophageal disorders US Medical PG Question 1: A scientist is studying the mechanism by which the gastrointestinal system coordinates the process of food digestion. Specifically, she is interested in how distension of the lower esophagus by a bolus of food changes responses in the downstream segments of the digestive system. She observes that there is a resulting relaxation and opening of the lower esophageal (cardiac) sphincter after the introduction of a food bolus. She also observes a simultaneous relaxation of the orad stomach during this time. Which of the following substances is most likely involved in the process being observed here?
- A. Neuropeptide-Y
- B. Secretin
- C. Ghrelin
- D. Vasoactive intestinal polypeptide (Correct Answer)
- E. Motilin
GERD and esophageal disorders Explanation: ***Vasoactive intestinal polypeptide***
- **VIP (Vasoactive intestinal polypeptide)** is a neuropeptide that mediates **relaxation** of the **smooth muscle** in the gastrointestinal tract, including the **lower esophageal sphincter** and the **orad stomach**, facilitating the passage of food.
- This relaxation is part of the **receptive relaxation** process, allowing the stomach to accommodate food without a significant increase in intragastric pressure.
*Neuropeptide-Y*
- **Neuropeptide-Y (NPY)** is primarily involved in stimulating **food intake** and **reducing energy expenditure**, acting as an orexigenic peptide.
- It does not directly mediate the relaxation of the **lower esophageal sphincter** or **orad stomach** in response to food bolus distension.
*Secretin*
- **Secretin** is a hormone released in response to **acid in the duodenum** and primarily stimulates the pancreas to release **bicarbonate-rich fluid**.
- Its main role is to neutralize stomach acid, not to mediate sphincter relaxation or stomach accommodation.
*Ghrelin*
- **Ghrelin** is known as the "**hunger hormone**" and primarily stimulates **appetite** and **growth hormone release**.
- It does not play a direct role in the relaxation of the **lower esophageal sphincter** or **orad stomach** during swallowing.
*Motilin*
- **Motilin** promotes **gastric and intestinal motility** during the **interdigestive phase**, responsible for the migrating motor complex (MMC).
- Its actions are generally prokinetic, rather than causing relaxation of the upper GI tract in response to a food bolus.
GERD and esophageal disorders US Medical PG Question 2: A 62-year-old man comes to the office complaining of dysphagia that started 4-5 months ago. He reports that he initially had difficulty swallowing only solid foods. More recently, he has noticed some trouble swallowing liquids. The patient also complains of fatigue, a chronic cough that worsens at night, and burning chest pain that occurs after he eats. He says that he has used over-the-counter antacids for "years" with mild relief. He denies any change in diet, but says he has "gone down a pant size or 2." The patient has hypertension and hyperlipidemia. He takes amlodipine and atorvastatin. He smoked 1 pack of cigarettes a day for 12 years while in the military but quit 35 years ago. He drinks 1-2 beers on the weekend while he is golfing with his friends. His diet consists mostly of pasta, pizza, and steak. The patient's temperature is 98°F (36.7°C), blood pressure is 143/91 mmHg, and pulse is 80/min. His BMI is 32 kg/m^2. Physical examination reveals an obese man in no acute distress. No masses or enlarged lymph nodes are appreciated upon palpation of the neck. Cardiopulmonary examination is unremarkable. An endoscopy is performed, which identifies a lower esophageal mass. Which of the following is the most likely diagnosis?
- A. Nutcracker esophagus
- B. Plummer-Vinson syndrome
- C. Small cell carcinoma
- D. Adenocarcinoma (Correct Answer)
- E. Squamous cell carcinoma
GERD and esophageal disorders Explanation: ***Adenocarcinoma***
- The patient's history of **dysphagia progressing from solids to liquids**, **weight loss**, and **long-standing GERD symptoms** (chronic cough, burning chest pain, use of antacids for years) are highly suggestive of **esophageal adenocarcinoma**, especially given the endoscopic finding of a **lower esophageal mass**.
- **Risk factors** present include **obesity** (BMI 32 kg/m²), **chronic GERD**, and a remote history of smoking, which contribute to the development of **Barrett's esophagus**, a precursor to adenocarcinoma.
- Adenocarcinoma typically arises in the **distal/lower esophagus** due to chronic acid reflux.
*Nutcracker esophagus*
- Characterized by **high-amplitude peristaltic contractions** of the esophagus, primarily causing **chest pain** and **dysphagia**.
- It is a **motility disorder**, not a structural lesion, and does not present with **progressive dysphagia from solids to liquids**, **weight loss**, or an **esophageal mass** on endoscopy.
*Plummer-Vinson syndrome*
- A rare condition characterized by the triad of **iron deficiency anemia**, **dysphagia**, and **esophageal webs** (typically in the upper esophagus).
- While it causes dysphagia, it does not present with an **esophageal mass**, **weight loss**, or a history of long-standing GERD.
- More common in middle-aged women and associated with increased risk of squamous cell carcinoma.
*Small cell carcinoma*
- **Small cell carcinoma** is primarily a type of **lung cancer**, although it can rarely occur in the esophagus.
- Esophageal small cell carcinoma is **very aggressive** and usually presents with symptoms similar to other esophageal cancers but is **much less common** than adenocarcinoma or squamous cell carcinoma in the esophagus.
*Squamous cell carcinoma*
- **Squamous cell carcinoma** of the esophagus is strongly associated with **smoking** and **alcohol use**, and typically arises in the **upper or middle esophagus**.
- While the patient has a remote smoking history, his **long-standing GERD**, **obesity**, and **lower esophageal mass** location make **adenocarcinoma** the more probable diagnosis, as adenocarcinoma arises from **Barrett's esophagus** in the distal esophagus due to chronic reflux.
GERD and esophageal disorders US Medical PG Question 3: A 62-year-old man is referred to a gastroenterologist because of difficulty swallowing for the past 5 months. He has difficulty swallowing both solid and liquid foods, but there is no associated pain. He denies any shortness of breath or swelling in his legs. He immigrated from South America 10 years ago. He is a non-smoker and does not drink alcohol. His physical examination is unremarkable. A barium swallow study was ordered and the result is given below. Esophageal manometry confirms the diagnosis. What is the most likely underlying cause of this patient’s condition?
- A. Pharyngoesophageal diverticulum
- B. Chagas disease (Correct Answer)
- C. Esophageal rupture
- D. Gastroesophageal reflux disease
- E. Squamous cell carcinoma of the esophagus
GERD and esophageal disorders Explanation: ***Chagas disease***
- The patient's history of living in **South America** and presenting with **dysphagia for both solids and liquids** (suggesting a motility disorder), along with the **barium swallow image showing esophageal dilation and a 'bird's beak' appearance** at the gastroesophageal junction, are highly characteristic of achalasia caused by Chagas disease.
- Chagas disease, caused by *Trypanosoma cruzi*, leads to the destruction of **myenteric plexus neurons** in the esophagus, resulting in achalasia (failure of the lower esophageal sphincter to relax) and megaesophagus.
*Pharyngoesophageal diverticulum*
- This typically presents as **Zenker's diverticulum**, causing **difficulty initiating a swallow**, regurgitation of undigested food, and sometimes halitosis, which is different from the described dysphagia for both solids and liquids.
- A Zenker's diverticulum would appear as a **pouch-like protrusion** in the posterior pharynx, not the diffuse esophageal dilation seen in the image.
*Esophageal rupture*
- Esophageal rupture (Boerhaave syndrome) is an acute, life-threatening condition associated with **severe chest pain, vomiting, and crepitus**, not a chronic, progressive dysphagia without pain.
- Imaging would reveal **extravasation of contrast** into the mediastinum or pleural space, not the smooth dilation and distal narrowing observed.
*Gastroesophageal reflux disease*
- While chronic GERD can lead to **strictures** and dysphagia, it typically causes **heartburn**, regurgitation, and sometimes odynophagia, and the dysphagia is usually progressive for solids first.
- The barium swallow would show reflux or a stricture, not the **classic achalasia findings** of a dilated esophagus tapering to a narrow distal segment.
*Squamous cell carcinoma of the esophagus*
- Squamous cell carcinoma usually presents with **progressive dysphagia, initially for solids**, and is often associated with weight loss, smoking, and alcohol use, none of which are present in this patient.
- A tumor would typically appear as an **irregular, focal narrowing or mass** on barium swallow, not the smooth, diffuse dilation seen in this image.
GERD and esophageal disorders US Medical PG Question 4: A 45-year-old man presents to the emergency department with difficulties swallowing food. He states that he experiences pain when he attempts to swallow his medications or when he drinks water. He reveals that he was diagnosed with HIV infection five years ago. He asserts that he has been taking his antiretroviral regimen, including emtricitabine, rilpivirine, and tenofovir. His temperature is 98°F (37°C), blood pressure is 100/60 mmHg, pulse is 90/min, respirations are 22/min, and oxygen saturation is 99% on room air. His physical exam is notable for a clear oropharynx, no lymphadenopathy, and a normal cardiac and pulmonary exam. No rashes are noted throughout his body. His laboratory results are displayed below:
Hemoglobin: 12 g/dL
Hematocrit: 37 %
Leukocyte count: 8,000/mm^3 with normal differential
Platelet count: 160,000/mm^3
Serum:
Na+: 138 mEq/L
Cl-: 108 mEq/L
K+: 3.5 mEq/L
HCO3-: 26 mEq/L
BUN: 35 mg/dL
Glucose: 108 mg/dL
Creatinine: 1.1 mg/dL
CD4+ count: 90/mm^3
HIV viral load: 59,000 copies/mL
What is the best next step in management?
- A. Fluconazole (Correct Answer)
- B. Nystatin
- C. Oral swab and microscopy
- D. Methylprednisolone
- E. Esophageal endoscopy and biopsy
GERD and esophageal disorders Explanation: ***Fluconazole***
- The patient's **odynophagia**, low **CD4+ count**, and high **HIV viral load** are highly suggestive of **esophageal candidiasis**.
- **Fluconazole** is the initial empiric treatment of choice for suspected esophageal candidiasis in HIV-positive patients, given its high efficacy and good tolerability.
*Nystatin*
- **Nystatin** is typically used for **oral candidiasis (thrush)**, which presents with white plaques in the mouth.
- The patient has a **clear oropharynx** and **odynophagia**, indicating esophageal involvement, for which nystatin is less effective.
*Oral swab and microscopy*
- While an **oral swab** can confirm oral candidiasis, it is not sufficient for diagnosing **esophageal candidiasis**.
- Given the patient's symptoms of odynophagia and high clinical suspicion in an immunocompromised patient, empiric treatment is preferred over initial diagnostic testing for uncomplicated esophageal candidiasis.
*Methylprednisolone*
- **Methylprednisolone** is a corticosteroid used to reduce inflammation and is not indicated for the treatment of **candidal infections**.
- Using corticosteroids in an immunocompromised patient with an active opportunistic infection could worsen his condition.
*Esophageal endoscopy and biopsy*
- **Esophageal endoscopy and biopsy** are typically reserved for patients who **fail empiric antifungal therapy** or present with **atypical symptoms** not consistent with candidiasis.
- Given the clear clinical picture, initial empiric treatment with fluconazole is the standard first step.
GERD and esophageal disorders US Medical PG Question 5: A 27-year-old woman presents with painful swallowing for the past 2 days. She received a kidney transplant 3 months ago for lupus-induced end-stage renal disease. She takes tacrolimus, mycophenolate mofetil, prednisone, and calcium supplements. The blood pressure is 120/80 mm Hg, the pulse is 72/min, the respirations are 14/min, and the temperature is 38.0°C (100.4°F). Esophagoscopy shows serpiginous ulcers in the distal esophagus with normal surrounding mucosa. Biopsy shows large cytoplasmic inclusion bodies. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Ganciclovir (Correct Answer)
- B. Budesonide
- C. No pharmacotherapy at this time
- D. Fluconazole
- E. Pantoprazole
GERD and esophageal disorders Explanation: ***Ganciclovir***
- The patient's presentation with **painful swallowing**, **serpiginous ulcers in the distal esophagus**, and **large cytoplasmic inclusion bodies** on biopsy, especially in an immunocompromised patient (kidney transplant recipient), is highly suggestive of **cytomegalovirus (CMV) esophagitis**.
- **Ganciclovir** is the first-line antiviral treatment for CMV infections, including esophagitis, particularly in transplant patients.
*Budesonide*
- **Budesonide** is a corticosteroid often used for inflammatory conditions like Crohn's disease or eosinophilic esophagitis.
- It is not indicated for viral infections and could potentially worsen the patient's immunocompromised state.
*No pharmacotherapy at this time*
- The patient has a clear symptomatic infection with characteristic findings (ulcers, inclusion bodies) in an immunocompromised state (post-transplant).
- Delaying treatment could lead to serious complications and dissemination of the CMV infection.
*Fluconazole*
- **Fluconazole** is an antifungal medication primarily used to treat *Candida* esophagitis, which typically presents with **linear, white plaques** and not serpiginous ulcers with cytoplasmic inclusion bodies.
- The biopsy findings rule out candidal infection, for which fluconazole would be appropriate.
*Pantoprazole*
- **Pantoprazole** is a proton pump inhibitor (PPI) used to reduce stomach acid, commonly prescribed for esophagitis due to reflux disease.
- While acid suppression can be part of supportive care, it does not address the underlying **viral etiology** of this patient's symptoms (CMV esophagitis).
GERD and esophageal disorders US Medical PG Question 6: A 56-year-old woman presents to her primary care physician complaining of heartburn, belching, and epigastric pain that is aggravated by coffee and fatty foods. She states that she has recently been having difficulty swallowing in addition to her usual symptoms. What is the most appropriate next step in management of this patient?
- A. Trial of an H2 receptor antagonist
- B. Trial of a proton pump inhibitor
- C. Upper endoscopy (Correct Answer)
- D. Nissen fundoplication
- E. Lifestyle changes - don't lie down after eating; avoid spicy foods; eat small servings
GERD and esophageal disorders Explanation: ***Upper endoscopy***
- The presence of **dysphagia** (difficulty swallowing) in a patient with chronic reflux symptoms is an **alarm symptom** that warrants immediate investigation to rule out serious conditions like **esophageal strictures** or **malignancy**.
- **Upper endoscopy** allows direct visualization of the esophagus, stomach, and duodenum, and enables biopsies if abnormalities are found.
*Trial of an H2 receptor antagonist*
- While H2 receptor antagonists can help manage reflux symptoms, they are generally prescribed for **mild to moderate GERD** without alarm symptoms.
- Starting this treatment without investigation could **delay diagnosis** of a potentially life-threatening condition given the dysphagia.
*Trial of a proton pump inhibitor*
- Proton pump inhibitors (PPIs) are highly effective for GERD symptoms and are often used as a first-line treatment for typical reflux.
- However, the presence of **dysphagia** is an **alarm symptom** that mandates further investigation with endoscopy before initiating or continuing empirical PPI therapy.
*Nissen fundoplication*
- **Nissen fundoplication** is a surgical procedure for severe GERD that is typically considered after **medical management has failed** and an **objective diagnosis** of GERD has been confirmed, often with endoscopy and pH monitoring.
- It is an **intervention**, not a diagnostic step, and would only be considered once the cause of dysphagia has been identified and ruled out for malignancy.
*Lifestyle changes - don't lie down after eating; avoid spicy foods; eat small servings*
- **Lifestyle modifications** are key components of GERD management and should be recommended to all patients with reflux symptoms.
- While beneficial, these changes alone are insufficient when an **alarm symptom** like dysphagia is present, as they would not address underlying structural issues or malignancy.
GERD and esophageal disorders US Medical PG Question 7: A 47-year-old man with gastroesophageal reflux disease comes to the physician because of severe burning chest pain and belching after meals. He has limited his caffeine intake and has been avoiding food close to bedtime. Esophagogastroduodenoscopy shows erythema and erosions in the distal esophagus. Which of the following is the mechanism of action of the most appropriate drug for this patient?
- A. Enhancement of the mucosal barrier
- B. Inhibition of ATPase (Correct Answer)
- C. Inhibition of H2 receptors
- D. Neutralization of gastric acid
- E. Inhibition of D2 receptors
GERD and esophageal disorders Explanation: **Inhibition of ATPase**
- The patient's symptoms (severe burning chest pain, belching after meals) and EGD findings (erythema and erosions in the distal esophagus) are classic for **Gastroesophageal Reflux Disease (GERD)**.
- The most effective treatment for GERD involves **proton pump inhibitors (PPIs)**, which work by irreversibly inhibiting the **H+/K+-ATPase** (proton pump) in the gastric parietal cells, thereby reducing acid secretion.
*Enhancement of the mucosal barrier*
- Medications that enhance the mucosal barrier, like **sucralfate**, provide a protective layer and are primarily used for stress ulcers or as an adjunct therapy, not as first-line treatment for erosive esophagitis.
- While beneficial, this mechanism does not directly address the *overproduction of acid* that is the primary cause of reflux and esophageal damage in GERD.
*Inhibition of H2 receptors*
- **H2-receptor blockers** (e.g., ranitidine, cimetidine) reduce acid secretion by blocking histamine's action on parietal cells, but they are generally less potent and effective than PPIs for healing erosive esophagitis.
- They tend to lose effectiveness over time due to **tachyphylaxis** and are often used for milder GERD symptoms or as maintenance therapy.
*Neutralization of gastric acid*
- **Antacids** (e.g., calcium carbonate, aluminum hydroxide) provide rapid, but temporary, relief by directly neutralizing existing stomach acid.
- They do not prevent acid production, making them unsuitable for managing persistent erosive esophagitis.
*Inhibition of D2 receptors*
- This mechanism is characteristic of **dopamine antagonists**, primarily used as antiemetics (e.g., metoclopramide) or antipsychotics (e.g., haloperidol).
- While metoclopramide can increase esophageal sphincter tone and gastric emptying, it is not the primary mechanism of action for the most effective drug in treating erosive esophagitis.
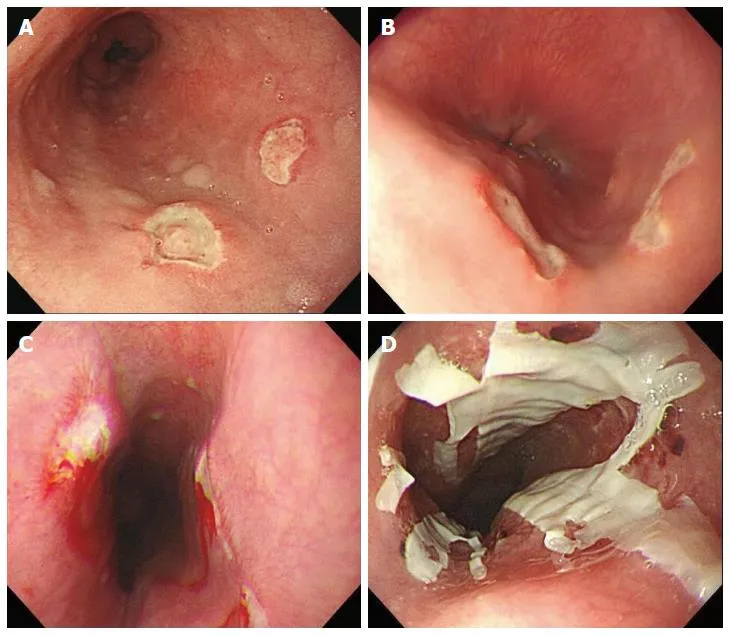
GERD and esophageal disorders US Medical PG Question 8: A 55-year-old man comes to the physician because of heartburn for the past 2 years. He has no chest pain, dysphagia, weight loss, or fever. He has no history of any serious illnesses. He takes omeprazole daily. Vital signs are within normal limits. Body mass index (BMI) is 34 kg/m2. Physical exam shows no abnormalities. An endoscopic image of the lower esophageal sphincter is shown. Which of the following is the most important next step in management?
- A. Endoscopic mucosal ablation therapy
- B. Esophagectomy
- C. High-dose pantoprazole
- D. Multiple endoscopic biopsies (Correct Answer)
- E. Laparoscopic Nissen fundoplication
GERD and esophageal disorders Explanation: ***Multiple endoscopic biopsies***
- The endoscopic image likely shows **Barrett's esophagus**, characterized by metaplastic columnar epithelium. This condition is a precursor to **esophageal adenocarcinoma**.
- **Biopsies** are crucial to assess for the presence and grade of **dysplasia**, which dictates further management strategies.
*Endoscopic mucosal ablation therapy*
- This therapy is typically reserved for patients with **high-grade dysplasia** or **intramucosal carcinoma** in Barrett's esophagus, after diagnosis has been confirmed by biopsy.
- It would be premature to consider ablation without a definitive histological diagnosis of dysplasia.
*Esophagectomy*
- **Esophagectomy** is a major surgical procedure reserved for advanced esophageal cancer or high-grade dysplasia refractory to endoscopic therapies.
- It is an overly aggressive and inappropriate initial step without histological confirmation and assessment of dysplasia or cancer.
*High-dose pantoprazole*
- While proton pump inhibitors (PPIs) like pantoprazole are used to manage GERD symptoms and may help prevent progression of Barrett's esophagus, this patient is already on omeprazole daily.
- Simply increasing the dose of PPI does not address the need for **histological evaluation** of the abnormal-appearing mucosa for dysplasia or cancer.
*Laparoscopic Nissen fundoplication*
- This surgical procedure aims to strengthen the lower esophageal sphincter to treat severe GERD when medical management fails.
- While it addresses reflux, it does not directly evaluate or treat the potential **precancerous changes** in the esophageal lining seen on endoscopy, making biopsies a more immediate and critical next step.
GERD and esophageal disorders US Medical PG Question 9: A 45-year-old African American male presents to his primary care physician complaining of difficulty swallowing that was initially limited to solids but has now progressed to liquids. Biopsy of the esophagus reveals dysplastic cells, but does not show evidence of glands or increased mucin. Which of the following most contributed to his condition?
- A. Gastroesophageal reflux disease
- B. Obesity
- C. Drinking extremely hot beverages
- D. Radiation exposure in the past 6 months
- E. Smoking (Correct Answer)
GERD and esophageal disorders Explanation: ***Smoking***
- **Smoking** is the most significant risk factor for **squamous cell carcinoma** of the esophagus, which is strongly suggested by the biopsy findings of **dysplastic cells without glands or mucin**.
- The combination of **progressive dysphagia** (solids to liquids) and smoking history in an **African American male** fits the classic demographic and presentation pattern for esophageal squamous cell carcinoma.
*Gastroesophageal reflux disease*
- **GERD** primarily leads to **esophageal adenocarcinoma** through **Barrett's esophagus**, which would show **glandular metaplasia** and **increased mucin production** on biopsy.
- The biopsy explicitly states **absence of glands and mucin**, making GERD-related adenocarcinoma unlikely as the primary pathologic process.
*Obesity*
- **Obesity** increases risk of **esophageal adenocarcinoma** by worsening **GERD** and promoting **Barrett's esophagus** development.
- Since the biopsy findings suggest **squamous cell carcinoma** rather than adenocarcinoma, obesity is not the most direct contributing factor in this case.
*Drinking extremely hot beverages*
- **Hot beverage consumption** is indeed a risk factor for **squamous cell carcinoma** of the esophagus, particularly in certain geographic regions.
- However, **smoking** remains the more prevalent and significant risk factor globally, especially when combined with **alcohol use**, making it the primary contributor.
*Radiation exposure in the past 6 months*
- **Radiation exposure** can increase risk of esophageal cancer, including **squamous cell carcinoma**, but typically requires a **longer latency period** (years to decades).
- A **6-month timeframe** is insufficient for radiation-induced carcinogenesis to manifest as advanced cancer with dysphagia and dysplastic changes.
GERD and esophageal disorders US Medical PG Question 10: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
GERD and esophageal disorders Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
More GERD and esophageal disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.